Abstract
Alcohol dependence (AD) is a complex and heterogeneous disorder. The identification of more homogeneous subgroups of individuals with drinking problems and the refinement of the diagnostic criteria are inter-related research goals. They have the potential to improve our knowledge of etiology and treatment effects, and to assist in the identification of risk factors or specific genetic factors. Mixture modeling has advantages over traditional modeling that focuses on either the dimensional or categorical latent structure. The mixture modeling combines both latent class and latent trait models, but has not been widely applied in substance use research. The goal of the present study is to assess whether the AD criteria in the population could be better characterized by a continuous dimension, a few discrete subgroups, or a combination of the two. More than seven thousand participants were recruited from the population-based Virginia Twin Registry, and were interviewed to obtain DSM-IV (Diagnostic and Statistical Manual of Mental Disorder, version IV) symptoms and diagnosis of AD. We applied factor analysis, latent class analysis, and factor mixture models for symptom items based on the DSM-IV criteria.
Our results showed that a mixture model with one factor and three classes for both genders fit well. The three classes were a non-problem drinking group and severe and moderate drinking problem groups. By contrast, models constrained to conform to DSM-IV diagnostic criteria were rejected by model fitting indices providing empirical evidence for heterogeneity in the AD diagnosis. Classification analysis showed different characteristics across subgroups, including alcohol-caused behavioral problems, comorbid disorders, age at onset for alcohol-related milestones, and personality. Clinically, the expanded classification of AD may aid in identifying suitable treatments, interventions and additional sources of comorbidity based on these more homogenous subgroups of alcohol use problems.
Keywords: latent trait, latent class, mixture model, diagnosis
1. Introduction
Alcohol abuse or dependence (AAD) is a clinically heterogeneous condition, with affected individuals varying in age of onset, clinical presentation, comorbid psychopathology, and severity. The diagnosis of AAD is usually based on subjective self-report symptoms or behaviors, as opposed to biological markers or known indices of pathophysiology. According to the DSM-IV (Diagnostic and Statistical Manual of Mental Disorder, version IV, American Psychiatric Association, 1994), individuals who meet three or more of seven criteria at any time in a year period are diagnosed as having alcohol dependence (AD). One of the assumptions behind this sum-score based diagnosis system is that each symptom provides the same amount of information as to whether an individual is affected. This assumption is typically not tested and is probably unrealistic. A further problem with the requirement of any combination of three out of seven symptoms is that those meeting criteria may be quite heterogeneous. Such variation between subjects with the same classification may hamper attempts to identify risk factors, prognosis or effective treatments. Therefore, the identification of more homogeneous groups of individuals with alcohol problems is an important research goal in this field.
A fundamental question for complex behavioral traits or disorders is whether individual differences in the trait have a single underlying continuous liability (risk factor), representing a situation where individuals differ with respect to severity, or whether the differences stem from qualitatively different subtypes (Pickles and Angold, 2003; Waller and Meehl, 1997). For these purposes, there are two main statistical methods. The common factor analysis (FA) is a variable-centered approach designed to model an underlying continuous dimension of diagnostic symptoms. Typically, these underlying dimensions (or ‘factors’) are assumed to be normally distributed. Their influence on two or more symptoms generates covariation between the symptoms, and it is these patterns of symptom covariation that suggest the presence of latent factors.
An alternative statistical framework is that of latent class analysis (LCA), which is a person-centered approach that can be used to explore the spectrum of severity based on an individual's profile of symptoms (Lazarsfeld and Henry, 1968; Moustaki, 1996). Usually, LCA assumes that symptom covariation in the population arises solely because the population consists of two or more subgroups. These subgroups differ in the means or variances of at least two of the symptoms. For example, if in one group both withdrawal and tolerance symptoms are more frequently endorsed than in a second group, it would appear that these symptoms covary in the combined population, even if there was no correlation between the symptoms within either of the groups.
