SYNOPSIS
To properly prepare for and respond to bioterrorism and other urgent public health threats and emergencies, response disciplines must work together in well coordinated efforts to address the preparedness needs of their communities and the nation. Traditional public health workforce and first responder roles have been challenged and new partnerships have emerged, increasing the need for innovative education and training. This article provides a review of an approach the Heartland Center for Public Health Preparedness took to foster these partnerships and increase the provision of competency-based, integrated responder education and training in the St. Louis, MO, metropolitan area.
The role of public health in emergency preparedness and response has expanded in the recent past. After the attacks of September 11, 2001, communities were mandated to improve their level of workforce preparedness and the role of public health was thrust into the forefront of emergency response. In the past, traditional first responders functioned in relative isolation from other community responders in training events for natural or man-made disasters. At the same time, the public health workforce continued to experience serious shortages, receive inadequate training, and work in relative isolation without systemic integration with other community responders.1 To properly prepare for and respond to bioterrorism and other urgent public health threats and emergencies, public health and traditional first responders must work together in well coordinated efforts to address the needs of their communities and the nation.
The 2002 Institute of Medicine (IOM) report, Who Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century, defines a public health professional as “a person educated in public health or a related discipline who is employed to improve health through a population focus.”2 The definition of public health workforce has come to include traditional first responders, such as law enforcement and fire protection services, in addition to local and state public health employees. Each discipline is employed to improve the health of the population and serve as part of the integrated community response required to adequately protect the communities they serve. The public health missions to monitor health status, identify health problems, protect the population, and investigate public health threats are consistent with the missions of public safety and first responder agencies. Public health and public safety share the same broad goals of protecting the community's health and safety, but apply different yet related skill sets to accomplish their congruent missions. The IOM report explains that the pubic health work setting must include other disciplines. Therefore, preparing the community for a disaster must encompass public health as well as public safety sectors.
The Heartland Center for Public Health Preparedness, one of 23 Centers for Public Health Preparedness (CPHP) funded by the Centers for Disease Control and Prevention (CDC) and the Association of Schools of Public Health (ASPH), has made strides in cultivating partnerships with a diverse array of responder counterparts. To accomplish the Heartland Center's mission, it was necessary to expand state and local level partnerships, as well as to broaden the definition of public health workforce to include partners from the public, private, and non-profit sectors. However, the disconnected nature of response disciplines posed a challenge. As documented in the Roadmap for Public Health Workforce Preparedness, preparedness and response efforts were layered over an existing but uncoordinated approach to addressing the education and training needs of the workforce.3 By strengthening local partnerships, the Heartland Center improved access to educational services for the multidisciplinary response workforce and developed an integrated approach to coordinate the preparedness effort.
Several projects developed in collaboration with the St. Louis Metropolitan Medical Response System (SLMMRS) illustrate the Heartland Center's approach to broadening partnerships and utilizing an integrated workforce development system. SLMMRS brings together response agencies including fire, police, health departments, hospitals, the Federal Bureau of Investigation (FBI), and branches of armed services from the bi-state metropolitan area into a platform to manage day-to-day emergencies and mass casualty coordination. A joint Heartland Center and SLMMRS project—an educational program called Bioterrorism and Forensic Epidemiology: Mutual Training for Law Enforcement and Public Health Officials on Investigative Responses—provides a best-practice example of an integrated partnership program.
PARTNERSHIP BACKGROUND
In 1999, the St. Louis City and County governments received a contract from the U.S. Department of Health and Human Services to develop an all-hazard disaster response plan for the St. Louis metropolitan area, which covers 12 counties, two states, and approximately 2.6 million people. SLMMRS was created as a result of this contract. According to the CDC's Bioterrorism and Public Health Emergency Preparedness and Response collaborative training plan, readiness at the community level has two components: a preparedness plan that meets predetermined criteria and a workforce that can demonstrate an understanding of preparedness, their local plan as well as their agency's role, and individual responsibilities under the plan.4 To adequately fulfill the SLMMRS and CDC mandate, a diverse group of responders came together in a partnership for emergency response and preparedness planning. SLMMRS partners include the Heartland Center for Public Health Preparedness, regional fire and Emergency Medical Services (EMS), local health departments, regional police departments, the St. Louis Division of the FBI, the Institute for Bio-Security (IBS), emergency management agencies, hospital emergency staff, medical examiners, and key military personnel.
As SLMMRS began to meet and discuss the possibility of a terrorist attack in the metropolitan area, the strengths and weaknesses of the response workforce emerged. It became clear that information sharing and possible resource sharing among hospitals, medical systems, and EMS would be necessary to adequately respond to a major event. SLMMRS coordinated this effort through the development of MEDCOMM (Medical Communications) and has developed an emergency patient tracking system (EPTS) that uses barcoded bracelets scanned by Personal Digital Assistants (PDAs) to record the severity of injuries, clinical information, and arrival time at hospital. SLMMRS also monitors regional hospitals and medical systems for need and availability of hospital beds and pertinent equipment through the EMSystem and Hospital Emergency Administrative Radio (HEAR) communication systems. SLMMRS' partnerships created during this effort increased the levels of preparedness and resource availability in the metropolitan area, thus resulting in one of the largest hospital system mutual aid agreements in the nation.
