Abstract
Objective:
Assess the effect of abatacept on progression of structural damage over 2 years in patients with rheumatoid arthritis who had an inadequate response to methotrexate.
Methods:
539 patients entered an open-label extension of the AIM (Abatacept in Inadequate responders to Methotrexate) trial and received abatacept. Radiographic assessment of the hands and feet was performed at baseline, year 1 and year 2. At year 2, each patient’s radiographs were scored for progression blinded to sequence and treatment allocation.
Results:
In patients treated with abatacept for 2 years, greater reduction in progression of structural damage was observed in year 2 than in year 1. The mean change in total Genant-modified Sharp scores was reduced from 1.07 units in year 1 to 0.46 units in year 2. Similar reductions were observed in erosion and joint space narrowing scores. Following 2 years of treatment with abatacept, 50% of patients had no progression of structural damage as defined by a change in the total score of ⩽0 compared with baseline. 56% of patients treated with abatacept had no progression during the first year compared with 45% of patients treated with placebo. In their second year of treatment with abatacept, more patients had no progression than in the first year (66% vs 56%).
Conclusions:
Abatacept has a sustained effect that inhibits progression of structural damage. Furthermore, the mean change in radiographic progression in patients treated with abatacept for 2 years was significantly lower in year 2 versus year 1, suggesting that abatacept may have an increasing disease-modifying effect on structural damage over time.
Rheumatoid arthritis (RA) is a chronic autoimmune disease that usually leads to synovial joint damage and consequent disability. Activated T cells play a crucial part in the immunopathology of RA.1 T cell proliferation and interaction with other cell types, including synovial macrophages, fibroblasts and B cells, result in the production of proinflammatory cytokines and matrix metalloproteinases that promote synovitis and erosive loss of subchondral bone. Thus, targeting T cell activation is a rational therapeutic approach for the treatment of RA.
T cell activation requires antigen recognition by the T cell receptor, referred to as signal 1, as well as a co-stimulatory signal, referred to as signal 2.2 One of the best characterised co-stimulatory pathways involves the interaction of CD28 expressed on T cells with CD80 and CD86 expressed on antigen-presenting cells. Endogenous down-regulation of CD28-mediated T cell co-stimulation occurs through T cell expression of cytotoxic T lymphocyte antigen 4 (CTLA-4). CTLA-4 binds to CD80 and CD86 with higher avidity than CD28, thus preventing co-stimulation through this pathway, and is a major down-regulatory signal for T cells.
Abatacept is a soluble, recombinant, fully human fusion protein composed of the extracellular domain of human CTLA-4 and the Fc domain of human IgG1, which has been modified to prevent complement fixation. Abatacept is the first in a class of biological agents that target the second signal required for full T cell activation, a mechanism of action that is fundamentally different than any other current biological RA therapy. The efficacy of abatacept monotherapy has been shown in a phase IIa trial in patients with RA with an inadequate response to disease-modifying anti-rheumatic drugs (DMARDs).3 The efficacy of abatacept added to methotrexate (MTX) was demonstrated in the phase IIb and phase III trials of patients with an inadequate response to MTX or tumour necrosis factor-targeting agents.4–6
Results from the 1-year phase III, randomised, double-blind trial of Abatacept in Inadequate responders to Methotrexate (AIM) trial have been previously reported.5 Abatacept added to MTX therapy resulted in clinically significant improvements in the signs and symptoms of RA, physical function and health-related quality of life in patients with an inadequate response to MTX. Further, abatacept resulted in a statistically significant slowing of the progression of structural damage after 12 months of treatment.
Progressive structural damage is associated with increasing disability over time.7 8 Thus, the effects of abatacept treatment on radiographic outcomes were assessed over longer-term treatment. Here we present radiographic assessments after 2 years of abatacept treatment in an open-label extension of the AIM trial. These data demonstrate that radiographic progression is significantly inhibited over the 2 years. The maintenance of efficacy of abatacept therapy on other clinical end points will be described in full in another report.
