Abstract
OBJECTIVE—To examine the longitudinal association of fat mass–and obesity-associated (FTO) variant with obesity, circulating adipokine levels, and FTO expression in various materials from human and mouse.
RESEARCH DESIGN AND METHODS—We genotyped rs9939609 in 2,287 men and 3,520 women from two prospective cohorts. Plasma adiponectin and leptin were measured in a subset of diabetic men (n = 854) and women (n = 987). Expression of FTO was tested in adipocytes from db/db mice and mouse macrophages.
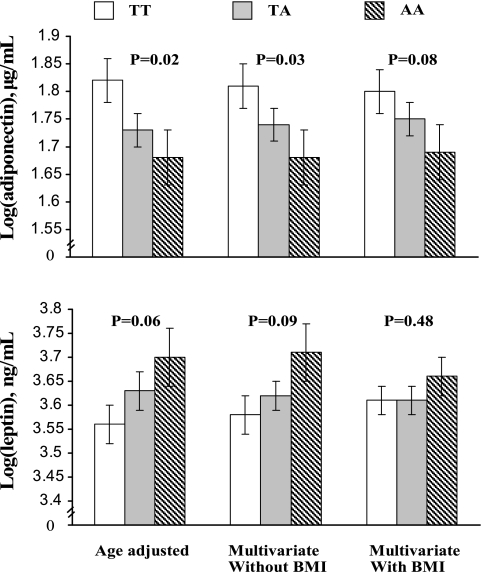
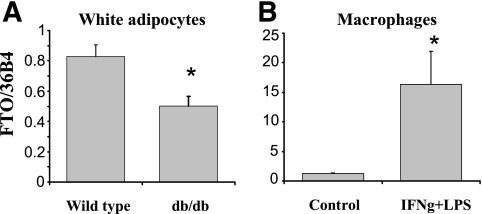
RESULTS—We observed a trend toward decreasing associations between rs9939609 and BMI at older age (≥65 years) in men, whereas the associations were constant across different age groups in women. In addition, the single nucleotide polymorphism (SNP) rs9939609 was associated with lower plasma adiponectin (log[e]− means, 1.82 ± 0.04, 1.73 ± 0.03, and 1.68 ± 0.05 for TT, TA, and AA genotypes, respectively; P for trend = 0.02) and leptin (log[e]− means, 3.56 ± 0.04, 3.63 ± 0.04, and 3.70 ± 0.06; P for trend = 0.06) in diabetic women. Adjustment for BMI attenuated the associations. FTO gene was universally expressed in human and mice tissues, including adipocytes. In an ancillary study of adipocytes from db/db mice, FTO expression was ∼50% lower than in those from wild-type mice.
CONCLUSIONS—The association between FTO SNP rs9939609 and obesity risk may decline at older age. The variant affects circulating adiponectin and leptin levels through the changes in BMI. In addition, the expression of FTO gene was reduced in adipocytes from db/db mice.
In a recent genome-wide association study, Frayling et al. (1) identified a common variant in fat mass–and obesity-associated (FTO) gene (rs9939609) that was related to higher BMI in both children and adults. In addition, adiposity appeared to mediate the association between FTO variant and the risk of type 2 diabetes (2,3). Several other studies have also observed associations between FTO variants and obesity-related traits in various populations (4–13).
Because most available data are cross-sectional, the longitudinal pattern of the associations between FTO variants and adiposity and age-specific genetic effects are not clearly defined. The primary aim of the present study is to address these issues by assessing the genetic effects in two prospective cohorts. Obesity status affects the endocrine function of adipose tissue by altering the secretion of adipokines, such as adiponectin and leptin, which have been related to ectopic fat accumulation, insulin sensitivity, and diabetes risk in epidemiological studies (14–16). We therefore examined the associations of FTO variant with circulating levels of adiponectin and leptin. In addition to the association analyses, to shed light on its potential functions, we also examined the expression of FTO gene in various tissues from humans and mice and investigated the expression in adipocytes from db/db mice and mice macrophages in response to inflammatory stimulants.
RESEARCH DESIGN AND METHODS
The Nurses’ Health Study (NHS) was established in 1976 when 121,700 female registered nurses aged 30–55 years and residing in 11 large U.S. states completed a mailed questionnaire on their medical history and lifestyle (17). Between 1989 and 1990, 32,826 women provided blood samples. The Health Professional Follow-Up Study (HPFS) is a prospective cohort study of 51,529 U.S. male health professionals aged 40–75 years at study initiation in 1986 (18). Between 1993 and 1999, 18,159 men provided blood samples. Information about health and disease is assessed biennially by self-administered questionnaires in both cohorts.
Diabetes cases were defined as self-reported diabetes confirmed by a validated supplementary questionnaire. For cases occurring before 1998, the diagnosis was made using criteria proposed by the National Diabetes Data Group (19). Medical record review confirmed 98% of the diagnoses. We used the American Diabetes Association diagnostic criteria for diagnosis after the 1998 cycles (20). Subjects for the present study were selected from those who provided blood samples and were free from cardiovascular disease or cancer at baseline. Healthy control subjects were matched on age and the time of blood drawing with diabetic patients. To reduce potential bias due to population stratification, we included only Caucasians of European ancestry. In total, 1,506 female and 1,076 male diabetic patients and 2,014 female and 1,211 male nondiabetic control subjects were included.
Assessment of adiposity.