In the past, several studies have investigated the dimensional structure of alcohol problems and whether there are distinct classes of individuals with respect to heavy alcohol use. Factor analysis suggested a unidimensional structure of the AD syndromes in a clinical sample (Allen et al., 1993). Using all DSM-IV alcohol diagnostic criteria, some studies supported a unidimensional structure for alcohol problems using a Rasch model and latent trait modeling (Krueger et al., 2004; Kahler and Strong, 2006; Proudfoot et al., 2006; Saha et al., 2006), while others suggested a two-dimensional model (i.e. the abuse and dependence items fall into different factors). Krueger and colleagues (2004) conducted a comprehensive examination of 110 alcohol problems. Although they suggested that alcohol problems can be organized along a continuum severity, the performance of DSM-III-R abuse and dependence was quite different when comparing the relative shapes of the severity indexes by the set of items measured in a specific diagnostic category. The abuse items followed a bi-model distribution with items found in both the mild and severe ends of the continuum, whereas the dependence items tended to be located at the severe end of the continuum. Nelson and colleagues' (1999) findings supported a two-factor solution in a mixed population and clinical sample for dependence and abuse. Using large-scale data from the National Longitudinal Survey, Harford and Muthen (2001) found a two-dimensional structure with one main factor on AD; they also provided further support for the validity of AD in general population samples. While it is still in debate whether abuse should be included in the same continuum as dependence, AD appears to be a more reliable unitary construct. In addition, two prospective studies used general population samples have indicated that the course of AD differs from that of abuse (Hasin et al., 1990; Hasin et al., 1997), and implied that alcohol dependence and abuse are different in nature. Because alcohol abuse and dependence also have different features in terms of their clinical presentation, etiology and demographic characteristics (Hasin et al., 2007), we focus on only alcohol dependence for the present study.
On the other hand, results from the LCA studies consistently showed a severity-based grouping in both adult and adolescent samples. A four-class solution has been identified for both genders among adult relatives of alcoholic probands, in which classes were distinguished primarily by increasing probability of endorsement (Bucholz et al., 1996). Using a large Australian twin sample, Lynskey and colleagues' (2005) results revealed a severity-based 4-class solution in females and a 5-class solution in males based on eleven DSM-IV dependence and abuse symptoms. For adolescent samples, a 5-class severity-based solution was reported for female twins (Bucholz et al., 2000) and a 3-class solution represented increasing severity of alcohol problems among adolescents in addiction treatment program (Chung and Martin, 2001).
Conceptually, FA and LCA provide different explanations of the covariation among symptoms. Historically, they have been applied independently and typically for different purposes. Yet it is possible to compare the fit of these models using omnibus model fitting indices, such as log-likelihood or parsimony-based indices such as Akaike's Information Criterion (AIC, Akaike, 1974) or Bayesian Information Criterion (BIC, Schwarz, 1978) that take into account the number of parameters estimated in the models. For example, LCA and latent-trait response models were applied separately on symptoms of major depression (MD) based on DSM-III-R criteria in a population based twin sample (Aggen et al., 2005; Sullivan et al., 2002). Results from LCA suggested seven latent classes that had interpretable profiles corresponding to typical MD, atypical MD, and minor depressive states (Sullivan et al., 2002). The factor and item response model applied to the same data identified a unidimensional scale of depression liability (Aggen et al., 2005). These studies illustrate an important point – that the same set of symptoms can be used to estimate both their defining properties of a unidimensional continuous scale of liability or unobserved class membership structures – neither of which would be possible if symptoms had been aggregated into an affected vs. unaffected binary diagnostic variable.
In the last decade, efforts to identify unobserved heterogeneity have led to the development of advanced structural equation models. Only recently have the two concepts (continuous dimensionality and categorical subtypes) been unified in a single combined model (Dolan and Van der Maas, 1998; Muthen and Shedden, 1999; Yung, 1997), usually called a ‘Factor Mixture Model (FMM)'. FMM's are a variant of finite mixture models (Everitt, 1988; Jedidi et al., 1997; McLachlan and Peel, 2000) which consist of a limited number of mixture components (the latent class model is also a finite mixture model). The FMM features two types of latent variables, namely a latent categorical variable, and one or more continuous factors within each class. It can be used as a tool to address the discrimination between latent classes on the one hand, and continuous dimensions on the other (i.e. if there exist underlying dimensions for the symptoms covariation, whether there are heterogeneous subgroups in the general population). The hope is that these models can provide superior measurements and classification of complex phenotypes. One of the implications of the availability of these new techniques is to provide empirical findings that will help inform decisions to refine the DSM criteria and possible subtypes. Nevertheless, only a few studies have employed the mixture models to study problematic behaviors and substance use. With cross-sectional data, mixture models were applied to tobacco dependence data and they fitted data better than either latent-trait or LCA models (Muthen and Asparouhov, 2006); (Muthen, 2006). Different kinds of combined mixture models have also been applied in longitudinal studies to explore subgroups with different growth trajectories. For instance, growth mixture modeling was applied to antisocial behavior and heavy drinking (Muthen and Muthen, 2000) and applied to assess intervention effects of reducing aggressive behavior (Muthen et al., 2002).