PATIENTS AND METHODS
The study design, baseline characteristics and results of the 12-month double-blind phase of this trial have been reported previously.5 Institutional review boards or independent ethics committees approved the clinical protocol, and written informed consent to the study protocol was provided by each patient.
Patients
Patients eligible to participate in the AIM trial were at least 18 years of age, met the American Rheumatism Association criteria for RA,9 and had RA for at least 12 months. All patients were screened for tuberculosis. At randomisation, all patients had persistent, active RA despite treatment with MTX, with ⩾10 swollen joints, ⩾12 tender joints and a C-reactive protein concentration of ⩾1.0 mg/dl. Patients were required to have received MTX therapy at a minimum dose of 15 mg/week for at least 3 months, with the dose having been stable for a minimum of 28 days prior to randomisation. A 28-day washout period was required for all other DMARDs. Reduction of MTX dosage in the first 6 months was permitted only in cases of toxicity. Stable dosages of nonsteroidal anti-inflammatory drugs or corticosteroids at ⩽10 mg prednisone/day were allowed, with a stable dosage for 25 days prior to randomisation. Adjustment of MTX and/or corticosteroid dosages were permitted after month 6, as was treatment with an additional DMARD if deemed appropriate by the investigator, including hydroxychloroquine, sulfasalazine, gold or azathioprine.
Study protocol
During the first year, patients were randomised to receive a fixed dose of abatacept of approximately 10 mg/kg body weight or placebo in a 2:1 ratio. The dose of abatacept was 500 mg for patients weighing less than 60 kg, 750 mg for patients weighing 60–100 kg, and 1 g for patients weighing more than 100 kg. Study medication was infused intravenously over 30 min on days 1, 15 and 29, and every 28 days subsequently. Patients completing the double-blind period were eligible to enter an open-label, long-term extension and receive abatacept therapy every 28 days at a dose of approximately 10 mg/kg, as described above. The loading dose used in the double-blind period was not utilised here. No premedication was required for the intravenous infusions.
Radiographic evaluation
Radiographic assessments of hands, wrists and feet were performed at baseline, year 1 and year 2, or upon early termination. The trial was powered for radiographic findings at year 1, and the primary end point was the change in erosion score, with secondary assessments of joint space narrowing (JSN) and total score using the Genant-modified Sharp scoring system.5 For each patient, baseline, year 1 and year 2 radiographs were all re-read at year 2 by two independent expert readers blinded to the original treatment allocation and the sequence of films.10
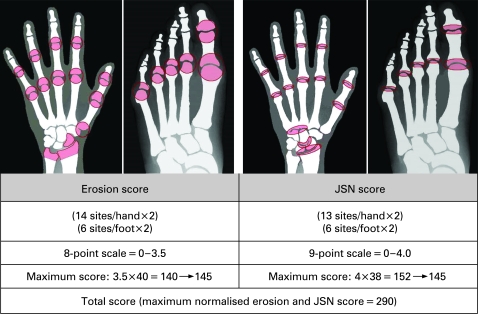
The Genant-modified Sharp scoring system (fig 1) assesses changes in structural damage, assigning scores for erosions of 0–3.5 (eight gradations) for 14 sites in each hand and wrist, and six sites in each foot.11 12 JSN scores of 0–4 (nine gradations) are assigned to 13 sites in each hand and six sites in each foot.12 The erosion and JSN scores are normalised to 145 for a maximum total Genant-modified Sharp score of 290.12 Inter-reader, intra-class correlation coefficient (ICC) was determined based on the baseline and year 1 readings.10 Smallest detectable difference was determined as 1.96 SD of the two independent baseline readings.13
Figure 1. Genant-modified Sharp scoring system. Coloured areas indicate sites used to evaluate erosion and joint space narrowing (JSN) scores. Each site was evaluated in 0.5-unit increments as indicated. Erosion and JSN scores are normalised to 145 for a maximum total score of 290.