At baseline (1976 for the NHS and 1986 for the HPFS), participants were asked to report their height and current body weight; the self-reported weight was then updated every 2 years during the follow-up through 2002 (1976, 1978, 1980, 1982, 1986, 1988, 1990, 1992, 1994, 1996, 1998, 2000, and 2002 in the NHS; and 1986, 1988, 1990, 1992, 1994, 1996, 1998, 2000, and 2002 in the HPFS) using self-administered questionnaires. To assess the adiposity in early adulthood, the 1980 NHS questionnaire asked about weight at 18 years of age (n = 3,337), and the 1986 HPFS questionnaire asked about weight at 21 years of age (n = 2,194). We calculated BMI as weight in kilograms divided by height squared in meters. In 1986–1987, participants in the NHS (n = 2,333) and HPFS (n = 1,898) reported direct measurements of their waists (at the umbilicus) and hips (at the largest circumference) to the nearest quarter of an inch, using a paper tape and detailed measuring directions. The validity of self-reported adiposity measures were assessed in a random sample living in the greater Boston area, with high correlation with measured weight (r ≥ 0.96) and waist (r = 0.95) (21,22). We defined obesity as BMI ≥30 kg/m2.
Assessment of biomarkers.
Blood samples were collected between 1989 and 1990 in NHS and between 1993 and 1999 in HPFS, as previously described (23,24). Biomarkers were measured in a subset of diabetic men (n = 854) and women (n = 987). Plasma adiponectin concentration was measured by competitive radioimunoassay (RIA; Linco Research, St. Charles, MO) with a coefficient of variation (CV) of 3.4%. Leptin was assayed by RIA (Linco Research) with intra-assay CV of 3.4–8.3%. A1C values were determined based on turbidimetric immunoinhibition using hemolyzed whole blood or packed red cells. The day-to-day variability at A1C concentrations of 5.5 and 9.1% was 1.9 and 3.0%, respectively.
Single nucleotide polymorphism selection and genotype determination.
To date, five single nucleotide polymorphisms (SNPs) in FTO genes have been reported to be associated with obesity traits. These SNPs are in strong to perfect linkage disequilibrium. We therefore selected one SNP, rs9939609, which was found by the first genome-wide association (GWA) study, as a proxy for other SNPs (pairwise r2 with rs9939609: rs17817449, 1.00; rs1421085, 0.97; rs3751812, 1.00; and rs9930506, 0.84; HapMap, Centre d’Etude du Polymorphisme Humain [CEPH]). DNA was extracted from the buffy coat fraction of centrifuged blood using the QIAmp Blood kit (Qiagen, Chatsworth, CA). The SNP was genotyped using TaqMan SNP allelic discrimination by means of an ABI 7900HT (Applied Biosystems, Foster City, CA). The internal quality of genotype data was assessed by typing 10% blinded samples in duplicate; resulting concordance was >99%. The call rate was >95%, and genotype distribution was in Hardy-Weinberg equilibrium (χ2 test).
Real-time RT-PCR and analyses of experimental data.
Mouse tissues were collected from wild-type (n = 3; C57BL/6 strain mice obtained from The Jackson Laboratories [Bar Harbor, ME]) and db/db mice (n = 3, 3 months old, male), a genetic model of obesity and type 2 diabetes. Mouse 3T3-L1 adipocytes were differentiated in media containing insulin, dexamethasone, and isobutylmethylxanthine for 8 days. Human adipocytes were differentiated from preadipocytes (obtained from a cell line maintained by Cambrex) in a similar manner. Mouse macrophages were generated from bone marrow of wild-type mice as described previously (25). Macrophages were cultured in Dulbecco's modification of Eagle's medium and 10% fetal bovine serum and treated with γ-interferon (IFN-γ) at a dose of 2 ng/ml overnight. Lipopolysaccharide (LPS; 10 ng/ml) was then added for an additional 8 h. RNA was isolated using TRIzol (Invitrogen) and reverse transcribed with the Quantitect RT kit (Qiagen). Human tissue (brain, heart lung, liver, spleen, intestine, kidney, muscle, leukocytes, preadipocytes, and adipocytes) cDNAs were purchased from Clontech (multiple choice cDNA). SYBR green–based real-time PCRs were conducted using RealMasterMix (Eppendorf) and detected by the 7300 Real-Time PCR system (Applied Biosystems). The expression of the 36B4 gene, which is a housekeeping gene to serve as a control, was used for normalization to obtain relative expression levels. The slope of efficiency curves for human FTO gene is −3.4 and for mouse is −3.6 (−4 means PCR product doubles each cycle). Oligo sequences used were as follows: human FTO, 5′-TTTAGTTCCACCCACCGAGT-3′ and 5′-ACATTCTGCAGAGCCAACTG-3′; mouse FTO, 5′-ATCACGATGAGAACCTGGTG-3′ and 5′-CCAACATGCCAAGTATCAGG-3′; and 36B4, 5′-AGATGCAGCAGATCCGCAT-3′ and 5′-GTTCTTGCCCATCAGCACC-3′.
For gene expression analyses, values are presented as means ± SE (n = 3), and group means were compared using Student's t test. The SAS statistical package was used for the analyses (SAS, version 8.2 for UNIX). Statistical significance was set at the 0.05 level, and all tests were two-tailed.
Statistical analyses.
Similar associations between FTO SNP rs9939606 and BMI were previously reported in diabetic patients and control subjects (1) and were also observed in our cohorts. Thus, we pooled diabetic and nondiabetic subjects in the analyses. The geometric means of BMI and waist circumference were compared among the genotypes using general linear models, adjusting for age and diabetes status. In the multivariable analyses, we also adjusted for physical activity (quintiles), smoking (never, past, and current), alcohol intake (nondrinker and drinker [0.1–4.9, 5–10, or >10 g/day]), family history of diabetes (yes/no), and menopausal status (pre- or postmenopausal [never, past, or current hormone use]; women only). Crude associations between genotype and binary outcomes (obesity and diabetes) were tested using Pearson's χ2 statistic, and unconditional logistic regression was used to test for association after adjusting for covariates. General linear models were used to compare the genotype difference in biomarkers (adiponectin and leptin) among diabetic patients, adjusting for age, BMI, physical activity, smoking, alcohol intake, duration of diabetes, A1C, and menopausal status (women only). Plasma adiponectin and leptin levels were logarithmically transformed to achieve a normal distribution. The geometric means of the back-transformed values were presented.