The hospital system mutual aid agreement has increased SLMMRS' capacity to manage the consequences of a disaster with mass causalities. As the Heartland Center became more involved with SLMMRS and the hospital system mutual aid agreement, the need for a public health agency mutual aid agreement emerged. Subsequently, SLMMRS and the Heartland Center drafted an agreement providing the first mechanism by which local public health agencies can share critical medical supplies and manpower across jurisdictional lines. The public health mutual aid agreement and the hospital mutual aid agreement provide a means for disconnected disciplines to open the lines of communication and share response roles. This agreement allowed public health to become a full participant in the SLMMRS board of directors, as well as validated their role in the emergency response effort. Although the agreement is currently in the formalization process, the addition of public health to the response team has increased collaboration and led to the development of integrated educational programs.
EDUCATIONAL PROGRAM
In spring 2003, representatives from the Eastern Missouri U.S. Attorney's Office attended a CDC conference describing a new program on investigative responses to bioterrorism for law enforcement and public health officials. Entitled “Bioterrorism and Forensic Epidemiology,” the training program's main goal was to strengthen public health/law enforcement partnerships, focusing on joint investigation, sharing of information, and evidence collection. The U.S. Attorney decided to develop this program for the St. Louis metropolitan area. SLMMRS served as the catalyst to bring the partners together to plan the innovative program, which was designed to improve integration between public health and first responders. SLMMRS and the U.S. Attorney brought together six key partners to help develop and deliver this breakthrough program: the St. Louis County Department of Health, St. Louis City Health Department, St. Louis FBI, the Heartland Center for Public Health Preparedness, the Institute for Bio-Security, and the St. Louis Metropolitan Police Department. The planning partners intended the program to reach across disciplines and mirror the diverse membership of the planning committee.
Program planning
Using information and suggestions from the CDC conference, the planning committee developed an innovative, competency-based program to reach the many disciplines responsible for emergency response and investigation. The committee's intention was to create a multi-part program that would highlight key positions and responsibilities. They referred to the CDC training plan, which describes the key target audiences for emergency response efforts as public health and health care professionals, emergency responders, law enforcement, and the business community.4 Program marketing was targeted to these audiences in the St. Louis metropolitan area. The committee decided to employ the knowledge of local leaders in the fields of epidemiology and law enforcement to explain similarities and differences between the two professions. They also planned to provide forensics, terrorism, and public health law content outlined in the CDC training plan.4 In addition, they planned for mixed-discipline groups to meet at the conclusion of each day to discuss their response roles, with case studies to guide their discussions. The committee realized the need to create a facilitative capacity for the case study discussions when expected attendance reached more than 300. A train-the-trainer approach was developed to identify facilitators and improve their competence.
Train-the-trainer approach.
The planning committee held a Bioterrorism and Forensic Epidemiology train-the-trainer program in August 2003. Approximately 75 public health and law enforcement professionals participated. The trainers were educated on the program background, as well as their role as case study facilitator. The trainers received two lectures on the similarities and differences between public health and law enforcement and were encouraged to provide feedback. Experiential techniques were utilized in the explanation of the case study scenarios. The participants were then asked to volunteer to facilitate the case study process during the region-wide conference scheduled for December 2003. Volunteer facilitators attended the expanded region-wide training as participants during the scheduled lectures, then facilitated the case-study discussions.
Didactic lectures.
Using the CDC training plan, the planning committee decided on a curriculum of didactic lectures focusing on core learning objectives such as criminal and epidemiological investigative methods, operations and procedures, and shared communication. These components were structured to provide competency-based learning in the key subject areas outlined in the CDC training plan: law enforcement for public health officials, public health matters for law enforcement, regional issues on agro-terrorism, weapons of mass destruction (WMD), federal incident command response, public health law, and Health Insurance Portability and Accountability Act (HIPAA) law overview.4
Regional conference
The Bioterrorism and Forensic Epidemiology: Mutual Training for Law Enforcement and Public Health Officials on Investigative Responses conference was held December 2–3, 2003, at the America's Center in St. Louis, MO. More than 350 representatives of public health, law enforcement, hospital staff, firefighters, EMS, and emergency management agencies attended. The workforce audience was divided into two groups defined by their response roles. The first group defined themselves as traditional public health workforce and attended a lecture on criminal investigative methods. The second group defined themselves as emergency or first responders and attended a lecture on epidemiological investigative methods. The groups reconvened to attend other competency-based lectures and case studies.
Case study breakout sessions were a key element of the two-day program. Two case studies—one focused on a smallpox response and another on an unknown substance investigation—were led by two volunteer facilitators (one from law enforcement and one from public health). During the breakout sessions, participants discussed actual emergency events and explored lessons learned.5 Through case study activities, participants learned how to perform emergency notification, how to determine whether the incident is a credible threat, how to collaborate and share information, and how to establish a unified command structure among public health, law enforcement, and other emergency response agencies.
