Abstract
OBJECTIVE—Hyperglycemia-induced inflammation is central in diabetes complications, and monocytes are important in orchestrating these effects. Toll-like receptors (TLRs) play a key role in innate immune responses and inflammation. However, there is a paucity of data examining the expression and activity of TLRs in hyperglycemic conditions. Thus, in the present study, we examined TLR2 and TLR4 mRNA and protein expression and mechanism of their induction in monocytic cells under high-glucose conditions.
RESEARCH DESIGN AND METHODS—High glucose (15 mmol/l) significantly induced TLR2 and TLR4 expression in THP-1 cells in a time- and dose-dependent manner (P < 0.05). High glucose increased TLR expression, myeloid differentiation factor 88, interleukin-1 receptor–associated kinase-1, and nuclear factor-κB (NF-κB) p65-dependent activation in THP-1 cells. THP-1 cell data were further confirmed using freshly isolated monocytes from healthy human volunteers (n = 10).
RESULTS—Pharmacological inhibition of protein kinase C (PKC) activity and NADPH oxidase significantly decreased TLR2 and TLR4 mRNA and protein (P < 0.05). Knocking down both TLR2 and TLR4 in the cells resulted in a 76% (P < 0.05) decrease in high-glucose–induced NF-κB activity, suggesting an additive effect. Furthermore, PKC-α knockdown decreased TLR2 by 61% (P < 0.05), whereas inhibition of PKC-δ decreased TLR4 under high glucose by 63% (P < 0.05). Small inhibitory RNA to p47Phox in THP-1 cells abrogated high-glucose–induced TLR2 and TLR4 expression. Additional studies revealed that PKC-α, PKC-δ, and p47Phox knockdown significantly abrogated high-glucose–induced NF-κB activation and inflammatory cytokine secretion.
CONCLUSIONS—Collectively, these data suggest that high glucose induces TLR2 and -4 expression via PKC-α and PKC-δ, respectively, by stimulating NADPH oxidase in human monocytes.
The major cause of death in type 1 and type 2 diabetic patients is atherosclerosis (1–3). The pathogenesis of the accelerated atherosclerosis is multifactorial. Inflammation is pivotal in the development of atherosclerosis. Recent studies have shown that diabetes is a proinflammatory state (4–6). We and others have shown that the proinflammatory phenotype in diabetes is characterized by elevated plasma C-reactive protein (CRP), cytokines, chemokines, adhesion molecules, monocytic activity, etc. (4–6). Hyperglycemia contributes to vascular complications of diabetes. High glucose has been shown to induce inflammatory cytokines, chemokines, p38 mitogen-activated protein kinase, reactive oxygen species (ROS), protein kinase C (PKC), and nuclear factor-κB (NF-κB) activity in both clinical and experimental systems (7–12). Several lines of evidence support a role for oxidative stress in the development of diabetes complications (13,14). Diabetic patients have increased O2− production in monocytes and neutrophils (8,13,15); however, the mechanism of the interactions among these mediators remain unclear.
Toll-like receptors (TLRs) recognize conserved pathogen-associated molecular patterns and induce innate immune responses that are essential for host defenses (16). TLRs are activated by both endogenous and exogenous agonists of microbial and nonmicrobial origin. TLR activation by their agonists triggers a signaling cascade, leading to cytokine production and initiation of an adaptive immune response (17). TLR expression is increased in a plethora of inflammatory disorders, including atherosclerosis and diabetes (18–20). Some of the endogenous ligands for TLR2 and TLR4 include high-mobility group B1, biglycan, hyaluronic acid fragments, necrotic cells, serum amyloid A, advanced glycation end products, and extracellular matrix components (18). Among the TLRs, TLR2 and TLR4 play an important role in atherosclerosis. TLR2 and TLR4 bind to components of the Gram-positive and -negative bacteria, respectively (17). They are expressed in multiple cells and tissues, primarily in monocytes. TLR2 and TLR4 expression is increased in atherosclerotic plaque macrophages and in animal models of atherosclerosis (21–25). Plaques of TLR4 knockout mice on a high-fat diet show reduced lesion size, lipid content, and macrophage infiltration (22). TLR2/LDLR−/− and TLR2/ApoE−/− double knockout mice are protected from the development of atherosclerosis (24). In addition, total loss of myeloid differentiation factor 88 (MyD88), a common adapter molecule of TLR2 and TLR4 in the cell, results in reduced plaque size, lipid content, inflammation, and plasma interleukin (IL)-1 and tumor necrosis factor-α (TNF-α) (25).
The interactions among inflammation, hyperglycemia, and diabetes have clear implications for the immune system. Mohammad et al. (26) reported increased TLR2 and TLR4 expression in type 1 diabetic NOD mice, correlating with increased NF-κB activation in response to endotoxin, and increased proinflammatory cytokines. Kim et al. (27) using TLR2−/−, TLR4−/− knockouts, and NOD mice have demonstrated that TLR2 senses β-cell death and contributes to the instigation of autoimmune diabetes. Devaraj et al. (20) showed increased TLR2 and TLR4 expression, intracellular signaling, and TLR-mediated inflammation in monocytes with significant correlation to A1C levels in type 1 diabetic patients. Also, Song et al. (28) reported increased TLR4 mRNA expression in differentiating adipose tissue of db/db mice. Creely et al. (29) showed increased TLR2 expression in the adipose tissue of type 2 diabetic patients with strong correlates to endotoxin levels. These observations taken together suggest a potential role for TLR2 and TLR4 in the pathology of diabetes with limited mechanistic details.
However, data examining the mechanism of increased TLR2 and TLR4 expression in diabetes are unknown. Therefore, this study aimed to test the ability of high glucose, one of the key abnormalities of the diabetic condition, to induce TLR expression in human monocytes.
RESEARCH DESIGN AND METHODS
Reagents.
THP-1 human monocytic cell line was obtained from American Type Culture Collection (Manassas, VA). All of the reagents, buffers, antibodies, and small interfering RNAs (siRNAs) used in the study and methods are detailed and available in an online appendix at http://dx.doi.org/10.2337/db08-0564.
Cell culture.
THP-1 cells were subcultured in endotoxin-free RPMI as described previously in detail (15,30). We monitored the endotoxin levels in the culture media and reagents (glucose, mannitol, etc.) using Limulus Amoebocyte Lysate Assay (Cambrex, Milwaukee, MI), and the average endotoxin level was <100 EU/ml consistently in all of the experiments, because any endotoxin contamination interferes with accurate TLR2 and TLR4 quantitation (20,30).
Treatments.