The present study links the variable-centered (latent trait) and person-centered (latent class) approaches in the substance use literature for AD. Our goal is to assess whether the factor structure, latent class, or finite mixture models provide better explanations of the patterns of symptoms co-occurrence for AD in a large population-based sample. In addition, a series of exogenous variables were also included in the analysis to validate whether there are distinguishable subgroups of problematic alcohol use.
2. Methods
2.1. Sample and assessment procedures
Subjects in this study were participants in the Virginia Adult Twin Study of Psychiatric and Substance Use Disorders and were recruited from the population-based Virginia Twin Registry (now part of the Mid-Atlantic Twin Registry). Longitudinal data were collected from female-female twin pairs (FF) who participated in up to four personal interviews and from male-male and male-female twin pairs (MM/MF) who participated in one or two waves of interviews. The current report is based on individuals with completed interviews, including 3325 females with a mean age when last assessed of 36.5 years (range 20-62) and 4217 males with mean age of 37.0 years (range 20-58). Details of sample ascertainment and characteristics are presented elsewhere (Kendler et al., 2004).
The DSM-IV symptoms and diagnosis of AD were assessed using adapted versions of standard structured interviews, SCID (the Structured Clinical Interview for DSM-III-R) (Bucholz et al., 1994; Spitzer and Williams, 1985). The individual symptoms of AD include tolerance (TOL), withdrawal symptoms (WD), drinking more than intended (MORE), unsuccessful attempts to cut down on use (CUT), excessive time related to alcohol (TIME), impaired social or work activities (IMP), and use despite physical consequences (PHY). Lifetime DSM-IV AD history was assessed at waves 4 for the FF sample (FF4) and waves 2 for the MM/MF sample (MM/MF2). The interview used to assess the DSM-IV AD criteria contained a stem item. Individuals who answered no to “have you ever taken a drink in your lifetime” skipped out the rest of AD assessment section. In total, there were 226 individuals reporting they never had taken a drink in their lifetime. For these abstainers, we assumed all DSM-IV symptom criteria were negative and coded them 0. Therefore, abstainers were not distinguished from individuals who did drink but never developed any alcohol problems meeting the DSM-IV criteria1.
Randomly selected sub-samples from FF4 (N=192) and MM/MF2 (N=195) were interviewed a second time within 2-8 weeks of their original interview. The intraclass test-retest correlations indicate excellent reliability for AD (0.96 among FF and 0.83 among MM/MF twins) (Kuo et al., 2006) and good reliability at the symptom level (correlations ranged from 0.67-0.84 in dependence symptoms). In addition to diagnostic information of AD and other psychiatric disorders, we also collected a battery of self-report questions in the interview, such as demographic variables and personality questionnaires.
2.2. Statistical Models
FMM models are suitable for multivariate data, which could be dichotomous, ordinal, or continuous indicators. Within each latent class there may exist one or more continuous factors that account for “residual” covariation among the indicators. Note that the FA model and LCA are special cases of the FMM. If the factor variance within each class is set to be zero, observed variables are independent given class (i.e., the assumption of local independence holds) and the FMM reduces to the latent class model because the factors can be dropped from the model. On the other hand, if only one class is specified, then the FMM model is reduced to a common factor model because the latent class variable can be dropped.
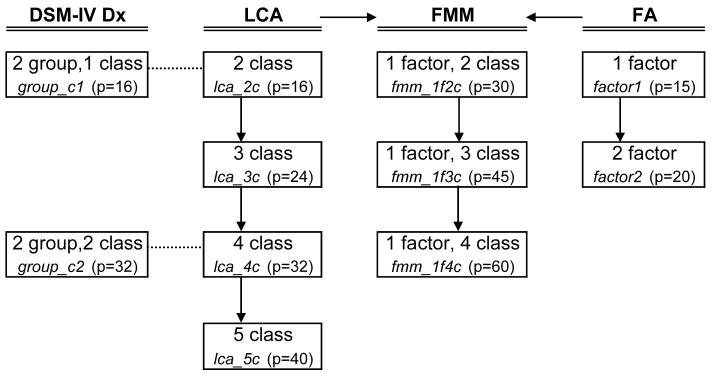
Figure 1 displays the analytic diagram of our modeling framework. It includes LCA models with 2 to 5-class solutions (lca_#c models), factor models with 1 and 2 factors (factor# models), and factor mixture models with 1 factor and 2 to 4 classes (fmm_1f#c models)2. To compare the model fitting with the DSM-IV diagnostic system, we also included models that grouped people into diagnosis/non-diagnosis AD categories based on sum scores of three or more symptoms. In each group, we allowed the models to have variation from 1 to 2 classes (group_c# models). The 2 group 1 class model (group_c1 model) follows the typical DSM-IV binary diagnostic system. The 2 group 2 class model (group_c2 model) given the flexibility to model heterogeneity within diagnostic and non-diagnostic group as each group allows having 2 classes.
