Abstract
We describe a program of research examining how the relationship between positive and negative affect varies both between individuals and within individuals over time. This Dynamic Model of Affect (DMA) proposes that under conditions that promote maximal information processing, positive and negative affective systems function relatively independently. In contrast, under conditions characterized by uncertainty, including pain and stress, the affects become strongly inversely related. Included in our consideration are potential individual differences in the ability to sustain affective differentiation during pain and other stressors, and the implications of this model for perceptions of social relations and for interventions to improve well-being among the chronically ill.
Chronic health problems increase with age, and represent a major source of the kind of unpredictable and uncontrollable circumstances that are especially problematic for individuals and their families. The most prevalent health problem experienced by aging populations is chronic pain, particularly pain caused by musculoskeletal diseases, estimated to affect up to 25% of the adult population (Lawrence et al., 1998). This debilitating medical condition impinges on individuals’ lives in multiple ways, often draining away much needed energy and interfering with the ability to fulfill important obligations and pursue valued activities. Mood disturbance is common; recent estimates suggest that 30 to 50% of chronic pain patients are currently depressed (Banks & Kerns, 1996).
Perhaps not surprisingly, much of the focus of efforts to assist patients in the management of chronic pain has been directed toward decreasing pain and the negative affect (NA) that so often accompanies it (Nicassio & Greenberg, 2001). One assumption that underlies the attention to alleviating negative affective experiences while largely disregarding positive affect (PA) is that negative and positive affective states vary along a single, bipolar dimension, ranging from high levels of positive affect on one end to high levels of negative affect at the opposite end (e.g., Feldman-Barrett & Russell, 1998; Green, Goldman, & Salovey, 1993; Russell & Carroll, 1999). According to this conceptualization, a decrease in pain and other negative affective states should invariably result in an increase in positive affect. Indeed, there is evidence consistent with this view (Lefebvre et al., 1999). Presumably, attention to positive affect in the alleviation of suffering in chronic pain would be equally tenable, but perhaps seems less salient, given the more pressing demands for resolution that accompany negative affective symptoms.
An alternative perspective posits that positive and negative affects exist on distinct dimensions, such that positive and negative affective systems can be activated independently (e.g., Watson, Wiese, Vaidya, & Tellegen, 1999; Cacioppo & Bernston, 1994; Cacioppo, Gardner, & Bernston, 1999). Evidence that everyday negative events relate to changes in NA but not PA, and that positive events relate to changes in PA but not NA, lends credence to this view (e.g. Gable, Reis, & Elliot 2000; Goldstein & Strube, 1994). Moreover, recent work examining the neural substrates of emotion, using brain imaging technologies such as positron emission tomography (PET) and functional magnetic resonance imaging (fMRI), has yielded findings that suggest the existence of distinct neural systems for positive and negative evaluative channels that can be manipulated independently (e.g., Canli, Desmond, Zhao, Glover, & Gabrieli,, 1998; Canli, Zhao, Desmond, Kang, Gross, & Gabrieli, 2001; Davidson, Jackson, & Kanlin, 2000). Although positive and negative affects appear to be regulated by separate neurocognitive systems (Canli et al., 1998), both rely extensively on neuronal feedback loops during stress to function optimally (Sackheim, & Weber, 1982).
Both the bipolar and bifactorial models are useful in describing the everyday experiences of affect, but neither provides a comprehensive framework that accounts for diverse affective phenomena. The question may not be whether PA and NA form one or two dimensions, but under what sort of circumstances a uni- or bi-dimensional model would apply. In this article, we present a body of work suggesting that the distinction between positive and negative affect varies in different situational contexts, a perspective we have called the Dynamic Model of Affect (DMA; Potter, Zautra, & Reich, 2000; Reich, Zautra, & Davis, 2003; Zautra, 2003; Zautra, Potter, & Reich, 1997). We argue that not only does affective differentiation vary within individuals over time but also that the degree of differentiation of affective states, and likely the influence of situational context on this differentiation, varies between individuals. Chronic pain provides an especially salient context in which to examine the changing relationship between PA and NA, in part, because pain itself has an affective component (Fernandez & Turk, 1992; Melzak & Wall, 1965). The neural substrates of the experience and anticipation of pain overlap with those of aversive emotion (Ploghaus et al., 1999). The experience of pain thus is likely to be influenced by affective changes and by interventions targeting affect differentiation. Below we review our work contributing to the development and elaboration of this model in chronic pain patients, and then discuss the implications of our perspective for promoting resiliency in the face of chronic pain and other health-related disorders.
The Dynamic Model of Affect
The model we propose builds on research examining the contextual determinants of information processing (e.g., Linville, 1985; 1987; Paulhus & Lim, 1994; Ursin & Olff, 1993). Like cognition, the experience of emotion always occurs in an environmental context. In a safe and predictable environment, we are able to process information from multiple sources, including emotional inputs, to develop an adaptive response. This complex processing demands substantial resources but provides us with a rich and nuanced assessment of our environment, and of the current demands our environment is placing upon us. Thus, in calm and predictable times, we acquire information arising not only from negatively valenced aspects of a situation, but also from its positively valenced features. Counts of positive and negative affect provide little overlapping information here, allowing us to access and integrate the fullest possible range of information. This allows us maximal flexibility in fashioning an optimal response at any given moment. In times of low stress, then, we would expect positive and negative affects to be relatively uncorrelated.
During times of stress and uncertainty, the need to process information rapidly takes precedence over any advantages that accrue from more differentiated evaluation of stimuli. In essence, we can no longer afford to expend our resources on complex, time-consuming processing. Rather our attention narrows to focus on the immediate demands and potential threats to our well-being. Our judgments become more simplified and rapid, allowing us to quickly adopt adaptive behaviors that are necessary to alleviate the discomfort of the situation. In such contexts, we preferentially process negative information at the expense of positive. Thus, during times of stress, PA and NA fuse to become a simple bipolar dimension reflected in a high inverse relationship between the two. Although our model proposes that stressful contexts influence affective information processing to some extent for all individuals (e.g., Zautra, Reich, Davis, Potter & Nicolson, 2000; Zautra et al., 1997), we suspect that the influence may be especially potent for chronic pain patients, a group whose cognitive resources may already stretched to the limit, especially when they are distressed (Hart, Wade, & Martelli, 2003). Compared to healthy individuals, for example, chronic pain patients are more likely to report a tendency to process information in a simple fashion (Reich, Zautra, & Potter, 2001). The chronic pain condition itself may serve as a stressor, reducing the individual's capacity for information processing, and shrinking affective space. Many of the difficulties with emotions that accompany stress, in fact, are also apparent among those in chronic pain. In our own work examining affective dynamics among those without chronic pain, we have found evidence consistent with the DMA (e.g., Reich et al., 2001; 2003; Williams et al., 2001; Zautra, Schultz, & Reich, 2000). Here we focus attention on individuals whose daily experiences occur in the context of chronic pain, to further examine the evidence for and explore the implications of the DMA.
