Abstract
Background
Extent of left ventricular dysfunction in patients with acute myocardial infarction (AMI) is an important predictor of subsequent morbidity and mortality. It is unclear, however, how often ejection fraction (EF) findings are evaluated in the setting of AMI, and the characteristics of patients who do not have their EF evaluated, particularly from the more generalizable perspective of a population-based investigation.
Purpose
The purpose of this study was to examine nearly 3 decade long trends (1975-2003) in the evaluation of EF in patients admitted with confirmed AMI (n=12,760) to all greater Worcester (MA) hospitals during 14 annual periods.
Results
The percentage of patients undergoing evaluation of EF prior to hospital discharge increased substantially between 1975 (4%) and 2003 (73%). Despite these encouraging trends, approximately one quarter of patients in our most recent study year did not receive an EF evaluation. In the mid-1970's through mid-1980's, radionuclide ventriculography was typically used to assess EF whereas echocardiography was most often used to evaluate EF during more recent periods. Predictors of not undergoing an evaluation of their cardiac function included older age, shorter length of hospital stay, code status limitations, dying during hospitalization, Medicare insurance, several comorbidities, and a recent non-Q-wave MI.
Conclusions
The results of this community-wide study suggest that a considerable proportion of patients with AMI fail to have their EF evaluated. Efforts remain needed to optimize the use of cardiac imaging studies and link the results of these studies to improved patient outcomes.
Introduction
The manner by which physicians evaluate and treat patients with acute myocardial infarction (AMI) has evolved considerably over the past 30 years leading to significant reductions in AMI associated morbidity and mortality1,2. The use of cardiac testing to determine which patients with AMI are at increased risk for adverse outcomes is important in determining who should receive more aggressive management or increased monitoring efforts. Determination of left ventricular ejection fraction (EF) findings in the setting of AMI has been shown to be a powerful predictor of prognosis3-9. Patients with left ventricular dysfunction after AMI have been shown to benefit from more aggressive pharmacological management, coronary revascularization, and defibrillator implantation to prevent sudden cardiac death10,11. Current guidelines published by the American College of Cardiology (ACC) and American Heart Association (AHA) list the evaluation of EF after AMI as a class I indication7-9. Determination of EF findings after AMI is also an indirect performance measure by the ACC, AHA, and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) since angiotensin converting enzyme inhibitors should be prescribed for persons with left ventricular dysfunction12,13. Limited data are available, however, particularly from the more generalizable perspective of a population-based investigation, describing current trends in the evaluation of EF in the setting of AMI and the characteristics of patients in whom EF is not determined.
Using data from a population-based registry of patients from a large New England metropolitan area with acute coronary disease2,14, we examined changing trends in the evaluation of EF among patients hospitalized with AMI over a nearly 3 decade-long period (1975-2003). A secondary goal of this community-wide study was to examine the characteristics of patients who did not undergo an evaluation of their EF during hospitalization for AMI.
Methods
Study population
The Worcester Heart Attack Study is an ongoing population-based investigation that is examining changes over time in the hospital incidence and case-fatality rates of AMI in residents of the Worcester (MA) metropolitan area (2000 census estimate = 478,000). Details of this study have been published previously2,14. In brief, the medical records of greater Worcester residents hospitalized with discharge diagnoses consistent with the possible presence of AMI at all metropolitan Worcester medical centers were individually reviewed and validated according to predefined diagnostic criteria that have been previously described2,14. Demographic and clinical data were abstracted from hospital medical records by trained nurse and physician reviewers. Information about the use of diagnostic procedures during hospitalization was obtained through the review of hospital medical records and physician's and nurse's progress notes2,14. Information was unfortunately not collected about prior EF findings in the study population. Data have been collected in our ongoing study on an approximate biennial basis for purposes of examining changing trends in the principal study outcomes on an alternate yearly basis. The 14 years under study consisted of 1975, 1978, 1981, 1984, 1986, 1988, 1990, 1991, 1993, 1995, 1997, 1999, 2001, and 2003.
Data analysis
Differences in the characteristics of greater Worcester residents hospitalized with AMI with and without a determination of EF during their acute hospitalization were examined through the use of chi-square tests of statistical significance for discrete variables and t-tests for continuous variables. A multivariable logistic regression analysis was used to examine demographic and clinical factors associated with the failure to have patient's EF measured during hospitalization for AMI. Multivariable adjusted odds ratios (OR) and accompanying 95% confidence intervals (CI's) were calculated in a standard manner.