Figure 1. Analytic diagram.
Note: The models that we fitted in our data, with specified model names (in italic) and numbers of free estimated parameters (p), including two models follow DSM system (yes/no two groups), four LCA, three FMM, and two FA models. All models were fitted in females and males separately. The dash lines between the DSM and LCA models mean that these models have the same numbers of free estimated parameters. The arrows point from both LCA and FA to FMM imply that they are special cases of the FMM models. DSM-IV Dx models refer to models that grouped people into diagnosis/non-diagnosis AD categories based on DSM-IV symptoms counts with 1 or 2 classes in each group (details see the methods section).
Abbreviation -LCA: latent class analysis; FMM: finite mixture model; FA: factor analysis.
The three main types of model were fitted to dichotomous AD symptoms based on DSM-IV criteria in our sample. These analyses were conducted separately by gender using the Mx program (Neale et al., 2003). The models displayed in the analytic diagram were compared using several goodness-of-fit indexes. In the case of latent class models, simulations showed that in some scenarios, BIC and adjusted BIC (especially in complex structure where items can have different endorsement probabilities for more than one latent classes) outperforms AIC (Nylund et al., in press). Therefore, AIC3, sample-size adjusted BIC (sBIC), and log-likelihood ratio test were used to compare across different models or among nested models. First, the more parsimonious models were identified for males and females separately. We then constrained parameters across genders in these models to test for gender invariance. For factor and mixture models, we constrained factor loadings and item response probabilities; for latent class models, we constrained item response probabilities across genders. we have selected the lowest (largest negative) value for AIC/BIC, and now explicitly state that in the text
Finally, if the model fitting results support the existence of subgroups of alcohol use, we examine sets of exogenous variables to further characterize the subgroups. These measures included alcohol-caused behavioral problems (BP), comorbid disorders, age at onset for alcohol-related milestones, and personality. For BP, we have complete measures of four problems (BP1- legal problems or traffic accidents; BP2- increasing chance of being injured; BP3- drunk or hangover; BP4- social activity impairment). We also included several potentially comorbid disorders: major depression (MD), generalized anxiety disorder (GAD), any phobia (Phobia), conduct disorder (CD), antisocial personality disorder (APD), any other illicit drug abuse (ADA), any other illicit drug dependence (ADD). In terms of alcohol-related milestones, we measured the subjects' reported age at which they: i) first got drunk; ii) drank regularly; iii) had the first AD symptom; and iv) had sufficient symptoms to meet criteria for an AD diagnosis. For personality, we used revised short-form of neuroticism (N), extroversion (E), and novelty seeking (NS).
One thing to note is that we analyzed all the above models using the Virginia twin sample but we did not correct for correlation between twins, because doing so would greatly increase the complexity of the models (see more details in discussion). In general, it is more reasonable to correct for clustering when the average group size is moderate to large; in the present case the group size is mostly two (31.1% one twin, 68.5% both twins, and 0.3% triplets and quadruplets) so the consequences for the model-fitting results are likely to be trivial (Rebollo et al., 2006).
3. Results
In our sample, 26.1% of men and 10.1% of women met criteria for DSM-IV lifetime AD diagnosis. Consistent with this prevalence difference, males have significantly (p<0.001) higher endorsement probability for every AD symptom than females (see Figure 2a). However, among those who meet AD diagnostic criteria, the symptom endorsement probability is relatively similar across genders (Figure 2b). Men endorsed the TOL and WD symptoms more frequently, and women endorsed the CUT symptom more frequently (p<0.01). Of all seven symptoms, MORE is the most frequently endorsed (more than 90% of those meeting diagnostic criteria reported drinking more than intended in both genders) and WD, IMP, and PHY are the low to moderate endorsed symptoms.
