Abstract
Inflammation induces marked changes in lipid and lipoprotein metabolism. Proprotein convertase subtilisin kexin 9 (PCSK9) plays an important role in regulating LDL receptor degradation. Here we demonstrate that LPS decreases hepatic LDL receptor protein but at the same time hepatic LDL receptor mRNA levels are not decreased. We therefore explored the effect of LPS on PCSK9 expression. LPS results in a marked increase in hepatic PCSK9 mRNA levels (4 hours-2.5 fold increase; 38 hours-12.5 fold increase). The increase in PCSK9 is a sensitive response with 1 ug LPS inducing a ½ maximal response. LPS also increased PCSK9 expression in the kidney. Finally, zymosan and turpentine, other treatments that induce inflammation, also stimulated hepatic expression of PCSK9. Thus, inflammation stimulates PCSK9 expression leading to increased LDL receptor degradation and decreasing LDL receptors thereby increasing serum LDL, which could have beneficial effects on host defense.
Keywords: Endotoxin, Zymosan, LDL receptor, Infection, Serum LDL
INTRODUCTION
Infection and inflammation induce marked changes in lipid and lipoprotein metabolism (for review see [1]). In rodents, LPS administration, a frequently used model for gram negative bacterial infection, increases VLDL and LDL levels while decreasing HDL levels [1]. Studies have shown that LPS administration decreases LDL receptor protein levels in the liver, which could lead to the decreased clearance of circulating LDL and account for the increase in serum LDL levels [2, 3]. However, the effects of LPS administration on LDL receptor mRNA expression in the liver have been variable with decreases in LDL receptor mRNA levels observed soon after LPS administration followed by increases in LDL receptor mRNA levels at later time points [2–4]. In contrast, the decrease in LDL receptor protein levels occurs rapidly after LPS administration and persists for an extended period of time [2, 3]. These results suggest that while the initial decrease in hepatic LDL receptors could be due to a decrease in LDL receptor mRNA levels the decrease observed at later time points must be due to other regulatory pathways.
Recent studies have shown that proprotein convertase subtilisin kexin 9 (PCSK9), a serine protease, plays an important role in regulating hepatic LDL receptor levels [5, 6]. Overexpression of PCSK9 in mice results in a marked decrease in hepatic LDL receptors and an increase in serum LDL [7–10]. Conversely, PCSK9 deficient mice (knock-out or antisense) have a marked increase in hepatic LDL receptors and a 50% decrease in serum cholesterol due to the increased clearance of LDL and HDL by the liver [11, 12]. Together these studies indicate that PCSK9 plays an important role in regulating hepatic LDL receptor protein levels and consequently serum cholesterol levels. Moreover, parabiosis studies have demonstrated that PCSK9 from a transgenic overexpressor mouse reduced LDL receptor levels in the liver of the paired nontransgenic mouse [13]. Similarly, the administration of recombinant human PCSK9 to mice also reduced hepatic LDL receptors by approximately 90% within 60 minutes [14, 15]. Together these observations indicate that circulating PCSK9 lowers LDL receptor levels. Furthermore studies have shown that PCSK9 binds to the LDL receptor on the plasma membrane leading to the redistribution of LDL receptors from the cell surface to lysosomes and their ultimate degradation [15–17].
Based on these observations we hypothesized that infection and inflammation stimulates the expression of PCSK9 in the liver thereby decreasing hepatic LDL receptor protein levels resulting in increases in circulating LDL levels.
MATERIALS AND METHODS
Materials
LPS (Escherichia coli 55:B5) was obtained from Difco Laboratories and diluted in pyrogenfree 0.9% saline. Zymosan A and TRI Reagent were purchased from Sigma (St. Louis, MO). Oil of turpentine was purchased from BDH Laboratory Supplies (Poole, England). LightCycler ® 450 SYBR Green I Master was purchased from Roche Applied Science (Indianapolis, IN), and iScript cDNA Synthesis Kit from BIO-RAD (Hercules, CA).