We used generalized estimating equations (GEEs) to analyze the associations between the genotypes and longitudinal BMI values (26,27). The analysis used the biennially collected repeated measurements of BMI from 1976 to 2002 in the NHS and from 1986 to 2002 in the HPFS. We used exchangeable correlation structure to account for the correlation of the repeated measures. Interaction between genotype and age was tested by creating a product term of the two variables in the model.
RESULTS
Table 1 shows the baseline characteristics of the participants by sex and diabetes status. The frequency of rs9939609 allele A in the study populations was 0.44, similar to the HapMap population frequency of 0.45 in the CEPH and other European populations (1,4).
TABLE 1.
Baseline characteristics of the men and women from the HPFS and NHS
| Characteristics | Men (HPFS)
|
Women (NHS)
|
||
|---|---|---|---|---|
| Diabetic | Nondiabetic | Diabetic | Nondiabetic | |
| Participants (n) | 1,076 | 1,211 | 1,506 | 2,014 |
| Age (years) | 56 ± 8 | 55 ± 9 | 44 ± 7 | 44 ± 7 |
| Physical activity* | 14.7 ± 19.0 | 21.5 ± 28.1 | 3.6 ± 2.8 | 4.1 ± 2.9 |
| Alcohol consumption (g/day) | 11.4 ± 16.8 | 12.3 ± 15.5 | 4.1 ± 8.3 | 6.4 ± 9.8 |
| Smoking | 11.0 | 7.0 | 28.9 | 21.8 |
| Family history of diabetes | 32.3 | 12.6 | 52.5 | 22.7 |
Data are n, means ± SD, and percent. Cohort baseline, 1976 for the NHS and 1986 for HPFS; physical activity and alcohol consumption were obtained from the 1980 questionnaire in NHS.
In hours of physical activity of at least moderate intensity per week for women and in MET hours per week for men.
Associations with adiposity at early and middle adulthood.
Table 2 shows the associations of SNP rs9939609 with BMI (n = 2,236 and 3,483 in men and women, respectively) and waist circumference (n = 1,898 and 2,333 in men and women, respectively) in 1986/1987, when both measures were available in the NHS and HPFS, and with BMI at early adulthood (n = 2,194 and 3,337 in men and women, respectively). The SNP was associated with higher BMI and waist circumference in women, under an additive inheritance model. In men, rs9939609 was associated with a higher BMI. SNP rs9939609 was also associated with higher BMI at early adulthood in men and women (Table 2). Although the genetic effects in men seemed not to fit well with the additive model, testing for the departure from the additive model was not significant. Because smoking may affect adiposity, we excluded current smokers in sensitivity analyses but did not find appreciable changes in the associations.
TABLE 2.
BMI and waist circumference (in cm) according to rs9939609 genotypes
| n | Mean measures by genotypes
|
P values
|
P values per allele | |||||
|---|---|---|---|---|---|---|---|---|
| TT | TA | AA | TA vs. TT | AA vs. TA | AA vs. TT | |||
| Men | 2,287 | 34* | 48* | 18* | ||||
| BMI (kg/m2), age 21 | 2,194 | 23.1 ± 3.0 | 23.1 ± 3.0 | 23.8 ± 3.2 | 0.94 | 0.0001 | 0.0002 | 0.0007 |
| BMI (kg/m2), 1986 | ||||||||
| All subjects | 2,236 | 26.2 ± 3.7 | 26.3 ± 3.6 | 26.7 ± 4.0 | 0.45 | 0.05 | 0.01 | 0.02 |
| Nonsmoker | 2,042 | 26.2 ± 3.8 | 26.3 ± 3.5 | 26.7 ± 4.0 | 0.58 | 0.18 | 0.09 | 0.09 |
| Waist circumference, 1987 | ||||||||
| All subjects | 1,898 | 97.7 ± 10.4 | 98.0 ± 10.0 | 98.4 ± 10.8 | 0.44 | 0.55 | 0.23 | 0.12 |
| Nonsmoker | 1,740 | 97.6 ± 10.4 | 97.9 ± 9.8 | 98.3 ± 10.8 | 0.39 | 0.68 | 0.28 | 0.14 |
| Women | 3,520 | 34* | 46* | 20* | ||||
| BMI (kg/m2), age 18 | 3,337 | 21.7 ± 3.3 | 21.9 ± 3.5 | 22.5 ± 3.7 | 0.06 | 0.0009 | <0.0001 | <0.0001 |
| BMI (kg/m2), 1986 | ||||||||
| All subjects | 3,483 | 26.8 ± 5.6 | 27.4 ± 5.9 | 28.2 ± 6.1 | 0.008 | 0.0099 | <0.0001 | <0.0001 |
| Nonsmoker | 2,624 | 26.9 ± 5.6 | 27.5 ± 5.9 | 28.3 ± 6.2 | 0.019 | 0.008 | <0.0001 | <0.0001 |
| Waist circumference, 1986 | ||||||||
| All subjects | 2,333 | 82.8 ± 13.1 | 83.9 ± 13.3 | 85.2 ± 14.3 | 0.27 | 0.12 | 0.02 | 0.02 |
| Nonsmoker | 2,007 | 82.7 ± 13.0 | 83.8 ± 13.1 | 85.4 ± 14.4 | 0.19 | 0.10 | 0.01 | 0.01 |
Data are means ± SD. Except for early adulthood (men, age 21; and women, age 18), analyses were adjusted for age and diabetes status.