Cells were cultured (1 × 106 cells/ml) for 3 days in 5.5 mmol/l (normal glucose) or for indicated time points with 10–25 mmol/l glucose, and as an osmotic control, 9.5–14.5 mmol/l mannitol was added along with normal glucose with daily changes in media. Cell viability, as determined by trypan blue exclusion, was >90%. In addition, cells were pretreated for 2 h with inhibitors followed by 24 h with normal and high glucose (15 mmol/l) (15,30). Cell supernatants, lysates, and RNA were collected for enzyme-linked immunosorbent assay (ELISA), Western blotting, and RT-PCR, respectively.
Fluorescence-activated cell sorter analysis of TLR2 and TLR4.
TLR2 and TLR4 expressions were determined using flow cytometry as described previously (20). Briefly, after treatment with high glucose, cells were incubated with anti-human TLR2 and TLR4 antibodies or isotype-matched IgG controls and were analyzed with BD FACS Array Bioanalyzer (BD Biosciences, San Jose, CA). Results are expressed as mean fluorescence intensity units (MFI)/105 cells. The intra- and interassay coefficient of variation (CV) were determined to be <10%.
RNA extraction and RT-PCR.
RNA was isolated from the monocytes using TRI reagent (Invitrogen, Carlsbad, CA) reagent. RT-PCR was performed using TLR2, TLR4, and 18s RNA primers (Invivogen, San Diego, CA) following the manufacturer's cycling parameters. Band intensities were determined using Image Quant Software (GE Healthcare Biosciences, Piscataway, NJ) as described previously (20). For real-time RT-PCR, primer probe sets were purchased from Superarray Bioscience (Gaithersburg, MD). Data were calculated using the 2−ΔΔCT method and are presented as fold induction of transcripts for the TLR gene normalized to 18s in cells treated with high glucose (30,31).
ELISA.
IL-1β, IL-6, monocyte chemoattractant protein-1 (MCP-1), and TNF-α were measured in the supernatants of monocytes by ELISA (R&D Systems, Minneapolis, MN), as reported previously (30). The intra- and interassay CV was between 7 and 10% for all of the assays.
Immunoprecipitation and Western blots.
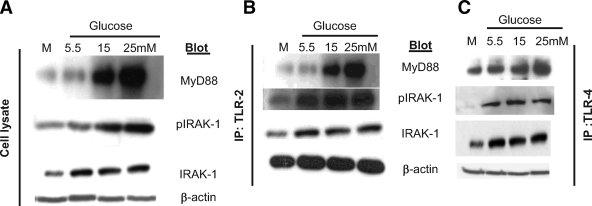
Cell lysates (100 μg) were immunoprecipitated with anti-TLR2 antibody or anti-TLR4 antibody (eBioscience) overnight at 4°C with gentle rocking. Immune complexes were resolved, transferred, and probed with phospho- and total antibodies as indicated in Fig. 3. Stripped membranes were further incubated with β-actin. Representative blots from four different experiments are presented.
FIG. 3.
A: Representative Western blot depicting the effect of high glucose on MyD88 and IRAK-1 phosphorylation in THP-1 cells. After culturing cells with high glucose, cells were lysed, and cell lysates were blotted for MyD88, total and phospho–IRAK-1, and β-actin as described in research design and methods (n = 4). B: Representative Western blot showing enhanced expression of MyD88, IRAK-1, and pIRAK-1 in THP-1 cell lysates immunoprecipitated with TLR2 antibody after high-glucose challenge as detailed in research design and methods. β-Actin was used as a loading control, n = 4 experiments. C: Representative Western blot showing enhanced expression of MyD88, IRAK-1, and pIRAK-1 in THP-1 cell lysates immunoprecipitated with TLR4 antibody after high-glucose challenge as detailed in research design and methods. β-Actin was used as a loading control, n = 4 experiments.
siRNA transfection assays.
Prevalidated siRNAs were obtained from Ambion, and transfection assays were performed as described previously (30,32) following the manufacturer's instructions, with suitable vehicle and scrambled siRNA controls, and subsequently treated with high glucose (15 mmol/l) for 24 h.
NF-κB transcription factor and PKC activity assays.
NF-κB p65 DNA binding activity in the high-glucose–treated nuclear extracts of monocytes and PKC activity in cytosolic fraction were determined using the nonradioactive TransAM transcription factor assay (Active Motif, Carlsbad, CA) and immunoassays (Stressgen, Ann Arbor, MI), respectively, as described in detail previously (30) following the manufacturer's instructions. The intra- and interassay CV for these assays was <7–10%.
Luciferase reporter gene assays for TLR2 and TLR4.
Assays were performed as described previously (33,34). Briefly, 293T cells were cotransfected with TLR4 and MD2 expression plasmids or TLR2 and TLR1 or TLR6 expression plasmids, a luciferase plasmid containing NF-κB(2x)-binding site, and β-galactosidase plasmid and corresponding empty vectors as controls using SuperFect transfection reagent (Qiagen, Valencia, CA), following the manufacturer's instructions. Transfected cells were treated with high glucose or synthetic TLR ligands for 15 h before lysis. Luciferase and β-galactosidase enzyme activities were determined using the Promega Luciferase Assay System and β-Galactosidase Enzyme System (Promega, Madison, WI). Luciferase activity was normalized by β-galactosidase activity to correct the transfection efficiency.
Statistical analysis.
Results of the experimental studies are reported as means ± SD. Differences were analyzed by ANOVA with appropriate post hoc analyses. A probability value of P < 0.05 was considered significant. All statistical analyses were performed using GraphPad Prizm Software (San Diego, CA).