Animals
Female C57BL/6 mice (8 weeks old) were obtained from Charles River Laboratories (Wilmington, MA). The animals were maintained in a normal-light-cycle room and were fed Purina mouse chow (Ralston Purina, St. Louis, MO) and water ad libitum. The high cholesterol diet was prepared by adding cholesterol to powdered mouse chow (2%). Animals were fed the high cholesterol diet for 7 days. Animals were injected with saline, LPS (5 mg/kg body weight, intraperitoneally), or zymosan A (80 mg/kg body weight, intraperitoneally) or Oil of Turpentine (100 µl subcutaneously in left hind leg) and food was removed from both control and treated animals after injection. These doses of LPS, zymosan, and turpentine were previously shown to induce the acute phase response in mice, but are far below the lethal dose [18]. At the indicated time after treatment, animals were administered halothane anesthesia and euthanized and liver and kidney were snap-frozen in liquid nitrogen, placed in storage tubes in a dry ice bath until the end of experiment, and then stored at −80°C until RNA extraction. All experiments were performed according to protocols approved by the Animal Studies Subcommittee of the San Francisco Veteran Affairs Medical Center.
Isolation of RNA and RT-PCR
Total RNA was isolated from 50 mg of snap-frozen liver and kidney tissue by the TRI Reagent method from Sigma. Total RNA was then quantified by measuring absorption at 260 nm. The reverse-transcription reagent iScript from BIO-RAD was used to prepare first strand cDNA for Quantitative RT-PCR from 1µg of total RNA. Real-time quantitative PCR was performed in the MX300P™ real-time PCR instrument (Stratagene, La Jolla, CA) using LightCycler® 480 SYBR Green I Master (Roche, Indianapolis, IN). The relative amount of all mRNAs was calculated using the comparative CT method. 36B4 mRNA was used as the invariant control for all experiments. QPCR primers are as follows:
| PCSK9 | mouse | 5’-TTGCAGCAGCTGGGAACTT-3’ |
| 5’-CCGACTGTGATGACCTCTGGA-3’ | ||
| LDLR | mouse | 5’-AGGCTGTGGGCTCCATAGG-3’ |
| 5’-TGCGGTCCAGGGTCATCT-3’ | ||
| 36B4 | human/mouse | 5’-GCGACCTGGAAGTCCAACTAC-3’ |
| 5’-ATCTGCTGCATCTGCTTGG-3’ |
Western Blot Analysis
Mouse liver membrane proteins were purified using Mem-Per kit (Pierce). SDS-PAGE was performed on 50 µg aliquots of membrane protein under reducing conditions. The samples were electrophoresed on an 8% gel using a minigel apparatus (Bio-Rad). The proteins were electrotransferred to a PVDF membrane (Amersham) followed by blocking with SuperBlock Blocking Buffer (Pierce). After washing with PBS containing 0.1% Tween-20, the membrane was incubated with either goat anti-mouse LDL receptor primary antibody (R&D Systems) at 1:1000 dilution overnight at 4°C. After repeat washing, the membrane was incubated with the anti-goat IgG HRP (Jackson ImmunoResearch) and signal was detected with ECL Plus (Amersham).
