SYNOPSIS
The Nevada State Health Division developed a local academic-practice partnership with the University of Nevada Reno's Master of Public Health Program to assess the bioterrorism risk communication, information, response, and training needs of professional and public stakeholder groups throughout Nevada. Between October 16, 2002, and April 13, 2004, 22 needs assessment focus groups and 125 key informant interviews were conducted to gather information on the diverse needs of the stakeholders. The themes that emerged from these activities included the need for effective pre-event education and training; a coordinated and responsive public health preparedness infrastructure; honest, accurate, and timely communication in the event of a bioterrorism situation; and appropriate information dissemination methods and technology. The data collected through this needs assessment gave the Nevada State Health Division vital information to plan public health preparedness initiatives. The establishment of local academic-practice partnerships for states without a Centers for Disease Control and Prevention-funded Academic Center for Public Health Preparedness is an effective way for health departments to develop their public health preparedness infrastructure while simultaneously training the future public health workforce.
The continual threat of biological terrorism has focused national attention on the public health emergency planning and response capabilities of state and local health departments. Immediately following the anthrax attacks in 2001, the Centers for Disease Control and Prevention (CDC) awarded an unprecedented level of funding to state and local health departments through cooperative agreements to address planning; surveillance and epidemiology; laboratory capacity; communications and information technology; risk communication and public information dissemination; and education and training.1
The public health preparedness funding directed toward local and state health departments complements a separate CDC initiative that established a national network of 23 Academic Centers for Public Health Preparedness (ACPHP) located in schools of public health.2 This network represents a collaboration between the CDC, the Association of Schools of Public Health (ASPH), and state and county health departments. According to the CDC, the “academic centers link schools of public health with state, local, and regional health departments to support bioterrorism preparedness and address public health infrastructure needs.”2 The primary objective of the ACPHP network is the development, implementation, and evaluation of competency-based trainings for the local public health workforce.3 The ACPHP have also been charged with working closely with state and local health departments to conduct public health preparedness activities funded by the CDC.3 Health departments located in states with an ACPHP have clearly benefited from tailored workforce training,2,4,5 and many academic centers have also provided local technical assistance that moves beyond training.
The ACPHP network provides a resource for local health departments that are struggling with the development, implementation, and evaluation of public health preparedness plans. However, there are no academic centers in the 13 states of the intermountain West, and there are only three centers on the West Coast (Los Angeles, Berkeley, and Washington). States without an academic center are theoretically served by centers in neighboring states, but distance and a lack of understanding of local context greatly limit crossstate collaboration.
The state of Nevada has been cited as a possible target for bioterrorism because of its status as a world tourism destination. More than 48 million people visit the state each year, typically traveling by air and visiting the casinos in Las Vegas and Reno.6 Nevada does not have its own ACPHP, but two California centers are available to support the state in its public health preparedness efforts: the University of California Los Angeles and the University of California Berkeley. Although each academic center has offered trainings to Nevada's public health workforce, public health professionals have so far underutilized such trainings because they are typically held in California and have not been designed to address the local context of preparedness in Nevada. In addition, these centers have not provided the state and local health departments with technical assistance in their public health preparedness activities.
Nevada has distinct needs that must be assessed locally before appropriate public health preparedness response plans and trainings are developed. For example, “first responders” in Nevada must include casino safety officers and risk managers who will undoubtedly be on the front line of a bioterrorism event occurring in or around a casino. In addition, Nevada is home to 19 federally recognized Native American tribes and 28 bands, colonies, and reservations that are home to more than 26,000 people.7,8 The status of tribes as sovereign nations,9 with few formal relationships with state and local governments, provides unique challenges for local planning and management of a bioterrorism situation.
To meet Nevada's unique public health preparedness needs, the Nevada State Health Division used a portion of its CDC public health preparedness funds to develop a local academic-practice partnership with the University of Nevada Reno's Master of Public Health (MPH) program. The Health Division contracted with the university to assess the bioterrorism risk communication, information, response, and training needs of key stakeholder groups in northern, southern, and rural Nevada. This local needs assessment was not designed to assess the competencies typically addressed by ACPHP network trainings. Rather, it was designed to assist the Health Division in developing a statewide risk communication plan. In addition, the results for several professional stakeholder populations were shared with a local training organization responsible for fulfilling the education and training requirements of the CDC public health preparedness cooperative agreement. The Health Division also plans to draw on the needs assessment results when working with academic centers to develop and implement competencybased trainings in the future.
The stakeholder populations assessed included those previously identified as critical to bioterrorism identification and response: public health and medical providers, emergency response personnel, government and community leaders, and the media.10–12 In addition, locally relevant stakeholder groups were also included in the needs assessment: casino safety officers and risk managers, tribes, and diverse segments of the public such as seniors, Hispanic Americans, African Americans, Asians and Pacific Islanders, the homeless, and students.