RESULTS
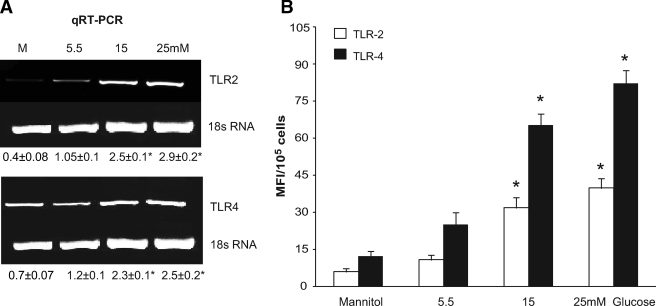
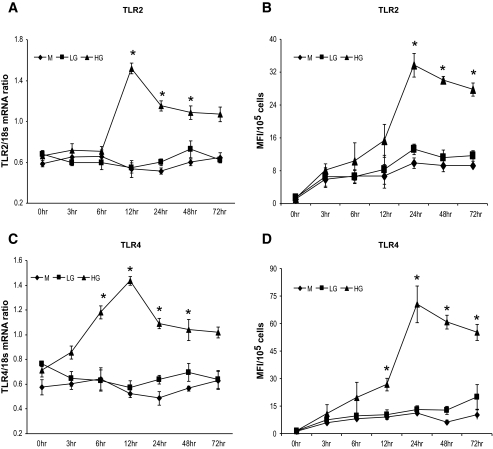
As depicted in Fig. 1A, both TLR2 and TLR4 mRNA were significantly increased under hyperglycemic conditions. High glucose significantly increased TLR2 and TLR4 protein compared with 5.5 mmol/l glucose (Fig. 1B). Because RT-PCR analysis is only semiquantitative, we used real-time RT-PCR to quantify the time-dependent changes in TLR2 and TLR4 mRNA levels. At 15 mmol/l glucose concentration, the TLR2-to-18s mRNA ratio was significantly higher at 12 h (Fig. 2A), whereas the TLR4-to-18s mRNA (Fig. 2C) ratio increased at 6 h compared with normal glucose with corresponding increase in TLR2 and TLR4 protein at 24 h (Fig. 2B and D). Addition of 9.5 mmol/l mannitol to normal glucose did not result in increased TLR2 and TLR4 levels, suggesting that the glucose-induced increase in TLR expression was not an osmotic effect. Because the maximal increase in TLR2 and TLR4 expression occurred at 24 h of incubation with high glucose, all subsequent experiments were conducted for this duration.
FIG. 1.
A: Representative RT-PCR gel of TLR2 and TLR4 mRNA expression in THP-1 cells after glucose challenge as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Densitometric values are normalized to 18s rRNA and expressed as mean ratio ± SD. *P < 0.05 vs. mannitol or 5.5 mmol/l glucose; n = 6 experiments. B: TLR2 and TLR4 protein expression was measured in THP-1 after glucose challenge by flow cytometry as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. mannitol or 5.5 mmol/l glucose; n = 6 experiments.
FIG. 2.
A: TLR2 mRNA expression in THP-1 cells after glucose challenge for indicated time points by real-time RT-PCR as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Values are expressed as mean ratio ± SD. *P < 0.001 vs. mannitol or 5.5 mmol/l glucose (LG) at 6 h; n = 4 experiments. B: TLR2 protein expression in THP-1 cells after glucose challenge for indicated time points by flow cytometry as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. mannitol or 5.5 mmol/l glucose (LG); n = 4 experiments. C: TLR4 mRNA expression in THP-1 cells after glucose challenge for indicated time points by real-time RT-PCR as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Values are expressed as mean ratio ± SD. *P < 0.001 vs. mannitol or 5.5 mmol/l glucose (LG) at 6 h; n = 4 experiments. D: TLR4 protein expression in THP-1 cells after glucose challenge for indicated time points by flow cytometry as described in research design and methods. Glucose (5.5 mmol/l) was added to mannitol control. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. mannitol or 5.5 mmol/l glucose (LG); n = 4 experiments.
We determined the time required for the high-glucose–induced TLR expression to return to basal levels. THP-1 cells incubated in high glucose for 24 h were transferred to normal glucose medium. The time course for TLR expression showed that TLR2 levels return to normal glucose levels at 48 h, whereas TLR4 takes 72 h (supplementary Fig. 1, which is available in the online appendix). In addition, we examined TLR2 and TLR4 expression in TLR4 and TLR2 siRNA-transfected cells under high glucose, respectively. The increased TLR2 expression under high glucose in TLR4 knockdown cells (9.4 ± 0.6 to 21.7 ± 1.5, P < 0.05) and TLR4 expression in TLR2 knockdown cells under high glucose was unaffected (9.5 ± 1.2 to 37 ± 0.9, P < 0.05).
High glucose induces MyD88-mediated signaling and NF-κB activity in THP-1 cells.
We determined the effect of high glucose on MyD88-dependent signaling pathway using immunoprecipitation and Western blotting techniques. TLR2 and TLR4 both activate MyD88 and NF-κB, common downstream signaling components for all TLRs except TLR3. Therefore, activation of NF-κB and production of proinflammatory cytokines induced by high glucose was used as a functional readout for the activation of TLR2 and TLR4.
High glucose significantly induced MyD88 expression and IL-1 receptor–associated kinase-1 (IRAK-1) phosphorylation in THP-1 cell lysates compared with normal glucose (Fig. 3A) with no change in β-actin levels, suggesting that the change was not due to cell growth. This was further confirmed by immunoprecipitation with TLR2 and TLR4 antibodies and blotting for MyD88 and IRAK-1 (Fig. 3B and C). High glucose induced the activation of NF-κB as determined by transcription factor assay (0.29 ± 0.02 ng/mg nuclear protein) compared with normal glucose (0.11 ± 0.01 ng/mg protein, P < 0.05).
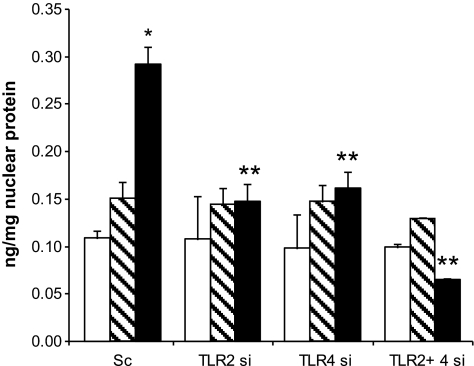
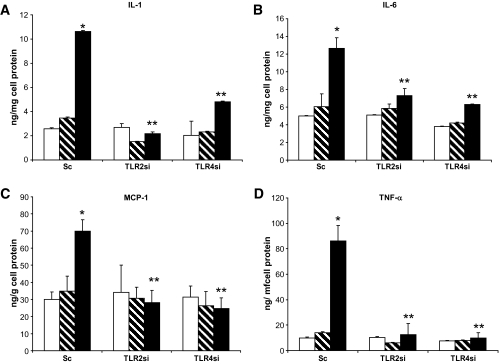
High-glucose–induced NF-κB activity and inflammatory cytokine expression are abrogated in the absence of TLR2 and TLR4 expression.
To further investigate TLR2- and TLR4-mediated inflammation under high glucose in monocytes, we used loss of function approach by knocking down TLR2 and TLR4 genes using specific siRNAs in THP-1 cells. After transfection with TLR2, TLR4, and TLR2+TLR4 siRNAs, cells were incubated in 15 mmol/l glucose for 24 h. Lack of TLR2 in THP-1 cells resulted in 48% decrease in NF-κB p65-dependent activity in the nuclear extracts compared with scrambled controls (Fig. 4; P < 0.05). Similarly, a 45% decrease was observed in the absence of TLR4 under high glucose (Fig. 4). Knocking down both TLR2 and TLR4 in the cells resulted in 76% decrease in NF-κB activity, suggesting an additive effect (Fig. 4). Next, we measured IL-1β, IL-6, MCP-1, and TNF-α release in the supernatants. Inhibition of TLR2 resulted in significant decreases in IL-1β (80%), IL-6 (42%), MCP-1 (60%), and TNF-α (85%), whereas loss of TLR4 resulted in 55% (IL-1β), 51%(IL-6), 65% (MCP-1), and 89% (TNF-α) decreases under high glucose compared with scrambled controls (Fig. 5A–D; P < 0.05).