Statistical analysis
The study was powered for change from baseline in the Genant-modified Sharp erosion score and used a rank-based analysis of covariance to compare changes between treatment groups at year 1. The radiographic analyses were performed on a modified intent-to-treat population at year 2. The modified intent-to-treat population included patients who were randomised and treated, completed the 1-year double-blind period, and continued to receive at least one dose of study medication during the open-label period. Patients who discontinued abatacept treatment during the open-label period were requested to return for follow-up radiography at year 2, regardless of any subsequent new anti-rheumatic therapy prescribed by the investigator. Radiographs were taken at the time of discontinuation in patients who were unwilling or unable to return at year 2. In these patients, 2-year data were imputed using linear extrapolation of the scores of the discontinuation film.
The changes from baseline in total Genant-modified Sharp scores, erosion scores and JSN scores were charted as cumulative probability plots to visually represent the distribution of all radiographic data. The observed cumulative proportion (scores ranked from the lowest to the highest and presented as a cumulative proportion of all scores) was plotted against the actual change from baseline of each score. The proportion of observations that fall below each possible change from baseline (y-axis) can be read on the x-axis.14
RESULTS
Patients and study completion
Of the 652 patients randomised and treated in the double-blind portion of the AIM trial, 433 received abatacept and 219 received placebo (table 1). As previously reported, baseline demographics and clinical characteristics did not differ significantly between patients in the abatacept and placebo groups.5 After the 12-month double-blind treatment period, all patients were eligible to receive open-label treatment with abatacept. More patients receiving abatacept treatment (89%) completed the 1-year double-blind phase relative to the placebo group (74%). Of the 547 patients who completed 12 months of treatment, 539 (83% of all randomised and treated patients) were treated with abatacept in the open-label period (378 initially randomised to abatacept (87%) and 161 to placebo (73.5%)). A high retention rate was maintained with open-label abatacept treatment, with 90% of the patients who entered the long-term extension completing 2 years.
Table 1. Number of subjects with radiographic assessments on days 365 and 729.
| Abatacept n = 376 (%) | Placebo n = 160 (%) | |
| Subjects included in analyses | ||
| Day 365 | 328 (87.2) | 144 (90.0) |
| Baseline and day 365 | 328 (87.2) | 144 (90.0) |
| Day 729 | 324 (86.2) | 143 (89.4) |
| Baseline and day 729 | 315 (83.8) | 139 (86.9) |
| Imputation on day 729* | 9 (2.4) | 4 (2.5) |
| Subjects not included in the analyses | ||
| No day 365 value† | 2 (0.5) | 1 (0.6) |
| No day 729 value‡ | 6 (1.6) | 2 (1.3) |
*Subjects are discontinued and qualified for imputation requirement. †Two subjects in the abatacept group had evaluative radiographic assessment outside the pre-specified visit window of day 365, and one subject in the placebo group had no radiographic assessment on day 365. ‡Subjects had evaluative radiographic assessment outside the pre-specified visit window of day 729.