Statistical analysis
Data are expressed as the mean ± S.E. from experiments with 4–5 animals. The statistical difference between two experimental groups was determined using the Student’s t test.
RESULTS AND DISCUSSION
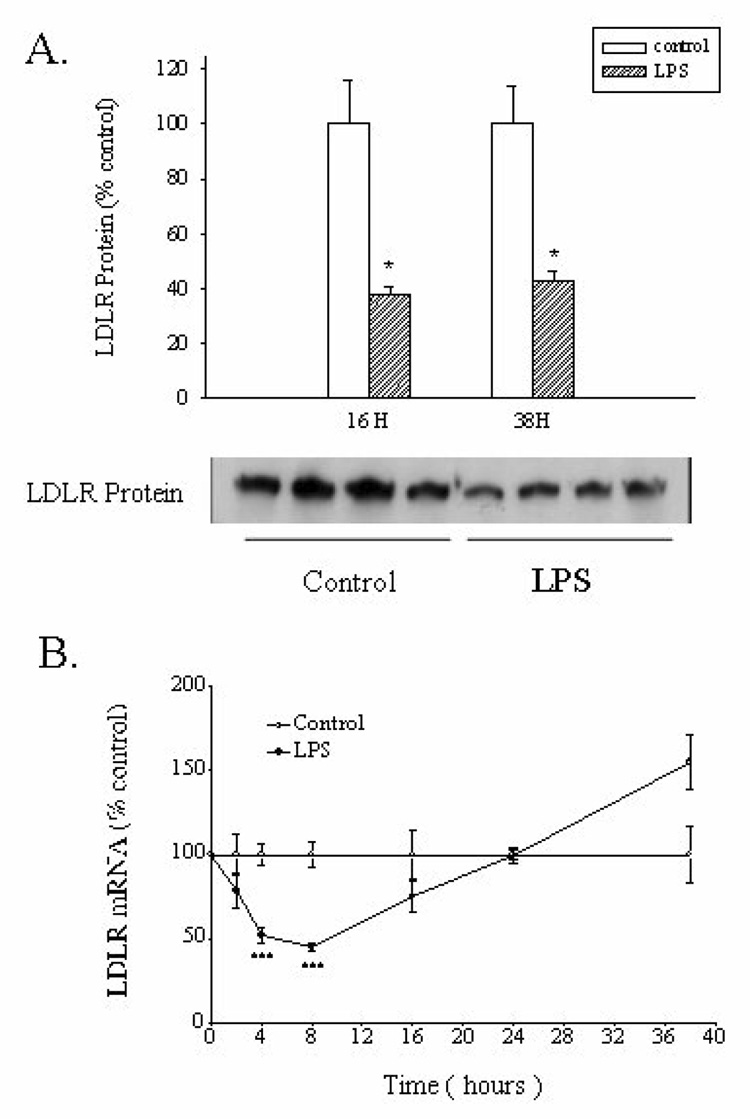
Our initial experiments determined the effect of the administration of LPS, a TLR 4 activator, on hepatic LDL receptor protein levels. As reported by other investigators, LPS treatment resulted in a marked decrease in LDL receptor protein levels in the liver (~60% decrease) (Figure 1A) [2, 3]. Figure 1B shows the effect of LPS on hepatic LDL receptor mRNA levels. As reported by other investigators [3], we also observed an early decrease in LDL receptor mRNA levels (50% decrease at 4 and 8 hours) but at later time points LDL receptor mRNA levels returned towards normal and by 38 hours were actually increased to 50% greater than controls. Thus, while the initial decrease in LDL receptor mRNA levels could contribute to the early decrease in LDL receptor protein levels, the late decrease in LDL receptor protein levels is unlikely to be accounted for by decreases in LDL receptor mRNA levels. We therefore explored the effect of LPS on other pathways that regulate LDL receptor protein levels.
Fig. 1. Effect of LPS administration on the expression of the LDL receptor in mouse liver.
Mice were injected intraperitoneally with LPS (5mg/kg body weight). The animals were euthanized at the indicated times after LPS administration. Liver membranes and Western blots were carried out as described in the Materials and Methods section. Total RNA was isolated from liver tissue, cDNA was synthesized with reverse transcriptase, and quantitative real-time PCR performed as described in Materials and Methods section. A. LDL receptor protein levels at 16 and 38 hours post LPS administration. B. LDL receptor mRNA levels at various times after LPS administration. The data are presented as the mean +/− SEM. Data are expressed as a percentage of controls. N=4–5 per group. * p< 0.01, *** p< 0.001
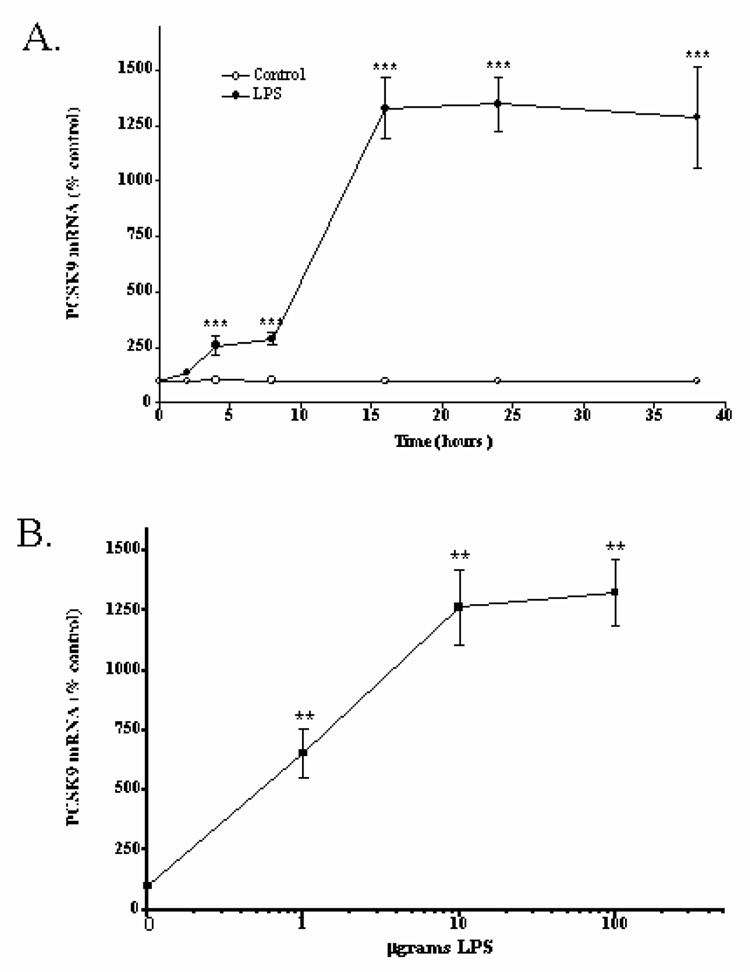
As shown in Figure 2, LPS treatment results in a marked increase in PCSK9 mRNA levels. The increase is seen as early as 4 hours following LPS treatment (2.5 fold increase) and is sustained for as long as 38 hours (12.5 fold increase) (Figure 2A). Additionally, the increase in PCSK9 is a relatively sensitive response to LPS with 1 µg LPS inducing a ½ maximal response (approximately 6 fold increase) (Figure 2B).