Stress, Pain, and Affect Differentiation
In our earliest work examining the changing relationship of PA and NA during stress for those in pain, we assessed the experience of interpersonal events, affect, and pain in 41 female rheumatoid arthritis (RA) patients (Zautra et al., 1997; Potter et al., 2000, Study 1). Participants were interviewed each week over a 12-week period regarding their experience of 21 daily events involving spouse, family, friends and coworkers during the preceding week, with the Inventory of Small Life Events (ISLE; Zautra, Guarnaccia, & Dohrenwend, 1986). This instrument provides a frequency count of negative interpersonal events that are independent of confounds such as personality, psychopathology, and physical well-being. PA and NA were assessed with the Positive and Negative Affect Schedule (Watson, Clark, & Tellegen, 1988), and pain was measured with a 101- point visual analog scale (VAS), ranging from “no pain” to “pain as bad as it could be.” Ratings of negative events were summed by week to provide an index of stress, which was then used to identify high and low stress weeks for each participant. The DMA predicts that the inverse correlation between PA and NA should be of greater magnitude during high vs. low stress weeks, and indeed this was the case. For the 390 weeks identified as low stress, the correlation between PA and NA was modest (r=−.12, p = .023). In contrast, during the 33 weeks identified as high stress, PA and NA were strongly inversely correlated (r= −.56, p = .001). Moreover, the two correlations were significantly different from one another (z=2.82, p = .003)1. We also ascertained whether stress altered the relationship between pain and the dimensions of affect. As expected, during weeks of low stress, pain was related to increased NA (r=.26, p < .001), but was unrelated to PA (r=.01, ns). The DMA predicts, though, that shrinking affective space associated with stress includes experience of pain, such that pain should become even more tightly bound to NA, and perhaps even show a relationship with PA. The predicted patterns were born out in the data; during high stress weeks, pain became more strongly related to greater NA (r=.63, p < .001), and with lesser PA (r=−.60, p < .001).
If pain functions as a stressor, we would expect PA and NA to become more highly related during pain episodes. We tested this possibility in a study of 175 patients with RA or osteoarthritis (OA) who were interviewed weekly for 12 weeks regarding their experience of pain, PA, and NA (Zautra, Smith, Affleck, & Tennen, 2001, Study 1). Pain was assessed with a 101-pt scale that queries participants about their average level of pain during the preceding week due to their arthritis, and PA and NA were measured with the PANAS (Watson et al., 1988). Hierarchical linear regression analyses were conducted to test the associations, which allowed us to estimate the average within-person correlation between PA and NA over time in a way that removes biases in that estimation due to between subjects differences in the levels of affect. Results revealed that, as expected, weekly increases in pain and decreases in PA each predicted weekly increases in NA (both ps < .001). Of particular relevance for the current question, changes in PA and pain interacted to predict changes in NA (p < .01). Consistent with our predictions based on the DMA, the data suggested that increases in weekly pain were related to a stronger inverse relationship between weekly PA and NA.
We replicated these findings in a second sample of patients diagnosed with Fibromyalgia (FM), a widespread pain syndrome of unknown etiology that affects approximately 4% of adult women (Lawrence et al., 1998). Sixty FM patients reported on their pain and affect three times per day for 30 consecutive days (Zautra et al, 2001, Study 2). Pain was assessed by averaging ratings of current pain intensity across each of 14 areas of the body, corresponding to the widespread pain criteria required for an FM diagnosis. PA and NA were measured with the Mood Adjective Checklist (Larsen & Diener, 1992). Again, hierarchical regressions were conducted to probe whether the associations between the affects varied depending on the experience of pain.
Consistent with the findings for RA patients, an interaction emerged between changes in daily PA and pain in the prediction of NA (p < .01), indicating that PA had a stronger inverse relationship with NA when pain was high. Thus, in two samples of patients with distinct pain conditions, employing different measures of pain and affect, and assessing experiences across differing time frames, we demonstrated that affective states appear to become less differentiated with increased pain. Pain, then, seems to foster the collapse of affective space akin to that elicited by stress.
To this point, we have presented findings generated from longitudinal data collected in the field to examine pain-affect dynamics. Complementary data are available from laboratory-based work, where affect-pain relationships in response to more tightly controlled stress conditions can be explored. We conducted comparisons between 20 women with FM and 21 age-matched women with OA during a laboratory session that included an initial rest period followed by a semi-structured interview regarding a recent interpersonal conflict (Davis, Zautra, & Reich, 2001). PA and NA were assessed with the PANAS (Watson et al., 1988), and pain with the 101-pt VAS described above.
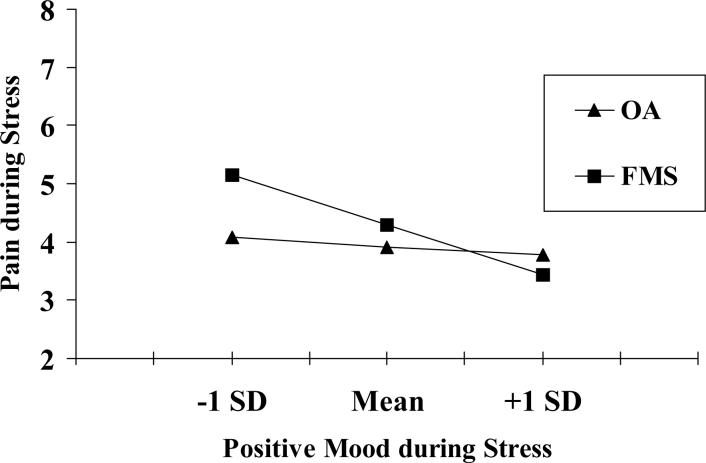
We were especially interested in comparing the two pain groups. Although living with chronic pain of any sort engenders difficulty, the degree of stress and uncertainty may not be constant across all types of pain conditions. In particular, living with pain that is unpredictable and poorly understood may be especially problematic. FM represents just such a condition. The pain in FM is widespread and debilitating, and has no known physical cause and no uniformly effective treatment. Thus, limited understanding of the condition together with a lack of prospects for relief are likely to enhance feelings of uncertainty for FM patients, even relative to other patients with serious pain conditions. In fact, we recently have found that ratings of uncertainty regarding their illness and prognosis are much higher in FM relative to OA patients (unpublished data). We reasoned that based on the DMA, women with FM would show greater collapse between pain and affect during stress than would their OA counterparts. A regression model was tested that predicted pain during stress from diagnostic group, pain at baseline, PA and NA during stress, and interactions between diagnosis and affect measures. Results revealed that NA was related to greater pain during stress across both pain groups. However, a different pattern emerged for PA. As displayed in Figure 1, PA was unrelated to pain during stress among women with OA, but significantly negatively related among women with FM. These findings held when controlling for age and other demographic variables, and suggest that FM patients may have more difficulty than OA patients sustaining the boundaries between positive affect and pain during stress.
Figure 1.
Diagnostic group differences in the relationship between positive mood and pain during a laboratory stressor
The Role of Individual Differences in Affective Dynamics
Are there individual difference factors that are likely to be important in affect differentiation, beyond their influences on the experience of pain and stress? In our experimental and longitudinal work, we probed for individual differences in the within-subject correlations between affects, and found evidence that all participants did not show the same pattern of relationships between PA and NA. We concluded that there may be personality differences that account for individual differences in the slopes linking PA and NA (Zautra, Berkhof, & Nicolson, 2002).