Two-year radiographic data were available from 87% of patients who entered the open-label period, which comprises 72% of all randomised and treated patients (467 of 652 patients; table 1). Observed data were available for 97% of patients who completed the open-label period; 454 of 467 patients had radiographs at baseline and at year 2. Baseline and an early termination film were available for the remaining 3% of patients, and 2-year data were imputed by linear extrapolation. The data include baseline and year 2 radiographs of 324 patients treated with abatacept for 2 years (observed data in 315 patients, imputed data in nine patients). Therefore, the 2-year data represent the majority of randomised patients. As previously reported in an abstract,10 a high degree of inter-observer agreement was demonstrated by ICC for radiographic assessments at baseline (0.90) and 12 months (0.92) and for change between baseline and 12 months (0.82). The smallest detectable differences were 3.5, 2.5 and 5.1, respectively, for erosion, JSN and total score. These correspond to 1.9%, 1.3% and 1.3%, respectively, of the maximum values for each of these scores and compare favourably with values reported for other studies.15 16
Radiographic results: population-level data
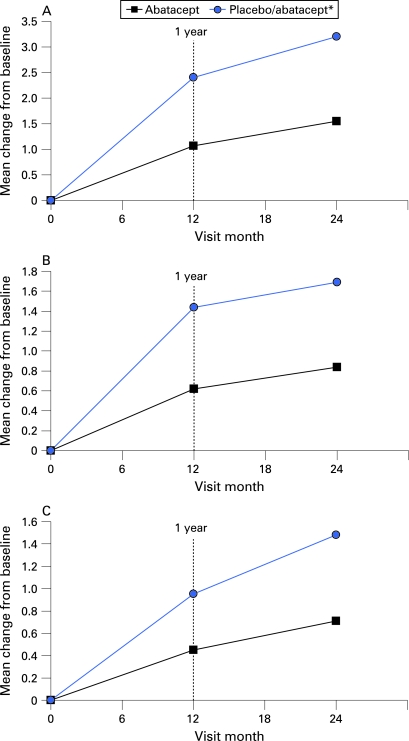
The progression of structural damage was significantly reduced in patients treated with abatacept over 2 years versus those treated with placebo initially. Baseline erosion and JSN scores were comparable in patients originally randomised to either treatment group. Significantly lower mean changes in radiographic progression were observed in patients treated with abatacept for 2 years, with mean changes in total score, erosion and JSN scores of 1.55, 0.84 and 0.71 units, respectively, compared with 3.17, 1.48 and 1.69 units in patients treated with placebo for 12 months prior to abatacept open-label therapy (fig 2, table 2).
Figure 2. Mean change from baseline in total (A), erosion (B) and joint space narrowing (C) Genant-modified Sharp scores for patients at 12 months and 2 years. *Placebo patients were switched to abatacept after 12 months. All patients received background methotrexate.
Table 2. Yearly mean changes in Genant-modified Sharp scores.
| Δ Baseline to year 1 | Δ Baseline to year 2 | Δ Year 1 to year 2 | |
| Total score | |||
| Abatacept | 1.07 | 1.55 | 0.46 |
| Placebo/abatacept | 2.40 | 3.17 | 0.75 |
| Erosion score | |||
| Abatacept | 0.62 | 0.84 | 0.21 |
| Placebo/abatacept | 1.44 | 1.69 | 0.25 |
| Joint space narrowing score | |||
| Abatacept | 0.45 | 0.71 | 0.24 |
| Placebo/abatacept | 0.95 | 1.48 | 0.50 |
Baseline is day 1 of study. All randomised and treated patients who entered the open-label period and had radiographs at baseline and year 1. Baseline and year 1 radiographs were re-read at day 729. Placebo patients were switched to abatacept in the long-term extension (year 2). All patients received background methotrexate.
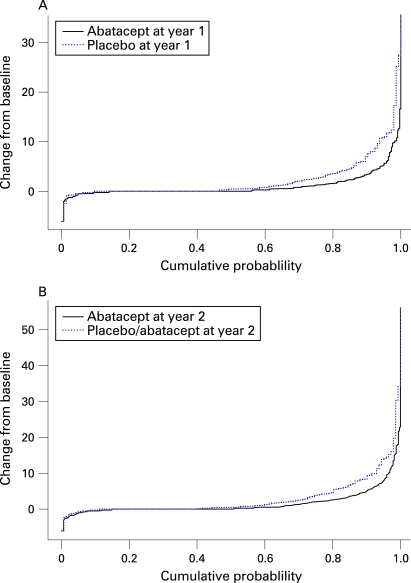
Patients treated with abatacept for 2 years also had lower median changes in radiographic progression scores. The median change from baseline in total Genant-modified Sharp scores was 0.0 units at year 1 and year 2 with abatacept treatment (fig 3), versus median changes of 0.46 and 0.51 units at year 1 and year 2, respectively, in patients who received placebo prior to abatacept therapy. Further, the median change in erosion score was 0.0 units in patients treated with abatacept for 2 years, compared with 0.26 units in patients originally in the placebo group.