From the outset, this two-year partnership has involved public health officials, academic faculty, and graduate and undergraduate students in all phases of project design, development, implementation, and evaluation. During the project's first year, an innovative two-semester bioterrorism risk communication course that combined academic theory and hands-on-experience was developed by MPH academic faculty and Health Division representatives. Ten undergraduate and graduate students were selected to participate in the project (tuition reimbursement and textbooks were provided). Students were trained in risk and crisis communication theory, bioterrorism, and research methodology. Students were equal partners in all aspects of the project, including protocol and instrument development, data collection and analysis, report writing, and presentation of project findings.
In the second year, students who completed year-one training received a stipend to conduct individual bioterrorism needs assessment projects with MPH faculty guidance. In addition, six students in an MPH graduate course in Cultural Diversity Issues in Public Health conducted applied research projects to determine the unique preparedness needs of diverse co-cultural populations in Nevada (African Americans, Asian and Pacific Islanders, Hispanics/Latinos, Native Americans, persons with disabilities, and seniors). Students were trained in bioterrorism, risk communication, cultural issues, and research methodology, and were again involved in all aspects of the project, including protocol and instrument development, participant identification, data collection and analysis, and report writing. Fully involving students as collaborators advanced one of the key aims of the larger academic centers, the training of Nevada's future public health workforce.13
This article outlines the process and results of the assessment conducted through our unique academic-practice partnership. After describing the needs assessment methodology and results, it describes the benefits of this partnership from Health Division, student, and faculty perspectives.
NEEDS ASSESSMENT
Methodology
Between October 16, 2002, and April 13, 2004, focus groups and key informant interviews were conducted statewide in efforts to adequately represent stakeholder populations in northern Nevada (primarily the Reno/Sparks area and Carson City), southern Nevada (primarily the Las Vegas area), and the state's 15 rural counties. This research received a human subjects exemption from the University of Nevada, Reno Social and Behavioral Institutional Review Board.
Focus groups.
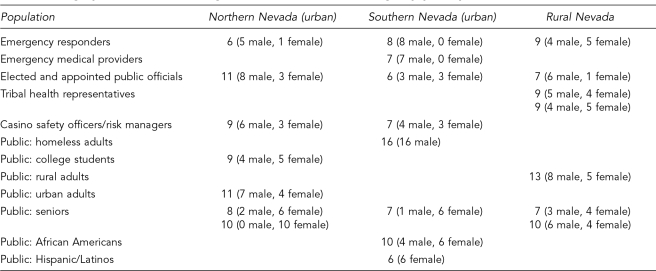
Twenty-two needs assessment focus groups were conducted with a diverse range of stakeholders, including emergency responders (three groups); emergency medical providers (one group); elected and appointed public officials (three groups); tribal health representatives (two groups); casino safety officers or risk managers (two groups); and diverse segments of the public population such as homeless adults, college students, rural adults, urban adults, seniors, African Americans, and Hispanics/Latinos (10 groups). Focus group methodology literature guided the number of participants we recruited for each group (6–10 participants).14 A total of 195 people participated in the focus groups; meetings lasted an average of two hours. Table 1 shows the geographic and gender breakdown of each focus group.
Table 1. Geographic distribution and gender of bioterrorism focus group participants.
Focus group participants were recruited through different mechanisms depending on the nature of the stakeholder population. Professional groups were recruited through professional directories and organizations, and public groups were recruited by posting fliers in community venues and by word of mouth.
Professional focus group participants discussed six topic areas: (1) bioterrorism awareness (two questions); (2) their perceived role in bioterrorism preparedness and response (one question); (3) sources to which they would turn and trust for preparedness information (two questions); (4) preferred methods of communication and information dissemination (one question); (5) anticipated barriers to risk communication and response (one question); and (6) information, education, and training needs (one question).
Discipline-specific questions were also asked of each professional group. Emergency responders were asked about their experience with the incident reporting system (one question). Emergency medical providers were asked about their awareness of smallpox and the smallpox vaccine (one question). Elected officials were asked how they determine the credibility of public preparedness information (one question) and how they decide whether or not to address the public about a possible threat (one question). Tribal health leaders were asked to describe the types of people who would be viewed as credible spokespersons on reservations (one question) and what cultural issues should be taken into consideration when disseminating information to tribes (one question). Casino safety officers and risk managers were asked how they would get information out to their employees and guests if a bioterrorism situation occurred (two questions).
Public focus group participants addressed four topic areas: (1) bioterrorism awareness (two questions); (2) sources the public would turn to and trust for public health and bioterrorism information (two questions); (3) effective information dissemination strategies to get public health and bioterrorism information to the public (two questions with probes about preferred content and format); and (4) anticipated barriers to risk communication and response (one question).
