Abstract
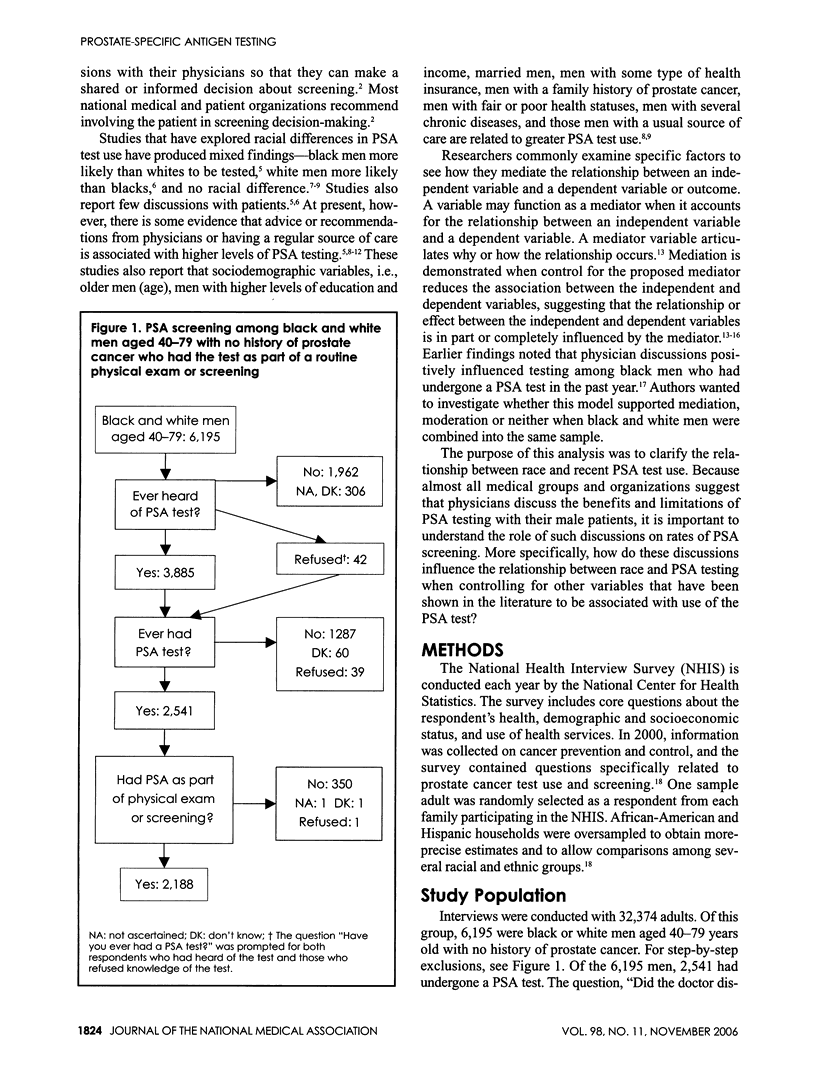
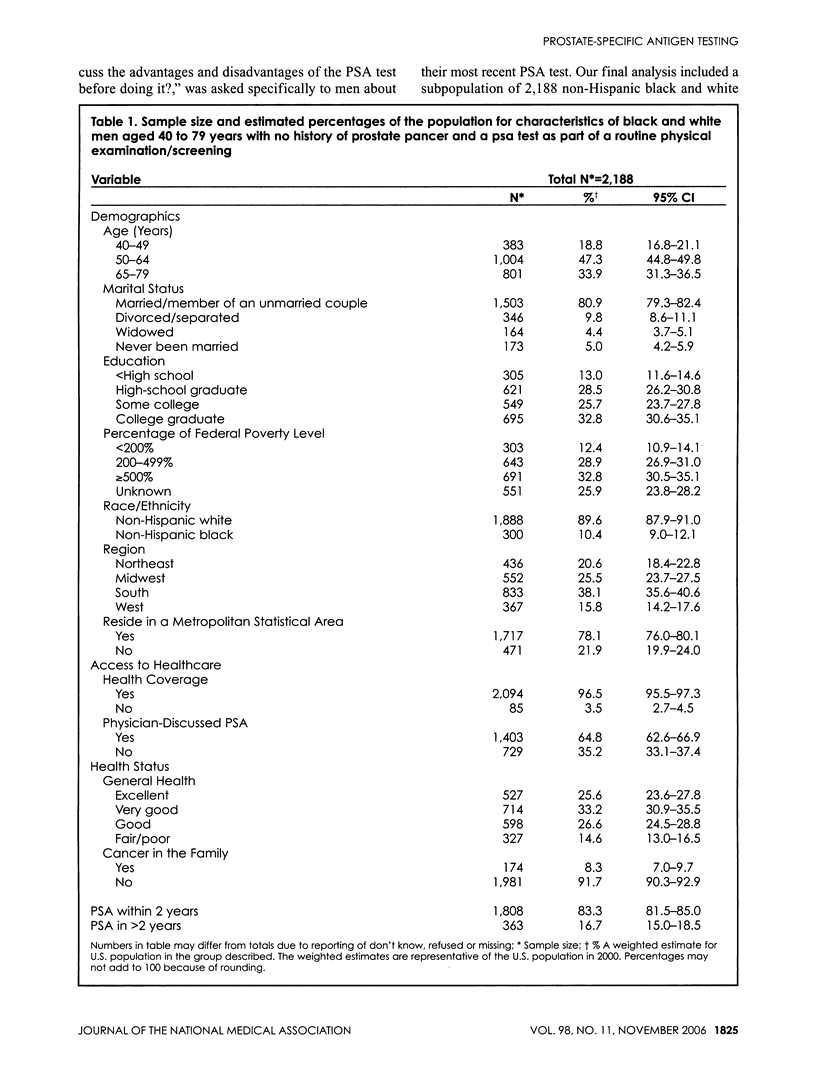
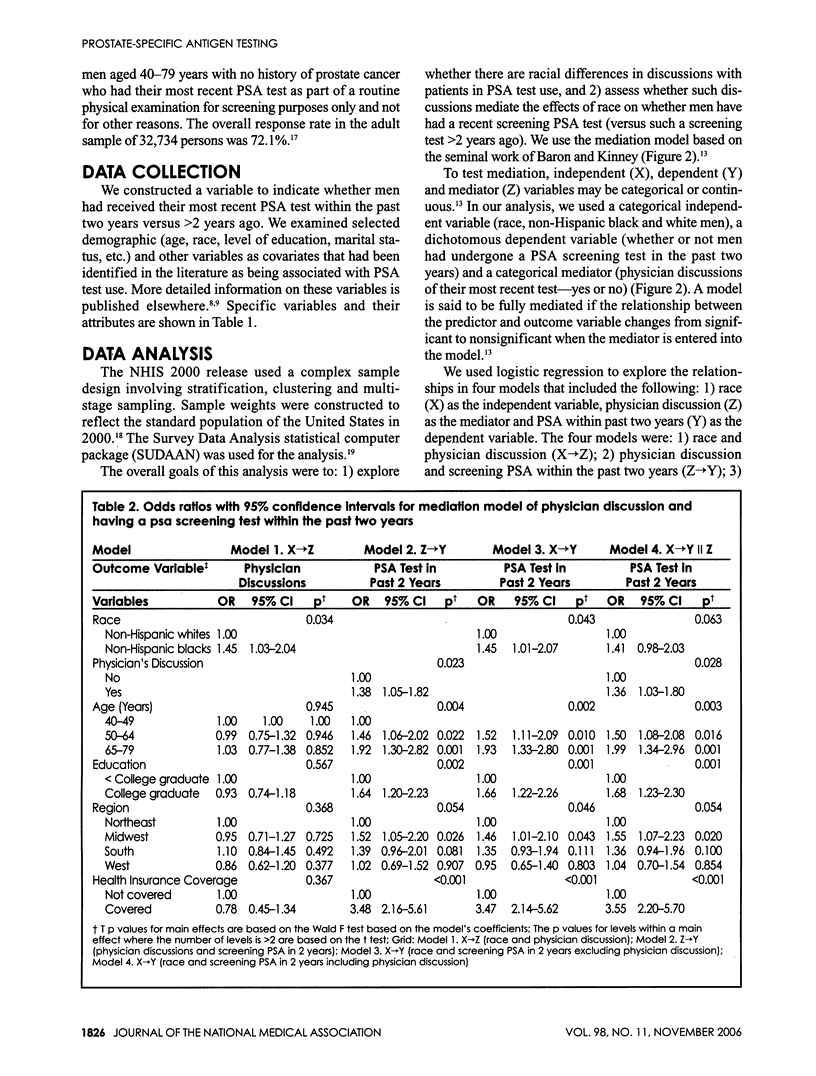
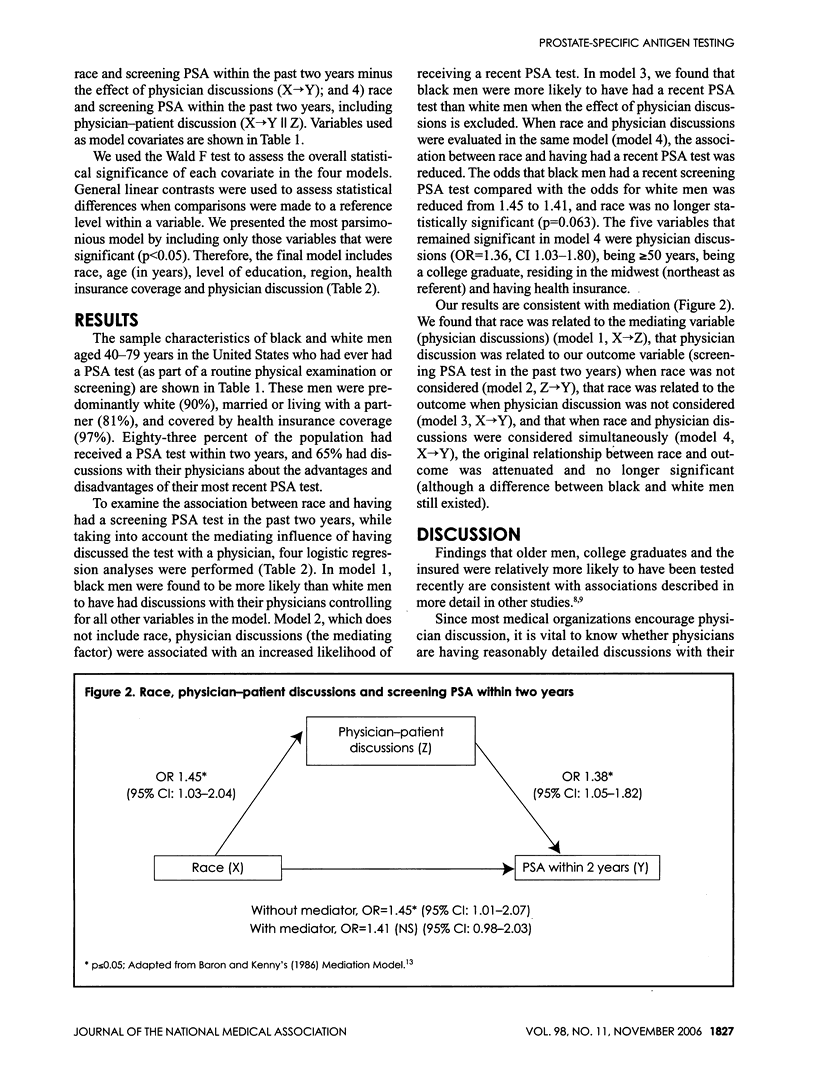
Many medical and professional organizations agree that men should discuss the advantages and disadvantages of testing for prostate-specific antigen (PSA) with their physicians before undergoing testing. In the 2000 National Health Interview Survey, men who had undergone a PSA test in the past were asked about their use of this test and discussions they had with physicians regarding its advantages and disadvantages. Among a group of 2,188 black and white men aged 40-79 years with no history of prostate cancer and a history of testing for PSA, we examined whether physician-patient discussions mediated the relationship between race and PSA testing. We specified that the test had to be their most recent one and part of a routine physical examination or screening test. We compared those tested within the past two years with those tested >2 years. Almost two-thirds of the men previously had discussions with their physicians about the advantages and disadvantages of the PSA test. Older men, college graduates, those living in the midwest and those with health insurance were more likely to have been tested recently. Discussion with a physician was found to mediate the relationship between race and PSA testing during the past two years. Black men were initially found to be more likely than white men to have been screened recently [odds ratio (OR)=1.45; 95% confidence interval (CI) 1.01-2.07], but in the full model race was no longer significant (OR=1.41; 95% Cl 0.98-2.03). Discussions about PSA testing were associated with more recent PSA screening (OR=1.38, 95% CI 1.05-1.82). These findings suggest that: 1) the relationships among race, physician discussions and PSA testing may need to be examined in more complex ways, and 2) the physician has an important role in men's decision to consider PSA testing.