Overall percentage of each genotype.
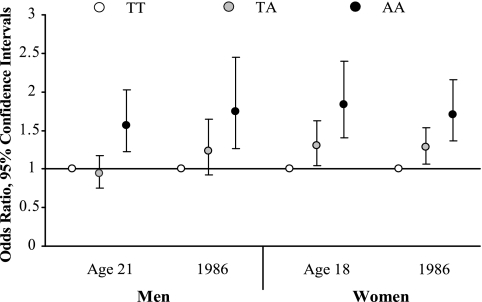
We further assessed the relation between rs9939609 and obesity risk (in 1986/1987). The AA homozygotes were associated with 1.75 (1.26–2.45) and 1.71 (1.36–2.16) times higher obesity risk in men and women, respectively (Fig. 1). Because few people were obese (2.6% in men and 3.4% in women) at early adulthood, we examined the associations between FTO genotypes and the risk of overweight (BMI ≥25 kg/m2) instead. In both men and women, the AA homozygotes were associated with 1.57 (1.22–2.03) and 1.84 (1.40–2.40) times higher overweight risk in men and women at early adulthood (Fig. 1).
FIG. 1.
Odds ratios (ORs) of overweight (BMI ≥25 kg/m2) at early adulthood and obesity (BMI ≥30 kg/m2) in 1986 associated with the TA and AA genotypes of the FTO SNP rs9939609 (T>A) compared with the AA genotype in men and women. Risk was adjusted for age and diabetes status. Error bars denote 95% CIs.
Associations with longitudinal measurements of adiposity.
rs9939609 was associated with higher BMI during the 26 years of follow-up in women (1976–2002) and was associated with BMI at nearly all time points during 16 years of follow-up in men (1986–2002) except in 1988 and 1998 (supplementary Fig. 1, which is available in an online appendix at http://dx.doi.org/10.2337/db08-0006). Similarly, the AA genotype was associated with greater obesity risk during the follow-up in women and men (except at 1992, 1996, and 2000 in men) (supplementary Fig. 2).
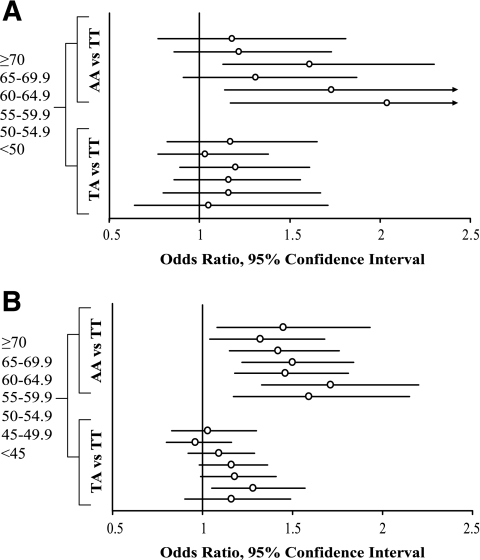
In longitudinal analyses using GEEs, associations were observed between rs9939609 and BMI and the obesity risk in both sexes (Table 3). Each allele A was associated with 0.25 (SE = 0.11; P = 0.03) and 0.59 (SE = 0.13; P < 0.0001) kg/m2 higher BMI, as well as 1.21 (1.05–1.38)–fold (P = 0.007) and 1.19 (1.07–1.31)–fold (P = 0.0008) higher risk of obesity in men and women, respectively. We further examined whether the associations between SNP rs9939609 and adiposity were consistent across different age groups (Figs. 2 and 3). It appears that the association between the SNP and obesity risk declined with older age especially in men, although tests for interaction between genotypes and age were not significant (P = 0.20 for men and 0.08 for women).
TABLE 3.
GEE analyses on the associations between rs9939609 and BMI and obesity in men (1986–2002) and women (1976–2002)
| TT | TA | AA | Per allele | P values | |
|---|---|---|---|---|---|
| Men | |||||
| BMI (kg/m2) | 26.5 ± 3.9 | 26.5 ± 3.8 | 27.1 ± 4.4 | 0.25 (0.02–0.47) | 0.03 |
| Obesity | 1.0 | 1.13 (0.90–1.41) | 1.47 (1.12–1.92) | 1.21 (1.05–1.38) | 0.007 |
| Women | |||||
| BMI (kg/m2) | 26.9 ± 5.6 | 27.5 ± 6.0 | 28.3 ± 6.3 | 0.59 (0.34–0.84) | <0.0001 |
| Obesity | 1.0 | 1.06 (0.90–1.24) | 1.46 (1.20–1.77) | 1.19 (1.07–1.31) | 0.0008 |
Data are means ± SD or OR (95% CI).
FIG. 2.
The geometric means of BMI by the genotypes of FTO SNP rs9939609 in different age groups among men (<50, 50–54.9, 55–59.5, 60–64.9, 65–69.9, and ≥70 years old) (A) and women (<45, 45–49.5, 50–54.9, 55–59.5, 60–64.9, 65–69.9, and ≥70 years old) (B). The analyses were adjusted for diabetes status. *P < 0.05.
FIG. 3.
ORs of obesity associated with the TA and AA genotypes of FTO SNP rs9939609 compared with TT genotype in different age groups of men (<50, 50–54.9, 55–59.5, 60–64.9, 65–69.9, and ≥70 years old) (A) and women (<45, 45–49.5, 50–54.9, 55–59.5, 60–64.9, 65–69.9, and ≥70 years old) (B). The analyses were adjusted for diabetes status. Error bars denote 95% CIs.