An MPH faculty member and two students conducted each group. A facilitator managed the group and wrote comments on posted flip charts, a scribe recorded all primary content in summary form on the flip charts, and a recorder hand wrote notes and managed two tape recorders. Within 24 hours of group completion, the scribe and recorder typed the flip chart notes and hand-written notes. The session tapes were not transcribed, but the recorder listened to session tapes and added any additional information not recorded in notes. The scribe repeated the same process and integrated her/his notes with those of the recorder. Finally, integrated notes and accompanying session tapes were sent to the facilitator for expansion and clarification as needed.
Following agreement on the content of the notes, the three team members individually coded the data and conducted thematic analyses designed to identify emergent themes and key content for the group. After the individual analyses were completed, the team shared their results. Thematic areas that were clearly identified by all team members were included in the final report. The team also discussed discrepancies in findings and decisions were made about inclusion, exclusion, or combination with other themes collaboratively. A final group analysis report was then written based on the individual coding and group discussion of findings. Once all groups within a particular population and accompanying analysis reports were completed, individual group reports were synthesized into a population summary report.
Key informant interviews.
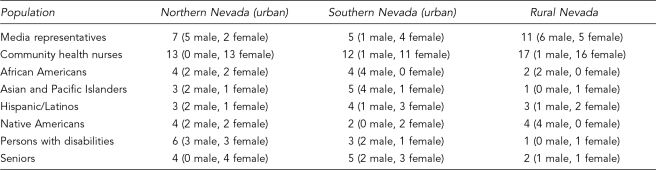
Key informant interviews were conducted with 23 media representatives from across the state and 42 community health nurses representing each urban and rural county. In addition, 10 key informants from each of six co-cultural groups identified by the Health Division were interviewed (African Americans, Asian and Pacific Islanders, Hispanics/Latinos, Native Americans, persons with disabilities, and seniors). A total of 125 key informants were interviewed (Table 2).
Table 2. Geographic distribution and gender of bioterrorism key informant interview participants.
The state and local health departments generated lists of 42 potential media participants and 60 potential community health nurse participants throughout the state. The Health Division sent rural nurses personal letters informing them about the project and inviting them to participate in a conference call about the project.
Co-cultural key informants were selected for potential participation based on perceived expertise and experience with the target population of interest; preference was given to those viewed as leaders by members of the target community. Selection was weighted according to areas of greatest population density and representation of urban and rural populations. Primary and secondary lists of 10 potential interviewees were generated for each population. All potential participants were sent letters of invitation prior to being called for the interview.
The interview protocol for the media, community health nurse, and co-culture key informant interviews required that a maximum of seven telephone calls be made to each potential participant to try to schedule an interview. If after seven attempts the potential participant had not returned a call, s/he was dropped from the interviewee list. If a return call was received, 10 call attempts were made to schedule the interview. If contact was not made after 10 attempts, no further attempts were made for that potential interviewee. The response rate for the media representatives was 55% (23/42) and for community health nurses, 70% (42/60). All co-cultural key informants who were interviewed were from the primary and secondary lists.
Media representatives answered open-ended questions in eight content areas: (1) sources to which they would turn and trust for preparedness information (four questions); (2) barriers to obtaining public health information (one question); (3) information preferences (one question); (4) issues related to source credibility (two questions); (5) their decisions about when and what type of information to release during a public health emergency (four questions); (6) their relationship with public health agencies (one question); (7) their suggestions for future risk communication and event management efforts (one question); and (8) their willingness to participate in public health preparedness activities (three questions).
Community health nurses answered open-ended questions in seven content areas: (1) their perceived role in public health preparedness and response (one question); (2) questions about bioterrorism they had received from the public (one question); (3) sources to which they would turn and trust for preparedness information (three questions); (4) information preferences (three questions); (5) barriers to obtaining public health information and communication with other public health collaborators (four questions); (6) other county stakeholder groups that should be included in risk communication (two questions); and (7) their perceptions of the information and communication needs of unique population groups in their county (six questions).
Co-cultural key informants answered open-ended questions addressing five content areas: (1) where members of the target population would go for bioterrorism information (two questions); (2) what they would want to know, and in what format (three questions); (3) issues related to the perceived credibility of information sources and government trust (three questions); (4) how information can most effectively be delivered to the co-cultural population (five questions); and (5) barriers to disseminating information to the co-cultural population (one question).
One MPH student was assigned to each of the six cocultural populations and one student was assigned to the media and community health nurse populations. Students were responsible for conducting all interviews for their assigned population and simultaneously typing the responses into computer files as the interview progressed. This provided immediate input of data and gave the interviewer the opportunity to ask for immediate response clarification as needed. Following each interview, the interviewer reviewed the interview file, adding and elaborating on typed responses as appropriate. Each interview was sent to the MPH faculty member and graduate student instructor facilitating the course for review. Once all interviews for a target population were complete, the interviewer conducted thematic analyses of interview data and wrote a summary report of findings for the co-cultural group. This report was edited for format and clarity by the graduate student instructor, and for content, based on a second review of the individual interviews by the MPH faculty member. The student and the faculty member discussed discrepancies in findings and decisions were made about inclusion, exclusion, or combination with other themes.