Fig. 2. Effect of LPS administration on the expression of PCSK9 in mouse liver.
Total RNA was isolated from liver tissue, cDNA was synthesized with reverse transcriptase, and quantitative real-time PCR performed as described in Materials and Methods section. A. Time course. Mice were injected intraperitoneally with LPS (5mg/kg body weight) and the animals were euthanized at the indicated times after LPS administration. B. Dose Response. Mice were injected intraperitoneally with the indicated dose of LPS and the animals were euthanized 16 hours after LPS administration. The data are presented as the mean +/− SEM. Data are expressed as a percentage of controls. N=4–5 per group. ** p< 0.005, *** p< 0.001
It is well recognized that PCSK9 expression is stimulated by SREBP-2 [10, 19, 20], a transcription factor whose activity is suppressed by increases in hepatic cholesterol content [21]. Cholesterol feeding increases hepatic cholesterol levels and down regulates SREBP-2 activity and therefore we next determined if LPS treatment could increase PCSK9 in cholesterol fed animals. In control animals fed the high cholesterol diet, the CT for PCSK9 was 31.1+/− 0.21, whereas in control animals fed the chow diet the CT was 29.0+/− 0.31, indicating that cholesterol feeding, presumably by decreasing SREBP activation, decreases PCSK9 expression. Nevertheless, LPS treatment increased PCSK9 mRNA levels in the liver of cholesterol fed mice by approximately 6 fold. If increases in SREBP activity mediated the LPS induced increase in PCSK9 mRNA levels one would have expected the effect of LPS to be markedly blunted in cholesterol fed mice. Moreover, if increases in SREBP activity caused the increase in PCSK9 expression one would also expect that LDL receptor mRNA levels would also be increased as SREBP-2 is well known to be a potent stimulator of LDL receptor gene expression [21]. However, our results demonstrate a discordance in expression of LDL receptor mRNA and PCSK9 mRNA (at 8 hours PCSK9 expression is increased 2–3 fold while LDL receptor expression is decreased by 50%) providing further evidence suggesting that increases in SREBP activity are not likely to underlie the changes in PCSK9 expression.
PCSK9 is produced in tissues other than the liver [6]. To determine if the ability of LPS to stimulate PCSK9 expression is liver specific we next determined the effect of LPS administration on PCSK9 mRNA levels in the kidney. LPS treatment increased PCSK9 mRNA levels by 3 fold in the kidney indicating that the stimulatory effect of inflammation on PCSK9 expression is not limited to the liver.