Figure 3. Cumulative probability distribution of changes from baseline in Genant-modified total Sharp scores by treatment at year 1 (A) and year 2 (B). The solid line represents patients treated with abatacept (A,B) and the dotted line represents patients treated with placebo (A) or treated with placebo for 12 months then abatacept for 12 months (B). All patients received background methotrexate.
The mean change in the total score, erosion and JSN score were lower from year 1 to year 2 (0.46, 0.21 and 0.24 units, respectively) than the mean change in these scores from baseline to year 1 (1.07, 0.62 and 0.45 units, respectively) in patients treated with abatacept for up to 2 years (table 2). The increasing effect of treatment was consistently observed for both erosions and JSN.
Radiographic results: patient-level data
Radiographic results at 2 years demonstrate the maintenance of effect of abatacept and MTX on non-progression of structural damage in patients with no progression at year 1 (table 3), defined as a change from baseline in total Sharp score of ⩽0. Overall, 50% of patients treated with abatacept did not progress from baseline to 2 years of treatment (163 of 324 patients). At 2 years, non-progression in erosions and JSN (change ⩽0) was observed from baseline in 56% and 68% of these patients, respectively. In patients treated with abatacept with no radiographic progression at year 1, 79% had no radiographic progression at year 2. Non-progression in erosions and JSN was maintained at 2 years in 83% and 87% of patients with no progression at 12 months.
Table 3. Patients with no progression in structural damage measured by Genant-modified Sharp scores in patients on abatacept therapy for 2 years.
| Percentage of patients with no progression in structural damage* | Percentage of patients with no progression in structural damage in year 2† | ||||
| Outcome | Baseline to year 1 (n = 328) | Baseline to year 2 (n = 324) | Non-progressors at end of year 1 remaining non-progressors† | Progressors at end of year 1 becoming non-progressors | |
| Erosion (%) | 61 | 56 | 83 | 49 | |
| Joint space narrowing (%) | 74 | 68 | 87 | 52 | |
| Total (%) | 56 | 50 | 79 | 45 | |
All patients received background methotrexate.
*Defined by a change in the total score of ⩽0 from baseline to year 1. †Defined by a change in the total score of ⩽0 from year 1 to year 2.
Non-progression at year 2 was also achieved in patients with initial damage progression on abatacept therapy. Of patients treated with abatacept who demonstrated radiographic progression at year 1, 45% had no progression of structural damage at year 2 (64 of 142 patients). Further, 53% of patients originally randomised to placebo with progression at year 1 did not progress at year 2 after receiving abatacept treatment (42 of 79 patients).
Cumulative probability plots showing the distribution of change from baseline in total Genant-modified Sharp scores for year 1 and year 2 are shown in fig 3. Comparison of the curves in patients treated in the abatacept group (solid line) versus patients originally randomised to placebo (dotted line) demonstrates that abatacept treatment is associated with results in decreased numbers of patients with progression of structural damage. Furthermore, the amount of structural damage in patients who progressed is lower in patients treated with abatacept for both year 1 and year 2.
DISCUSSION
Abatacept has been shown to significantly reduce disease activity in patients with RA. The previously described randomised, double-blind, placebo-controlled portion of the phase III study of abatacept in patients with RA with an inadequate response to MTX demonstrated statistically significant improvement in the signs and symptoms of disease, physical function assessed by the health-assessment questionnaire disability index, and health-related quality of life.5 In addition, abatacept positively impacted the rate of structural damage progression at 12 months, reducing it by approximately 50% compared with placebo. This placebo-controlled radiographic finding from randomised clinical trials provides an assessment of short-term effects on structural damage. However, only long-term radiographic progression has been associated with physical disability.8 Therefore, it is important to assess longer-term effects on structural damage beyond 1 year of therapy.