Case-control studies on type 2 diabetes.
In the crude analyses, the TA and AA genotypes were associated, respectively, with a 1.17 (1.01–1.36)–fold and 1.24 (1.02–1.50)–fold higher risk of type 2 diabetes compared with the TT genotype in women (P for trend = 0.019) (Table 4). The associations between FTO genotypes and diabetes risk became nonsignificant when adjusted for BMI. However, adjusting for other diabetes risk factors, such as age, smoking, alcohol consumption, and physical activity, did not alter the association for diabetes. This SNP was not associated with diabetes risk in men.
TABLE 4.
Associations between rs9939609 genotypes and the risk of type 2 diabetes in men and women
| Diabetic | Nondiabetic | Model 1 | P values | Model 2 | P values | Model 3 | P values | |
|---|---|---|---|---|---|---|---|---|
| Men (n = 2,287) | ||||||||
| TT | 362 (33.6) | 406 (33.5) | 1.0 | 1.0 | ||||
| TA | 486 (45.2) | 556 (45.9) | 0.98 (0.81–1.18) | 0.83 | 0.95 (0.78–1.17) | 0.64 | 0.95 (0.78–1.16) | 0.64 |
| AA | 228 (21.2) | 249 (20.6) | 1.03 (0.82–1.29) | 0.82 | 0.94 (0.73–1.21) | 0.63 | 0.99 (0.78–1.26) | 0.94 |
| Women (n = 3,520) | ||||||||
| TT | 484 (32.1) | 726 (36.0) | 1.0 | 1.0 | 1.0 | |||
| TA | 739 (49.1) | 944 (46.9) | 1.17 (1.01–1.36) | 0.036 | 1.08 (0.92–1.27) | 0.33 | 1.21 (1.03–1.43) | 0.019 |
| AA | 283 (18.8) | 344 (17.1) | 1.24 (1.02–1.50) | 0.034 | 1.02 (0.83–1.26) | 0.84 | 1.26 (1.03–1.56) | 0.029 |
Data are n (%) and OR (95% CI). Model 1, crude analysis; model 2, adjusted for BMI; model 3, adjusted for other covariates than BMI, including age, physical activity (quintiles), smoking (never, past, and current), alcohol intake (nondrinker and drinker [0.1–4.9, 5–10, or >10 g/day]), family history of diabetes, and menopausal status (pre- or postmenopausal [never, past, or current hormone use]; for women only).
Associations with adipokine concentrations in patients with type 2 diabetes.
We further assessed whether FTO SNP rs9939609 was associated with adipose-secreted adipokines. We measured leptin and adiponectin in a subset of patients with type 2 diabetes (987 women and 854 men). In women, the FTO genotypes were associated with lower plasma adiponectin levels (log[10]-transformed means: 1.82 ± 0.04, 1.73 ± 0.03, and 1.68 ± 0.05 for TT, TA, and AA genotypes, respectively; P = 0.02), adjusting for age (Fig. 4). The association remained when adjusted for smoking, alcohol consumption, physical activity, duration of diabetes, A1C, and menopausal status. Further adjustment for BMI attenuated the association. Allele A tended to be associated with higher leptin levels, with borderline significance. The genotype-associated difference in leptin disappeared when adjusted for BMI. In men, we did not find associations between FTO genotypes and adipokine levels.
FIG. 4.
The geometric means (SEs) of plasma adiponectin and leptin levels (log-transformed) by the genotypes of FTO SNP rs9939609 among women with type 2 diabetes. The multivariate analyses were adjusted for age, physical activity (quintiles), smoking (never, past, and current), alcohol intake (nondrinker and drinker [0.1–4.9, 5–10, or >10 g/day]), duration of diabetes, A1C, and menopausal status (pre- or postmenopausal [never, past, or current hormone use]).
FTO gene expression profile and in tissues/cells with high metabolic capacities.
To shed light on its potential role in adiposity, we conducted expression profiling of the FTO gene in human and mouse tissues and found similar expression patterns between the two species (supplementary Fig. 3). FTO was present at high levels in several metabolically active tissues (from humans and wild-type C56BL/6 mice), including brain, heart, kidney, and adipose tissue, with the highest expression in brain from humans and mice. In white adipose tissue isolated from db/db mice, FTO expression was reduced by ∼50% compared with lean wild-type controls (Fig. 5A). Interestingly, FTO is also expressed by macrophages and was induced by inflammatory stimulants, IFN-γ, and LPS (Fig. 5B).
FIG. 5.
Regulation of FTO expression by genetic obesity and inflammatory stimulants. A: FTO is downregulated in adipose tissue of db/db mice. Adipose tissue was harvested from lean wild-type (n = 3) and obese, diabetic db/db mice (n = 3), and gene expression was determined by real-time RT-PCR. B: FTO is induced by proinflammatory stimulants in the macrophages. Bone marrow–derived wild-type mouse macrophages were incubated with or without 2 ng/ml IFN-γ overnight followed by 10 ng/ml LPS treatment for 8 h. The experiments were done in triplicate. *P < 0.05.
DISCUSSION
In this study, we confirmed that the SNP rs9939609 was associated with higher BMI and obesity risk (1) in men and women from two independent U.S. cohorts. Frayling et al. (1) observed that the FTO genotype–associated difference in BMI occurred as early as 7 years old. We observed associations between FTO SNP and high BMI in early adulthood. The genetic effects were constant across different ages in women but tended to decrease at older ages in men. The mechanisms underlying this observation are not clear. A longitudinal twin study suggests that the genetic components regulating body weight may vary throughout life (28) and decrease with advanced age (29,30). Adiposity loss with age may partly explain the reduction in association at senior age. In addition, environmental influences accumulate with age and likely exert stronger influences on later BMI. It appears that the decreasing trend of BMI with advanced age is more pronounced in men than in women, but the test for interaction between sex and FTO was not statistically significant.