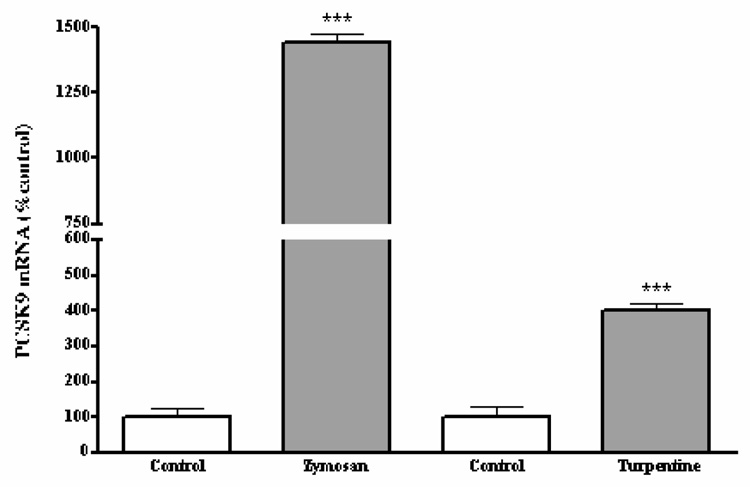
We next determined if other treatments that induce inflammation and the acute phase response also effected the expression of PCSK9. As shown in figure 3, the administration of zymosan, a fungal product that activates TLR2, also results in a marked increase in PCSK9 mRNA levels in the liver (~14 fold increase). Similarly, the intramuscular administration of turpentine, which causes a sterile abscess, increased hepatic PCSK9 mRNA levels 3–4 fold (figure 3). The smaller induction of PCSK9 that occurs with turpentine treatment compared to either LPS or zymosan administration is not surprising given that the degree of inflammation induced by turpentine treatment is less than that produced by the other treatments.
Fig. 3. Effect of zymosan and turpentine treatment on the expression of PCSK9 in mouse liver.
Mice were injected intraperitoneally with zymosan (80mg/kg body weight) or subcutaneously with turpentine (100ul) and euthanized 16 hours after treatment. Total RNA was isolated from liver tissue, cDNA was synthesized with reverse transcriptase, and quantitative real-time PCR performed as described in Materials and Methods section. The data are presented as the mean +/− SEM. Data are expressed as a percentage of controls. N=4–5 per group. *** p< 0.001 vs. control.
Unfortunately we were unable to measure changes in PCSK9 protein levels following LPS administration in either mouse liver or serum despite attempts with several commercial antibodies. While there are good assays for measuring PCSK9 in human serum such assays are not available for the mouse. In reviewing the literature, mouse PCKS9 protein levels are measured almost exclusively in animals that are markedly overexpressing PCSK9 protein.
The mechanism by which inflammation stimulates the expression of PCSK9 is unknown. As discussed above, during inflammation it is unlikely that activation of SREBP accounts for the changes given the results in cholesterol fed animals and the discordance between PCSK9 and LDL receptor expression. Recent studies have shown that activation of either FXR or PPAR alpha inhibits the expression of PCSK9 [22–24]. Studies by our laboratory have shown that the levels of both of these nuclear hormone receptor transcription factors, as well as their obligate heterodimer partner RXR, are decreased during inflammation in both the liver and kidney and therefore it is possible that the increase in PCSK9 is due to decreases in the activity of FXR and/or PPAR alpha [25–27].
In conclusion, the present study demonstrates that infection and inflammation stimulates the expression of PCSK9, which would result in the increased degradation of LDL receptors thereby increasing serum LDL levels. The increase in serum LDL could have beneficial effects on host defense by binding and neutralizing LPS and other toxins or by providing a source of cholesterol to macrophages and other cells that play a crucial role in host defense [1].