The authors conducted a final thematic analysis across population focus group and key informant reports, providing the basis for the overarching themes discussed in this article The themes that consistently emerged across all stakeholder populations in the focus groups and key informant interviews were prioritized for inclusion.
Results
Four overarching themes emerged in all needs assessment focus groups and key informant interviews conducted with professional groups and diverse segments of the public: (1) the need for effective pre-event education and training; (2) a coordinated and responsive public health preparedness infrastructure; (3)honest, accurate, and timely communication in the event of a bioterrorism situation; and (4) appropriate information dissemination methods and technology.
Effective pre-event education and training.
Stakeholder groups were unanimous in their desire for pre-event bioterrorism education and training. Both public and professional groups emphasized that bioterrorism education and training must occur well before an event to minimize panic and foster appropriate response. Specifically, the public was interested in tailored, personally relevant, and accurate educational information addressing the following questions: (1) what are the possible biological threats; (2) how are different biological agents transmitted; (3) what are the signs and symptoms of infection; (4) what preventive measures can be taken; (5) how will a bioterrorism situation be managed and by whom; (6) how will information be communicated with the public and through what channels; (7) who will the official spokespersons be and what are their qualifications; and (8) where can the public go for more information.
Professional participants believed that the unique characteristics of a bioterrorism situation would require them to play unfamiliar roles that place them outside their comfort zone. Professional stakeholders will need ongoing professional education and training to better understand and assume the responsibilities of their new roles. For example, emergency response and casino representatives believed that they will need training in biological agent recognition, identification, and reporting; isolation and containment; public education and risk communication; and stabilization and recovery.
Similarly, the media has the potential to play a major role in educating the public through large-scale print, radio, and television awareness campaigns. However, all stakeholder groups (including media representatives) realized that for the media to effectively educate the public, they must first be trained in infectious diseases, bioterrorism, risk communication, and event management. Because bioterrorism is not a high frequency event, all groups noted that it is difficult to update and maintain knowledge and skills in this area. Ongoing training and drills will improve the disaster response competencies of all professional stakeholder groups.
A coordinated and responsive public health preparedness infrastructure.
Both public and professional stakeholders articulated the need for a coordinated and responsive public health preparedness infrastructure. Participants were aware that planning is the first step in developing such an infrastructure, but felt that most planning efforts have occurred in isolation. For example, public health preparedness planning funded by the CDC and hospital preparedness planning funded by the Health Resources and Services Administration (HRSA) have not been coordinated statewide. According to participants, public health response will be greatly compromised if individual planning efforts are not integrated into a comprehensive response plan. Participants believed that closer coordination and collaboration would also help clarify roles, minimize “turf battles,” decrease duplication, and save money. They agreed that state and local health departments should take the leadership role in coordinating diverse risk communication and response planning efforts.
It was very clear from focus group and key informant responses that planning efforts in Nevada must involve the casino industry, which has generally been left out of public health preparedness initiatives. Casinos were very interested in collaborating with other stakeholder groups to address public health preparedness issues. Most casino representatives believed that their current emergency plans did not sufficiently address bioterrorism, and they were interested in learning from and collaborating with public health leaders. Smaller casinos expressed a desire to have health departments take primary responsibility for planning for and responding to bioterrorism situations; larger casinos believed they could play a major role in detection and response and were interested in taking proactive steps to be able to do so.
As the public will undoubtedly turn to the media for information regarding bioterrorism, involving the media during the planning phase of bioterrorism preparedness was also cited as critical. In addition to the training noted previously, media representatives identified the need for clear risk communication plans that would be implemented if a bioterrorism situation emerged. Participants believed that such plans should address the importance of open, timely communication to the media; media access to official spokespersons; the establishment of pre-event relationships based on trust and cooperation; and collaboratively developed press release formats.
Planning efforts in Nevada also cannot ignore the role of Native American tribes. Their status as independent sovereign nations with treaty-based relationships with the federal government creates a unique dynamic between state and local government and Native American tribes in terms of public health response. Tribal representatives stated that currently there are few cooperative agreements among tribes, bands, and reservations with local, county, and state governments. Tribal representatives voiced the need for such agreements to clarify issues including communication, resource sharing, and event management for emergency situations occurring on and off tribal lands. In addition, because they are independent nations, each tribe has both a unique administrative structure and service infrastructure requiring the negotiation of individual relationships and communication approaches with each tribal entity.