The retention rate of patients receiving abatacept treatment was high, with 89% completing the 1-year double-blind portion of the AIM trial,5 and 90% of the patients entering the long-term extension completing year 2, suggesting the tolerability and durability of response to abatacept. Further, radiographic data were collected from a high percentage of patients, with 2-year data available from 87% of patients entering the open-label period, and observed data for 97% of patients; linear imputation based on baseline and early termination films was used in only 3% of patients.
Of note, an increased proportion of patients randomised to the placebo group withdrew from the double-blind portion of the study (between baseline and year 1) due to lack of efficacy (18% vs 3% in the abatacept group).5 Patients initially randomised to placebo who discontinued the study during the double-blind period are not included in these calculations. As these patients with worsening disease were not included in the assessment of radiographic outcomes, the progression of structural damage in patients initially randomised to placebo may be underestimated. As is standard for the assessment of radiographic outcome, readers were blinded to the sequence of radiographs, thus eliminating bias for the expectation of benefit.
Abatacept therapy resulted in inhibition of structural damage progression over time. After 2 years of treatment, a significant reduction in the progression of structural damage was observed in patients treated with abatacept for 2 years relative to placebo for 12 months plus abatacept for 12 months.8 Lower mean changes in total Genant-modified Sharp scores at both 12 months and year 2 were 1.07 vs 2.4 units, and 1.55 vs 3.17 units, respectively. Notably, abatacept had a clear benefit on both the erosion and JSN scores.
The treatment effect for abatacept relative to placebo was an approximately 50% reduction in mean progression of structural damage in the first year of the study. The rate of progression of structural damage when patients had received placebo treatment for 2 years can be estimated by linear extrapolation from the 12-month data of patients randomised to placebo. Patients in the placebo group progressed >2 units in year 1 and can be projected to progress 4–5 units over 2 years using linear extrapolation. Overall, patients receiving abatacept treatment for 2 years progressed approximately 1.5 units versus the expected progression of approximately 4.5 units if placebo treatment had been continued for the second year. Thus, the effect of abatacept treatment in the second year of treatment would hypothetically reduce radiographic progression by an estimated two-thirds when compared with patients with established disease receiving MTX alone.
Fewer abatacept-treated patients had progression of structural damage, and, overall, 50% of patients receiving abatacept did not have radiographic progression over 2 years. In addition, 79% of patients treated with abatacept with no progression at year 1 maintained no progression of structural damage at year 2, demonstrating a durable effect on radiographic outcomes with abatacept therapy. In addition, 45% of patients with some progression at year 1 had no progression in year 2. As the overwhelming number of patients entering the second year of treatment completed the year, we are not reporting on a selected group of responders.
The increasing effect of abatacept treatment on the progression of structural damage is consistent with other efficacy data; the proportion of patients with American College of Rheumatology (ACR) 50 and 70 responses were statistically significantly increased from 6 months to 12 months in this study.5 The ACR 20, 50 and 70 responses; improvement in physical function; and improvement in both the physical and mental components of the Short-Form-36 health-related quality of life scale in patients treated with abatacept for up to 3 years will be described in full in a future report.