Acknowledgements
This work was supported by grants from the Research Service of the Department of Veterans Affairs and by National Institutes of Health Grant 5 RO1 AR049932.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Khovidhunkit W, Kim MS, Memon RA, Shigenaga JK, Moser AH, Feingold KR, Grunfeld C. Effects of infection and inflammation on lipid and lipoprotein metabolism: mechanisms and consequences to the host. J Lipid Res. 2004;45:1169–1196. doi: 10.1194/jlr.R300019-JLR200. [DOI] [PubMed] [Google Scholar]
- 2.Li L, Thompson PA, Kitchens RL. Infection induces a positive acute phase apolipoprotein E response from a negative acute phase gene: role of hepatic LDL receptors. J Lipid Res. 2008 doi: 10.1194/jlr.M800172-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liao W, Rudling M, Angelin B. Endotoxin suppresses rat hepatic low-density lipoprotein receptor expression. Biochem J. 1996;313(Pt 3):873–878. doi: 10.1042/bj3130873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feingold KR, Pollock AS, Moser AH, Shigenaga JK, Grunfeld C. Discordant regulation of proteins of cholesterol metabolism during the acute phase response. J Lipid Res. 1995;36:1474–1482. [PubMed] [Google Scholar]
- 5.Horton JD, Cohen JC, Hobbs HH. Molecular biology of PCSK9: its role in LDL metabolism. Trends Biochem Sci. 2007;32:71–77. doi: 10.1016/j.tibs.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez D. PCSK9: an enigmatic protease. Biochim Biophys Acta. 2008;1781:184–191. doi: 10.1016/j.bbalip.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Benjannet S, Rhainds D, Essalmani R, Mayne J, Wickham L, Jin W, Asselin MC, Hamelin J, Varret M, Allard D, Trillard M, Abifadel M, Tebon A, Attie AD, Rader DJ, Boileau C, Brissette L, Chretien M, Prat A, Seidah NG. NARC-1/PCSK9 and its natural mutants: zymogen cleavage and effects on the low density lipoprotein (LDL) receptor and LDL cholesterol. J Biol Chem. 2004;279:48865–48875. doi: 10.1074/jbc.M409699200. [DOI] [PubMed] [Google Scholar]
- 8.Lalanne F, Lambert G, Amar MJ, Chetiveaux M, Zair Y, Jarnoux AL, Ouguerram K, Friburg J, Seidah NG, Brewer HB, Jr, Krempf M, Costet P. Wild-type PCSK9 inhibits LDL clearance but does not affect apoB-containing lipoprotein production in mouse and cultured cells. J Lipid Res. 2005;46:1312–1319. doi: 10.1194/jlr.M400396-JLR200. [DOI] [PubMed] [Google Scholar]
- 9.Maxwell KN, Breslow JL. Adenoviral-mediated expression of Pcsk9 in mice results in a low-density lipoprotein receptor knockout phenotype. Proc Natl Acad Sci U S A. 2004;101:7100–7105. doi: 10.1073/pnas.0402133101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park SW, Moon YA, Horton JD. Post-transcriptional regulation of low density lipoprotein receptor protein by proprotein convertase subtilisin/kexin type 9a in mouse liver. J Biol Chem. 2004;279:50630–50638. doi: 10.1074/jbc.M410077200. [DOI] [PubMed] [Google Scholar]
- 11.Graham MJ, Lemonidis KM, Whipple CP, Subramaniam A, Monia BP, Crooke ST, Crooke RM. Antisense inhibition of proprotein convertase subtilisin/kexintype 9 reduces serum LDL in hyperlipidemic mice. J Lipid Res. 2007;48:763–767. doi: 10.1194/jlr.C600025-JLR200. [DOI] [PubMed] [Google Scholar]
- 12.Rashid S, Curtis DE, Garuti R, Anderson NN, Bashmakov Y, Ho YK, Hammer RE, Moon YA, Horton JD. Decreased plasma cholesterol and hypersensitivity to statins in mice lacking Pcsk9. Proc Natl Acad Sci U S A. 2005;102:5374–5379. doi: 10.1073/pnas.0501652102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagace TA, Curtis DE, Garuti R, McNutt MC, Park SW, Prather HB, Anderson NN, Ho YK, Hammer RE, Horton JD. Secreted PCSK9 decreases the number of LDL receptors in hepatocytes and in livers of parabiotic mice. J Clin Invest. 2006;116:2995–3005. doi: 10.1172/JCI29383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grefhorst A, McNutt MC, Lagace TA, Horton JD. Plasma PCSK9 preferentially reduces liver LDL receptors in mice. J Lipid Res. 2008;49:1303–1311. doi: 10.1194/jlr.M800027-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qian YW, Schmidt RJ, Zhang Y, Chu S, Lin A, Wang H, Wang X, Beyer TP, Bensch WR, Li W, Ehsani ME, Lu D, Konrad RJ, Eacho PI, Moller DE, Karathanasis SK, Cao G. Secreted PCSK9 downregulates low density lipoprotein receptor through receptor-mediated endocytosis. J Lipid Res. 2007;48:1488–1498. doi: 10.1194/jlr.M700071-JLR200. [DOI] [PubMed] [Google Scholar]
