Abstract
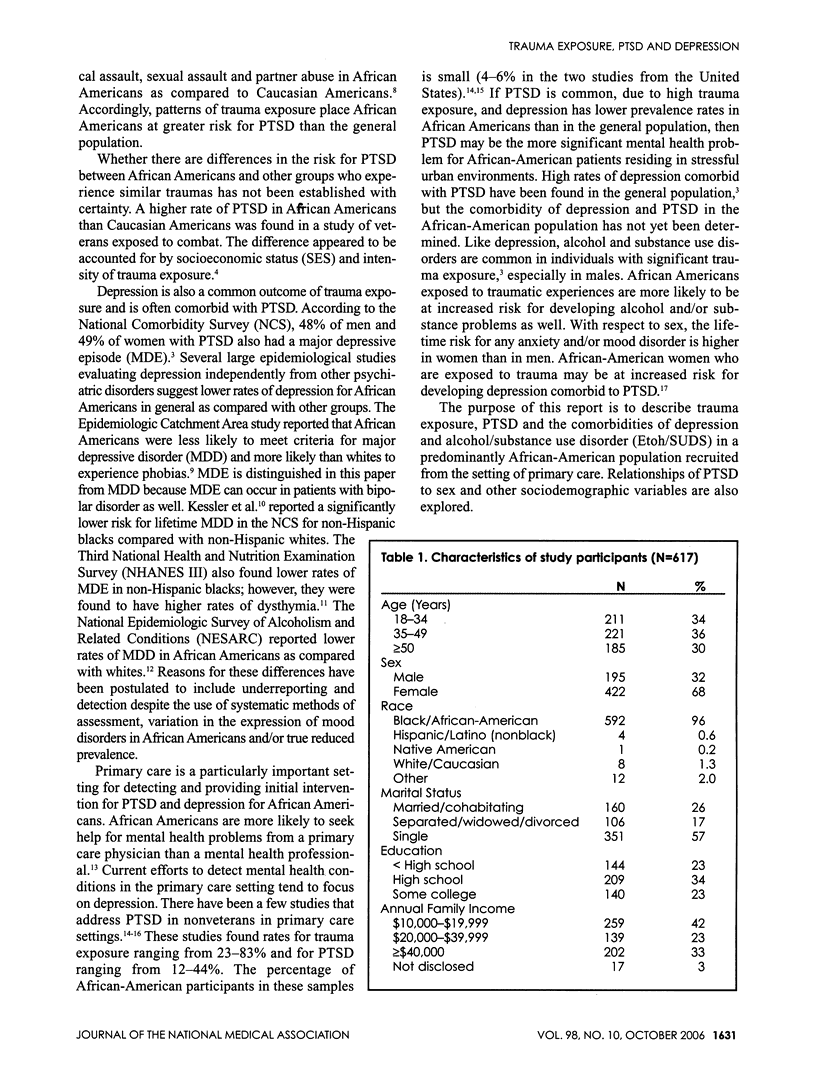
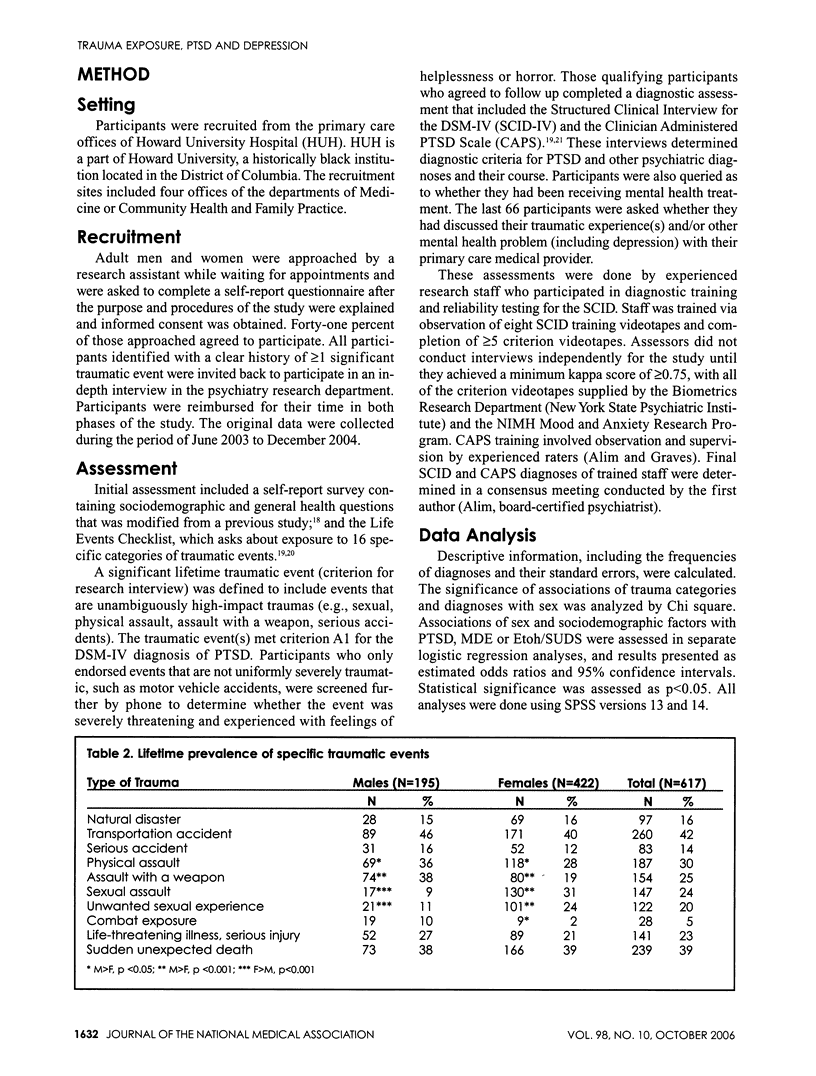
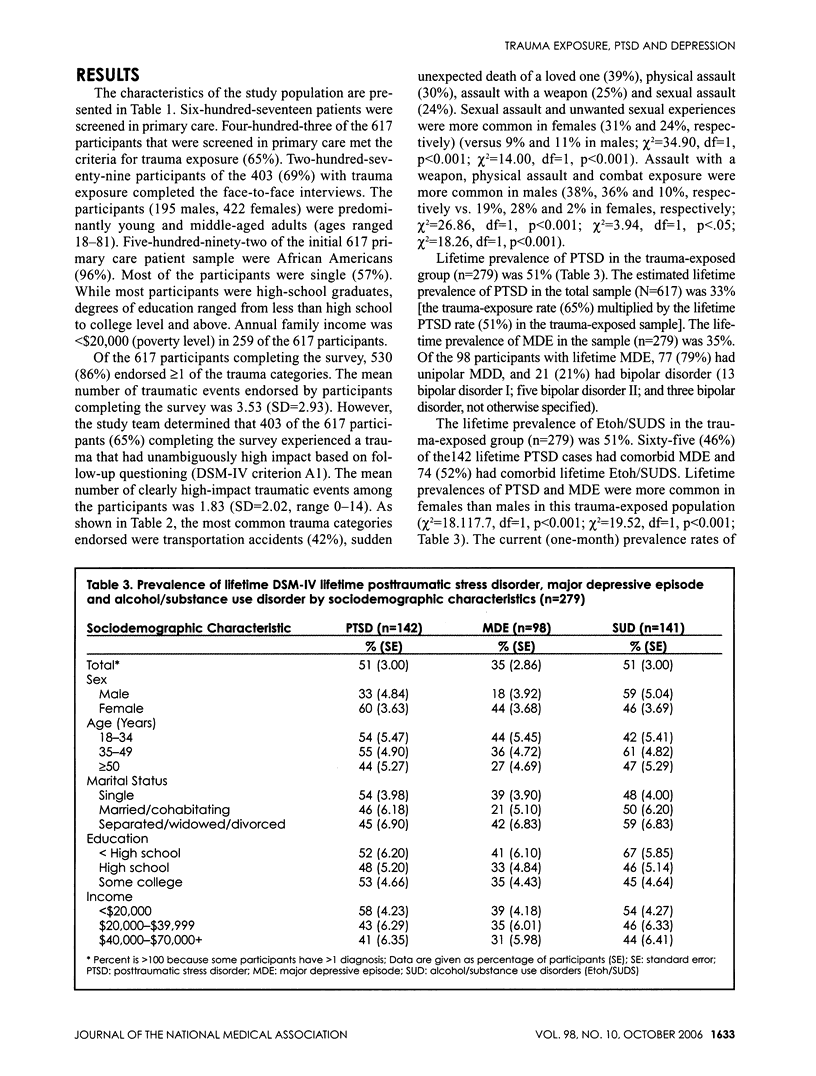
OBJECTIVE: Trauma exposure is high in African Americans who live in stressful urban environments. Posttraumatic stress disorder (PTSD) and depression are common outcomes of trauma exposure and are understudied in African Americans. African Americans are more likely to seek treatment for psychiatric disorders in a primary care setting. Our study evaluated trauma exposure, PTSD and major depression in African Americans attending primary care offices. METHOD: Six-hundred-seventeen patients (96% African Americans) were surveyed for trauma exposure in the waiting rooms of four primary care offices. Those patients reporting significant traumatic events were invited to a research interview. Of the 403 patients with trauma exposure, 279 participated. RESULTS: Of the 617 participants, 65% reported > or = 1 clearly traumatic event. The most common exposures were transportation accidents (42%), sudden unexpected death of a loved one (39%), physical assault (30%), assault with a weapon (29%) and sexual assault (25%). Lifetime prevalence of PTSD and a major depressive episode (MDE) among those with trauma exposure (n=279) was 51% and 35%, respectively. The percent of lifetime PTSD cases (n=142) with comorbid MDE was 46%. Lifetime PTSD and MDE in the trauma-exposed population were approximately twice as common in females than males, whereas current PTSD rates were similar. CONCLUSIONS: Our rate of PTSD (approximately 33% of those screened) exceeds estimates for the general population. Rates of MDE comorbid with PTSD were comparable to other studies. These findings suggest the importance of screening African Americans for PTSD, in addition to depression, in the primary care setting.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blumberg Samuel H. Crisis intervention program: an alternative to inpatient psychiatric treatment for children. Ment Health Serv Res. 2002 Mar;4(1):1–6. doi: 10.1023/a:1014071507949. [DOI] [PubMed] [Google Scholar]