It is difficult to compare results across clinical trials with other treatments that have described radiographic outcomes. Confounding factors include the treatment and disease history of each study population, differing rates of radiographic progression for the control group in each trial, and the use of different scoring systems for the measurement of radiographic damage. The current study assessed the efficacy of abatacept in patients with established RA and long duration of disease, whereas several trials of other biological therapies, such as those targeting tumour necrosis factor, involved patients with early RA (eg, the ERA trial of etanercept17 and the PREMIER trial of adalimumab18) or MTX-naive patients (the TEMPO trial of etanercept19). The Sharp-modified Sharp and the van der Heijde-modified Sharp scoring systems utilised in the trials of tumour necrosis factor-targeting agents,16 17 20 as well as the Genant-modified Sharp scoring system utilised here and in the interleukin-1 receptor antagonist and rituximab studies,18 21 all have differences in joints assessed, scales applied and maximum achievable scores. Thus, Sharp-, van der Heijde- and Genant-modified Sharp scores cannot be directly inter-converted, although they correlate moderately well cross-sectionally and longitudinally. In addition, the definition of the progression of structural damage varied among studies, including progression defined as change ⩾0 or the smallest detectable difference among readers.16–18 20 21 The Genant-modified scoring system employed in this study showed high inter-reader agreement (0.90–0.92 cross-sectionally and 0.82 for change) and high sensitivity to change (smallest detectable difference) for erosion (3.5), JSN (2.5) and total score (5.1).10
The inhibition of progression of structural damage with abatacept has clinical implications for the prevention of disability over time. The association of progression of structural damage and impaired physical function over the long term has been well correlated, and is strongest in established disease.7 8 Impacting the rate of joint destruction with continued abatacept treatment is likely to impede progressive functional disability, and thus may have increasing benefit for patients over time. Further study in this and other patient populations will assess the efficacy of abatacept therapy over longer periods of time.
Footnotes
Funding: This study was funded by Bristol-Myers Squibb.
Competing interests: HG has been reimbursed by Bristol-Myers Squibb, Amgen, Wyeth, Novartis, Merck, Sanofi-Aventis, Lilly, GSK, Roche and Genentech for speaking fees and honoraria. HG has also received research funding from these organisations. HG is a founder and share holder of Synarc, Inc., and serves as a member of the board of directors. RW has been reimbursed >$10 000 by Bristol-Myers Squibb and Schering-Plough for speaking fees and honoraria. J-CB is an employee of Bristol-Myers Squibb, and has shares with the company. RA is an employee of Bristol-Myers Squibb, and has shares with the company. GV is an employee of Bristol-Myers Squibb, and has shares with the company. JT is an employee of Bristol-Myers Squibb, and has shares with the company. JK has been reimbursed >$10 000 by Bristol-Myers Squibb for speaking fees and honoraria. CP is an employee and shareholder of Synarc, Inc., and is a provider of central image analysis, molecular marker assays and subject recruitment for global clinical trials for numerous pharmaceutical and biotechnology companies across a broad range of therapeutic areas.
REFERENCES
- 1.Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 2001;344:907–16 [DOI] [PubMed] [Google Scholar]
- 2.Goronzy JJ, Weyand CM. T-cell regulation in rheumatoid arthritis. Curr Opin Rheumatol 2004;16:212–17 [DOI] [PubMed] [Google Scholar]
- 3.Moreland LW, Alten R, Van den Bosch F, Appelboom T, Leon M, Emery P, et al. Costimulatory blockade in patients with rheumatoid arthritis: a pilot, dose-finding, double-blind, placebo-controlled clinical trial evaluating CTLA-4Ig and LEA29Y eighty-five days after the first infusion. Arthritis Rheum 2002;46:1470–9 [DOI] [PubMed] [Google Scholar]