One of the most important outcomes of the program was the introduction of key emergency response personnel across disciplines. Many people involved in the training had never met, yet would potentially be working together in an emergency situation. This type of personal introduction and networking results in efficient incident command systems during a disaster, possibly saving time, money, and most importantly, lives. The case studies resulted in a growth of partnerships and an expansion of the participants' understanding of the public health workforce definition to include traditional first responders.
EVALUATION
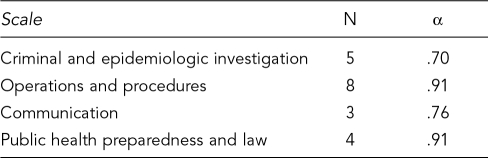
Because of the importance and innovative nature of the program, the Heartland Center completed a competency-based evaluation using 20 competency/skill items to evaluate the participants' perceived ability pre- and post-training. The items corresponded to four scales: Criminal and Epidemiological Investigations Methods (five items); Operations and Procedures (eight items); Communications (three items); and Public Health Preparedness and Public Health Law (four items). Participants rated their personal ability to complete each of the competencies on a scale from 1 to 4, with 1 signifying “I have no ability to perform this skill” and 4 signifying “I have complete ability to perform this skill.” Reliability analysis revealed acceptable alpha coefficients for each scale (Table 1).
Table 1. Internal consistency reliability coefficients for scales (Cronbach's Alpha).
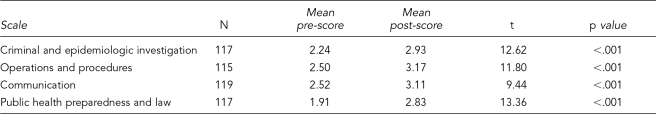
Summary scores were computed for each scale. The mean score was higher for the post measurement on each scale (Table 2). Paired t-tests comparing pre- and post-scale scores revealed a statistically significant improvement for each scale (Table 2).
Table 2. Pre- and post-training scores.
CONCLUSION
The partnership between SLMMRS and the Heartland Center for Public Health Preparedness has demonstrated leadership and innovation by bringing key emergency response partners together into new working partnerships to achieve common training objectives. The Bioterrorism and Forensic Epidemiology program is one example of this. The large number of responders who participated in the program demonstrates great interest and need for emergency response training. The program itself, although not unique, provided an individualized experience wherein law enforcement, public health, hospital staff, and public and private agencies came together to discuss emergency response and perceived roles. As people were introduced and peers interacted, response roles and responsibilities were described, understood, and respected. The innovation of the Bioterrorism and Forensic Epidemiology program and the SLMMRS partnership is exemplified in the personal connection and understanding of fellow response partners during an emergency.
Although the evaluation design suffers from the validity problems inherent in the group pre/post test design, program evaluation results do suggest that the format and content of the training can produce significant increases in perceived ability. The positive evaluations and the additional requests exemplify the success and need of these partnerships. Because of this success, the rate of workforce change is potentially high with real impact in day-to-day working partnerships among hospitals, law enforcement, and public health. There is a realization in the emergency response workforce that working partnerships are critical to developing new strategies of deterring, detecting, containing, and preventing terrorist events. Many important resources will respond and organize at the local level, utilizing first responders and public health. These important local assets will not only be deployed to the emergency, but will also assume key command responsibilities in coordinating the response. It is critical that the responders know their fellow response agencies and understand how they can work collaboratively to keep the public healthy and safe.
Acknowledgments
The authors would like to thank H. Richard Smith, Director of Operations for the St. Louis Metropolitan Medical Response System, and Matthew T. Drake, Assistant U.S. Attorney, Office of the U.S. Attorney, Eastern District of Missouri, for their ongoing leadership and partnership as described in this article. The authors would also like to thank Carolyn Soke, Graduate Assistant for the Heartland Center for Public Health Preparedness, for her help in preparation of this article.
REFERENCES
- 1.Turnock BJ, Hutchison KD. The local public health workforce: size, distribution, and composition of influence on core function performance, Illinois 1998-1999. Chicago: Illinois Center for Health Workforce Studies; 2000. [Google Scholar]
- 2.Institute of Medicine. Who will keep the public healthy? Educating public health professionals for the 21st century. Washington: National Academies Press; 2002. [PubMed] [Google Scholar]
- 3.Turnock BJ. Roadmap for public health workforce preparedness. J Public Health Manag Pract. 2003;9:471–80. doi: 10.1097/00124784-200311000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (US) Bioterrorism and public health emergency preparedness and response: a national collaborative plan. Center for Disease Control and Prevention; 2002. [Google Scholar]
- 5.Columbia University School of Nursing. Defining Emergency Exercises: A working guide to the terminology used in practicing emergency response in communities and public health agencies. Center for Health Policy; 2004. [Google Scholar]