Abstract
Understanding whether the gradient in children’s health becomes steeper with age is an important first step in uncovering the mechanisms that connect economic and health status, and in recommending sensible interventions to protect children’s health. To that end, this paper examines why two sets of authors, Chen et al (2006) and Case et al (2002), using data from the same source, reach markedly different conclusions about income-health gradients in childhood. We find that differences can be explained primarily by the inclusion (exclusion) of a small number of young adults who live independently.
Keywords: USA, Socioeconomic status, child health
Introduction
The relationship between socioeconomic status (SES) and health in childhood is an active and important area of research, one that may improve our understanding of the origins of socioeconomic gradients in adult health, and mechanisms through which the intergenerational transmission of poverty takes place. For these reasons, we read with interest the recent article “Socioeconomic status and health: Do gradients differ within childhood and adolescence?” (Chen, Martin and Matthews, 2006). These authors examine how family income is related to a number of childhood health measures, and how these relationships change with the age of the child. For two acute conditions—accidental injuries and acute respiratory conditions—they find that the relationship between low income and poor health becomes more pronounced during adolescence. However, for global health measures, including parent-assessed health and two measures of activity limitations due to poor health, they do not find that income gradients in health are larger for older children. This result stands in sharp contrast to recent findings that the relationship between household income and parent-assessed health becomes more pronounced as children age, with no diminution of the gradient in adolescence (Case, Lubotsky and Paxson, 2002).
The larger literature on this topic is also marked by differences in conclusions about the age pattern of gradients in children’s health. For example, Currie and Stabile (2003) present Canadian evidence that is consistent with that of Case, Lubotsky and Paxson, suggesting that universal health insurance neither reduces socioeconomic gradients in children’s health nor changes the age patterns of these gradients. However, other research concludes that the SES gradients in health that are present in earlier childhood flatten or disappear in adolescence, only to re-emerge in adulthood (West, 1997; West and Sweeting, 2004). These divergent results may be due to differences across studies in the measures of health or SES that are used, as well as differences in sample sizes and methods of data collection and analysis. The difference in findings regarding parent-assessed health between Chen, Martin and Matthews (CMM) and Case, Lubotsky and Paxson (CLP) are more surprising, given that the two sets of authors rely on the same data source – the US National Health Interview Survey (NHIS) – and base their analyses on the same measure of socioeconomic status.
Understanding whether the gradient in children’s health becomes steeper with age is an important first step in uncovering the mechanisms that connect economic and health status, and in recommending sensible interventions to protect children’s health. To that end, this paper examines why these authors reach such different conclusions about the income gradient in parent-assessed health in childhood. We find these differences can be explained primarily by the inclusion, as if they were dependent children, of younger adults living independently. Secondary factors include CMM’s use of only one year of data, resulting in a relatively small sample size, and their use of a categorical rather than a US dollar-based measure of income.
Methods
Sample choice
CLP analyzed 10 years of NHIS data for approximately 230,000 children aged 0 to 17, surveyed between 1986 and 1995. CMM analyzed data from the 1994 round of the NHIS for approximately 30,000 children aged 0 to 18. CMM note that, in most cases, a proxy adult respondent (typically the child’s mother) reported on the health of persons under age 19. For simplicity, they refer to these responses as ‘parental reports.’
From this description, it is clear that the samples analyzed varied in two important ways. CLP worked with a data set that was an order of magnitude larger. In addition, CLP excluded 18-year-olds from their analysis, while CMM did not. CLP noted that they chose not to include 18-year-olds because they were concerned about the living arrangements of college-aged individuals, and whether these respondents would report their current incomes or the incomes of the families in which they were raised.
Data from the 1994 NHIS suggest it may be problematic to include 18-year-olds in such analyses. In the NHIS, all relationships are recorded relative to a reference person, who is the person who rents or owns the housing unit surveyed. While, overall, less than one percent of children in 1994 reported themselves to be the household reference person, two percent of 17-year-olds and 17 percent of 18-year-olds did so. (In what follows, we will refer to a young adult who is not the household reference person as ‘dependent’ and one who is the household reference person as ‘independent.’) Nearly 80 percent of independent 18-year-olds have completed at least 12 years of schooling (in contrast to 50 percent of the dependent 18-year-olds), suggesting that a non-trivial fraction of 18-year-olds living away from their families of origin may be enrolled in college. The current household income of such 18-year-olds will be a poor guide to the socioeconomic status of the households in which they were raised, and may be an inaccurate estimate of their access to resources. Indeed, only 2 percent of dependent 18- year-olds reported household incomes of less than $5,000, while fully 70 percent of independent 18-year-olds did so. Moreover, if the healthiest and highest SES 18-year-olds were more likely to have left for college, their systematic absence in their households of origin and their presence in newly formed (apparently low income) households will bias estimates of the impact of household socioeconomic status on health outcomes, at least to some degree.