- Breslau N., Kessler R. C., Chilcoat H. D., Schultz L. R., Davis G. C., Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998 Jul;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Das Amar K., Olfson Mark, Gameroff Marc J., Pilowsky Daniel J., Blanco Carlos, Feder Adriana, Gross Raz, Neria Yuval, Lantigua Rafael, Shea Steven. Screening for bipolar disorder in a primary care practice. JAMA. 2005 Feb 23;293(8):956–963. doi: 10.1001/jama.293.8.956. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K. M., Boldizar J. P. The prevalence and consequences of exposure to violence among African-American youth. J Am Acad Child Adolesc Psychiatry. 1993 Mar;32(2):424–430. doi: 10.1097/00004583-199303000-00026. [DOI] [PubMed] [Google Scholar]
- Friedman M. J. Posttraumatic stress disorder. J Clin Psychiatry. 1997;58 (Suppl 9):33–36. [PubMed] [Google Scholar]
- Gray Matt J., Litz Brett T., Hsu Julie L., Lombardo Thomas W. Psychometric properties of the life events checklist. Assessment. 2004 Dec;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Greenberg P. E., Sisitsky T., Kessler R. C., Finkelstein S. N., Berndt E. R., Davidson J. R., Ballenger J. C., Fyer A. J. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999 Jul;60(7):427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Hasin Deborah S., Goodwin Renee D., Stinson Frederick S., Grant Bridget F. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005 Oct;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Jonas Bruce S., Brody Debra, Roper Margaret, Narrow William E. Prevalence of mood disorders in a national sample of young American adults. Soc Psychiatry Psychiatr Epidemiol. 2003 Nov;38(11):618–624. doi: 10.1007/s00127-003-0682-8. [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61 (Suppl 5):4–14. [PubMed] [Google Scholar]
- Kessler R. C., Sonnega A., Bromet E., Hughes M., Nelson C. B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995 Dec;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., Berglund Patricia, Demler Olga, Jin Robert, Koretz Doreen, Merikangas Kathleen R., Rush A. John, Walters Ellen E., Wang Philip S., National Comorbidity Survey Replication The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003 Jun 18;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., Berglund Patricia, Demler Olga, Jin Robert, Merikangas Kathleen R., Walters Ellen E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Koss M. P., Woodruff W. J., Koss P. G. Relation of criminal victimization to health perceptions among women medical patients. J Consult Clin Psychol. 1990 Apr;58(2):147–152. doi: 10.1037//0022-006x.58.2.147. [DOI] [PubMed] [Google Scholar]