FIG. 4.
Inhibition of TLR2 and TLR4 receptors using siRNA ameliorates high-glucose–induced NF-κB p65-dependent DNA binding activity in the nuclear extracts of THP-1 cells by ELISA as described in research design and methods. Values are normalized to milligrams nuclear protein and expressed as means ± SD. *P < 0.05 vs. Sc + high glucose (HG); Sc, scramble control siRNA; TLR2si, TLR2 receptor siRNA; TLR4si, TLR4 receptor siRNA. n = 4 experiments in duplicate. □, Mannitol;  , LG (5.5 mmol/l); ▪, HG (15 mmol/l).
, LG (5.5 mmol/l); ▪, HG (15 mmol/l).
FIG. 5.
A: IL-1β concentration in supernatants of THP-1 cells after high-glucose treatment in the absence of TLR2 and TLR4 was measured using ELISA. Values are normalized to milligrams cell protein. *P < 0.05 vs. mannitol; **P < 0.05 vs. Sc + high glucose (HG); Sc, scramble control siRNA; TLR2si, TLR2 receptor siRNA; TLR4si, TLR4 receptor siRNA. n = 4 experiments in duplicate. B: IL-6 concentration in supernatants of THP-1 cells after high-glucose treatment in the absence of TLR2 and TLR4 was measured using ELISA. Values are normalized to milligrams cell protein. *P < 0.05 vs. mannitol; **P < 0.05 vs. Sc + HG; Sc, scramble control siRNA; TLR2si, TLR2 receptor siRNA; TLR4si, TLR4 receptor siRNA. n = 4 experiments in duplicate. C: MCP-1 concentration in supernatants of THP-1 cells after high-glucose treatment in the absence of TLR2 and TLR4 was measured using ELISA. Values are normalized to milligrams cell protein. *P < 0.05 vs. mannitol; **P < 0.05 vs. Sc + HG; Sc, scramble control siRNA; TLR2si, TLR2 receptor siRNA; TLR4si, TLR4 receptor siRNA. n = 4 experiments in duplicate. D: TNF-α IL-1β concentration in supernatants of THP-1 cells after high-glucose treatment in the absence of TLR2 and TLR4 was measured using ELISA. Values are normalized to milligrams cell protein. *P < 0.05 vs. mannitol; **P < 0.05 vs. Sc + HG; Sc, scramble control siRNA; TLR2si, TLR2 receptor siRNA; TLR4si, TLR4 receptor siRNA. n = 4 experiments in duplicate. □, Mannitol;  , LG (5.5 mmol/l); ▪, HG (15 mmol/l).
, LG (5.5 mmol/l); ▪, HG (15 mmol/l).
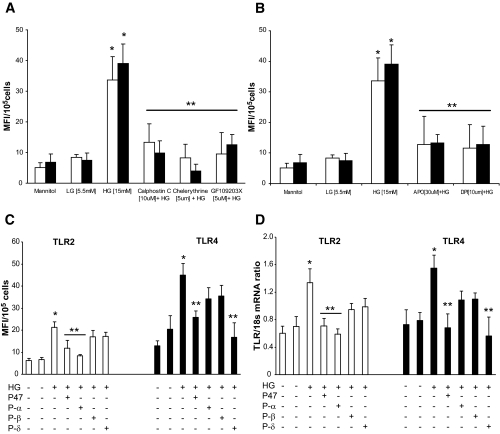
PKC-α and PKC-δ are involved in high-glucose–induced TLR2 and TLR4 expression.
We investigated the high-glucose–induced TLR2 and TLR4 activation-mediated mechanistic events in THP-1 cells using two strategies: 1) specific pharmacological inhibitors, and 2) siRNA technology.
First, we examined the role of PKC in TLR2 and TLR4 activation from THP-1 cells under high glucose. PKC inhibitors calphostin C (10 μmol/l; an inhibitor of PKC-α, -β, -δ, -ɛ, and -η), GF109203X (5 μmol/l; an inhibitor of PKCα, -β, and -ɛ), and chelerythrine (not isoform-selective PKC inhibitor; competitively interferes with the phosphate acceptor site and noncompetitively inhibits the ATP-binding site; 5 μmol/l) resulted in a significant decrease in TLR2 and TLR4 expression (Fig. 6A) in THP-1 cells compared with normal glucose.
FIG. 6.
A: Effect of PKC inhibitors (calphostin C, chelerythrine, and GF109203X) on TLR2 and TLR4 protein expression in THP-1 cells. After culturing cells with inhibitors and high glucose, cells were washed, labeled, and analyzed by flow cytometry as described in research design and methods. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. high glucose; n = 4 experiments. B: Effect of NADPH oxidase inhibitors (apocyanin and DPI) on TLR2 and TLR4 protein expression in THP-1 cells. After culturing cells with inhibitors and high glucose, cells were washed, labeled, and analyzed by flow cytometry as described in research design and methods. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. high glucose; n = 4 experiments. C: Inhibition of NADPH oxidase subunit p47Phox and PKC isoforms using siRNAs effects high-glucose–induced TLR2 and TLR4 protein expression of THP-1 cells by flow cytometry as described in research design and methods. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. scramble control siRNA + LG; **P < 0.05 vs. scramble + high glucose (HG); p47, p47Phox siRNA; P-α, PKC-α siRNA, P-β, PKC-β siRNA; P-δ, PKC-δ siRNA; +, present; −, absent. n = 4 experiments in duplicate. D: Inhibition of NADPH oxidase subunit p47Phox and PKC isoforms using siRNAs effects high-glucose–induced TLR2 and TLR4 mRNA expression of THP-1 cells by real-time RT-PCR as described in research design and methods. Values are expressed as mean ratio ± SD. *P < 0.05 vs. scramble control siRNA + LG; **P < 0.05 vs. scramble + HG; p47, p47Phox siRNA; P-α, PKC-α siRNA; P-β, PKC-β siRNA; P-δ, PKC-δ siRNA; +, present; −, absent. n = 4 experiments in duplicate. □,TLR2; ▪, TLR4.