The DMA suggests that a decrease in the complexity of information processing during times of stress accounts for the collapse in affective space we observe. To the extent that this simplified processing plays an important role in the shifting relationship between the affects, we would expect that individuals who show a propensity to process information in a less complex fashion to show less differentiation between positive and negative affects, and between affects and pain. Our group investigated this possibility in a cross-sectional study of 112 chronic pain patients with FM (Potter et al., 2000, Study 2). Individuals’ tendency toward cognitive simplicity was assessed with the Response to Lack of Structure subscale (RLS) from the Personal Need for Structure Scale (Neuberg & Newson, 1993). The RLS, which measures individuals’ tendency to overgeneralize and to lack structure in their everyday lives, admittedly provides only a very coarse assessment of the propensity for complex processing. For our purposes, high RLS scores correspond to a tendency toward simpler, less complex information processing. PA and NA were assessed with the PANAS (Watson et al., 1988), and pain was assessed by an item from the SF-36 that rated pain during previous 4 weeks on a 6-point scale, ranging from “none” to “very severe” (McHorney, Ware, Lu, & Sherbourne, 1994). Consistent with our earlier findings, the correlation between PA and NA in the sample as a whole was modest (r = −.21, p = .03).
The central question, though, was whether the correlation between the affects varied depending on cognitive processing style. We examined high and low cognitive simplicity groups, based on a median split of RLS scores, and found that in the low simplicity group (i.e., more complex processing), PA and NA were uncorrelated (r=.01, ns). In contrast, in the high simplicity group (i.e., less complex processing), PA and NA were negatively correlated (r=−.32, p = .02). Moreover, the magnitude of correlations differed significantly between the high/low simplicity groups (Fisher's z test=1.76, p = .04). We have now replicated this finding in a second sample of chronic pain patients (Reich et al., 2001).
The DMA predicts that constrictions in information processing, such as those reflected in cognitive simplicity scores, are likely to affect not only reports of PA and NA, but also affect-related variables, including pain. We therefore explored whether the simplicity effects on affect dynamics extended to pain; that is, was there a stronger relationship between between NA and pain, and between PA and pain, among those high vs. low in cognitive simplicity? The data suggest that the answer is ‘yes’. The correlation between NA and pain was positive and significant for both groups (rs = .34 and .47 for low and high simplicity groups, respectively, ps < .05). Although the magnitude of the correlations was not significantly different, the pattern was in the expected direction. The findings were clearer for the PA-pain relationship. In the low cognitive simplicity group, PA was unrelated to pain (r=.004, ns), whereas in the high simplicity group, PA and pain showed a significant negative correlation (r=−.33, p = .01). The magnitude of the difference in PA-pain correlations between simplicity groups was significant (Fishers z test=1.76, p = .04). Thus, in line with DMA predictions, chronic pain patients who show less cognitive complexity also show less differentiation between PA and NA, and between the affects and pain, than their more cognitively complex counterparts. A more nuanced measure of cognitive complexity, particularly one that better captures on-line processing, may yield a richer picture of its day-to-day impact on adaptation.
Of particular relevance to the ability to sustain affective differentiation are skills related to emotion regulation. We recognize that a number of aspects of emotion regulation are likely to play a role, including the ability to identify, understand, process, and express one's emotions. In our initial exploration, we chose to focus on emotional identification/understanding because arguably it represents an early link in the chain of emotional regulation processes. Based on the DMA, we reasoned that increased skill in understanding their emotions should relate to greater differentiation between NA and PA among individuals in chronic pain. In longitudinal data presented earlier (Zautra et al., 2001, Study 1), we examined whether FM pain patients’ ability to label their own emotions, termed mood clarity (Salovey & Mayer, 1990), related to affect differentiation over time. Recall that participants completed 12 weekly assessments of pain and affect. In addition, prior to weekly assessments, participants provided ratings on the Mood Clarity subscale of the Trait Meta-Mood Scale (Salovey, Mayer, Goldman, Turvey, & Palfai, 1995), which measures the extent to which individuals believe that they are clear about what they are feeling. Higher scores correspond to greater levels of mood clarity. Hierarchical regression analyses including PA, pain, and Mood Clarity as predictors of changes in NA yielded an interaction between PA and Mood Clarity (Beta = .20, p < .01). As expected, higher levels of Mood Clarity were related to weaker associations between PA and NA. Unexpectedly, we did not replicate this pattern in a second sample of pain patients (Zautra et al., 2001, Study 2), indicating that the role of trait levels of emotional understanding in promoting affective differentiation may not be straightforward. Nevertheless, the evidence to this point suggests that individual differences, especially those that have relevance for the complexity of information processing, warrant further investigation as potential moderators of the dynamic interplay between PA and NA.
The DMA and Social Relationships
To this point, we have focused on the effects of stress and uncertainty on individuals’ ability to access information from both positive and negative emotional registers. The DMA, though, also may have implications for our perceptions of the social world. Social engagement derives from needs that arise from both affective systems, such that we seek contact for both enjoyment and alleviation of suffering. During calm periods, we may be exceptionally capable of viewing our social relationships in a nuanced manner, in essence being able to entertain an awareness not only of aspects that are experienced as negative but also those that elicit positive emotional responses. During times of difficulty, however, the negative aspects of a relationship may overshadow its affirming qualities, yielding a more simplified experience of interpersonal relations. Why is the ability to sustain a complex view of social relationships, even during times of stress, likely to be an especially important factor contributing to long-term resilience? Social relationships are key to managing life difficulties, including chronic illness, so that sustained recognition of their positive facets during times of difficulty may both prevent individuals from alienating those in their networks, and allow them to derive benefits from interpersonal connections even in the midst of interpersonal discord.
Recently we began to examine whether the patterns we observed with regard to affective complexity during times of stress hold for social complexity as well. Our initial attempts to explore this issue have focused on comparisons between those experiencing the stress of chronic pain, and healthy controls. Based on the DMA, we expected that chronic pain patients would tend to view their relationships more simply, reflected in higher inverse associations between ratings of relationship support and conflict, compared to controls. In one test of this hypothesis, we examined the relationship between ratings of spouse/partner supportive and dismissive behaviors in a sample of women living with partners. Participants were pain patients who had been diagnosed with OA (n= 75) and/or FM (n=78), and healthy controls (HC: n=45). Perceptions of partner behaviors were obtained from both the participants and their partners with a scale developed by Manne and Zautra (1989). Support behaviors were assessed with items such as “He expressed interest or concern for my well-being,” while those reflecting disregard were assessed with items such as “He was impatient with me.” The version of the questionnaire presented to partners was reworded to indicate that the ratings were meant to reflect their own behavior.
Using multiple-group structural equation modeling, we assessed mean differences on ratings of spouse support and disregard from both respondents. We also examined differences in the relationship between participant ratings of their partners’ support and disregard, as well as between the partners’ ratings of their own support and disregard, across the FM, OA, and HC groups. These analyses showed that the relationship between support and disregard ratings by the participants varied by diagnostic group. Ratings by both FM and OA pain patients were more highly negatively related than were ratings made by healthy controls, after accounting for similarities in ratings from both respondents. Specifically, the residual correlation between support and disregard among FM patients (−.46) and OA patients (−.46) was significantly larger in magnitude than the residual correlation between support and disregard among HCs (−.15). This pattern is in line with our prediction that those stressed by chronic pain view their intimate relationships with less social complexity than do healthy women. Interestingly, the residual covariance between partners’ ratings of their own support and disregard did not differ significantly from zero, regardless of whether they were partnered with pain patients or healthy women. This suggests that living with a chronic pain condition reduces the social complexity of the patients, but not their partners.