Figure 2 (a,b).
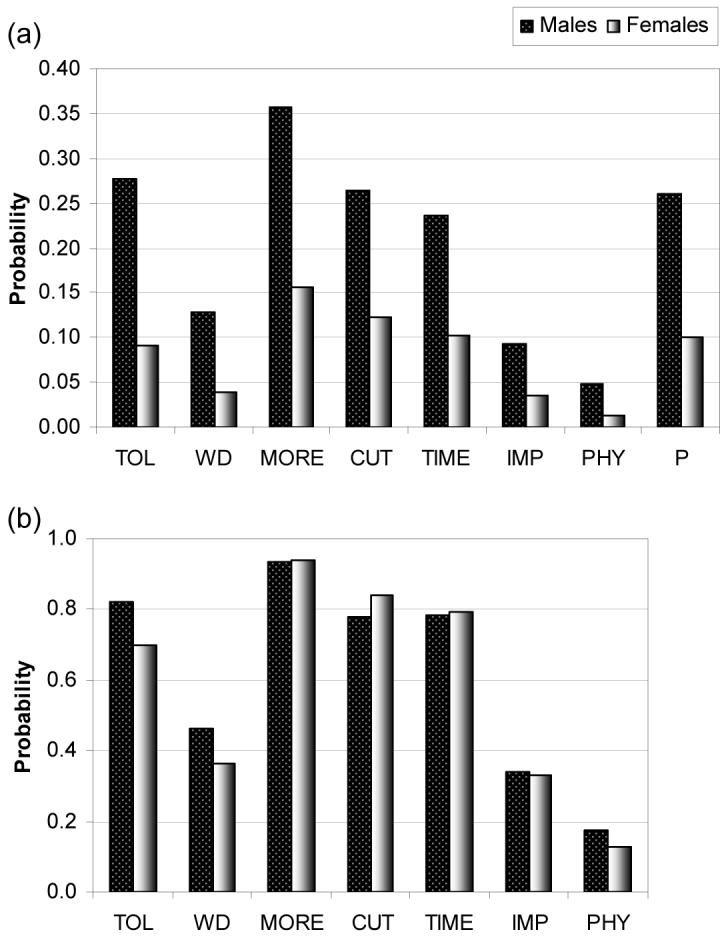
Symptom endorsement probability for DSM-IV alcohol dependence.
(a) the total sample, (b) individuals with alcohol dependence diagnosis.
Abbreviation - The individual symptoms of AD: tolerance (TOL), withdrawal symptoms (WD), drinking more than intended (MORE), unsuccessful attempts to cut down on use (CUT), excessive time related to alcohol (TIME), impaired social or work activities (IMP), and use despite physical consequences (PHY).
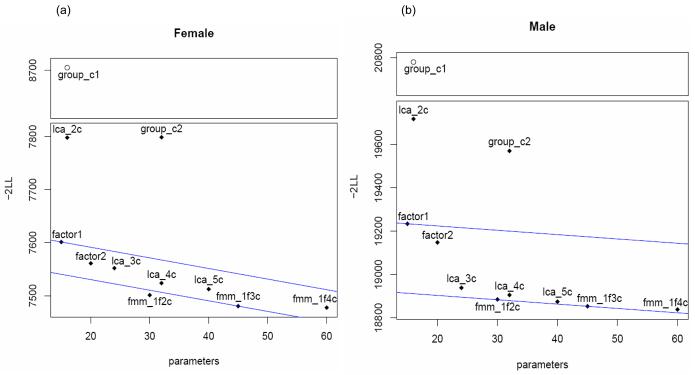
The results of model fitting, −2 times log-likelihood (−2LL), AIC, and sBIC for each model in Figure 1 are listed in Table 1 and the −2LL are also shown in Figure 3 (a,b). Because AIC has a linear relationship with −2LL and is a function of the number of parameter freely estimated in the model (p), two AIC contour lines were drawn in Figure 3 to assist with the comparison of model fits. The first AIC line passes model factor1 (e.g. with a p of 15 for factor1 model the intercept of the AIC line for females equals to 7601.235+30), and the second passes model fmm_1f3c to make most of our models fall in between these two AIC contour lines. The model that is close or falls below the second AIC line has lower −2LL and fits data well. For both genders, the DSM-IV diagnostic models (group_c1 and group_c2) fit our data poorly and the −2LLs are far above the AIC contour lines.