Finally, participants consistently stated that bioterrorism risk communication and response plans must be routinely pilot-tested to ensure that a coordinated and responsive public health infrastructure is in place. Professional stakeholder groups were particularly concerned that sufficient pilot testing and revision of risk communication and response plans have not occurred. Mock events, tabletop exercises, and simulations are useful. However, to date most of these evaluative efforts have focused on coordination among professional groups tasked with incident response. To adequately test the efficacy of response plans, other key stakeholder groups such as the media, casinos, and the general public must also be included.
The inclusion of the general public in pilot testing and mock exercises may uncover the concerns and needs of different sub-populations. For example, seniors and people with disabilities in our study were concerned that they would not be considered a priority in preparedness and response efforts. Participants from these groups were concerned about whether evacuation plans would address the needs of frail individuals and those with mobility impairments. They were also concerned about the efficacy of assistive technology in the event of an electrical blackout. Pilot testing and mock exercises would also uncover unique infrastructure problems evident in the rural areas, including lack of local media (which leads to a reliance on urban media or, in some areas, media from contiguous states); health care providers and/or facilities; local resources to manage response; and reliable Internet and telephone systems.
Honest, accurate, and timely communication.
All stakeholder groups were very clear that during a bioterrorism situation, they want honest, accurate, and timely information. Participants were adamant that withholding information would damage trust in government and public health agencies and cause panic, effectively inhibiting response. Stakeholders want relevant and accurate information available to them immediately so that they can act as partners in response. Similarly, the general perception of professional groups was that without efficient and accurate dissemination of information to the public, it is much more difficult to appropriately handle emergency situations.
Two sub-themes emerged that help clarify participant perspectives on the need for honest and accurate information. First, the public wants consistent information across sources. For example, if bioterrorism information on one official website is contradicted by information on another official website, public confidence in the knowledge and competence of experts responsible for managing public health emergencies is eroded. Public stakeholders said they want public health and government officials to communicate with a unified voice and whenever possible, use the same materials.
Second, there is need for an identified, credible spokesperson seen by the public as the “official” voice in managing a public health emergency. Characteristics desired in a spokesperson include someone who is knowledgeable, able to establish proactive relationships with the media and diverse stakeholder groups, and open and direct in communication. Participants believed that credibility and trust could be enhanced if the spokesperson was visibly involved in preevent education and training. During an event, spokespersons should not evade questions; rather they should state what they know at a given time and provide frequent updates when new information becomes available. Spokespersons must establish themselves as competent, reliable, approachable authorities in bioterrorism, public health emergencies, and risk communication. By designating a spokesperson to disseminate information, duplication and misinformation can be avoided and the likelihood of a timely response increases.
Appropriate information dissemination methods and technology.
Equally as important as the quality of information is the appropriate dissemination of that information to stakeholders. Analysis of the focus group and key informant interview data suggests that multiple information dissemination methods are necessary for effective risk communication. In addition, information and educational materials must be tailored to the needs of specific stakeholder groups.
Both professional and public participants indicated that the primary method by which they would initially access information in the event of a bioterrorism situation was the media. Stakeholders uniformly expressed a desire for a statewide 1-800 number staffed 24 hours a day, seven days a week by knowledgeable public health professionals. In addition, many participants indicated that they would like to have access to a state bioterrorism website that was easy to navigate. Professional stakeholders suggested secure locations on a bioterrorism web site where tailored-response information would be available. Beyond these generalities, a number of Nevada's diverse public populations identified unique information preferences.
Nevada's rural communities stated that they often prefer print alternatives (fliers, brochures, posters, and fact sheets) to technology-based methods due to unreliable or absent telephone and Internet service, limited media access, and in some cases, lack of electricity. In addition, some stakeholder groups, particularly African American, Asian, Hispanic, and Native American participants, prefer more personal approaches to information dissemination and already have comprehensive communication networks in place, including phone trees, contact lists, and established door-to-door and word-of mouth strategies. Several groups also indicated a preference for community-based information dissemination methods, with churches and schools playing a leadership role. Participants stated that tapping into existing networks and integrating community leaders into planning and dissemination strategies will ultimately enhance information dissemination and public health response.
Professional and public stakeholders also highlighted the need to ensure that the materials developed to provide information are appropriate for the targeted population. For example, for health care providers, medical terminology facilitates communication. However, for the general public, it typically inhibits understanding. Seniors and individuals with disabilities described their need for large print, closed captioning, accessible Internet, and TTD/TTY services. Diverse racial and ethnic populations also urged that bilingual information and educational materials be developed and disseminated via culturally accessible channels.