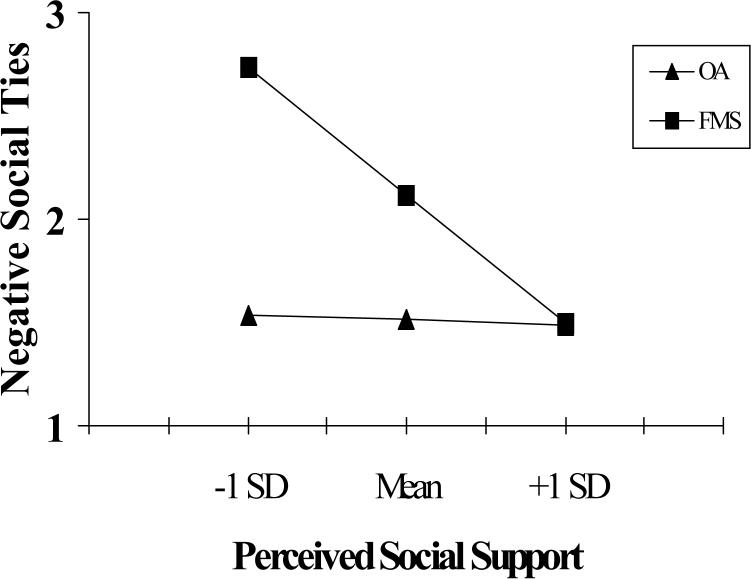
Given the vague nature and unpredictable course of the symptoms in FM, the DMA would predict that these patients are especially vulnerable to perceiving their social networks along a single dimension during times of stress. To examine this possibility, we assessed pain, physical functioning, and social relations in a sample of 50 FM patients, 29 OA patients scheduled for knee replacement surgery, and 22 OA patients with significant pain but not scheduled for surgery (Davis et al., 2001). Information was collected regarding pain level with the Bodily Pain subscale and disability with the Physical Functioning subscale of the SF-36 (Ware, Snow, Kosinski, & Gandek, 1993); social support with a measure developed by Sherbourne and Stewart (1991); and negative social ties with a scale developed by Finch and colleagues (1989). Ratings were made with regard to experiences during the past week for pain and physical functioning measures, and during the past month with regard to social network measures. Comparisons between groups revealed that the FM and OA/surgery groups were comparable in terms of pain level, with both reporting more pain than the OA/Control group. The OA/Surgery group was more disabled than either FM or OA/Control women. With regard to social network ratings, the FM and both OA groups were not different in level of perceived support, although FM patients reported that they experienced more negative social interactions relative to OA/Surgery group (p < .05). More interesting for our current discussion, however, was the relationship between perceived support and negative social ties for the groups, depicted in Figure 2. Regression analyses revealed that the relationship between perceived support and negative social ties among FM patients was strong and negative (Beta = −.64, t=−.57, p < .0001). In contrast, interpersonal stress was unrelated to perceived support in both groups of women with OA (Betas < −.33, ts < −1.56, ps > .14 for both groups). Thus, perceptions of positive and negative social ties were more tightly interwoven in women with FM, even when compared to those in OA/Surgery group with similar levels of pain and even more disability. Two noteworthy limitations in this study were that the data were cross-sectional and social relationships were assessed in general, not allowing the study of specific relationships.
Figure 2.
The interaction of diagnostic group and negative social ties predicting perceived social support in pain patients (Davis, Zautra, & Reich, 2001)
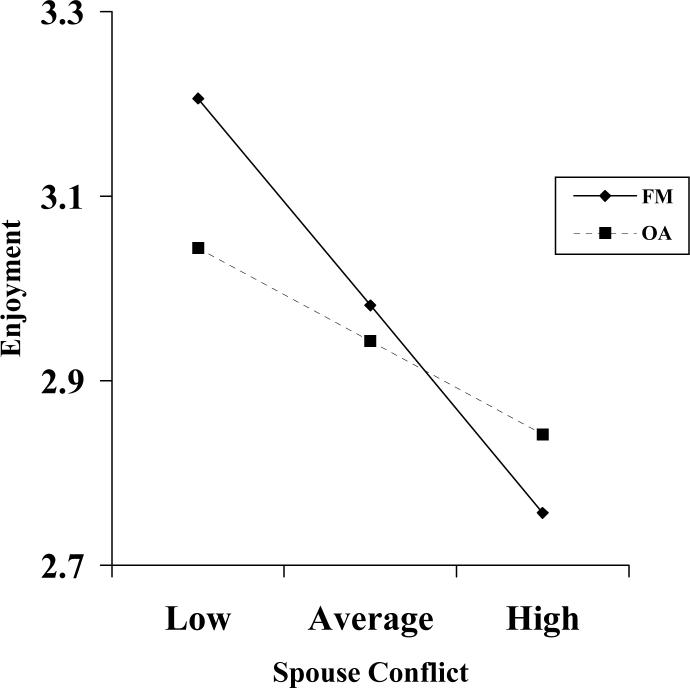
We sought to extend our work on social complexity in FM and OA patients in a subsequent study that contained repeated measures of the occurrence of negative and positive social events, allowing an assessment of within-person associations between interpersonal stress and support over time. To the extent that FM patients live with greater uncertainty due to their illness, they should show a diminished ability to maintain a sense of support during times of interpersonal stress compared to OA patients. Women who had OA (n=38) and/or FM (n=86) and who reported that they were living with a romantic partner were recruited from the community and completed weekly phone interviews for up to 12 weeks. Included among the questions were items gleaned from the Inventory of Small Life Events scale (ISLE: Zautra, Schultz, & Reich, 2000), which assessed the occurrence of positive and negative interpersonal events in each of four relationship domains: spouse/partner, friends, family, and co-workers. Participants also rated the extent to which they felt enjoyment, and a feeling of being loved and cherished during the time they spent in each type of social relationships each week, on a 4-point scale, ranging from “not at all” to “a lot.” We focused our attention on events that occurred with spouses because we believed these would be the most common and important events for women in our sample.
Our hypothesis was tested using hierarchical linear modeling, which enabled us to estimate the relationship between the weekly measures of stress and feelings of support for the average participant, as well as differences between FM and OA groups in the stress-support associations (Bryk & Raudenbush, 1992). We controlled for mean level of conflict with spouse in the prediction of support to remove trait-like stability and examined only state-like fluctuations. We also centered the spouse negative events variable on the mean for each person (Kreft, de Leeuw, & Aiken, 1995).
The results, displayed in Table 1, revealed that FM and OA women experienced similar levels of love and caring from their partners overall, reflected in a nonsignificant effect for diagnosis. Not surprisingly, increases in weekly spouse negative events were related to decreases in perceived levels of partner love and caring. Of relevance for our hypothesis, the interaction between diagnosis and weekly negative spouse events indicated that the inverse relationship between the occurrence of spouse events and feelings of love/caring was stronger for FM relative to OA participants. This interaction is depicted in Figure 3. Consistent with our prediction, when FM patients experienced increased negative events with their partners, they showed larger decreases in feelings of being loved compared to OA patients.