Table 1.
Model fitting results for models in Analytic diagram (see Figure 1) by gender.
| Female |
Male |
||||||
|---|---|---|---|---|---|---|---|
| p | −2LL | AIC | sBIC | −2LR | AIC | sBIC | |
| lca_2c | 16 | 7798.053 | −38721.947 | −53457.487 | 19717.387 | −39290.613 | −66398.815 |
| lca_3c | 24 | 7551.881 | −38952.119 | −53560.848 | 18938.960 | −40053.040 | −66767.372 |
| lca_4c | 32 | 7523.628 | −38964.372 | −53535.464 | 18905.866 | −40070.134 | −66756.723 |
| lca_5c | 40 | 7512.241 | −38959.759 | −53531.045 | 18875.082 | −40084.918 | −66751.726 |
| fmm_1f2c | 30 | 7500.969 | −38991.031* | −53571.507* | 18885.487 | −40094.513 | −66778.579* |
| fmm_1f3c | 45 | 7480.234 | −38981.766 | −53544.886 | 18853.908 | −40096.092* | −66755.599 |
| fmm_1f4c | 60 | 7477.397 | −38954.603 | −53509.316 | 18839.074 | −40080.926 | −66724.246 |
| factor1 | 15 | 7601.235 | −38918.765 | −53555.896 | 19234.329 | −39773.671 | −66640.343 |
| factor2 | 20 | 7560.952 | −38949.048 | −53563.708 | 19148.048 | −39849.952 | −66670.560 |
| group_c1 | 16 | 8704.830 | −37815.170 | −53004.099 | 20779.159 | −38228.841 | −65867.928 |
| group_c2 | 32 | 7798.848 | −38689.152 | −53417.635 | 19570.052 | −39405.948 | −66431.127 |
Note: P- numbers of parameter estimated; LL- log-likelihood; AIC- Akaike's Information Criterion; sBIC- sample size adjusted Bayesian Information Criterion. Numbers in Bold represent the best three models and
represents the best model based on the index selection.
Figure 3 (a,b).
The -2 times log-likelihood (-2LL) for each model described in the analytic diagram by gender (see note in Figure 1).
Note: Two AIC contour lines were added, which pass through model “factor1” and model “fmm_1f3c”.
The LCA models with three to five classes perform better in general than the FA models, which contain several the 2nd or 3rd best-fitting models based on AIC and sBIC selection (see model fitting results in Table 1). The index AIC tends to choose model with one more class than that using sBIC, which is consistent with the findings in Nylund and colleagues. According to indexes AIC and sBIC, the best-fitting models for both genders are FMM models; FMM with 1 factor and 2 classes is the best-fitting model for both genders using sBIC, but 1 factor 3 classes model is for males using AIC. Using −2LR (−2 times log-likelihood ratio) test, the FMM 1-factor 2-class model did not differ significantly in fit from 3 classes model in females (p=0.15), but was significantly worse than the 3-class model in males (p=0.007). According to the model fitting results, we examined gender invariance among several models to assist for final model selection, including lca_3c, lca_4c, fmm_1f2c, and fmm_1f3c. The LCA models with constrained item response probability across genders significantly worsen model fitting (P<0.0001); while both FMM models exhibit gender invariance in factor loadings but not in item response probability. In addition, both FMM models with gender invariance in factor loadings have better fit indexes results than those of LCA models using AIC and sBIC. Therefore, the final model is chosen between the FMM 1 factor 2- or 3-class models.
To make comparison between the FMM 1 factor 2- or 3-class models (with gender invariance in factor loadings) more meaningful and interpretable, we plot item response probabilities for each class in these two models by gender (Figure 4). The fmm-1f2c model has very similar patterns of item response probabilities for both genders (Figure 4a), however, it basically forms one non-drinking and one drinking group and therefore does not identify different patterns of alcohol use. For fmm-1f3c model (Figure 4b), there were two classes of drinking group and the item response patterns display qualitative differences between the two drinking groups. In general, model-fitting should not focus exclusively on goodness-of-fit criteria, but also on the interpretability of results (Barrett, 2007; Burnham and Anderson, 2002).
Figure 4 (a,b).