Variable construction
CLP and CMM also differ in their construction of the household income variable. For all years from 1986 to 1995, the NHIS reports information on total household income for 27 income categories, coded from 0 to 26—corresponding to $1000 intervals for incomes between $0 and $20,000, and to $5,000 intervals for incomes between $20,000 and $50,000. The highest income category is “$50,000 or more,” so all household incomes above $50,000 are top coded.
CLP assigned incomes to these income categories using data from the 1986–1995 March Current Population Surveys (CPS), which are nationally representative surveys of over 50,000 American households per year. Although CLP assigned incomes using information on both the income bracket and the education level of the household reference person, here we take the simpler approach, closer in spirit to the CMM measure, of assigning incomes using only the income bracket. Specifically, we compute the mean total household income in the CPS, using survey weights, for households within each NHIS income category and each year, and assign these mean income levels to NHIS respondents as appropriate. Thus, an NHIS household with an income category of “$20,000 to $25,000” in 1994 is assigned the average income level of all CPS households observed in 1994 whose incomes ranged from $20,000 to $25,000. (See the Appendix to CLP for details.) CLP’s specifications generally used the logarithm of household income as an explanatory variable. Implicit in this specification is the assumption that, in wealthy and poor households alike, a one-percent increase in household income has the same marginal effect on the health of children of a given age. However, CLP note that their results are robust to changes in functional form. In particular, their finding that the gradient in children’s health becomes steeper with each year of age continues to hold when household income is used in place of the logarithm of household income.
CMM chose to measure household income as the categorical income variable published in the NHIS. That is, their income variable consists of integer values from 0 to 26. Implicit in this choice is an assumption that a $1000 increase in income in poorer households (i.e., a one-unit change in the NHIS’s categorical income variable for households with incomes below $20,000) has the same marginal effect on children’s health as does a $5,000 increase in income in wealthier households (i.e., a one-unit change for households with incomes above $20,000 annually). This specification has the unusual implication that the effect of an additional dollar is five times as large for households with incomes of $19,999 than it is for households with incomes of $20,000.
Data analysis
We re-analyzed the NHIS data using STATA/SE 9.2. Following CMM, we first ran logistic regressions using 1994 data only, in which an indicator that a child is reported in fair or poor health is regressed on the income measure used by CMM, age, an income-age interaction, and controls for race (white, black, other) and sex. The sample includes 27,833 children aged 0 to 18. (Of the 33,911 children in the 1994 sample, 6,078 had missing values for health status, race or income.) The analysis is repeated, restricting the sample to dependent children (that is, removing 232 children – primarily 17 and 18 year olds – reported to be the household reference person). We then estimate this model combining two years of data, 1994 and 1995 (n=52,803), and then again using 10 years of NHIS data from 1986–95 (n=274,623). Finally, we repeat these analyses using the logarithm of income in place of the CMM measure. All results were weighted using sampling weights. In all cases, we report odds ratios (ORs) so that our results can be directly compared to those of CMM. The tables report robust standard errors, from which 95% confidence intervals can be readily constructed.
Results
Table 1 presents the results of logistic regressions using the CMM categorical income measure in columns 1 to 5, and using the CLP log income measure in columns 6 to 8. Column 1 reproduces CMM’s estimate of the impact of household income on the log odds of reporting a child in fair or poor health, and column 2 produces results reported in CMM that they find no significant age-income interaction term. The lack of a significant age-income interaction term is also seen in column 6, where the categorical income measure has been replaced by log income. However, once the 232 independent young adults are removed from the sample (column 7), the age-income interaction using log income becomes statistically significant (P<.05). The age-income interaction is also statistically significant using cardinal income when dependents are removed and one additional year of survey data is used in the analysis (column 4). For both income specifications using 10 years of NHIS data (columns 5 and 8), once young adults living independently are removed from the sample, we find age-income interactions that are statistically significant (P’s<.01). Thus, CMM’s conclusion that the relationship between income and health does not change with age can be overturned by removing dependents, and either expanding the sample or using a money-based rather than categorical income measure.