Table 1.
Hierarchical Linear Regression Predicting Weekly Changes in Spouse Support in FM and OA Groups
| Predictor Variable | β | t(df) | p |
|---|---|---|---|
| Dx (FM=1, OA=0) | −.0950 | −1.11(121) | ns |
| Weekly Negative Spouse Events | −.1730 | −2.64(1047) | <.01 |
| DX X Weekly Negative Spouse Events | −.1909 | −2.47(1047) | <.02 |
| Mean Negative Spouse Events | −.5833 | −9.50(121) | <.0001 |
Note. Dx = diagnosis. The model specified an autoregressive covariance matrix, and the weekly negative spouse events variable was centered on the mean for each person and specified as a random effect.
Figure 3.
The interaction of diagnostic group and negative spouse events predicting perceived enjoyment of spouse in pain patients. “High” and “low” represent 1 SD from the mean.
Our findings in pain patients in general, and FM patients in particular, are consistent with predictions based on the DMA that a state of high stress and uncertainty fosters simplified processing of all types of affective information, including aspects of social relationships. Compared to healthy controls, pain patients’ perceptions of the positive and negative features of social relationships were more highly related. Moreover, pain patients who deal with extreme uncertainty, in this case, those with FM, show even more affective simplification in important intimate relationships than do others with more predictable pain. The ability to maintain social complexity may be a key to resilience among those suffering from a chronic pain condition, who rely heavily on their networks for assistance in managing their illness. Given the ubiquity of interpersonal conflict, individuals who are unable to preserve an appreciation of the complexity of their relationships during times of such stress may be in danger of losing their support. Extension of the examination of social complexity in groups dealing with other medical conditions (e.g., cancer) and in normal controls will provide the opportunity for a more thorough evaluation of its meaning and effects.
Although the focus here has been on affective experiences of pain patients themselves, it is possible that caregivers’ ability to sustain affective differentiation will also prove important. In fact, the affective and social complexity of patients’ partners and other important social network members may have profound implications for the affective complexity and adaptation of the pain patient herself. In a recent report, Cameron, Keltner, & John (2003) found that people became more similar over time to roommates and romantic partners in terms of their positive and negative affective experiencing, a process the authors termed “emotional convergence.” We know of no data examining the convergence of affective differentiation in relationships, but there is evidence to suggest that relationship partners do become more similar in terms of their cognitive complexity over time (Burleson & Denton, 1992). Pain patientsm may profit from exposure to caregivers with high levels of cognitive complexity, potentially enhancing their own information processing ability, and ultimately their capacity to preserve affective differentiation during pain and other stressors. Indeed, in seminal work identifying predictors of marital satisfaction over time, Gottman and his colleagues found that it is not the absence of negative interactions that characterize couples who remain happy and stable over time, but rather the presence of ample positive interactions (e.g., Gottman, Coan, Carrere, & Swanson, 1998). To the extent that the affective resources of a spouse or partner can be brought to bear, pain patients themselves may experience added benefits.
Considering Affective Dynamics in Interventions for Chronic Pain
There are a number of implications of the DMA, but the most practical centers on its application to the psychosocial treatment of chronic pain disorders. The most widely used, empirically validated interventions for chronic pain at present are cognitive-behavioral (CBT: Bradley & Alperts, 1999, Rossy et al., 1999). In a recent comprehensive review of the literature on the effectiveness of CBT in arthritis, Nicasscio & Greenberg (2001) found that although CBT is generally beneficial in improving pain management, it has not been shown to influence the affective disturbance of pain patients in most treatment outcome studies. These findings are perhaps not surprising, given that CBT interventions have usually drawn on bipolar models of affect and focused on pain and disability as major therapeutic targets. Typically in CBT, efforts are directed at first increasing patients’ awareness of their automatic, maladaptive thoughts, and then changing those thoughts through disputation, reframing, and reappraisal.
Yet if simplified processing of affectively-laden information contributes to poor adaptation in the face of pain and other stressors, then intervention efforts directed at enhancing individuals’ ability to process affect with greater complexity may prove useful, especially during times of pain and stress when NA tends to dominate. One such approach, centering on the use of mindfulness meditation, has been garnering empirical support over the past decade for the treatment of pain and prevention of depression relapse (Kabat-Zinn, Lipworth, & Burney, 1985; Segal, Williams, & Teasdale, 2002; Teasdale et al., 2002). Mindfulness techniques are designed to increase conscious attention to and nonjudgmental acceptance of one's thoughts and feelings. This approach encourages effortful processing of mental events, in contrast to the automatic processing that occurs during pain and other stressors. When a difficult or painful experience emerges, individuals are encouraged to attend to this experience with deliberateness, and to hold it in awareness with an accepting, nonjudgmental frame of mind. Similar to traditional CBT, dysfunctional thought patterns are identified. But rather than promoting attempts to neutralize such thoughts through the processes of reframing and reappraisal, a mindful approach promotes detached observation. The goal is to develop the ability to recognize negative thoughts, feelings, and sensations as momentary objects of awareness, and to foster the recognition that thoughts are not facts but rather interpretations of events that reflect a variety of influences, including past learning and current mood states.
An optimal outgrowth of a mindful treatment approach for those in chronic pain would be an increase in their emotional complexity, such that they would be able to sustain access to positive affective resources. During times of pain and stress when positive and negative affect are strongly related, the ability to continue to laugh and experience pleasure may leave less room for the powerful negative emotions that can seem so overwhelming. During times of low pain and stress when positive and negative affect represent separate dimensions, the ability to enhance positive emotions could serve to “broaden and build” the resources for coping with flare-ups of pain and increase overall life satisfaction (Fredrickson, 1998). Developing a variety of supportive relationship and sources of pleasure could prove invaluable in sustaining an individual through a major health crisis.
Recent evidence gleaned from healthy individuals points to substantial neurophysiological changes with mindfulness training that are consistent with a “broadening” of positive affective resources. Davidson and colleagues (2003) assessed patterns of brain electrical activity in response to positive and negative emotion induction in a group of 41 healthy adults randomly assigned to either participation in an 8-week mindfulness meditation training program or a wait-list control group, with assessments occurring at both pre- and post-intervention. The authors posited that those assigned to mindfulness meditation would show increased left-sided activation, a pattern associated with increased positive affectivity. The findings were consistent with this prediction. The mindfulness group had greater relative left-sided brain activation post-treatment in general and in response to both the positive and negative mood inductions, compared to the wait-list control group.
Of particular relevance for our discussion of affective dynamics in chronic pain are the increases in left-sided activation that occurred in response to the experience of negative emotion among those trained to increase awareness and acceptance of internal experiences, including their emotions. These findings suggest that an intervention that enhances emotional skills may increase the ability of those with chronic pain conditions to preserve positive engagement during their experience of pain and stress, and to respond to these negative events more adaptively by finding positive emotional features embedded within the negative (Zautra, 2003, pp. 124−131). Although a mindfulness meditation intervention has been applied to the treatment of chronic pain and other medical conditions (e.g, Kabat-Zinn et al., 1985), its effect on affective dynamics in these populations has yet to be explored. As findings accumulate from controlled studies that include appropriate control groups, any distinct benefits of mindfulness interventions should be brought into sharper focus. Our research team is in the midst of a clinical trial of rheumatoid arthritis patients to examine the impact of a mindfulness-based intervention on aspects of resilience, including affective complexity.