- 4.Genovese MC, Becker JC, Schiff M, Luggen M, Sherrer Y, Kremer J, et al. Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 2005;353:1114–23 [DOI] [PubMed] [Google Scholar]
- 5.Kremer JM, Genant HK, Moreland LW, Russell AS, Emery P, Abud-Mendoza C, et al. Effects of abatacept in patients with methotrexate-resistant active rheumatoid arthritis: a randomized trial. Ann Intern Med 2006;144:865–76 [DOI] [PubMed] [Google Scholar]
- 6.Kremer JM, Westhovens R, Leon M, Di Giorgio E, Alten R, Steinfeld S, et al. Treatment of rheumatoid arthritis by selective inhibition of T-cell activation with fusion protein CTLA4Ig. N Engl J Med 2003;349:1907–15 [DOI] [PubMed] [Google Scholar]
- 7.Scott DL, Pugner K, Kaarela K, Doyle DV, Woolf A, Holmes J, Hieke K. The links between joint damage and disability in rheumatoid arthritis. Rheumatology (Oxford) 2000;39:122–32 [DOI] [PubMed] [Google Scholar]
- 8.Welsing PM, van Gestel AM, Swinkels HL, Kiemeney LA, van Riel PL. The relationship between disease activity, joint destruction, and functional capacity over the course of rheumatoid arthritis. Arthritis Rheum 2001;44:2009–17 [DOI] [PubMed] [Google Scholar]
- 9.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24 [DOI] [PubMed] [Google Scholar]
- 10.Peterfy C, Miaux Y, Wu C, Jiang Y, Sieffert M, Mokliatchouk O, et al. High inter-observer reproducibility of Genant-modified Sharp radiographic scoring of hands and feet of patients with rheumatoid arthritis in the AIM (Abatacept in Inadequate responders to Methotrexate). Ann Rheum Dis 2005;64Suppl III:460 [Google Scholar]
- 11.Genant HK. Methods of assessing radiographic change in rheumatoid arthritis. Am J Med 1983;75:35–47 [DOI] [PubMed] [Google Scholar]
- 12.Genant HK, Jiang Y, Peterfy C, Lu Y, Redei J, Countryman PJ. Assessment of rheumatoid arthritis using a modified scoring method on digitized and original radiographs. Arthritis Rheum 1998;41:1583–90 [DOI] [PubMed] [Google Scholar]
- 13.Lassere M, Boers M, van der Heijde D, Boonen A, Edmonds J, Saudan A, Verhoeven AC. Smallest detectable difference in radiological progression. J Rheumatol 1999;26:731–9 [PubMed] [Google Scholar]
- 14.Strand V, Landewe R, van der Heijde D. Using estimated yearly progression rates to compare radiographic data across recent randomised controlled trials in rheumatoid arthritis. Ann Rheum Dis 2002;61(Suppl 2):ii64–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharp JT, Wolfe F, Lassere M, Boers M, Van Der Heijde D, Larsen A, et al. Variability of precision in scoring radiographic abnormalities in rheumatoid arthritis by experienced readers. J Rheumatol 2004;31:1062–72 [PubMed] [Google Scholar]
- 16.St Clair EW, van der Heijde DM, Smolen JS, Maini RN, Bathon JM, Emery P, et al. Combination of infliximab and methotrexate therapy for early rheumatoid arthritis: a randomized, controlled trial. Arthritis Rheum 2004;50:3432–43 [DOI] [PubMed] [Google Scholar]
- 17.Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH, Keystone EC, et al. A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med 2000;343:1586–93 [DOI] [PubMed] [Google Scholar]
- 18.Breedveld FC, Weisman MH, Kavanaugh AF, Cohen SB, Pavelka K, van Vollenhoven R, et al. The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum 2006;54:26–37 [DOI] [PubMed] [Google Scholar]
- 19.Klareskog L, van der Heijde D, de Jager JP, Gough A, Kalden J, Malaise M, et al. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet 2004;363:675–81 [DOI] [PubMed] [Google Scholar]
- 20.Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC, et al. Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 2006;54:2793–806 [DOI] [PubMed] [Google Scholar]
- 21.Genant HK. Interleukin-1 receptor antagonist treatment of rheumatoid arthritis patients: radiologic progression and correlation of Genant/Sharp and Larsen scoring methods. Semin Arthritis Rheum 2001;30:26–32 [DOI] [PubMed] [Google Scholar]