Results
Study Sample Characteristics
The study population consisted of 12,760 patients who experienced a documented AMI over the 14 individual study years between 1975 and 2003. The average age of the study sample was 69 years, 59% were men, and a considerable proportion of the study population had a history of prior MI (35%), diabetes (28%), and/or stroke (10%).
Changing Trends in the Evaluation of EF During Hospitalization for AMI
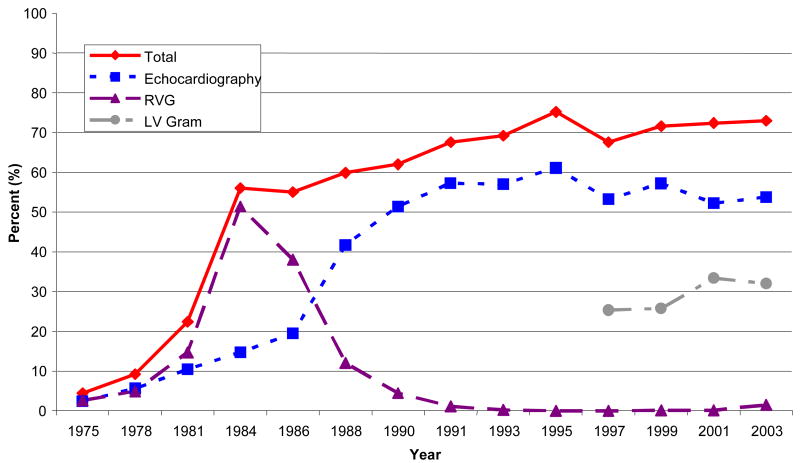
The proportion of patients undergoing an EF determination prior to hospital discharge, and the various studies used to determine EF findings over time, are shown in Figure 1. In 1975, only 4.4% of patients with confirmed AMI underwent an EF evaluation prior to hospital discharge. Over time, we observed a significant increase in the percentage of patients hospitalized with AMI who had an evaluation of their EF performed prior to hospital discharge (Figure 1). Despite these encouraging trends, in the most recent year under study (2003) slightly more than one quarter (27%) of patients with confirmed AMI failed to receive an EF evaluation prior to hospital discharge. The proportion of metropolitan Worcester residents undergoing an EF determination has not changed appreciably since the early 1990's (Figure 1). Virtually identical trends in the measurement of left ventricular function were observed when either all deaths, or early hospital deaths (e.g., within first 48 hours), were excluded. For example, after excluding all early hospital deaths in the study sample, 4.6% of patients with confirmed AMI underwent an EF evaluation prior to hospital discharge in 1975 with this percentage increasing to 74.3% in 2003.
Figure 1.
Trends in the Evaluation of Ejection Fraction Over Time
A relatively large percentage of our total study sample underwent multiple evaluations of their cardiac function during hospital admission. Overall, 27.0% of patients underwent any 2 cardiac imaging tests and 0.8% (n=103) underwent all 3 tests (e.g., echocardiography, RVG, cardiac catheterization) during their acute hospital admission. The use of multiple (≥2) cardiac tests to determine cardiac function was relatively similarly observed in patients with (25.7%) and without (29.8%) an uncomplicated AMI (development of heart failure, shock, or atrial fibrillation during hospitalization).
In terms of changing trends in the use of multiple cardiac tests to determine a patient's EF (Figure 2), <1% of all study patients underwent both echocardiography and cardiac catheterization in 1975/78 whereas 45.5% of patients underwent both of these testing procedures in 2001/03. In examining changing trends in the use of echocardiography and radionuclide studies, <1% of study patients underwent both of these procedures during 1975/78; no patients underwent both of these procedures after 1995 (Figure 2). Essentially similar trends were observed when these analyses were restricted to patients with an uncomplicated AMI.
Changing Trends in the Type of Studies Used to Evaluate EF
The types of studies used to evaluate EF have evolved considerably over time (Figure 1). Radionuclide ventriculography (RVG) was the most common method utilized to assess extent of left ventricular dysfunction during the mid to late-1970's. The frequency of RVG use peaked in the mid-1980's, however, and declined sharply thereafter. In contrast, the use of echocardiography increased markedly after the early 1980's (Figure 1). Between 1990 and 2003, the majority of patients admitted with AMI who had an EF determination underwent an echocardiogram. Data regarding the use of left ventricular angiography to estimate EF has been recorded in this study population only since 1997. The percentage of patients having an EF estimation by left ventriculography increased between 1999 and 2001 (26% to 33%) and remained stable in 2003. Extremely few patients with AMI underwent a gated-SPECT myocardial perfusion imaging study to estimate their EF.