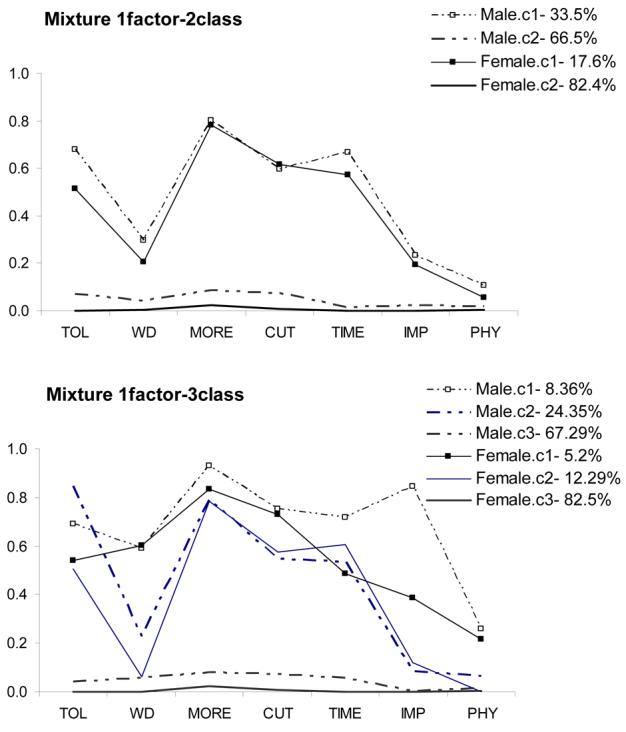
Symptom profiles of model (a) fmm_1f2c and (b) fmm_1f3c.
Note: The endorsement probability for each symptom is based on the model with constrained factor loadings in class 1 and 3 across genders and the factor loadings in the moderate dependence group in females were specified to be proportional to those in males.
Abbreviation - The individual symptoms of AD: tolerance (TOL), withdrawal symptoms (WD), drinking more than intended (MORE), unsuccessful attempts to cut down on use (CUT), excessive time related to alcohol (TIME), impaired social or work activities (IMP), and use despite physical consequences (PHY).
We therefore chose the FMM 1-factor and 3-class model with gender invariance in factor loadings as the final model to compare parameter estimates across genders. Results indicate one severe and one moderate dependence drinking group (classes 1 & 2), and one non-problem drinking group (class 3). The class membership probabilities for classes 1-3 are 5.2%, 12.3%, 82.5% in females and 8.4%, 24.4%, 67.3% in males. In this model, residual correlations among symptoms have been taken into account in each class by including the factor structure. The unidimensional factor structure seems to serve reasonably well. Constraining the factor loadings to be equal across genders in the severe dependence and non-problem drinking groups did not worsen the model fit. However, doing so in the moderate dependence group resulted in a loss of fit (see Table 2 factor loadings). When the factor loadings in the moderate dependence group in females were specified to be proportional to those in males, the model fit was not significantly worse than freely estimating factor loadings by gender, suggesting a unidimensional structure with greater factor variance in males. However, because the severity dependence groups (class 1 & 2) are smaller, the power to reject a unidimensional structure and factor invariance in these two classes may be limited.
Table 2.
Factor loadings of the model fmm_1f3c with constrained factor loadings in class 1 and 3 across genders.
| Class 1 | Class2_female | Class2_male | Class3 | |
|---|---|---|---|---|
| TOL | 0.99 | −0.16 | −0.06 | 1.00 |
| WD | 0.69 | 0.99 | 0.45 | 1.00 |
| MORE | 0.56 | 0.66 | 0.24 | 1.00 |
| CUT | 0.63 | 0.15 | 0.42 | 0.99 |
| TIME | 1.00 | 0.18 | 0.61 | 0.86 |
| IMP | 0.99 | 0.42 | 0.44 | 1.00 |
| PHY | 0.68 | 0.92 | 0.57 | 0.82 |
Note: The individual symptoms of AD: tolerance (TOL), withdrawal symptoms (WD), drinking more than intended (MORE), unsuccessful attempts to cut down on use (CUT), excessive time related to alcohol (TIME), impaired social or work activities (IMP), and use despite physical consequences (PHY).
The class symptom profiles varied somewhat across genders (see Figure 4 a,b). For men, they seem to form severity-based subgroups in that almost every symptom was endorsed more frequently in class 1 than class 2 other than TOL. Also the severe dependence group has great impairment (IMP) compare to moderate dependence group. By contrast, in women the main difference between these two classes was that WD and IMP were endorsed more frequently in class 1. Comparing the symptom profiles for each class across genders, results showed that TIME and IMP were more frequently endorsed by men than women in the severe dependence group, whereas in the moderate dependence group, TOL was the symptom more frequently endorsed by men.