Second, we determined which isoform of PKC mediates TLR2 and TLR4 expression from human monocytes under high glucose, using isotype gene-specific siRNAs to PKC-α, PKC-β (β), and PKC-δ. PKC-α siRNA significantly decreased TLR2 expression (protein and mRNA) in THP-1 cells (60%), whereas inhibition of PKC-δ decreased TLR4 expression by 63%. PKC-β siRNA had no effect on TLR2 and TLR4 expression (Fig. 6C and D).
NADPH oxidase cytosolic subunit p47Phox is involved in high-glucose–induced TLR2 and TLR4 expression in THP-1 cells.
NADPH oxidase is accepted as the most important mechanism for ROS generation in phagocytic cells. Previously, we have shown that p47Phox is an essential component of monocyte NADPH oxidase production and required for ROS generation under high-glucose conditions (15,30). Therefore, we examined the role of NADPH oxidase (p47Phox) in TLR2- and TLR4-modulated inflammation under high glucose using pharmacological inhibitors (apocyanin and diphenyleneiodonium) and siRNAs. Cells were pretreated with the inhibitors followed by exposure to high glucose for 24 h. Both inhibitors significantly decreased TLR2 and TLR4 expression in THP-1 cells under high glucose (Fig. 6B).
In a second set of experiments, p47Phox siRNA-transfected cells were exposed to high glucose for 24 h. TLR2 and TLR4 surface expression was measured by flow cytometric analysis. p47Phox knockdown resulted in 45% inhibition in TLR2 and 50% decrease in TLR4 expression under high glucose in THP-1 cells compared with scrambled controls (Fig. 6C and D).
PKC signaling is proximal to p47Phox in mediating high-glucose–induced TLR2 and TLR4 expression.
Based on the identification of p47Phox, PKC-α, and PKC-δ as mediators of TLR2 and TLR4 expression, respectively, under high glucose, we sought to determine the proximal signaling mediator using siRNA knockdown strategy.
1) Because PKC-α and PKC-δ are known to activate p47Phox, we examined the effect of p47Phox inhibition on PKC-α, PKC-δ, and PKC-β mRNA expression. In p47Phox siRNA-transfected high-glucose–exposed cells, PKC-α (1.4 ± 0.1 to 1.26 ± 0.3 PKCα/18s) and PKC-δ (1.4 ± 0.3 to 1.3 ± 0.15 PKCδ/18s) ratios were unchanged as assessed by real-time RT-PCR, indicating that PKC-α and PKC-δ are proximal to p47Phox.
2) In PKC-α, PKC-δ, and PKC-β siRNA-transfected cells challenged with high glucose, p47Phox mRNA–to–18s ratios did not change with PKC-β inhibition (data not shown) but significantly decreased with PKC-α (1.6 ± 0.1 to 0.5 ± 0.03 p47Phox-to-18s ratio) and PKC-δ (1.4 ± 0.2 to 0.5 ± 0.09 p47Phox-to-18s ratio) inhibition, suggesting that p47Phox is downstream of PKC.
High glucose also induces other TLRs.
To identify other TLRs and associated signaling mediators induced under high glucose, we used sensitive, quantitative, and reproducible TLR Pathway RT2 PCR arrays (Superarray). Twenty-one genes were expressed at significantly higher levels in high-glucose–treated cells compared with normal glucose, including TLR2, TLR3, TLR4, TLR6, TLR7, MyD88, and IRAK-1 (supplementary Table 1, which is available in the online appendix), further confirming our data.
High glucose induces dimerization of TLR2 with TLR6 in 293T cells.
To further confirm high-glucose–induced TLR2 and TLR4 expression, we used reporter-based cotransfection assays (33). High glucose induced significant NF-κB transactivation in TLR4-MD2–cotransfected 293T cells (control, 86 ± 3 compared with high glucose, 288 ± 9 relative luciferase activity [RLA], P < 0.05). Lee et al. (33) previously showed that TLR2 dimerizes with TLR1 or TLR6 and results in receptor activation and downstream signaling upon nonsaturated fatty acid challenge. To determine whether TLR1 or TLR6 is required for the activation of TLR2 by high glucose, 293T cells were cotransfected with murine TLR2 and either TLR1 or TLR6. High glucose activated NF-κB when TLR2 was cotransfected with TLR6 (control, 115 ± 3.5 compared with high glucose:, 319 ± 6 RLA, P < 0.05) and not TLR1. Purified lipopolysaccharide, Pam3CysSerLys4 (Pam3CSK4), and macrophage activating lipopeptide 2Kda were used as positive controls (data not shown). These results demonstrate that high glucose induces the TLR4 and TLR2 receptor activity and engagement, resulting in NF-κB activation and further confirming our data.
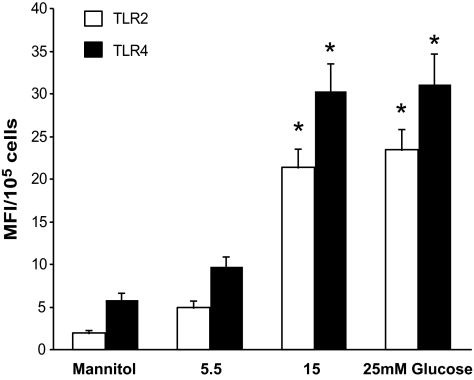
Additionally, we confirmed the in vitro mechanism of TLR2 and TLR4 activation under high-glucose conditions in human monocytes (n = 10 healthy volunteers; Fig. 7) using identical assays.
FIG. 7.
TLR2 and TLR4 protein expression was measured in freshly isolated and pooled human monocytes from healthy volunteers (n = 3 volunteers/experiment) after glucose challenge by flow cytometry as described in research design and methods. Values are expressed as MFI/105 cells ± SD. *P < 0.05 vs. mannitol or 5.5 mmol/l glucose; n = 4 experiments. □, TLR2; ▪, TLR4.
DISCUSSION
The cellular and molecular mechanisms whereby diabetes accelerates cardiovascular disease remain to be elucidated. The Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications Studies clearly showed that reducing glycemia with insulin treatment decreases cardiovascular events (1–3). Hyperglycemia induces inflammation, affects extracellular matrix and procoagulant proteins, increases apoptosis in endothelial cells, decreases proliferation, and inhibits fibrinolysis, resulting in endothelial dysfunction. Hyperglycemia also induces oxidative stress (4–7).