Characteristics of Patients Not Undergoing Evaluation of Ventricular Function
In comparison to those receiving an evaluation of their cardiac function, patients not having an evaluation of their left ventricular EF were more likely to be older, women, have a do not resuscitate code status, have Medicare insurance, have had a prior history of angina, heart failure, chronic pulmonary disease, or AMI, and to have developed a Q-wave MI during their index hospitalization (Table 1). Patients not undergoing an EF evaluation were more likely to have died during hospitalization despite a decreased likelihood of developing atrial fibrillation or heart failure during hospitalization. The average hospital stay was 9.7 days for patients who underwent an evaluation of EF during their hospitalization compared to 10.5 days for those who did not undergo a determination of their EF. Patients not undergoing an evaluation of their EF were less likely to have been prescribed effective cardiac medications, and to have undergone invasive cardiac procedures, in comparison to patients who had their EF assessed.
Table 1.
Characteristics of Patients Hospitalized with Acute Myocardial Infarction (AMI) According to Measurement of Ejection Fraction (EF)
| Characteristic | % of study sample with characteristic | % with EF not measured (n=5,595) | P-value | % with EF not measured in 2001/2003 (n=655) | P-value | ||
|---|---|---|---|---|---|---|---|
| % | n | % | n | % | |||
| Age (yrs) | |||||||
| < 55 | 16.1 | 2,049 | 41.3 | <.001 | 340 | 17.9 | <.001 |
| 55-64 | 19.9 | 2,532 | 43.1 | 395 | 22.5 | ||
| 65-74 | 26.5 | 3,372 | 42.1 | 508 | 25.0 | ||
| 75-84 | 25.5 | 3,239 | 43.4 | 704 | 28.1 | ||
| ≥ 85 | 12.0 | 1,532 | 53.0 | 449 | 40.1 | ||
| Sex | |||||||
| Men | 58.8 | 7,510 | 43.0 | <0.01 | 1,347 | 25.2 | <0.01 |
| Women | 41.1 | 5,250 | 45.1 | 1,049 | 30.0 | ||
| DNR/DNI code status | |||||||
| Present (+) * | 21.4 | 1,474 | 44.0 | <0.001 | 581 | 40.4 | <0.01 |
| Absent (-) | 78.6 | 5,397 | 24.0 | 1,679 | 22.2 | ||
| Insurance Status | |||||||
| Private | 4.1 | 384 | 29.2 | 31 | 16.1 | ||
| Medicare | 50.5 | 4,688 | 34.2 | <0.001 | 889 | 29.9 | 0.08 |
| Medicaid | 2.9 | 264 | 29.2 | 70 | 17.1 | ||
| HMO | 27.6 | 2,565 | 28.6 | 1,103 | 26.8 | ||
| Medical history | |||||||
| Angina | |||||||
| Present (+) | 25.6 | 3,271 | 47.2 | <0.001 | 537 | 33.9 | <0.001 |
| Absent (-) | 74.4 | 9,487 | 42.7 | 1,859 | 25.4 | ||
| Diabetes | |||||||
| Present (+) | 27.6 | 3,515 | 41.8 | <0.01 | 785 | 30.1 | <0.05 |
| Absent (-) | 72.4 | 9,243 | 44.6 | 1,611 | 26.0 | ||
| Heart failure | |||||||
| Present (+) | 18.4 | 2,351 | 50.7 | <0.001 | 575 | 42.1 | <0.001 |
| Absent (-) | 81.6 | 10,407 | 42.3 | 1,821 | 22.7 | ||
| Hypertension | |||||||
| Present (+) | 56.2 | 7,175 | 40.3 | 1,697 | 29.2 | <0.01 | |
| Absent (-) | 43.8 | 5,583 | 48.4 | <0.001 | 699 | 22.9 | |
| Stroke | |||||||
| Present (+) | 9.6 | 1,224 | 42.0 | 292 | 30.1 | 0.25 | |
| Absent (-) | 90.4 | 11,534 | 44.0 | 0.17 | 2,104 | 26.9 | |
| COPD ∞ | |||||||
| Present (+) | 17.4 | 779 | 31.6 | <0.05 | 460 | 30.6 | 0.08 |
| Absent (-) | 82.6 | 3,701 | 28.2 | 1,936 | 26.6 | ||
| AMI Characteristics (%) | |||||||