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arredondo Elva M., Pollak Kathryn I., Costanzo Philip, McNeilly Maya, Myers Evan. Primary care residents' characteristics and motives for providing differential medical treatment of cervical cancer screening. J Natl Med Assoc. 2003 Jul;95(7):576–584. [PMC free article] [PubMed] [Google Scholar]
- Baron R. M., Kenny D. A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986 Dec;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Carter F., Graham E., Pal N., Gonzalez E., Roetzheim R. Prostate cancer screening in primary care. South Med J. 1999 Mar;92(3):300–304. doi: 10.1097/00007611-199903000-00008. [DOI] [PubMed] [Google Scholar]
- Chan Evelyn C. Y., Vernon Sally W., Ahn Chul, Greisinger Anthony. Do men know that they have had a prostate-specific antigen test? Accuracy of self-reports of testing at 2 sites. Am J Public Health. 2004 Aug;94(8):1336–1338. doi: 10.2105/ajph.94.8.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demark-Wahnefried W., Strigo T., Catoe K., Conaway M., Brunetti M., Rimer B. K., Robertson C. N. Knowledge, beliefs, and prior screening behavior among blacks and whites reporting for prostate cancer screening. Urology. 1995 Sep;46(3):346–351. doi: 10.1016/S0090-4295(99)80218-0. [DOI] [PubMed] [Google Scholar]