DISCUSSION
Our results confirm the need for competency-based training for the public health workforce.2–5,13 To be effective, such trainings should help professional groups understand non-traditional roles that they may be asked to play in bioterrorism response.15,16 As our findings demonstrate, training should also be expanded to include non-traditional groups. In Nevada, there is an urgent need for professional trainings for casino safety officers and risk managers who have little public health experience, but will likely be key players if a bioterrorism situation occurs in the state. Our results also support previous research demonstrating the immediate need to train media representatives in bioterrorism and public health preparedness issues.17
An area that has been largely ignored by the literature is the need to develop, implement, and evaluate bioterrorism trainings for the public. The perfect time for developing educational campaigns and trainings may be during “times of calm.”18 Professional groups in our needs assessment felt that the delivery of pre-event training for the public will dispel myths, create a sense of trust, and make their jobs easier when they are actually called upon to respond. Public participants were eager to learn more about bioterrorism and felt that disseminating information before an event adds credibility and will decrease panic if an event actually occurs.
Study participants consistently discussed the need for a coordinated and responsive public health preparedness infrastructure. One approach to coordinated response has been the development of emergency preparedness plans within a variety of response frameworks including public health, hospital, emergency response, and state and county planning.1,9,19 However, as participants discussed frequently, funding to develop these plans and, as a result, planning efforts themselves, have occurred largely in isolation. Involving affected stakeholders in the planning process and sharing individual plans is critical.19 However, key populations such as the media, casino representatives, and the tribes have not been included in public health preparedness planning in Nevada to date. The omission of such groups can undermine planning efforts and may actually hinder appropriate response. For example, the media can be a useful resource for risk communication and response if their needs are also addressed.11,20 Media representatives who participated in our study said that risk communication plans should emphasize open and timely communication with the media, media access to official spokespersons, and the establishment of pre-event media-public health relationships. Our results also support previous calls for the development of pre-event media guidelines and press release formats for covering bioterrorism events.11
Ensuring a coordinated and responsive public health preparedness infrastructure will require simulations and pilot testing of response plans and systems.15 Participants strongly recommended frequent testing, tabletop exercises, and mock events to evaluate the comprehensiveness of plans and identify barriers to execution. Simulated exercises including the public, media representatives, and other non-traditional response groups were recommended. Although such groups are often excluded, a recent simulated outbreak exercise demonstrated the usefulness of including the public and media.17
Our results confirm many of the best practices that have recently been outlined for public health risk and crisis communication, particularly the need to involve stakeholders as legitimate partners and the need for honest and open communication.20 Professional and public participants in our needs assessment wanted truthful information available to them immediately so that they could work as partners in response. They highlighted the central role that trust plays in effective communication and response21 and stated that withholding information ultimately erodes public trust. One suggestion for strengthening public trust included the dissemination of consistent information across diverse sources. This recommendation confirms previous research highlighting public unease with sole-source information.17 Also supporting previous research was the recommendation to designate a credible bioterrorism spokesperson22 who would be visibly involved in pre-event education, training, and information dissemination. During an event, such spokespersons should not evade questions due to incomplete information, but should clearly articulate what they do know.23,24
A final theme that emerged from our data was the need to use diverse information dissemination methods and tailor information to different stakeholder groups. As shown in previous research, the media, particularly television, is the first place the public will turn for information when a public health emergency occurs.22 Recent research has highlighted the importance of making bioterrorism information available on the Internet,25 and the professional and public stakeholders in our study were interested in this option. There was also a great deal of interest in being able to access a statewide 1-800 hotline staffed by public health professionals. However, participants warned against relying on technical forms of information dissemination, particularly in rural counties where television, radio, telephone, and Internet service may be limited. In addition, many participants, particularly African Americans, Asians, Hispanics, and Native Americans, preferred more personal approaches to risk communication, such as word of mouth and receiving information from churches, schools, and other community leaders.
Regardless of the method used to communicate risk information, there was general agreement that the information must be culturally and linguistically appropriate for diverse populations. Recent literature has focused attention on the importance of addressing health literacy when communicating about health issues.18,26,27 This is a challenge when describing infectious diseases and risk assessment. However, every effort should be made to simplify complex materials for the public. It is also important to ensure that appropriate formats are available for the elderly, individuals with disabilities, and non-English speaking populations.
Data limitations
The use of purposive sampling as well as focus group and key informant interview methodologies limits the generalizability of our findings. Due to the size and diverse nature of Nevada's populace, the perspectives of unrepresented or underrepresented populations may differ significantly from those of the participants represented in this report. In addition, as significant developments in bioterrorism awareness and preparedness occurred concurrently with this project, persons who participated in later segments of this initiative may have been better informed regarding bioterrorism than those in the early stages of the needs assessment. Similarly, the methodologies used in this project assess the perspectives of participants at a particular point in time and those views may change over time. Despite these limitations, findings were consistent within groups and across diverse populations.
Benefits of academic partnership
By partnering with students and faculty from a local MPH program, the Health Division was able to gain an understanding of the bioterrorism risk communication, information, response, and training needs of various professional and public stakeholder groups throughout the state. The data collected through this needs assessment gave the Health Division vital information to plan public health preparedness initiatives. This academic-practice partnership also offered a number of benefits to the Health Division and university collaborators, including cost-effectiveness, community insight, and the ability to train future public health workers.