Table 1.
Exploring income-age interactions using data from the National Health Interview Survey
| CMM income measure (cardinal income) | CLP income measure (log income) | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Income | 0.935 (0.004)** | 0.935 (0.008)** | 0.941 (0.008)** | 0.941 (0.006)** | 0.940 (0.003)** | 0.636 (0.029)** | 0.683 (0.034)** | 0.682 (0.012)** |
| Age × Income | 1.000 (0.001) | 0.999 (0.008) | 0.998 (0.0006)** | 0.998 (0.0003)** | 1.004 (0.004) | 0.989 (0.005)* | 0.987 (0.002)** | |
| Sample | All | All | Dependents | Dependents | Dependents | All | Dependents | Dependents |
| Years | 1994 | 1994 | 1994 | 1994–95 | 1986–95 | 1994 | 1994 | 1986–95 |
| Observations | 27,833 | 27,833 | 27,601 | 52,803 | 274,623 | 27,833 | 27,601 | 274,623 |
Note: Odds ratios from logistic regression models, standard errors in parentheses. The dependent variable equals 1 if the child is in fair or poor health, 0 otherwise. Log income is calculated using the mean of each income bracket in the March Current Population Surveys. All models include controls for age, race, and sex, and are weighted using survey weights. Models that include more than one year of data include year indicators.
significant at 5%.
significant at 1%.
The estimates imply substantial changes in the relationship between income and health as children become older. The results in column 8 suggest that a change in household income from $54,000 to $12,000 (a change from the 75th to the 25th percentile of the income distribution in 1994) at age 3 increases the probability of being in fair or poor health from 1.456 percent to 2.736 percent. The same change in household income at age 15 increases the probability from 1.446 percent to 3.407 percent.
Table 1 indicates that the inclusion of a small number of young adults living on their own changes the estimated age-income interaction term dramatically. This can also be seen in Figure 1, which plots the odds ratios for log income from logistic regressions run separately for each age, from 0 to 18, for all children observed in the NHIS from 1986 to 1995. The lightly shaded diamonds represent the odds ratios for log income from age-specific regressions run for all children, while the darkly shaded circles correspond to the odds ratios for dependent children only. These show convincingly that income is increasingly protective with age when the newly-independent children are excluded. Note that, from age 0 to age 13, there are no differences in the estimated coefficients for the two samples—dependents only and all children—because no children below age 14 are reported to be living on their own. The low incomes of college-aged young adults living independently have a very large effect on the estimated relationship between income and health status in the NHIS for 17 and 18 year olds. Similar results are found using ordered probits of health status, measured on a five-point scale. When we re-estimated the models in Table 1 using ordered probits rather than logistic regressions, we found that excluding independent young adults resulted in large and statistically significant age-income interactions, even using only 1994 data and the CMM income measure.
Figure 1. Age patterns in the fair/poor health gradient, NHIS 1986–1995.
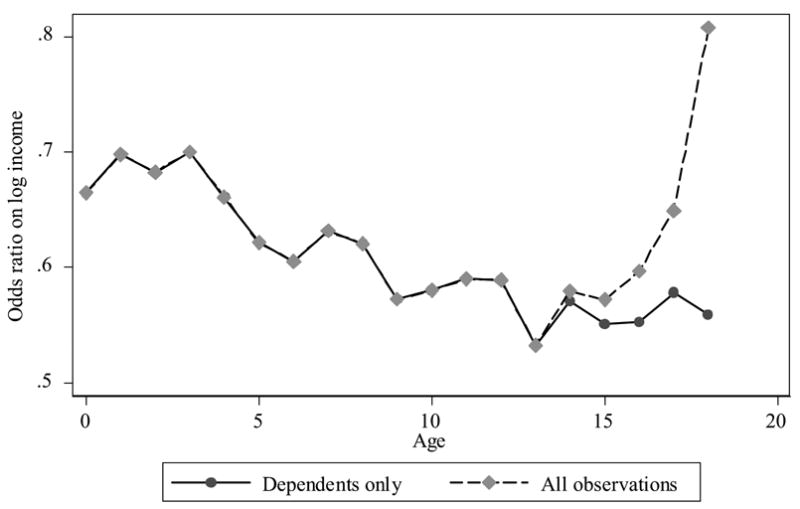
Note: Each point represents the OR on log income from logistic regressions estimated separately for each year of age. The dependent variable equals 1 if the child is in fair/poor health, 0 otherwise. Odds ratios are adjusted for race, sex, and survey year. All specifications are weighted using sampling weights.