In women, rs9939609 was associated with greater risk of type 2 diabetes. Adjustment for BMI abolished the association. This finding is consistent with the observations from recent GWA studies (2,3), supporting the idea that obesity mediates the effects of FTO variant on the development of type 2 diabetes.
Adipose tissue acts as endocrine organ through secreting hormone-like adipokines, which mediate the effects of obesity on various metabolic disorders (31). Adiponectin is the most abundant adipokine in the circulation (32). Adiponectin improves insulin action and metabolism of glucose and lipids (33,34). Low blood adiponectin levels have been related to increased risk of obesity and diabetes (35,36). Our data indicated that low adiponectin levels associated with the risk allele A were secondary to the changes in BMI and may partly mediate the genetic effects on diabetes risk. The association between FTO SNP and adiponectin was observed in diabetic patients. Future studies are warranted to replicate the findings in the general population.
Little is known about the function of FTO gene. Our data comparing both human and mouse genes confirm high expression of FTO gene in brain (1). Gerken et al. (37) recently demonstrated that FTO was highly expressed in arcuate, paraventricular, dosomedial, and ventromedial nuclei. Of note, all of these sites are of critical importance in controlling energy balance. These data suggest FTO gene may affect the neuroregulation of energy balance. In addition, FTO expression was high in heart, kidney, and adipose tissues (particularly brown fat in mice).
The expression of FTO was moderately increased in adipocytes compared with preadipocytes and was substantially reduced in white adipose tissues of obese, diabetic db/db mice, indicating that it may play a role in adipocyte function but not adipogenesis. The mechanism underlying the reduced expression of FTO in adipocytes from the genetic models with direct interruptions of the leptin axis (db/db mice) is not clear. The data suggest that FTO is likely a part of the pathway mediating the neuroregulation (e.g., leptin) of energy metabolism in adipose tissue, and blocking the leptin signal may inhibit the downstream changes in adipose tissue that induce the expression of FTO. Furthermore, FTO was found to be expressed in leukocytes and was drastically upregulated in macrophages stimulated with IFN-γ and LPS. Given that metabolic dysregulation is recognized as a state of chronic inflammation (38,39), it is possible that FTO is a molecular link between metabolism and inflammation in the pathogenesis of obesity-related metabolic diseases.
SNP rs9939609 is highly correlated with many other SNPs within a 47-kb region encompassing parts of the first two introns and exon 2 of FTO gene. Sequencing the chromosomes did not result in clear candidate functional variants in the FTO coding region, minimal splice sites, or 3′-untranslated region (1). Further work is warranted to explore the genetic mechanism underpinning the observed associations.
Several limitations need to be acknowledged. Population stratification, mostly arising from either ethic admixture or genetic substructure within an ethnically homogenous group, may cause spurious associations. However, neither is likely to explain the associations observed in the present study. Our study populations are highly homogeneous by including only European whites. In addition, there is no evidence showing regional difference in rs9939606 across European countries (1).
The participants in our study do not represent random samples of U.S. men and women. However, major cohort studies, such as the Framingham Heart Study, have also not relied on national samples. Clearly, data validity is the chief prerequisite that must be fulfilled before the results can be generalized. In previous analyses, the observed genetic and environmental associations for obesity, type 2 diabetes, coronary heart disease, and other diseases in our cohorts are very similar to those found in other broadly based U.S. populations (40–44). Nonetheless, the findings in the present study need to be replicated in other ethnic groups.
Adiposity measures were self-reported in our cohorts. However, self-reported information has been reliably validated, with a high correlation with technician-measured variables (21,22). In addition, previous analyses in NHS and HPFS have demonstrated that self-reported BMI and waist circumference strongly predicted various chronic diseases (40,45,46).
We examined only one SNP, rs9939609, which was reported by the original GWA study (1). Several other SNPs were associated with obesity in subsequent studies (4,5), but these SNPs are all in strong to perfect linkage disequilibrium with rs9939609. Thus, genotyping of these SNPs would have been redundant.
In conclusion, we confirmed associations between the FTO SNP rs9939609 and higher obesity risk. Our data suggest that the genetic association for obesity may decline at older age. In addition, the genetic variant may affect circulating adiponectin levels through the changes in BMI. The expression of FTO gene was reduced in adipocytes from db/db mice. Little is known about the function of FTO gene, and thus, further investigation is warranted to identify the causal genetic variants and potential mechanisms underlying the observed genetic associations.
Supplementary Material
Acknowledgments
L.Q. has received an American Heart Association Scientist Development Award and was supported by the Boston Obesity Nutrition Research Center (DK46200). C.-H.L. has received an American Heart Association Scientist Development Award. F.B.H. has received an American Heart Association Established Investigator Award. This work has been supported by National Institutes of Health Grants DK-58845 and CA-87969.