| Initial | 65.1 | 8,308 | 41.6 | <0.001 | 1,553 | 22.8 | <0.001 |
| Prior | 34.9 | 4,452 | 48.1 | 843 | 35.7 | ||
| Q wave | 42.3 | 5,403 | 46.1 | <0.001 | 493 | 15.6 | <0.001 |
| Non Q wave | 57.7 | 7,357 | 42.2 | 1,903 | 30.4 | ||
| Clinical Complications (%) | |||||||
| Atrial fibrillation | |||||||
| Present (+) | 16.8 | 2,140 | 38.5 | <0.001 | 517 | 24.2 | 0.07 |
| Absent (-) | 83.2 | 10,620 | 44.9 | 1,879 | 28.2 | ||
| Cardiogenic shock | |||||||
| Present (+) | 6.7 | 855 | 46.8 | 0.07 | 123 | 16.3 | <0.01 |
| Absent (-) | 93.3 | 11,905 | 43.6 | 2,273 | 27.9 | ||
| Heart failure | |||||||
| Present (+) | 39.7 | 5,059 | 40.4 | <0.001 | 941 | 25.7 | 0.15 |
| Absent (-) | 60.4 | 7,701 | 46.1 | 1,455 | 28.4 | ||
| Death | |||||||
| Present (+) | 85.4 | 1,861 | 66.5 | 248 | 45.6 | <0.001 | |
| Absent (-) | 14.6 | 10,899 | 40.0 | <0.001 | 2,148 | 25.2 | |
| Medications | |||||||
| ACE inhibitors† | |||||||
| Administered (+) | 44.4 | 3,048 | 21.1 | <0.001 | 1,517 | 20.2 | <0.001 |
| Not Administered (-) | 55.6 | 4,450 | 36.8 | 879 | 39.6 | ||
| Aspirin | |||||||
| Administered (+) | 62.7 | 8,003 | 30.6 | <0.001 | 2,158 | 25.4 | <0.001 |
| Not Administered (-) | 37.3 | 4,757 | 66.1 | 238 | 45.4 | ||
| Beta blockers | |||||||
| Administered (+) | 59.6 | 7,600 | 30.8 | <0.001 | 2,097 | 24.9 | <0.001 |
| Not Administered (-) | 40.4 | 5,160 | 63.0 | 299 | 44.8 | ||
| Thrombolytics† | |||||||
| Administered (+) | 17.5 | 1,650 | 23.0 | <0.001 | 169 | 20.1 | <0.05 |
| Not Administered (-) | 82.5 | 7,768 | 33.6 | 2,223 | 27.9 | ||
| Procedures | |||||||
| Cardiac catheterization | |||||||
| Present (+) | 28.6 | 3,645 | 14.5 | <0.001 | 1,268 | 14.0 | <0.001 |
| Absent (-) | 71.4 | 9,105 | 55.6 | 1,128 | 42.4 | ||
| Percutaneous coronary intervention† | |||||||
| Present (+) | 17.0 | 1,596 | 19.4 | <0.001 | 849 | 17.9 | <0.001 |
| Absent (-) | 83.0 | 7,813 | 34.4 | 1,547 | 32.5 | ||
| Coronary artery bypass surgery | |||||||
| Present (+) | 3.5 | 442 | 7.7 | <0.001 | 167 | 2.4 | <0.001 |
| Absent (-) | 96.5 | 12,302 | 45.2 | 2,229 | 29.2 | ||
data on code status collected since 1991
data on the use of ACE inhibitors collected since 1990
data collected since 1986
data collected since 1997
A logistic regression analysis utilizing all baseline demographic and clinical characteristics was carried out for purposes of examining factors significantly associated with the failure to undergo an evaluation of left ventricular dysfunction prior to hospital discharge in our study sample (Table 2). Patients not undergoing evaluation of their EF were significantly more likely to be 85 years or older, to have a history of angina, heart failure, or MI, and to have been admitted to greater Worcester hospitals with a non-Q wave infarction. These patients were more likely to have died during hospitalization, despite a decreased likelihood of developing the hospital complications of heart failure, cardiogenic shock, or atrial fibrillation. These patients were also less likely to have been prescribed effective cardiac medications and to have undergone cardiac catheterization or coronary artery bypass grafting in comparison to patients who had their EF assessed.
Table 2.