Cost effectiveness and timeliness.
The Health Division did not have a highly developed infrastructure for needs assessment research. Therefore, the available options included hiring staff with appropriate skills or contracting with an outside entity. The creation of new positions within the state personnel system and the recruitment of qualified candidates would have created unacceptable delays. Contracting with a private-sector consultant could have been done in a relatively short time frame, but would have been more costly. A private consultant might also have required additional time to become familiar with the state's relevant public health issues. The development of a local academic partnership allowed the Health Division to capitalize on familiarity with local context, quick response time, and through student involvement, a cost-effective approach to needs assessment. In addition, because public health faculty supervised project activities, it was easier to maintain the public health focus.
Community insight.
A key advantage of using students and faculty to obtain focus group and key informant information was the stakeholder perception that academic institutions are neutral third parties. This view made it easier for stakeholders to share both positive and negative information that was critical to improving preparedness activities. Through this initiative, university collaborators were able to elicit professional and community concerns and assist the Health Division in the development of responsive community-based initiatives.
Training the future public health workforce.
An additional benefit to academic partnerships is the ability to expose future public health workers to real-life public health problems. This initiative balanced theoretical and methodological training with community-based applied research experience. Students involved in this initiative were able to bolster their understanding of the needs of important stakeholder groups and the limitations and challenges inherent in public health practice. As a result of constant interaction with various stakeholder groups throughout Nevada, students were able to learn from and network with professionals, agencies, and communities with diverse perspectives and unique expertise.
As full collaborators in this academic-practice initiative, students also gained valuable and marketable experience in research design, data analysis, and report writing, dissemination, and publication. Students presented findings at local, regional, and national conferences and some were able to use the needs assessment as a basis for their MPH theses and professional projects. The applied research training, exposure to public health practice, and interaction with diverse public and professional populations gave students a strong foundation for their future careers in public health.
CONCLUSION
The bombing of the World Trade Center towers and the Pentagon in September 2001 and the anthrax situation in October 2001 illustrated the need for a coordinated and responsive public health system. State and local health departments across the nation have been tasked with ensuring that their local infrastructure is capable of detecting and appropriately responding to a bioterrorism situation. This is a daunting task because the incubation period of many agents that could be used for bioterrorism creates a situation wherein local authorities may not know that an event has occurred until well after an infectious agent has been released.18
The establishment of local academic-practice partnerships for states like Nevada without a CDC-funded ACPHP, can provide a very effective way for state and local health departments to develop their public health preparedness infrastructure while simultaneously training the future public health workforce.
Acknowledgments
In addition, the authors would like to thank Martha Framsted, Public Information Officer, Nevada State Health Division, and our student research team: Carla Bellusa, Jessey Bargmann, Kyle Leathers, Joyce Letner, Dr. Timothy Ricks, Teresa Sacks, Marcia Sarratea, Anna Treacy, Keri Pruitt, Bryce Putnam, and Jennifer Vinson. We would also like to acknowledge Matthew Wolden for his assistance in editing this manuscript.
Footnotes
Funding for this project was provided by the Nevada State Health Division through CDC Public Health Preparedness Grants U90/ CCU916964-03-01 and U90/CCU916964-04-01.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) [cited 2005 Jan 13];Continuation guidance for cooperative agreement on public health preparedness and response for bioterrorism—budget year five. Available from: URL: http://www.bt.cdc.gov/planning/continuationguidance/index.asp.
- 2.Centers for Disease Control and Prevention (US); Academic Centers for Public Health Preparedness. [cited 2005 Jan 13];CDC program in brief. Available from: URL: http://www.cdc.gov/programs/partnr01.htm.
- 3.Association of Schools of Public Health. Academic Centers for Public Health Preparedness. Available from: URL: http://www.asph.org/acphp/about.cfm.
- 4.Atchison CG, Uden-Holman T, Greene BR, Prybil LD. Developing the academic institution's role in response to bioterrorism: the Iowa Center for Public Health Preparedness. J Public Health Manag Pract. 2003;9:418–26. doi: 10.1097/00124784-200309000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Morse SS. Building academic-practice partnerships: the Center for Public Health Preparedness at the Columbia University Mailman School of Public Health, before and after 9/11. J Public Health Manag Pract. 2003;9:427–32. doi: 10.1097/00124784-200309000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Nevada Commission on Tourism. [cited 2005 Jan 13];Discover the facts. Fourth Quarter 2003. Available from: URL: http://www.travelnevada.com/news_discover.asp.