Given the importance of social relationships to health and well-being, a tendency to perceive network members in a more simplified way during pain and stress could be problematic for pain patients. It may lead them to ignore potential sources of positive engagement, or to alienate supportive ties during times of greatest need. What types of interventions could enhance the social complexity of pain patients? Certainly treatments that target patients’ emotional complexity, including mindful techniques, should influence social information processing as well. Advantages might also accrue, though, from an expanded therapeutic focus that includes the emotional differentiation skills of key members of the patients’ network. Like other medical conditions, chronic pain affects the lives of not only patients themselves, but also of their loved ones (Turk, Kerns, & Rosenberg, 1992). A patient's pain or its absence may come to dominate the family's emotional life, often leaving both patients and caregivers with a sense of helplessness and distress. Involving important family members in the treatment of chronic pain patients is not a novel approach (e.g., Kerns, Otis, & Wise, 2002; Keefe et al., 1999; Martire et al., 2003), but typically these interventions have maintained a focus on the patient as the primary target; family members are enlisted to support the cognitive and behavioral pain management strategies of the patients themselves.
We suggest that a treatment explicitly targeting the affective complexity of both patients and their caregivers may have additional benefit, particularly in instances where the pain and problems associated with it have been impervious to other treatments. An increased ability of caregivers to maintain their own emotional differentiation should make them better able to sustain positive affective engagement with the patient even during times of pain or conflict. Recent developments in approaches to marital therapy might be relevant here, where emphasis on acceptance of and detachment from unsolvable problems is highlighted as a means to establish greater intimacy and satisfaction (Jacobsen, Christensen, Prince, Cordova, & Eldridge, 2000).
Potential Applications of the DMA to Other Health Problems
Thusfar, we have focused on affective dynamics in the context of managing chronic pain, but the DMA also is likely to be relevant to other health problems where a lack of ability to maintain affective differentiation contributes to the development or worsening of illness-related symptoms. Substance abuse represents a major health issue that can be viewed through the lens of the DMA. Intoxicating substances serve many purposes, and most prominent among them is emotion regulation. Both reduction of social anxiety and other negative affective states, and amplification of positive states have been shown to motivate substance use (Swendsen et al., 2000). Zautra (2003) proposed that one of the unintended consequences of overuse/abuse/dependency may be a transformation of the affective consequences in the direction of increasing simplicity. The substance itself, over time, increasingly functions as a stressor, provoking a narrowing of affective space. An individual may find him/herself in an either/or state, depending upon the degree to which the “need” for the substance is satisfied.
Successful programs such as Alcoholics Anonymous and motivational interviewing (Miller & Rollnick, 2002) may act by reopening the mind to an awareness of the social and emotional complexities involved in substance use as well as social engagement. Using a dynamic model of affect complexity may further the development of emotion and motivation based interventions for those suffering from problems of substance use and abuse. Motivational interviewing has been a particularly effective approach for building a genuine motivation on the part of a substance abuser to change and engage in treatment (Miller & Rollnick, 2002). A central technique is called “decisional balance” in which the therapist/counselor encourages the abuser to fully consider all of the advantages and disadvantages of his/her behavior. Affective differentiation or mindfulness could be very useful in helping the individual access memories of the full range of positive and negative affects and experiences associated with taking the substance. Fully accessing the positive helps to identify the barriers to engaging treatment and helps prevent relapse. Fully accessing the negative provides a more obvious avoidance motivation. Developing an appreciation of both positive and negative affective experiences may increase cognitive complexity and motivation to escape the negative consequences of substance abuse and approach the positive consequences of other forms of enjoyment. Our application of the DMA to current treatment strategies for substance abuse remain speculative, however, until explicit tests of hypotheses derived from the model are carried out in these groups.
The DMA and its extension to include social complexity may also be a useful heuristic for understanding increased risk of coronary heart disease (CHD) associated with a hostile disposition (Miller, Smith, Turner, Guijarro, & Hallet,1996). One of the mechanisms proposed to explain the CHD-hostility association focuses on the propensity of hostile individuals to exhibit exaggerated or prolonged behavioral and physiological reactivity to environmental stressors compared with their nonhostile counterparts. Yet hostile individuals are not overly reactive to all types of events; rather, they seem especially responsive to interpersonal events (Suls & Wan, 1993), even when those interpersonal exchanges are rather benign (e.g., Davis, Matthews, & McGrath, 2000). According to Beck (1999), hostile individuals have developed easily accessible cognitive schemas that prepare them to be wary and suspicious in interpersonal situations. In essence, these individuals would be characterized by an inability to maintain social complexity during their interpersonal encounters. In these contexts, their information processing becomes simplified such that they tend to interpret others’ behavior as personally threatening. The acute experience of threat leads to heightened physiological and affective arousal and, we would argue, affective simplification as well. Under such circumstances, there is little possibility that hostile individuals would experience the positive affect that is fundamental to sustaining close social ties and well-being. Although CBT interventions have proven helpful in ameliorating anger-proneness and some of its health consequences (Beck & Fernandez, 1998), there may be benefit from expanding the focus of treatment to include targeting affective differentiation, especially in social contexts, in a manner that increases access to positive social engagement for these vulnerable individuals.
Caveats and Future Directions
In this article, we have provided evidence in support of the proposition that in the context of pain and other stressors, informational space contracts such that NA and PA registers collapse to form a single dimension. Moreover, the stress-related changes in affective differentiation appear to extend to the construal of affective dimensions of social relationships in pain patients. A host of questions remain, however. One issue involves generalizability. Although our data were gathered using both field and laboratory approaches, varied measures of pain and affect, and diverse time fames, all of our samples have been comprised of predominantly white female participants from western cultures. Whether the DMA applies to chronic pain groups from other social and/or cultural backgrounds needs to be demonstrated. For example, because some eastern cultures view emotions in a dialectical way that juxtaposes seemingly conflicting feelings (Schimmack, Oishi, & Diener, 2002), individuals reared in such environments may be inured to stress- or pain-related changes in affective space.
Although we predicted and observed less affective differentiation in FM relative to OA patients, a number of differences between these pain groups could account for the findings. We have speculated that greater unpredictability and uncertainty regarding their illness make FM patients especially vulnerable, but have not yet explicitly tested this hypothesis. Moreover, FM patients tend to differ from OA patients along other dimensions that may have implications for affective complexity, including depressive symptoms, leaving open the possibility that differences other than aspects of the pain syndrome itself may account for the pattern of findings.
Also the nature and extent of individual differences in affective and social complexity have yet to be determined. We have discussed evidence suggesting that aspects of cognitive simplicity and lack of mood clarity may be two factors that increase vulnerability to affective simplification during times of stress, but other candidates are certainly viable. Likewise, there are likely to be individual differences in the ability to sustain social differentiation during difficult times, with hostility being but one example. Finally, empirical tests of the application of the DMA to health conditions other than pain where affect regulation plays an important role are also likely to be fruitful, including such conditions as cancer, asthma, diabetes, and obesity.