- Dunn A. S., Shridharani K. V., Lou W., Bernstein J., Horowitz C. R. Physician-patient discussions of controversial cancer screening tests. Am J Prev Med. 2001 Feb;20(2):130–134. doi: 10.1016/s0749-3797(00)00288-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen S. A., Waterman B., Skinner C. S., Scherrer J. F., Romeis J. C., Bucholz K., Heath A., Goldberg J., Lyons M. J., Tsuang M. T. Sociodemographic and health status characteristics with prostate cancer screening in a national cohort of middle-aged male veterans. Urology. 1999 Mar;53(3):516–522. doi: 10.1016/s0090-4295(98)00545-7. [DOI] [PubMed] [Google Scholar]
- Finney Rutten Lila J., Meissner Helen I., Breen Nancy, Vernon Sally W., Rimer Barbara K. Factors associated with men's use of prostate-specific antigen screening: evidence from Health Information National Trends Survey. Prev Med. 2005 Apr;40(4):461–468. doi: 10.1016/j.ypmed.2004.07.011. [DOI] [PubMed] [Google Scholar]
- Gordon N. P., Hiatt R. A., Lampert D. I. Concordance of self-reported data and medical record audit for six cancer screening procedures. J Natl Cancer Inst. 1993 Apr 7;85(7):566–570. doi: 10.1093/jnci/85.7.566. [DOI] [PubMed] [Google Scholar]
- Jacobsen Paul B., Lamonde Laurie A., Honour Melissa, Kash Kathryn, Hudson Perry B., Pow-Sang Julio. Relation of family history of prostate cancer to perceived vulnerability and screening behavior. Psychooncology. 2004 Feb;13(2):80–85. doi: 10.1002/pon.760. [DOI] [PubMed] [Google Scholar]
- Jordan T. R., Price J. H., King K. A., Masyk T., Bedell A. W. The validity of male patients' self-reports regarding prostate cancer screening. Prev Med. 1999 Mar;28(3):297–303. doi: 10.1006/pmed.1998.0430. [DOI] [PubMed] [Google Scholar]