- 7.Department of the Interior (US), Bureau of Indian Affairs. Indian entities recognized and eligible to receive services from the United States Bureau of Indian Affairs. [cited 2005 Jan 13];Federal Register. 2003 68:68180–4. Available from: URL: http://www.fns.usda.gov/fdd/programs/fdpir/bia-list.pdf.
- 8.Census Bureau (US) [cited 2005 Jan 13];Census 2000 data for the State of Nevada. Available from: URL: http://www.census.gov/census2000/states/nv.html.
- 9.Bashir A, Lafronza V, Fraser MR, Brown CK, Cope JR. Local and state collaboration for effective preparedness planning. J Public Health Manag Pract. 2003;9:344–51. doi: 10.1097/00124784-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Hamburg MA. Bioterrorism: a challenge to public health and medicine. J Public Health Manag Pract. 2000;6:38–44. doi: 10.1097/00124784-200006040-00007. [DOI] [PubMed] [Google Scholar]
- 11.Wyatt HW. The role and responsibility of the media in the event of a bioterrorist act. J Public Health Manag Pract. 2000;6:63–7. doi: 10.1097/00124784-200006040-00011. [DOI] [PubMed] [Google Scholar]
- 12.Cherry CL, Kainer MA, Ruff TA. Biological weapons preparedness: the role of physicians. Intern Med J. 2003;33:242–53. doi: 10.1046/j.1445-5994.2003.00391.x. [DOI] [PubMed] [Google Scholar]
- 13.Lichtveld M, Cioffi J, Henderson J, Sage M, Steele L. People protected—public health prepared through a competent workforce. J Public Health Manag Pract. 2003;9:340–3. doi: 10.1097/00124784-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Morgan DL. Planning focus groups. Thousand Oaks (CA): Sage Publications; 1998. pp. 71–5. [Google Scholar]
- 15.Bioterrorism alleging use of anthrax and interim guidelines for management—United States, 1998. MMWR Morb Mortal Wkly Rep. 1999;48:69–74. [PubMed] [Google Scholar]
- 16.Garrett LC, Magruder C, Molgard CA. Taking the terror out of bioterrorism: planning for a bioterrorist event from a local perspective. J Public Health Manag Pract. 2000;6:1–7. doi: 10.1097/00124784-200006040-00003. [DOI] [PubMed] [Google Scholar]
- 17.DiGiovanni C, Reynolds B, Harwell R, Stonecipher EB, Burkle FM. Community reaction to bioterrorism: prospective study of simulated outbreak. Emerg Infect Dis. 2003;9:708–12. doi: 10.3201/eid0906.020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rudd RE, Comings JP, Hyde JN. Leave no one behind: improving health and risk communication through attention to literacy. J Health Commun. 2003;8(Suppl 1):104–15. doi: 10.1080/713851983. [DOI] [PubMed] [Google Scholar]
- 19.Gallo RJ, Campbell D. Bioterrorism: challenges and opportunities for local health departments. J Public Health Manag Pract. 2000;6:5762. doi: 10.1097/00124784-200006040-00010. [DOI] [PubMed] [Google Scholar]
- 20.Covello VT. Best practices in public health risk and crisis communication. J Health Commun. 2003;8(Suppl 1):5–8. doi: 10.1080/713851971. [DOI] [PubMed] [Google Scholar]
- 21.Shore DA. Communicating in times of uncertainty: the need for trust. J Health Commun. 2003;8(Suppl 1):13–4. doi: 10.1080/713851977. [DOI] [PubMed] [Google Scholar]
- 22.Pollard WE. Public perceptions of information sources concerning bioterrorism before and after anthrax attacks: an analysis of national survey data. J Health Commun. 2003;8(Suppl 1):93–103. doi: 10.1080/713851974. [DOI] [PubMed] [Google Scholar]
- 23.Koplan JP. Communication during public health emergencies. J Health Commun. 2003;8(Suppl 1):144–5. doi: 10.1080/713851967. [DOI] [PubMed] [Google Scholar]
- 24.Golan K. Surviving a public health crisis: tips for communicators. J Health Commun. 2003;8(Suppl 1):126–7. doi: 10.1080/713851978. [DOI] [PubMed] [Google Scholar]
- 25.Hobbs J, Kittler A, Fox S, Middleton B, Bates DW. Communicating health information to an alarmed public facing a threat such as a bioterrorist attack. J Health Commun. 2004;9:67–75. doi: 10.1080/10810730490271638. [DOI] [PubMed] [Google Scholar]
- 26.Parker RM, Gazmararian JA. Health literacy: essential for health communication. J Health Commun. 2003;8(Suppl 1):116–8. doi: 10.1080/713851963. [DOI] [PubMed] [Google Scholar]
- 27.Payne JG, Schulte SK. Mass media, public health, and achieving health literacy. J Health Commun. 2003;8(Suppl 1):124–5. doi: 10.1080/713851972. [DOI] [PubMed] [Google Scholar]