In this study, we make the novel observation that the expression and activity of TLR2 and TLR4, key innate immune system sensors, under high-glucose conditions are increased, we delineate the corresponding signaling events, and we demonstrate functional activation in human monocytes. Our results show that high glucose dose- and time-dependently induces a marked increase in TLR2 and TLR4 mRNA and protein expression, and these effects are not osmotic because mannitol had no effect. THP-1 cells are a well-characterized human monocytic cell line, and data were further confirmed in human monocytes. Signaling through TLRs is believed to be the critical first step in monocytes activation. Increase in TLR2 and TLR4 expression observed here is consistent with those reported in macrophages of atherosclerotic lesions (35), human endothelial cells (36) smooth muscle cells of coronary arteries (37), dendritic cells (38), keratinocytes (39), preadipocytes (40), adipocytes (41), and pancreatic islets (27). However, all of these studies were performed under nondiabetic conditions with minimal information on the TLR-mediated downstream signaling and mechanism of activation. In this context, we have provided sequential data that in human monocytes, high glucose results in increased TLR2 and TLR4 expression and activity, resulting in MyD88-dependent signaling and culminating in NF-κB transactivation, leading to significant proinflammatory cytokine secretion. Inhibition of TLR2 and TLR4 together in cells was additive, resulting in a further decrease in NF-κB activity, indicating that activation of both receptors is critical. This mechanism involves PKC and NADPH oxidase activation, thus elaborating the steps that potentiate TLR2 and TLR4 activation-mediated inflammation seen in diabetes.
TLRs activate two types of downstream signaling pathways: MyD88-dependent and MyD88-independent pathways (16). MyD88 is an immediate and common downstream adaptor molecule recruited by activated TLRs through their Toll-IL-1 receptor domain domain. MyD88, in turn, recruits IRAK and induces phosphorylation. IRAK-1 associates with TRAF6, leading to the activation of IKK complex and resulting in the activation of NF-κB transcription factor. The activation of MyD88-dependent signaling pathway leads to the induction of inflammatory cytokines. In this study, we show that TLR2 and TLR4 activation recruits the MyD88-dependent signaling pathway. We demonstrate increased expression of MyD88, phosphorylation of IRAK-1, and activation of NF-κB with concomitant increase in inflammatory cytokine secretion.
However, the fundamental question of how high glucose activates TLR2 and TLR4 in the monocytes and how this leads to increased inflammation needs to be determined. Dimerization is a critical event in the functional activation of TLRs (33). TLR2 activity requires heterodimerization with TLR1 or TLR6 to confer sensitivity to agonists (33,42). Dimerization of the cytoplasmic domain of TLR2 with TLR6 or TLR1 results in cytokine production. Previous studies in macrophage cell lines showed that TLR2 and TLR6 functioned cooperatively to detect Gram-positive bacteria, peptidoglycan, and zymosan (34). Luciferase reporter assays suggest that high glucose induces TLR2 and TLR6 heterodimerization, via NF-κB activation and cytokine production, in addition to real-time RT-PCR data (supplementary Table 1). These results indicate that TLR2 and TLR6 dimerize to facilitate NF-κB and inflammatory gene activation. The dimerization of TLR4 was shown to be a prerequisite for the ligand-induced receptor activation, which needs to be determined in addition to understanding the role of other TLRs (supplementary Table 1) under high glucose in future studies. These results suggest that high glucose induces TLR2 receptor dimerization, and this, in turn, engages downstream MyD88-dependent signaling pathway.
In an attempt to determine the time taken for the high-glucose–induced TLR2 and TLR4 expression attunement to basal levels, we transferred high-glucose–exposed cells to normal glucose serum-free media. We measured TLR2 and TLR4 expression, which suggests that high-glucose–induced TLR expression persists for 48–72 h before coming back to normal glucose levels. The physiological consequences of this prolonged expression remain to be elucidated. In another set of experiments, we measured TLR2 and TLR4 expression in TLR4- and TLR2-deficient cells. Our data indicate that both TLR2 and TLR4 are unaffected by the absence of either of them.
The PKC pathway mediates a wide range of cellular signals and is involved in the activation of NF-κB (43). Published data suggest that all TLR family members activate nearly identical cytoplasmic signaling pathways except TLR3; recently, it was indicated that a TLR2, TLR4, and PKC axis exists under different conditions. In addition, diabetes and cells cultured under high glucose show increases in PKC activity (12,16,30). We previously showed that increased monocyte superoxide release under high glucose is via activation of PKC-α (16,30). To obtain further insight into the regulation of TLR2 and TLR4 via PKC under high glucose, we used a twin strategy: First, pharmacological inhibitors of PKC (calphostin C, chelerythrine, and GFX2093) inhibited high-glucose–induced TLR2 and TLR4 expression. Second, inhibition of PKC-α using siRNA reduced TLR2 expression, whereas siRNA of PKC-δ resulted in decreased TLR4 expression. Our results are in line with those observed in neutrophils where both TLR2 and TLR4 are activated through PKC-α/β–(44) and PKC-α/δ–dependent activation in murine macrophages. Thallas-Bonke et al. (45) report that activation of NADPH oxidase via PKC-α is a key mechanism in diabetic renal disease. PKC-δ activation plays a critical role in the endoplasmic reticulum stress–mediated cell death in cardiac myocytes and ischemic hearts of rats (46). Bey et al. (47) showed that PKC-δ plays a pivotal role in stimulating monocyte NADPH oxidase activity through its regulation of phosphorylation and translocation of p47Phox. Furthermore, Ryan et al. (48) recently showed that ROS regulates TLR4-mediated activation of NF-κB and IL-8 expression. All of these studies strengthen our findings that TLR2 and TLR4 are regulated by PKC-α and PKC-δ, and this is associated with p47Phox-dependent NADPH oxidase activity under high glucose.
NF-κB signaling occurs via oxidant-sensitive pathways (49). The NADPH oxidase complex in phagocytic cells and the generation of oxidants serve a crucial function in host defense against invading microorganisms (50). In addition, Shi et al. (51) recently reported that TLR4 is activated by free fatty acids, acts as a molecular link between inflammation and innate immune system, and plays a role in the regulation of energy balance and insulin resistance in response to changes in the nutritional environment. Data from the current study add to increased TLR activity and increased insulin resistance seen in diabetic milieu. Our previous studies showed that the monocyte is a key target of NADPH oxidase activity under high glucose (15,30). NADPH oxidase–derived oxidants mediate the high-glucose–induced NF-κB activation and result in enhanced IL-6 and IL-1β expression in monocytes (9,15,30). Although high glucose induces oxidative burst in monocytes, it remains unclear whether the released oxidants contribute to the high-glucose–induced NF-κB activation and thus are involved in stimulating TLR2-TLR4 expression. It is possible that increased NF-κB binding and ROS generation may occur early, whereas increased TLR expression may contribute to NF-κB binding later (at 24 h) (12). In this study, we show inhibitors of NADPH oxidase (apocyanin and DPI) abrogate high-glucose–induced TLR2 and TLR4 expression in monocytes. We further demonstrate that the loss of cytosolic component of NADPH oxidase, namely p47Phox, impairs TLR2 and TLR4 activation under high glucose that in turn activates NF-κB and inflammatory cytokines. Our present results are in accordance with an earlier report suggesting a TLR4-TLR2 cross-talk mediated by NADPH oxidase in endothelial cells (36).