Factors Significantly Associated With Not Having Ejection Fraction Evaluated in Patients Hospitalized With Acute Myocardial Infarction (AMI)
| Total Study Sample | Patients Hospitalized in 2001/2003 | |||
|---|---|---|---|---|
| Characteristic | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Age (years) | ||||
| 55-64 | 0.86 | 0.84,0.87 | 0.98 | 0.65,1.47 |
| 65-74 | 0.85 | 0.74,0.98 | 1.03 | 0.69,1.53 |
| 75-84 | 0.78 | 0.68,0.90 | 0.88 | 0.71,1.67 |
| ≥85 | 1.32 | 1.11,1.57 | 1.09 | 0.71,1.67 |
| Medical History | ||||
| Angina (+) | 1.19 | 1.07,1.31 | 1.39 | 1.09,1.77 |
| Heart failure (+) | 1.52 | 1.35,1.71 | 1.94 | 1.50,2.51 |
| AMI Characteristics | ||||
| Prior | 1.24 | 1.13,1.37 | 1.51 | 1.21,1.88 |
| Non Q wave | 1.34 | 1.22,1.47 | 1.48 | 1.09,2.00 |
| Clinical Complications | ||||
| Heart failure (-) | 2.28 | 2.08,2.51 | 1.92 | 1.51,2.44 |
| Shock (-) | 1.31 | 1.08,1.57 | 2.35 | 1.30,4.28 |
| Atrial fibrillation (-) | 1.43 | 1.27,1.61 | 1.31 | 1.01,1.70 |
| Death | 2.74 | 2.39,3.14 | 1.85 | 1.30,2.65 |
| Medications | ||||
| ACE-inhibitors** (-) | -- | -- | 2.01 | 1.62,2.50 |
| Aspirin (-) | 1.36 | 1.22,1.51 | 1.14 | 0.82,1.58 |
| Beta blockers (-) | 1.45 | 1.31,1.60 | 1.34 | 0.99,1.82 |
| Thrombolytics** (-) | -- | -- | 1.03 | 0.66,1.60 |
| Procedures | ||||
| Cardiac catheterization (-) | 3.56 | 3.16,4.01 | 5.10 | 3.51,7.39 |
| Percutaneous coronary intervention** | -- | -- | 2.10 | 1.42,3.09 |
| CABG (-) | 2.22 | 1.51,3.27 | 5.81 | 2.06,16.41 |
respective referent categories: age <55 years, absence of selected comorbidities, initial, Q wave MI, presence of selected clinical complications, prescribed effective cardiac medications and/or coronary revascularization procedures
Data not available over entire study period
In order to provide contemporary insights into the profile of patients with AMI not undergoing an evaluation of their cardiac function, we carried out a similar analysis of factors associated with not undergoing an EF evaluation in patients hospitalized with AMI during our 2 most recent study years (Table 2). The results of this analysis showed that relatively similar factors were associated with the nonevaluation of EF in patients hospitalized with AMI during 2001 and 2003.
Finally, since patients who died during hospitalization were at increased risk for not having their cardiac function evaluated, we carried out an additional analysis in which patients who died during hospitalization were excluded. The results of this analysis, controlling for similar demographic and clinical factors as well as length of hospital stay, showed that relatively similar factors were associated with the nonevaluation of EF in our total study sample, as well as in patients hospitalized with AMI in our 2 most recent study periods (Table 3).
Table 3.