Published ahead of print at http://diabetes.diabetesjournals.org on 22 July 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, Shields B, Harries LW, Barrett JC, Ellard S, Groves CJ, Knight B, Patch AM, Ness AR, Ebrahim S, Lawlor DA, Ring SM, Ben-Shlomo Y, Jarvelin MR, Sovio U, Bennett AJ, Melzer D, Ferrucci L, Loos RJ, Barroso I, Wareham NJ, Karpe F, Owen KR, Cardon LR, Walker M, Hitman GA, Palmer CN, Doney AS, Morris AD, Davey-Smith G, Hattersley AT, McCarthy MI: A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316: 889–894, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott LJ, Mohlke KL, Bonnycastle LL, Willer CJ, Li Y, Duren WL, Erdos MR, Stringham HM, Chines PS, Jackson AU, Prokunina-Olsson L, Ding CJ, Swift AJ, Narisu N, Hu T, Pruim R, Xiao R, Li XY, Conneely KN, Riebow NL, Sprau AG, Tong M, White PP, Hetrick KN, Barnhart MW, Bark CW, Goldstein JL, Watkins L, Xiang F, Saramies J, Buchanan TA, Watanabe RM, Valle TT, Kinnunen L, Abecasis GR, Pugh EW, Doheny KF, Bergman RN, Tuomilehto J, Collins FS, Boehnke M: A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316: 1341–1345, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeggini E, Weedon MN, Lindgren CM, Frayling TM, Elliott KS, Lango H, Timpson NJ, Perry JR, Rayner NW, Freathy RM, Barrett JC, Shields B, Morris AP, Ellard S, Groves CJ, Harries LW, Marchini JL, Owen KR, Knight B, Cardon LR, Walker M, Hitman GA, Morris AD, Doney AS, McCarthy MI, Hattersley AT: Replication of genome-wide association signals in U.K. samples reveals risk loci for type 2 diabetes. Science 316: 1336–1341, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dina C, Meyre D, Gallina S, Durand E, Korner A, Jacobson P, Carlsson LM, Kiess W, Vatin V, Lecoeur C, Delplanque J, Vaillant E, Pattou F, Ruiz J, Weill J, Levy-Marchal C, Horber F, Potoczna N, Hercberg S, Le Stunff C, Bougneres P, Kovacs P, Marre M, Balkau B, Cauchi S, Chevre JC, Froguel P: Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet 39: 724–726, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, Najjar S, Nagaraja R, Orrú M, Usala G, Dei M, Lai S, Maschio A, Busonero F, Mulas A, Ehret GB, Fink AA, Weder AB, Cooper RS, Galan P, Chakravarti A, Schlessinger D, Cao A, Lakatta E, Abecasis GR: Genome wide association scan shows genetic variants in the FTO gene are associated with obesity related traits. PLoS Genet 3: e115, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peeters A, Beckers S, Verrijken A, Roevens P, Peeters P, Van Gaal L, Van Hul W: Variants in the FTO gene are associated with common obesity in the Belgian population. Mol Genet Metab 93: 481–484, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Price RA, Li WD, Zhao H: FTO gene SNPs associated with extreme obesity in cases, controls and extremely discordant sister pairs. BMC Med Genet 9: 4, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andreasen CH, Stender-Petersen KL, Mogensen MS, Torekov SS, Wegner L, Andersen G, Nielsen AL, Albrechtsen A, Borch-Johnsen K, Rasmussen SS, Clausen JO, Sandbaek A, Lauritzen T, Hansen L, Jorgensen T, Pedersen O, Hansen T: Low physical activity accentuates the effect of the FTO rs9939609 polymorphism on body fat accumulation. Diabetes 57: 95–101, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Hunt SC, Stone S, Xin Y, Scherer CA, Magness CL, Iadonato SP, Hopkins PN, Adams TD: Association of the FTO gene with BMI. Obesity 16: 902–904, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan JT, Dorajoo R, Seielstad M, Sim X, Rick OT, Seng CK, Yin WT, Saw SM, Kai CS, Aung T, Tai ES: FTO variants are associated with obesity in the Chinese and Malay populations in Singapore. Diabetes. In press [DOI] [PMC free article] [PubMed]
- 11.Chang YC, Liu PH, Lee WJ, Chang TJ, Jiang YD, Li HY, Kuo SS, Lee KC, Chuang LM: Common variation in the fat mass and obesity-associated (FTO) gene confers risk of obesity and modulates BMI in the Chinese population. Diabetes 57: 2245–2252, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hinney A, Nguyen TT, Scherag A, Friedel S, Bronner G, Muller TD, Grallert H, Illig T, Wichmann HE, Rief W, Schafer H, Hebebrand J: Genome wide association (GWA) study for early onset extreme obesity supports the role of fat mass and obesity associated gene (FTO) variants. PLoS ONE 2: e1361, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omori S, Tanaka Y, Takahashi A, Hirose H, Kashiwagi A, Kaku K, Kawamori R, Nakamura Y, Maeda S: Association of CDKAL1, IGF2BP2, CDKN2A/B, HHEX, SLC30A8, and KCNJ11 with susceptibility to type 2 diabetes in a Japanese population. Diabetes 57: 791–795, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Canu T, Ragogna F, Scifo P, Del Maschio A, Luzi L: Serum retinol-binding protein-4, leptin, and adiponectin concentrations are related to ectopic fat accumulation. J Clin Endocrinol Metab 92: 4883–4888, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Spranger J, Kroke A, Mohlig M, Bergmann MM, Ristow M, Boeing H, Pfeiffer AF: Adiponectin and protection against type 2 diabetes mellitus. Lancet 361: 226–228, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Soodini GR: Adiponectin and leptin in relation to insulin sensitivity. Metab Syndr Relat Disord 2: 114–123, 2004 [DOI] [PubMed] [Google Scholar]
- 17.Colditz GA, Manson JE, Hankinson SE: The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health 6: 49–62, 1997 [DOI] [PubMed] [Google Scholar]