- Northouse L. L., Caffey M., Deichelbohrer L., Schmidt L., Guziatek-Trojniak L., West S., Kershaw T., Mood D. The quality of life of African American women with breast cancer. Res Nurs Health. 1999 Dec;22(6):449–460. doi: 10.1002/1098-240x(199912)22:6<449::aid-nur3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- Purvis Cooper Crystale, Merritt Tracie L., Ross Louie E., John Lisa V., Jorgensen Cynthia M. To screen or not to screen, when clinical guidelines disagree: primary care physicians' use of the PSA test. Prev Med. 2004 Feb;38(2):182–191. doi: 10.1016/j.ypmed.2003.09.035. [DOI] [PubMed] [Google Scholar]
- Ross Louie E., Coates Ralph J., Breen Nancy, Uhler Robert J., Potosky Arnold L., Blackman Donald. Prostate-specific antigen test use reported in the 2000 National Health Interview Survey. Prev Med. 2004 Jun;38(6):732–744. doi: 10.1016/j.ypmed.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Stark N., Paskett E., Demark-Wahnefried W., Carbone E., Godley P. Prostate cancer as a public health issue in North Carolina. N C Med J. 2001 Sep-Oct;62(5):286–290. [PubMed] [Google Scholar]
- Steele C. B., Miller D. S., Maylahn C., Uhler R. J., Baker C. T. Knowledge, attitudes, and screening practices among older men regarding prostate cancer. Am J Public Health. 2000 Oct;90(10):1595–1600. doi: 10.2105/ajph.90.10.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan Judith, Breen Nancy, Coates Ralph J., Rimer Barbara K., Lee Nancy C. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003 Mar 15;97(6):1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force Screening for prostate cancer: recommendation and rationale. Ann Intern Med. 2002 Dec 3;137(11):915–916. doi: 10.7326/0003-4819-137-11-200212030-00013. [DOI] [PubMed] [Google Scholar]
- Volk Robert J., Cass Alvah R. The accuracy of primary care patients' self-reports of prostate-specific antigen testing. Am J Prev Med. 2002 Jan;22(1):56–58. doi: 10.1016/s0749-3797(01)00397-x. [DOI] [PubMed] [Google Scholar]