Factors Significantly Associated With Not Having Ejection Fraction Evaluated in Patients Hospitalized With Acute Myocardial Infarction (AMI)
| Total Study Sample | Patients Hospitalized in 2001/2003 | |||
|---|---|---|---|---|
| Characteristic | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Age (years) | ||||
| 55-64 | 0.85 | 0.73,0.99 | 0.84 | 0.63,1.12 |
| 65-74 | 0.79 | 0.68,0.91 | 0.90 | 0.68,1.18 |
| 75-84 | 0.86 | 0.74,1.01 | 0.79 | 0.60,1.05 |
| ≥85 | 1.37 | 1.13,1.66 | 0.94 | 0.67,1.30 |
| DNR status** | -- | ---- | 1.35 | 1.08,1.70 |
| Medical History | ||||
| Angina (+) | 1.22 | 1.10,1.36 | 1.31 | 1.09,1.58 |
| Heart failure (+) | 1.52 | 1.33,1.74 | 2.05 | 1.66,2.53 |
| Diabetes (+) | 1.05 | 0.95,1.17 | 1.21 | 1.02,1.45 |
| AMI Characteristics | ||||
| Prior | 1.26 | 1.14,1.40 | 1,48 | 1.25,1.76 |
| Non Q wave | 1.41 | 1.27,1.55 | 1.53 | 1.23,1.90 |
| Clinical Complications | ||||
| Heart failure (-) | 2.24 | 2.02,2.49 | 1.97 | 1.61,2.39 |
| Atrial fibrillation (-) | 1.34 | 1.17,1.53 | 1.34 | 1.06,1.69 |
| Medications | ||||
| ACE-inhibitors** (-) | -- | --,-- | 1.94 | 1.65,2.29 |
| Aspirin (-) | 1.32 | 1.17,1.49 | 1.24 | 0.92,1.67 |
| Beta blockers (-) | 1.39 | 1.25,1.55 | 1.32 | 1.05,1.68 |
| Procedures | ||||
| Cardiac catheterization (-) | 3.41 | 3.01,3.86 | 5.40 | 4.09,7.12 |
| Percutaneous coronary intervention** | -- | --,-- | 2.91 | 2.17,3.91 |
| CABG (-) | 2.05 | 1.37,3.08 | 1.90 | 1.05,3.44 |
respective referent categories: age <55 years, DNR status (-), absence of selected comorbidities, initial, Q wave MI, presence of selected clinical complications, prescribed effective cardiac medications and/or coronary revascularization procedures
Data not available over entire study period
Discussion
The results of this observational study in residents of a large and representative New England community demonstrate a significant increase in the proportion of patients who underwent a determination of their cardiac functional status prior to hospital discharge for AMI during the past nearly 3 decades. Evolution in the type of studies used to evaluate left ventricular dysfunction was noted, with echocardiography becoming the predominant technique for the evaluation of EF during recent study years. Patients were also more likely to undergo multiple diagnostic tests to determine their cardiac function during recent as compared to more distant study years. Despite improving trends in the determination of EF in patients hospitalized with AMI, slightly more than one quarter of greater Worcester residents with AMI in 2003 failed to have an EF evaluation prior to hospital discharge. A number of demographic and clinical factors were associated with the failure to undergo an EF examination.
Changing Trends in the Evaluation of EF in Patients Hospitalized With AMI
We observed a considerable increase in the proportion of patients with AMI who underwent evaluation of their left ventricular function during the period under study. While this trend is encouraging since EF is a powerful predictor of hospital and long-term prognosis, our study showed that the percentage of patients having an estimation of EF prior to hospital discharge for AMI appears to have reached a plateau since the late 1990's; more importantly, in the most recent study year (2003), a considerable proportion of patients failed to receive an evaluation of EF despite strong recommendations from published guidelines7-9.
Our findings are consistent with the published literature with regards to the evaluation of cardiac function in patients hospitalized with AMI. Data from the National Registry of Myocardial Infarction (NRMI) show that between 1994 and 2002, approximately one-third of patients with AMI did not receive an evaluation of their EF prior to hospital discharge15,16. During the most recent study period (2000-2002) of this large observational study, approximately one-quarter of patients did not have their EF determined15. In the VALIANT study registry, nearly 1 out of every 6 patients hospitalized with AMI without heart failure over the period 1999 to 2001 did not undergo an EF evaluation prior to hospital discharge17. Among patients with AMI complicated by heart failure, an even greater percentage did not undergo evaluation of their EF. In a study of Olmsted County (MN) residents hospitalized with AMI between 1979 and 1998, the proportion of patients receiving a determination of their EF increased over time; however, during the most recent decade (1988-1998) of this observational study, approximately 1 in 5 patients did not receive an EF evaluation within 10 days of their index MI18. An even smaller percentage of patients underwent an evaluation of their EF prior to hospital discharge.
The results of our study also provides insights into the changing, and contemporary, use of multiple cardiac imaging tests to diagnose left ventricular dysfunction in patients with AMI. Our findings suggest that there may be an overuse of the assessment of left ventricular dysfunction in patients hospitalized with AMI, including those who had an uncomplicated hospital course. These practice trends warrant further monitoring given the costs and resources devoted to these diagnostic imaging studies and the additional extent, type, and quality of information that might be obtained by the use of multiple cardiac imaging studies.