The DMA offers new ways to examine health-related effects of emotion by proposing a new integration of stress and emotion in our daily lives. This approach offers a set of testable hypotheses governing how emotions set the stage for good and also poor health. Stressful situations appear to magnify the influence of positive emotions not only on healthy behaviors, but also on neuro-immune processes that restore physiological balance following disturbing events. The ability to maintain affective complexity in the face of life's inevitable difficulties, including challenges to health, may be a hidden key to resilience across the lifespan. We hope that our work encourages future research using cutting edge approaches to increase our understanding of this exceedingly complex domain of human functioning.
Footnotes
All z-tests of differences were conducted for dependent correlations in within-subject comparisons, and for independent correlations in between-subject comparisons.
References
- Banks SM, Kerns RS. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin. 1996;119:95–110. [Google Scholar]
- Beck AT. Prisoners of hate: The cognitive basis of anger, hostility, and violence. Harper Collins; New York, NY: 1999. [Google Scholar]
- Beck R, Fernandez E. Cognitive-behavioral therapy in the treatment of anger: A meta-analysis. Cognitive Therapy and Research. 1998;22:63–74. [Google Scholar]
- Bradley LA, Alperts KR. Psychological and behavioral approaches to pain management for patients with rheumatic disease. Rheumatic Disease Clinics of North America. 1999;25:215–232. doi: 10.1016/s0889-857x(05)70061-2. [DOI] [PubMed] [Google Scholar]
- Bryk. AS, Raudenbush SW. Hierarchical linear models: Applications and data analyses methods. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Burleson BR, Denton WH. A new look at similarity and attraction in marriage: Similarities in social-cognitive and communication skills as predictors of attraction and satisfaction. Communication Monographs. 1992;59:268–287. [Google Scholar]
- Cacioppo JT, Bernston GG. Relationship between attitudes and evaluative space: A critical review, with emphasis on the separability of positive and negative substrates. Psychological Bulletin. 1994;115:401–423. [Google Scholar]
- Cacioppo JT, Gardner WL, Bernston GG. The affect system has parallel and integrative processing components: Form follows function. Journal of Personality and Social Psychology. 1999;76:839–855. [Google Scholar]
- Cameron A, Keltner D, Oliver JP. Emotional convergence between people over time. Journal of Personality and Social Psychology. 2003;84:1054–1068. doi: 10.1037/0022-3514.84.5.1054. [DOI] [PubMed] [Google Scholar]
- Canli T, Desmond JE, Zhao Z, Glover G, Gabrieli JD. Hemispheric asymmetry for emotional stimuli detected with fMRI. Neuroreport. 1998;9:3233–3239. doi: 10.1097/00001756-199810050-00019. [DOI] [PubMed] [Google Scholar]
- Canli T, Zhao Z, Desmond JE, Kang E, Gross J, Gabrieli JD. An fMRI study of personality influences on brain reactivity to emotional stimuli. Behavioral Neuroscience. 2001;115:33–42. doi: 10.1037/0735-7044.115.1.33. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Jackson CD, Kalin NH. Emotion, plasticity, context and regulation: Perspectives from affective neuroscience. Psychological Bulletin. 2000;126:890–909. doi: 10.1037/0033-2909.126.6.890. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Davis MC, Matthews KA, McGrath CE. Hostile attitudes predict elevated vascular resistance during interpersonal stress in men and women. Psychosomatic Medicine. 2000;62:17–25. doi: 10.1097/00006842-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Reich JW. Vulnerability to stress among women in chronic pain from fibromyalgia and osteoarthritis. Annals of Behavioral Medicine. 2001;23:215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- Feldman Barrett L, Russell JA. Independence and bipolarity in the structure of affect. Journal of Personality and Social Psychology. 1998;74:967–984. [Google Scholar]
- Fernandez E, Turk DC. Sensory and affective components of pain: Separation and synthesis. Psychological Bulletin. 1992;112:205–212. doi: 10.1037/0033-2909.112.2.205. [DOI] [PubMed] [Google Scholar]
- Finch JF, Okun MA, Barrera M, Zautra AJ, Reich JW. Positive and negative social ties among older adults: measurement models and the prediction of psychological stress and well-being. American Journal of Community Psychology. 1989;17:585–605. doi: 10.1007/BF00922637. [DOI] [PubMed] [Google Scholar]
- Gable SL, Reis HT, Elliot AJ. Behavioral activation and inhibition in everyday life. Journal of Personality and Social Psychology. 2000;78:1135–1149. doi: 10.1037//0022-3514.78.6.1135. [DOI] [PubMed] [Google Scholar]
- Goldstein MD, Strube MJ. Independence revisited: The relation between positive and negative affect in a naturalistic setting. Personality and Social Psychology Bulletin. 1994;20:57–64. [Google Scholar]
- Gottman JM, Coan J, Carrere S, Swanson K. Predicting marital happiness and stability from newlywed interactions. Journal of Marriage and the Family. 1998;60:5–22. [Google Scholar]
- Green DP, Salovey P, Truax KM. Static, dynamic, and causative bipolarity of affect. Journal of Personality and Social Psychology. 1999;76:856–867. doi: 10.1037//0022-3514.76.5.856. [DOI] [PubMed] [Google Scholar]
- Hart RP, Wade JB, Martelli MF. Cognitive impairment in patients with chronic pain: The significance of stress. Current Pain and Headache Reports. 2003;7:116–226. doi: 10.1007/s11916-003-0021-5. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: An acceptance-based, promising new treatment for couple discord. Journal of Consulting and Clinical Psychology. 2000;68:351–355. doi: 10.1037//0022-006x.68.2.351. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, Beaupre P, Weisberg J, Helms M. Spouse-assisted coping skills in training in the management of knee pain in osteoarthritis: Long-term followup results. Arthritis Care and Research. 1999;12:101–111. doi: 10.1002/1529-0131(199904)12:2<101::aid-art5>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Otis JD, Wise EA. Treating families of chronic pain patients: Application of a cognitive-behavioral transactional model. In: Turk DC, editor. Psychological approaches to pain management: A practitioners’ handbook. 2nd ed. Guilford Press; New York, NY: 2002. pp. 256–275. [Google Scholar]
- Kreft IG, de Leeuw J, Aiken LS. The effect of different forms of centering in hierarchical linear models. Multivariate Behavioral Research. 1995;30:1–21. doi: 10.1207/s15327906mbr3001_1. [DOI] [PubMed] [Google Scholar]
- Larsen R, Diener E. Promises and problems with the circumplex model of emotion. In: Clarke MS, editor. Emotion. Sage; Newbury Park, CA: 1992. pp. 25–59. [Google Scholar]
- Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, Heyse SP, Hirsch R, Hochberg MC, Hunder GG, Liang MH, Pillemer SR, Steen VD, Wolfe F. Estimates of the prevalence of arthritis and selected muscluloskeletal disorders in the United States. Arthritis and Rheumatism. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Lefebvre JC, Keefe FJ, Affleck G, Raezer LB, Starr K, Caldwell DS, Tennen H. The relationship of arthritis self-efficacy to daily pain, daily mood, and daily pain coping in rheumatoid arthritis patients. Pain. 1999;80:425–435. doi: 10.1016/s0304-3959(98)00242-5. [DOI] [PubMed] [Google Scholar]