- 18.Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B, Stampfer MJ: Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 338: 464–468, 1991 [DOI] [PubMed] [Google Scholar]
- 19.National Diabetes Data Group: Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 28: 1039–1057, 1979 [DOI] [PubMed] [Google Scholar]
- 20.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20: 1183–1197, 1997 [DOI] [PubMed] [Google Scholar]
- 21.Willett W, Stampfer MJ, Bain C, Lipnick R, Speizer FE, Rosner B, Cramer D, Hennekens CH: Cigarette smoking, relative weight, and menopause. Am J Epidemiol 117: 651–658, 1983 [DOI] [PubMed] [Google Scholar]
- 22.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC: Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1: 466–473, 1990 [DOI] [PubMed] [Google Scholar]
- 23.Pischon T, Girman CJ, Hotamisligil GS, Rifai N, Hu FB, Rimm EB: Plasma adiponectin levels and risk of myocardial infarction in men. JAMA 291: 1730–1737, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Meigs JB, Li TY, Rifai N, Manson JE: Inflammatory markers and risk of developing type 2 diabetes in women. Diabetes 53: 693–700, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Lee CH, Chawla A, Urbiztondo N, Liao D, Boisvert WA, Evans RM, Curtiss LK: Transcriptional repression of atherogenic inflammation: modulation by PPARdelta. Science 302: 453–457, 2003 [DOI] [PubMed] [Google Scholar]
- 26.Zeger SL, Liang KY: Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42: 121–130, 1986 [PubMed] [Google Scholar]
- 27.Diggle PJ, Liang KY, Zeger SL: Analysis of Longitudinal Data. Oxford, U.K., Clarendon Press, 1994
- 28.Fabsitz RR, Carmelli D, Hewitt JK: Evidence for independent genetic influences on obesity in middle age. Int J Obes Relat Metab Disord 16: 657–666, 1992 [PubMed] [Google Scholar]
- 29.Stunkard AJ, Foch TT, Hrubec Z: A twin study of human obesity. JAMA 256: 51–54, 1986 [PubMed] [Google Scholar]
- 30.Korkeila M, Kaprio J, Rissanen A, Koskenvuo M: Effects of gender and age on the heritability of body mass index. Int J Obes 15: 647–654, 1991 [PubMed] [Google Scholar]
- 31.Ronti T, Lupattelli G, Mannarino E: The endocrine function of adipose tissue: an update. Clin Endocrinol 64: 355–365, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T, Engel J, Brownlee M, Scherer PE: Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin: implications for metabolic regulation and bioactivity. J Biol Chem 278: 9073–9085, 2003 [DOI] [PubMed] [Google Scholar]
- 33.Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K, Eto K, Akanuma Y, Froguel P, Foufelle F, Ferre P, Carling D, Kimura S, Nagai R, Kahn BB, Kadowaki T: Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 8: 1288–1295, 2002 [DOI] [PubMed] [Google Scholar]
- 34.Berg AH, Combs TP, Du X, Brownlee M, Scherer PE: The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 7: 947–953, 2001 [DOI] [PubMed] [Google Scholar]
- 35.Hu E, Liang P, Spiegelman BM: AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem 271: 10697–10703, 1996 [DOI] [PubMed] [Google Scholar]
- 36.Hotta K, Funahashi T, Arita Y, Takahashi M, Matsuda M, Okamoto Y, Iwahashi H, Kuriyama H, Ouchi N, Maeda K, Nishida M, Kihara S, Sakai N, Nakajima T, Hasegawa K, Muraguchi M, Ohmoto Y, Nakamura T, Yamashita S, Hanafusa T, Matsuzawa Y: Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol 20: 1595–1599, 2000 [DOI] [PubMed] [Google Scholar]
- 37.Gerken T, Girard CA, Tung YC, Webby CJ, Saudek V, Hewitson KS, Yeo GS, McDonough MA, Cunliffe S, McNeill LA, Galvanovskis J, Rorsman P, Robins P, Prieur X, Coll AP, Ma M, Jovanovic Z, Farooqi IS, Sedgwick B, Barroso I, Lindahl T, Ponting CP, Ashcroft FM, O’Rahilly S, Schofield CJ: The obesity-associated FTO gene encodes a 2-oxoglutarate-dependent nucleic acid demethylase. Science 318: 1469–1472, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H: Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112: 1821–1830, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hotamisligil GS: Inflammation and metabolic disorders. Nature 444: 860–867, 2006 [DOI] [PubMed] [Google Scholar]
- 40.Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC: Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 345: 790–797, 2001 [DOI] [PubMed] [Google Scholar]
- 41.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC: Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med 343: 16–22, 2000 [DOI] [PubMed] [Google Scholar]
- 42.Qi L, Meigs J, Manson JE, Ma J, Hunter D, Rifai N, Hu FB: HFE genetic variability, body iron stores, and the risk of type 2 diabetes in U.S. women. Diabetes 54: 3567–3572, 2005 [DOI] [PubMed] [Google Scholar]
- 43.Qi L, Zhang C, van Dam RM, Hu FB: Interleukin-6 genetic variability and adiposity: associations in two prospective cohorts and systematic review in 26,944 individuals. J Clin Endocrinol Metab 92: 3618–3625, 2007 [DOI] [PubMed] [Google Scholar]
- 44.Qi L, van Dam RM, Meigs JB, Manson JE, Hunter D, Hu FB: Genetic variation in IL6 gene and type 2 diabetes: tagging-SNP haplotype analysis in large-scale case-control study and meta-analysis. Hum Mol Genet 15: 1914–1920, 2006 [DOI] [PubMed] [Google Scholar]
- 45.Hu FB, Willett WC, Li T, Stampfer MJ, Colditz GA, Manson JE: Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med 351: 2694–2703, 2004 [DOI] [PubMed] [Google Scholar]
- 46.Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson RR, Speizer FE, Hennekens CH: A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 322: 882–889, 1990 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.