Diagnostic Modalities Used to Evaluate EF in Patients With AMI
We observed an evolution in the type of tests used to assess left ventricular dysfunction during hospitalization for AMI. While RVG was the primary method used to assess EF during the 1970's, the development of two-dimensional echocardiography in the 1970's, and publication of studies validating its use in the early 1980's19, has led to the expanded use of this imaging modality as the primary means to assess EF19. Expanded use of two-dimensional echocardiography is not surprising since echocardiography provides detailed information about cardiac function and anatomy, does not require exposure to ionizing radiation, is portable, and offers the immediate reporting of clinically relevant information.
Ejection fraction findings can also be obtained with technetium and thallium-based gated nuclear imaging studies. Data regarding the use of nuclear perfusion imaging studies have been collected in our population-based investigation since 1995; however, data regarding the use of gated images to determine EF has not been collected. In 2003, only 2.2% of patients underwent a nuclear imaging study prior to hospital discharge, primarily to assess for residual ischemia in the infarct related territory and for the detection of ischemia in other coronary vascular areas.
In 1990, the first ACC/AHA guidelines for the management of patients with AMI were published7. Echocardiography was given a class 1 recommendation for use in patients with large infarcts and evidence of clinical complications; a class IIB recommendation was given for patients with a moderate infarct without clinical complications7. Subsequent iterations of these guidelines for the care of patients with AMI have recommended the use of echocardiography in all patients not undergoing left ventriculography8,9.
Despite these recommendations, the proportion of greater Worcester residents hospitalized with AMI undergoing an evaluation of their EF prior to hospital discharge appears to have reached a plateau since the early 1990's. This may be explained in part by the clinical and demographic factors associated with not undergoing an EF determination. Advanced age and code status limitations may have been associated with a desire to not undergo extensive cardiac testing, which is also supported by our data showing a reduced likelihood of undergoing cardiac catheterization and coronary artery bypass surgery in individuals not undergoing a determination of their EF. Individuals not undergoing an EF evaluation had a shorter duration of hospitalization as compared to patients who had their EF evaluated and the assessment of cardiac function may have been postponed until the time of subsequent outpatient follow-up. Patients without an assessment of their cardiac function were also more likely to have a history of heart failure and prior MI and may have had a recent evaluation of their EF, although reevaluation of left ventricular function in the setting of a new AMI would seem prudent.
While patients who did not have their cardiac function assessed were less likely to be treated with effective treatment regimens then patients who had their EF findings determined, appropriate caveats need to be associated with the interpretation of these data. With the notable exception of the use of ACE inhibitors/ARB's, the decision to use virtually all other effective cardiac medications by clinicians in the management of patients with AMI is made independently of patient's EF findings. Many patients who do not undergo an assessment of their cardiac function may be managed with less intensive medical and revascularization strategies with different treatment goals.
Previous studies have demonstrated similar factors associated with not obtaining an EF after AMI15-18. Our investigation extends these findings by studying a large patient population and offering a relatively contemporary perspective into factors associated with the failure to have EF determined.
Study strengths and limitations
The strengths of this study include its multi-hospital population-based perspective and inclusion of patients from a large well characterized New England metropolitan area hospitalized with independently validated AMI.
There are several potential limitations of this study, however. Since the present study only evaluated tests performed in the inpatient setting, we could not account for individuals undergoing EF determination soon after hospital discharge. Due to reimbursement and other cost incentives, physicians in the greater Worcester area may have performed a considerable number of echocardiographic or nuclear diagnostic studies outside of the acute hospital setting, which may have affected some of the trends observed. In some patients in whom an echocardiogram was attempted, imaging limitations (e.g., inability to alter position of patient, presence of chronic lung disease) may have limited the ability to determine EF. The fact that patients without an evaluation of their EF were more likely to have a history of heart failure and MI suggests that these patients may have had a previous evaluation of their left ventricular function, though our data collection process could not determine the timing of this evaluation. Since indications for the use of diagnostic tests after AMI may be different, we cannot comment on the indications for test use and how tests results were utilized.
Conclusions
The results of this large population-based observational study show improving trends in the evaluation of EF prior to hospital discharge among patients hospitalized with AMI. Echocardiography has become the predominant technique utilized to assess left ventricular function. Future research should be conducted to confirm our findings and to determine why differences in the characteristics of patients undergoing, as compared to those not undergoing, an evaluation of their EF exist. Efforts to increase the proportion of patients having an EF determination prior to hospital discharge for AMI are warranted as well as studies that link the results of cardiac imaging assessments to improved patient outcomes. It is axiomatic, however, that not all patients clearly need an assessment of their EF after hospitalization for AMI as the ideal target rate of left ventricular EF determination is unknown.