It is now established that increased inflammation is a key etiological factor in the development of many chronic diseases, including cancer, atherosclerosis, and diabetes. Our results suggest that inflammatory effects of high glucose may be at least in part mediated through the modulation of inflammatory responses resulting from TLR activation induced by hyperglycemia in diabetes.
Supplementary Material
Acknowledgments
M.R.D. has received American Diabetes Association Grant 7-07-JF-16. I.J. has received National Institutes of Health Grant K24-AT-00596. S.D. has received NIHIK59801.
Published ahead of print at http://diabetes.diabetesjournals.org on 23 July 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Ruderman NB, Haudenschild C: Diabetes as an atherogenic factor. Prog Cardiovasc Dis 26: 373–412, 1984 [DOI] [PubMed] [Google Scholar]
- 2.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B, the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group: Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 353: 2643–2653, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M: Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339: 229–234, 1998 [DOI] [PubMed] [Google Scholar]
- 4.Schram MT, Chaturvedi N, Schalkwijk C, Giorgino F, Ebeling P, Fuller JH, Stehouwer CD, the EURODIAB Prospective Complications Study: Vascular risk factors and markers of endothelial function as determinants of inflammatory markers in type 1 diabetes: the EURODIAB Prospective Complications Study. Diabetes Care 26: 2165–2173, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Schalkwijk CG, Poland DC, van Dijk W, Kok A, Emeis JJ, Drager AM, Doni A, van Hinsbergh VW, Stehouwer CD: Plasma concentration of C-reactive protein is increased in type I diabetic patients without clinical macroangiopathy and correlates with markers of endothelial dysfunction: evidence for chronic inflammation. Diabetologia 42: 351–357, 1999 [DOI] [PubMed] [Google Scholar]
- 6.Devaraj S, Glaser N, Griffen S, Wang-Polagruto J, Miguelino E, Jialal I: Increased monocytic activity and biomarkers of inflammation in patients with type 1 diabetes. Diabetes 55: 774–779, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Jialal I, Devaraj S, Venugopal SK: Oxidative stress, inflammation, and diabetic vasculopathies: the role of alpha tocopherol therapy. Free Radic Res 6: 1331–1336, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Jain SK, Kannan K, Lim G, Matthew-Greer J, McVie R, Bocchini JA: Elevated blood interleukin-6 levels in hyperketonemic type 1 diabetic patients and secretion by acetoacetate-treated cultured U937 monocytes. Diabetes Care 26: 2139–2143, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Shanmugam N, Reddy MA, Guha M, Natarajan R: High-glucose–induced expression of proinflammatory cytokine and chemokine genes in monocytic cells. Diabetes 52: 1256–1264, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Igarashi M, Wakasaki H, Takahara N, Ishii H, Jiang ZY, Yamauchi T, Kuboki K, Meier M, Rhodes CJ, King GL: Glucose or diabetes activates p38 mitogen-activated protein kinase via different pathways. J Clin Invest 103: 185–195, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ceolotto G, Gallo A, Miola M, Sartori M, Trevisan R, Prato SD, Semplicini A, Avogaro A: Protein kinase C activity is acutely regulated by plasma glucose concentration in human monocytes in vivo. Diabetes 48: 1316–1322, 1999 [DOI] [PubMed] [Google Scholar]
- 12.Dandona P, Chaudhuri A, Ghanim H, Mohanty P: Proinflammatory effects of glucose and anti-inflammatory effect of insulin: relevance to cardiovascular disease. Am J Cardiol 99: 15B–26B, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Hill H, Hogan N, Rallison M, Santos JI, Charette RP, Kitahara M: Functional and metabolic abnormalities of diabetic monocytes. Adv Exp Med Biol 69: 621–627, 1980 [DOI] [PubMed] [Google Scholar]
- 14.Yan SF, Ramasamy R, Schmidt AM: Mechanisms of disease: advanced glycation end-products and their receptor in inflammation and diabetes complications. Nat Clin Pract Endocrinol Metab 4: 285–293, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Devaraj S, Venugopal SK, Singh U, Jialal I: Hyperglycemia induces monocytic release of interleukin-6 via induction of protein kinase C-α and -β. Diabetes 54: 85–91, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Uematsu S, Akira S: Toll-like receptors and innate immunity. J Mol Med 84: 712–725, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Beutler B: Inferences, questions and possibilities in Toll-like receptor signaling. Nature 430: 257–263, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Tsan MF, Gao B: Endogenous ligands of Toll-like receptors. J Leukocyte Biol 76: 514–519, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Tobias PS, Curtiss LK: Toll-like receptors in atherosclerosis. Biochem Soc Trans 35: 1453–1455, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Devaraj S, Dasu MR, Rockwood J, Winter W, Griffen SC, Jialal I: Increased toll-like receptor (TLR) 2 and TLR4 expression in monocytes from patients with type 1 diabetes: further evidence of a proinflammatory state. J Clin Endocrinol Metab 93: 578–583, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li H, Sun B: Toll-like receptor 4 in atherosclerosis. J Cell Mol Med 11: 88–95, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michelsen KS, Wong MH, Shah PK, Zhang W, Yano J, Doherty TM, Akira S, Rajavashisth TB, Arditi M: Lack of Toll-like receptor 4 or myeloid differentiation factor 88 reduces atherosclerosis and alters plaque phenotype in mice deficient in apolipoprotein E. Proc Natl Acad Sci U S A 101: 10679–10684, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu X, Ukai T, Yumoto H, Davey M, Goswami S, Gibson FC III, Genco CA: Toll-like receptor 2 plays a critical role in the progression of atherosclerosis that is independent of dietary lipids. Atherosclerosis 196: 146–154, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mullick AE, Tobias PS, Curtiss LK: Modulation of atherosclerosis in mice by Toll-like receptor 2. J Clin Invest 115: 3149—3156, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjorkbacka H, Kunjathoor VV, Moore KJ, Koehn S, Ordija CM, Lee MA, Means T, Halmen K, Luster AD, Golenbock DT, Freeman MW: Reduced atherosclerosis in MyD88-null mice links elevated serum cholesterol levels to activation of innate immunity signaling pathways. Nat Med 10: 416–421, 2004 [DOI] [PubMed] [Google Scholar]