- McCauley J., Kern D. E., Kolodner K., Dill L., Schroeder A. F., DeChant H. K., Ryden J., Derogatis L. R., Bass E. B. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997 May 7;277(17):1362–1368. [PubMed] [Google Scholar]
- McGee Z. T., Davis B. L., Brisbane T., Collins N., Nuriddin T., Irving S., Mutakkabir Y., Martin K. Urban stress and mental health among African-American youth: assessing the link between exposure to violence, problem behavior, and coping strategies. J Cult Divers. 2001 Fall;8(3):94–104. [PubMed] [Google Scholar]
- Norris F. H. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol. 1992 Jun;60(3):409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Robins L. N., Helzer J. E., Weissman M. M., Orvaschel H., Gruenberg E., Burke J. D., Jr, Regier D. A. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry. 1984 Oct;41(10):949–958. doi: 10.1001/archpsyc.1984.01790210031005. [DOI] [PubMed] [Google Scholar]
- Selner-O'Hagan M. B., Kindlon D. J., Buka S. L., Raudenbush S. W., Earls F. J. Assessing exposure to violence in urban youth. J Child Psychol Psychiatry. 1998 Feb;39(2):215–224. [PubMed] [Google Scholar]
- Shakoor B. H., Chalmers D. Co-victimization of African-American children who witness violence: effects on cognitive, emotional, and behavioral development. J Natl Med Assoc. 1991 Mar;83(3):233–238. [PMC free article] [PubMed] [Google Scholar]
- Stein M. B., McQuaid J. R., Pedrelli P., Lenox R., McCahill M. E. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry. 2000 Jul-Aug;22(4):261–269. doi: 10.1016/s0163-8343(00)00080-3. [DOI] [PubMed] [Google Scholar]
- Taubman-Ben-Ari O., Rabinowitz J., Feldman D., Vaturi R. Post-traumatic stress disorder in primary-care settings: prevalence and physicians' detection. Psychol Med. 2001 Apr;31(3):555–560. doi: 10.1017/s0033291701003658. [DOI] [PubMed] [Google Scholar]
- Vogel L. C., Marshall L. L. PTSD symptoms and partner abuse: low income women at risk. J Trauma Stress. 2001 Jul;14(3):569–584. doi: 10.1023/A:1011116824613. [DOI] [PubMed] [Google Scholar]