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area and through funding support provided by the National Institutes of Health (RO1 HL35434).
References
- 1.National Institutes of Health; National heart, Lung, and Blood Institute. Morbidity and Mortality: 2004 Chartbook on Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: National Institutes of Health; 2004. [Google Scholar]
- 2.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, Dalen JE. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 3.Schulze RA, Jr, Rouleau J, Rigo P, Bowers S, Strauss HW, Pitt B. Ventricular arrhythmias in the late hospital phase of acute myocardial infarction: relation to left ventricular function detected by gated cardiac blood pool scanning. Circulation. 1975;52:1006–1011. doi: 10.1161/01.cir.52.6.1006. [DOI] [PubMed] [Google Scholar]
- 4.Schulze RA, Jr, Strauss HW, Pitt B. Sudden death in the year following myocardial infarction: relation to ventricular premature contractions in the late hospital phase and left ventricular ejection fraction. Am J Med. 1977;62:192–199. doi: 10.1016/0002-9343(77)90314-x. [DOI] [PubMed] [Google Scholar]
- 5.The Multicenter Postinfarction Research Group. Risk stratification and survival after myocardial infarction. N Engl J Med. 1983;309:331–336. doi: 10.1056/NEJM198308113090602. [DOI] [PubMed] [Google Scholar]
- 6.Penco M, Sciomer S, Vizza MD, Dagianti A, Vitarelli A, Romano S, Dagianti A. Clinical impact of echocardiography in prognostic stratification after acute myocardial infarction. Am J Cardiol. 1998;81:17G–20G. doi: 10.1016/s0002-9149(98)00048-4. [DOI] [PubMed] [Google Scholar]
- 7.The American College of Cardiology/American Heart Association Task Force. Guidelines for the early management of patients with acute myocardial infarction. J Am Coll Cardiol. 1990;16:249–287. doi: 10.1016/0735-1097(90)90575-a. [DOI] [PubMed] [Google Scholar]
- 8.The American College of Cardiology/ American Heart Association Task Force. ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2004;44:E1–E212. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 9.The American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. ACC/AHA Guidelines for the Clinical Application of Echocardiography. Circulation. 1997;95:1686–1744. doi: 10.1161/01.cir.95.6.1686. [DOI] [PubMed] [Google Scholar]
- 10.Moss AJ, Wojciech Z, Jackson Hall W, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 11.Pfeffer MA, Braunwald E, Moyle LA, et al. Effect of Captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The Save Investigators. N Engl J Med. 1992;327:669–677. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- 12.JCAHO. Specifications Manual for National Hospital Quality Measures Version 1.03. 2006 Available at http://www.jointcommission.org.
- 13.Krumholz HM, et al. ACC/AHA Clinical Performance Measures for Adults With ST-Elevation and Non–ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2006;47:236–265. doi: 10.1016/j.jacc.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975-1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 15.Vaccarino V, Rathore S, Wenger N, Frederick P, Abramson J, Barron H, Manhapra A, Mallik S, Krumholz H. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barron HV, Michaels AD, Maynard C, Every NR. Use of angiotensin-converting enzyme inhibitors at discharge in patients with acute myocardial infarction in the United States: data from the National Registry of Myocardial Infarction 2. J Am Coll Cardiol. 1998;32:360–367. doi: 10.1016/s0735-1097(98)00225-3. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez AF, Velazquez EJ, Solomon SD, Kilaru R, Diaz R, O'Connor CM, Ertl G, Maggioni AP, Rouleau JP, van Gilst W, Pfeffer MA, Califf RM. Left ventricular assessment in myocardial infarction. The VALIANT Registry. Ann Intern Med. 2005;165:2162–2169. doi: 10.1001/archinte.165.18.2162. [DOI] [PubMed] [Google Scholar]
- 18.Lopez-Jimenez F, Goraya TY, Hellerman JP, Jacobsen SJ, Reeder GS, Weston SA, Roger VL. Measurement of ejection fraction after myocardial infarction in the population. Chest. 2004;125:397–403. doi: 10.1378/chest.125.2.397. [DOI] [PubMed] [Google Scholar]
- 19.Crawford M. How reliable are echocardiographic studies in the diagnosis of myocardial dysfunction? Cardiovasc Clin. 1983;13:51–63. [PubMed] [Google Scholar]