- 16.Fisher TS, Lo Surdo P, Pandit S, Mattu M, Santoro JC, Wisniewski D, Cummings RT, Calzetta A, Cubbon RM, Fischer PA, Tarachandani A, De Francesco R, Wright SD, Sparrow CP, Carfi A, Sitlani A. Effects of pH and low density lipoprotein (LDL) on PCSK9-dependent LDL receptor regulation. J Biol Chem. 2007;282:20502–20512. doi: 10.1074/jbc.M701634200. [DOI] [PubMed] [Google Scholar]
- 17.Zhang DW, Lagace TA, Garuti R, Zhao Z, McDonald M, Horton JD, Cohen JC, Hobbs HH. Binding of proprotein convertase subtilisin/kexin type 9 toepidermal growth factor-like repeat A of low density lipoprotein receptor decreases receptor recycling and increases degradation. J Biol Chem. 2007;282:18602–18612. doi: 10.1074/jbc.M702027200. [DOI] [PubMed] [Google Scholar]
- 18.Memon RA, Staprans I, Noor M, Holleran WM, Uchida Y, Moser AH, Feingold KR, Grunfeld C. Infection and inflammation induce LDL oxidation in vivo. Arterioscler Thromb Vasc Biol. 2000;20:1536–1542. doi: 10.1161/01.atv.20.6.1536. [DOI] [PubMed] [Google Scholar]
- 19.Dubuc G, Chamberland A, Wassef H, Davignon J, Seidah NG, Bernier L, Prat A. Statins upregulate PCSK9, the gene encoding the proprotein convertase neural apoptosis-regulated convertase-1 implicated in familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2004;24:1454–1459. doi: 10.1161/01.ATV.0000134621.14315.43. [DOI] [PubMed] [Google Scholar]
- 20.Jeong HJ, Lee HS, Kim KS, Kim YK, Yoon D, Park SW. Sterol-dependent regulation of proprotein convertase subtilisin/kexin type 9 expression by sterol-regulatory element binding protein-2. J Lipid Res. 2008;49:399–409. doi: 10.1194/jlr.M700443-JLR200. [DOI] [PubMed] [Google Scholar]
- 21.Brown MS, Goldstein JL. The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell. 1997;89:331–340. doi: 10.1016/s0092-8674(00)80213-5. [DOI] [PubMed] [Google Scholar]
- 22.Kourimate S, Le May C, Langhi C, Jarnoux AL, Ouguerram K, Zair Y, Nguyen P, Krempf M, Cariou B, Costet P. Dual mechanisms for the fibrate-mediated repression of proprotein convertase subtilisin/kexin type 9. J Biol Chem. 2008;283:9666–9673. doi: 10.1074/jbc.M705831200. [DOI] [PubMed] [Google Scholar]
- 23.Lambert G, Jarnoux AL, Pineau T, Pape O, Chetiveaux M, Laboisse C, Krempf M, Costet P. Fasting induces hyperlipidemia in mice overexpressing proprotein convertase subtilisin kexin type 9: lack of modulation of very-low-density lipoprotein hepatic output by the low-density lipoprotein receptor. Endocrinology. 2006;147:4985–4995. doi: 10.1210/en.2006-0098. [DOI] [PubMed] [Google Scholar]
- 24.Langhi C, Le May C, Kourimate S, Caron S, Staels B, Krempf M, Costet P, Cariou B. Activation of the farnesoid X receptor represses PCSK9 expression in human hepatocytes. FEBS Lett. 2008;582:949–955. doi: 10.1016/j.febslet.2008.02.038. [DOI] [PubMed] [Google Scholar]
- 25.Beigneux AP, Moser AH, Shigenaga JK, Grunfeld C, Feingold KR. The acute phase response is associated with retinoid X receptor repression in rodent liver. J Biol Chem. 2000;275:16390–16399. doi: 10.1074/jbc.M000953200. [DOI] [PubMed] [Google Scholar]
- 26.Kim MS, Shigenaga J, Moser A, Feingold K, Grunfeld C. Repression of farnesoid X receptor during the acute phase response. J Biol Chem. 2003;278:8988–8995. doi: 10.1074/jbc.M212633200. [DOI] [PubMed] [Google Scholar]
- 27.Kim MS, Sweeney TR, Shigenaga JK, Chui LG, Moser A, Grunfeld C, Feingold KR. Tumor necrosis factor and interleukin 1 decrease RXRalpha, PPARalpha, PPARgamma, LXRalpha, and the coactivators SRC-1, PGC-1alpha, and PGC-1beta in liver cells. Metabolism. 2007;56:267–279. doi: 10.1016/j.metabol.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]