- 26.Mohammad MK, Morran M, Slotterbeck B, Leaman DW, Sun Y, Grafenstein H, Hong SC, McInerney MF: Dysregulated Toll-like receptor expression and signaling in bone marrow-derived macrophages at the onset of diabetes in the non-obese diabetic mouse. Int Immunol 18: 1101–1113, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Kim HS, Han MS, Chung KW, Kim S, Kim E, Kim MJ, Jang E, Lee HA, Youn J, Akira S, Lee MS: Toll-like receptor 2 senses beta-cell death and contributes to the initiation of autoimmune diabetes. Immunity 27: 321–333, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Song MJ, Kim KH, Yoon JM, Kim JB: Activation of Toll-like receptor 4 is associated with insulin resistance in adipocytes. Biochem Biophys Res Commun 346: 739–745, 2006 [DOI] [PubMed] [Google Scholar]
- 29.Creely SJ, McTernan PG, Kusminski CM, Fisher M, Da Silva NF, Khanolkar M, Evans M, Harte AL, Kumar S: Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab 292: E740–E747, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Dasu MR, Devaraj S, Jialal I: High glucose induces IL-1β expression in human monocytes: mechanistic insights. Am J Physiol Endocrinol Metab 293: E337–E346, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pfaffl MW: A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acid Res 29: e45, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dasu MR, Devaraj S, Du Clos TW, Jialal I: The biological effects of CRP are not attributable to endotoxin contamination: evidence from TLR4 knockdown human aortic endothelial cells. J Lipid Res 48: 509–512, 2007 [DOI] [PubMed] [Google Scholar]
- 33.Lee JY, Zhao L, Youn HS, Weatherill AR, Tapping R, Feng L, Lee WH, Fitzgerald KA, Hwang DH: Saturated fatty acid activates but polyunsaturated fatty acid inhibits Toll-like receptor 2 dimerized with Toll-like receptor 6 or 1. J Biol Chem 279: 16971–16979, 2004 [DOI] [PubMed] [Google Scholar]
- 34.Zhao L, Kwon MJ, Huang S, Lee JY, Fukase K, Inohara N, Hwang DH: Differential modulation of Nods signaling pathways by fatty acids in human colonic epithelial HCT116 cells. J Biol Chem 282: 11618–11628, 2007 [DOI] [PubMed] [Google Scholar]
- 35.Edfeldt K, Swedenborg J, Hansson GK, Yan ZQ: Expression of toll-like receptors in human atherosclerotic lesions: a possible pathway for plaque activation. Circulation 105: 1158–1161, 2002 [PubMed] [Google Scholar]
- 36.Fan J, Frey RS, Malik AB: TLR4 signaling induces TLR2 expression in endothelial cells via neutrophil NADPH oxidase. J Clin Invest 112: 1136–1137, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang X, Coriolan D, Murthy V, Schultz K, Golenbock DT, Beasley D: Proinflammatory phenotype of vascular smooth muscle cells: role of efficient Toll-like receptor 4 signaling. Am J Physiol Heart Circ Physiol 289: H1069–H1076, 2005 [DOI] [PubMed] [Google Scholar]
- 38.Kaisho S, Akira S: Regulation of dendritic cell function through Toll-like receptors. Curr Mol Med 3: 373–385, 2003 [DOI] [PubMed] [Google Scholar]
- 39.Miller LS, Sorensen OE, Liu PT, Jalian HR, Eshtiaghpour D, Behmanesh BE, Chung W, Starner TD, Kim J, Sieling PA, Ganz T, Modlin RL: TGF-alpha regulates TLR expression and function on epidermal keratinocytes. J Immunol 174: 6137–6143, 2005 [DOI] [PubMed] [Google Scholar]
- 40.Saillan-Barreau C, Cousin B, Andre M, Villena P, Casteilla L, Penicaud L: Human adipose cells as candidates in defense and tissue remodeling phenomena. Biochem Biophys Res Commun 309: 502–505, 2003 [DOI] [PubMed] [Google Scholar]
- 41.Bès-Houtmann S, Roche R, Hoareau L, Gonthier MP, Festy F, Caillens H, Gasque P, Lefebvre d'Hellencourt C, Cesari M: Presence of functional TLR2 and TLR4 on human adipocytes. Histochem Cell Biol 127: 131–137, 2007 [DOI] [PubMed] [Google Scholar]
- 42.Takeuchi O, Sato S, Horiuchi T, Hoshino K, Takeda K, Dong Z, Modlin RL, Akira S: Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins. J Immunol 169: 10–14, 2002 [DOI] [PubMed] [Google Scholar]
- 43.Moscat J, Diaz-Meco MT, Rennert P NF-κB activation by protein kinase C isoforms and B-cell function. EMBO Rep 4: 31–36, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asehnoune K, Strassheim D, Mitra S, Yeol Kim J, Abraham E: Involvement of PKCalpha/beta in TLR4 and TLR2 dependent activation of NF-kappaB. Cell Signal 17: 385–394, 2005 [DOI] [PubMed] [Google Scholar]
- 45.Thallas-Bonke V, Thorpe SR, Coughlan MT, Fukami K, Yap FY, Sourris KC, Penfold SA, Bach LA, Cooper ME, Forbes JM: Inhibition of NADPH oxidase prevents advanced glycation end product-mediated damage in diabetic nephropathy through a protein kinase C-α–dependent pathway. Diabetes 57: 460–469, 2008 [DOI] [PubMed] [Google Scholar]
- 46.Qi X, Vallentin A, Churchill E, Mochly-Rosen D: DeltaPKC participates in the endoplasmic reticulum stress-induced response in cultured cardiac myocytes and ischemic heart. J Mol Cell Cardiol 43: 420–428, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bey EA, Xu B, Bhattacharjee A, Oldfield CM, Zhao X, Li Q, Subbulakshmi V,Feldman GM, Wientjes FB, Cathcart MK: Protein kinase C delta is required for p47Phox phosphorylation and translocation in activated human monocytes. J Immunol 173: 5730–5738, 2004 [DOI] [PubMed] [Google Scholar]
- 48.Ryan KA, Smith MF Jr, Sanders MK, Ernst PB: Reactive oxygen and nitrogen species differentially regulate Toll-like receptor 4-mediated activation of NF-kappa B and interleukin-8 expression. Infect Immun 72: 2123–2130, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bowie A, O'Neill LA: Oxidative stress and nuclear factor-kappaB activation: a reassessment of the evidence in the light of recent discoveries. Biochem Pharmacol 59: 13–23, 2000 [DOI] [PubMed] [Google Scholar]
- 50.Babior BM: NADPH oxidase: an update. Blood 93: 1464–1476, 1999 [PubMed] [Google Scholar]
- 51.Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS: TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 116: 3015–3025, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.