Discussion
The differences in the age patterns observed for income-health gradients between CMM and CLP are not driven by CMM’s use of a categorical income variable. Both the CLP and the CMM age-income interactions terms are insignificant when young adults living independently are included in the analysis. Both become highly significant and imply large changes in the gradient with age when the analysis is restricted to dependent children and 10 years of NHIS data are used.
Neither are the differences between the CLP and CMM results due to the much larger sample size used by CLP. When the model shown in column (8) of Table 1 is estimated with independent young adults included, the age-income interaction is not significantly different from one (OR=1.001, P=.523). Rather, the differences between the CLP and CMM results are driven primarily by CMM’s inclusion of independent 18-year-olds. We believe it is inappropriate to include these young adults in an analysis of the impact of socioeconomic status on health in childhood and adolescence, as the “socioeconomic status” markers available for these independent college-aged individuals are likely to be a poor reflection of the socioeconomic status they enjoyed for much (or most) of their lives.
CMM examined two global health measures in addition to parent-assessed health: activity limitations and school limitations. We repeated our analyses using these health measures to see if results are sensitive to the treatment of independent young adults, the definition of income and the sample size. CMM’s conclusion that income gradients in school limitations do not increase with age is not affected by these changes. The measure of school limitations is available only for children ages 5 to 17, and so the issue of including or excluding independent children—most of whom are 18 years old—is less important for this health measure than for others. However, for activity limitations, we find a large and statistically significant age-income gradient when independent young adults are excluded, but only when 10 years of data are used. In this case, the decision to include or exclude this group makes a large difference to the results. For example, using the CLP income measure and including independent young adults, the odds ratio for the age-income interaction exceeds 1 (OR=1.007, P<.05), implying that the differences in activity limitations across income levels become smaller with age. However, this conclusion is reversed when only dependent children are included (OR=0.995, P<.05).
Estimates that use alternative measures of socioeconomic status in a child’s household of origin are likely to have similar problems. CMM construct and use a variable measuring the years of education of a parent (or responsible adult) in each child’s household. However, creation of this variable is made problematic by the 17- and 18-year-olds who report themselves as the household reference person. For these young adults, the education of the “responsible adult” defaults to their own education (in most cases, 12 years of completed schooling). This adds measurement error to a variable intended to capture long-term effects of parents’ education, and may bias all estimated coefficients.
Young adults are an important group, deserving of attention. However, we will learn more by following them longitudinally (out of their households of origin and into adulthood – see, for example, Case, Fertig and Paxson, 2005) than we will learn looking at them in cross-sectional studies, such as the NHIS.
Author Comments: This research was supported by NICHD grant HD041141. We thank Angus Deaton for comments on an earlier draft.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr Anne Case, Princeton University Princeton, NJ UNITED STATES.
Christina Paxson, Princeton University, cpaxson@princeton.edu.
Tom Vogl, Princeton University, tvogl@princeton.edu.
References
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. Journal of Health Economics. 2005;24:365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Case A, Lubotsky D, Paxson C. Economic status and health in childhood: The origins of the gradient. American Economic Review. 2002;92:1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Chen E, Martin AD, Matthews KA. Socioeconomic status and health: Do gradients differ within childhood and adolescence? Social Science & Medicine. 2006;62:2161–2170. doi: 10.1016/j.socscimed.2005.08.054. [DOI] [PubMed] [Google Scholar]
- Currie J, Stabile M. Socioeconomic status and child health: Why is the relationship stronger for older children? American Economic Review. 2003;93:1813–1823. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- West P. Health inequalities in the early years: Is there equalization in youth? Social Science and Medicine. 1997;44:833–858. doi: 10.1016/s0277-9536(96)00188-8. [DOI] [PubMed] [Google Scholar]
- West P, Sweeting H. Evidence on equalization in health in youth from the West of Scotland. Social Science and Medicine. 2004;59:13–27. doi: 10.1016/j.socscimed.2003.12.004. [DOI] [PubMed] [Google Scholar]