- Linville PW. Self-complexity and affective extremity: Don't put all your eggs in one basket. Social Cognition. 1985;3:94–120. [Google Scholar]
- Linville PW. Self-complexity as a cognitive buffer against illness and depression. Journal of Personality and Social Psychology. 1987;62:663–676. doi: 10.1037//0022-3514.52.4.663. [DOI] [PubMed] [Google Scholar]
- Manne S, Zautra AJ. The effects of spouse critical remarks on psychological adjustment in rheumatoid arthritis. Journal of Personality and Social Psychology. 1989;56:608–617. doi: 10.1037//0022-3514.56.4.608. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Keefe FJ, Starz TW, Osial TA, Dew JR, Reynolds CF. Feasibility of a dyadic intervention for management of osteoarthritis: A pilot study with older patients and their spousal caregivers. Aging and Mental Health. 2003;7:53–60. doi: 10.1080/1360786021000007045. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Lu JFR, Sherbourne CD. The MOS 36-itme short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patients groups. Medical Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Melzak R, Wall. PD. Pain mechanisms: A new theory. Science. 1965;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing for change. 2nd Ed. Guilford Press; New York: 2002. [Google Scholar]
- Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. A meta-analytic review of research on hostility and physical health. Psychological Bulletin. 1996;119:22–48. doi: 10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- Neuberg SL, Newson JT. Personal need for structure: Individual differences in the desire for simple structure. Journal of Personality and Social Psychology. 1993;65:113–131. [Google Scholar]
- Nicassio PM, Greenberg MA. The effectiveness of cognitive –behavioral and psychoeducational interventions in the management of arthritis. In: Weisman MH, Weinblatt M, Louie J, editors. Treatment of rheumatic diseases. 2nd ed. William Saunders; Orlando: 2001. pp. 147–161. [Google Scholar]
- Ploghaus A, Tracey I, Gati JS, Clare S, Manon RS, Matthews PM, Rawlins JN. Dissociating pain from its anticipation in the human brain. Science. 1999;284:1979–1981. doi: 10.1126/science.284.5422.1979. [DOI] [PubMed] [Google Scholar]
- Potter PT, Zautra AJ, Reich JW. Stressful events and information processing dispositions moderate the relationship between positive and negative affect: Implications for pain patients. Annals of Behavioral Medicine. 2000;22:1002–1012. doi: 10.1007/BF02895113. [DOI] [PubMed] [Google Scholar]
- Paulhus DL, Lim DTK. Arousal and evaluative extremity in social judgments: A dynamic complexity model. European Journal of Social Psychology. 1994;24:89–99. [Google Scholar]
- Reich JW, Zautra AJ. Arousal and the relationship between positive and negative affect: An analysis of the data of Ito, Cacioppo, and Lang (1998). Motivation and Emotion. 2002;26:209–222. [Google Scholar]
- Reich JW, Zautra AJ, Potter PT. Cognitive structure and the independence of positive and negative affect. Journal of Social and Clinical Psychology. 2001;20:99–115. [Google Scholar]
- Reich JW, Zautra AJ, Davis M. Dimensions of affect relationships: Models and their integrative implications. Review of General Psychology. 2003;7:66–83. [Google Scholar]
- Rossy LA, Buckelew SP, Dorr N, Hagglund KJ, Thayer JF, McIntosh MJ, Hewett JE, Johnson JC. A meta-analysis of fibromyalgia treatment interventions. Annals of Behavioral Medicine. 1999;21:180–191. doi: 10.1007/BF02908299. [DOI] [PubMed] [Google Scholar]
- Russell JA, Carroll JM. On the bipolarity of positive and negative affect. Psychological Bulletin. 1999;125:3–30. doi: 10.1037/0033-2909.125.1.3. [DOI] [PubMed] [Google Scholar]
- Sackheim HA, Weber SL. Functional brain symmetry in the regulation of emotion: Implication for bodily manifestations of stress. In: Goldberger L, Breznitz S, editors. Handbook of stress: Theoretical and clinical aspects. Free Press; New York: 1982. pp. 183–199. [Google Scholar]
- Salovey P, Mayer JD. Emotional intelligence. Imagination, Cognition and Personality. 1990;9(3):185–211. [Google Scholar]
- Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. In: Pennebaker JW, editor. Emotion, disclosure, and health. American Psychological Association; Washington, DC: 1995. pp. 125–154. [Google Scholar]
- Schimmack U, Oishi S, Diener E. Cultural influences on the relation between pleasant emotions and unpleasant emotions: Asian dialectic philosophies or individualism-collectivism? Cognition and Emotion. 2002;16:705–719. [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart A. The MOS social support survey. Social Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Suls J, Wan CK. The relationship between trait hostility and cardiovascular reactivity: a quantitative review and analysis. Psychophysiology. 1993;30:615–626. doi: 10.1111/j.1469-8986.1993.tb02087.x. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: An experience sampling test of the self-medication hypothesis. Journal of Abnormal Psychology. 2000;109:198–204. [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Turk DC, Kerns RD, Rosenberg R. Effects of marital interaction on chronic pain and disability: Examining the down side of social support. Rehabilitation Psychology. 1992;37:259–274. [Google Scholar]
- Ursin H, Olff M. The stress response. In: Stanford SC, Solomon P, editors. Stress: From synapse to syndrome. Academic Press; New York: 1993. pp. 4–23. [Google Scholar]
- Ware JE, Jr., Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and interpretation guide. The Health Institute, New England Medical Center; Boston: 1993. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Wiese D, Vaidya J, Tellegen A. The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. Journal of Personality and Social Psychology. 1999;76:820–838. [Google Scholar]
- Zautra AJ. Emotions, stress, and health. Oxford University Press; New York: 2003. [Google Scholar]
- Zautra AJ, Berkhof J, Nicolson NA. Changes in affect interrelationships as a function of stressful events. Cognition and Emotion. 2002;16:309–318. [Google Scholar]
- Zautra ZJ, Guarnaccia CA, Dohrenwend BP. Measuring small life events. American Journal of Community Psychology. 1986;14:629–655. doi: 10.1007/BF00931340. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Potter PT, Reich JW. The independence of affects is conext-dependent: An integrative model of the relationship between positive and negative affect. In: Schaie KW, Powell M, editors. Annual Review of Gerontology. Vol. 17. Springer; New York: 1997. pp. 75–103. [Google Scholar]
- Zautra AJ, Reich JW, Davis MC, Potter PT, Nicolson NA. The role of stressful events in the relationship between positive and negative affects: Evidence from field and experimental studies. Journal of Personality. 2000;68:927–951. doi: 10.1111/1467-6494.00121. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Schultz AS, Reich JW. The role of everyday events in depressive symptoms for older adults. In: Williamson GM, Parmelee PA, Shaffer DR, editors. Physical illness and depression: A handbook of theory, research, and practice. Plenum; New York: 2000. pp. 65–92. [Google Scholar]
- Zautra A, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: Applications of a dynamic model of affect. Journal of Consulting and Clinical Psychology. 2001;69:786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]