3.1. Validation of classes via comparison of exogenous variables
Modeling results suggested that three latent classes could be reliably identified from the DSM AD symptoms endorsement patterns. We next sought to validate these subgroups by examining a number of putative variables that might predict class membership. These included alcohol-related behavioral problems; comorbid psychiatric disorders; age at onset for alcohol-related events; and personality measures (see Figure 5a). Each subject was assigned to a specific class group based on his/her highest probability of class membership (all above 0.5, suggesting that individuals can unambiguously assign into one class), given their response pattern. Among four alcohol-caused behavioral problems in our measure (BP1- legal problems or traffic accidents; BP2- increasing chance of being injured; BP3- drunk or hangover; BP4- social activity impairment), there was a consistent trend of increasing endorsement probability with increasing severity level of alcohol dependence. It is noteworthy that even within the non-problem drinking group, 12% reported ever having legal problems or traffic accidents and 20% reported an increased chance of being injured because of drinking. In addition, both severe and moderate dependence groups had significantly higher (2-3 fold) maximum drinks in a single day than did the non-problem drinking group.
Figure 5 (a,b).
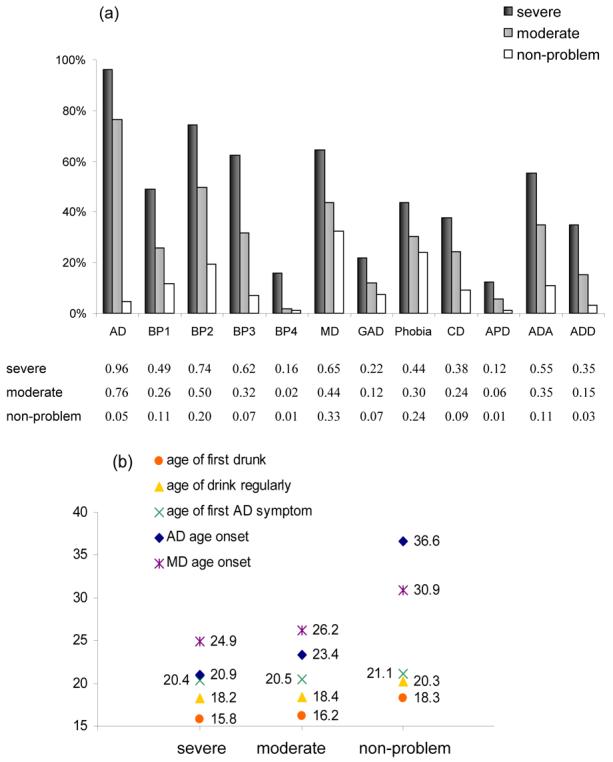
Characteristics of three drinking subgroups.
(a) Prevalence of comorbid disorders and alcohol-related behavior problems for each class; (b) age at onset (years) for a variety of drinking milestones and MD diagnosis.
Abbreviation - AD: alcohol dependence; BP1: legal problems or traffic accidents because of drinking; BP2: under the effects of alcohol that increased chance of being injured; BP3: drunk or hangover when at work/school; BP4: lose a job or get kicked out of school because of drinking; MD: lifetime major depression; GAD: generalized anxiety disorder; Phobia: any phobia; CD: conduct disorder; APD: antisocial personality disorder; ADA: any illicit drug abuse; ADD: any illicit drug dependence.
We found that the lifetime prevalence of every comorbid disorder we examined was the lowest in non-problem drinking group, and significantly greater in moderate and severe dependence groups. Rates of comorbidity were especially high for GAD (22%), CD (38%), APD (12%), ADA (55%), and ADD (35%) in the severe dependence group, compared to 7%, 9%, 1%, 11%, and 3%, respectively, in the non-problem drinking group. This observation is consistent with results from the National Comorbidity Survey, in which high comorbidity between drinking problems and other psychiatric disorders was also found (Kessler et al., 1997).
Three age at onset milestones for alcohol-related problems were considered: i) first got drunk; ii) drank regularly; iii) had the first AD symptom; and iv) had sufficient symptoms to meet criteria for an AD diagnosis. For each stage, the severe dependence group has the earliest age at onset, followed by moderate and non-problem drinking groups (see Figure 5b). The time difference from drinking regularly to AD diagnosis was longer in the non-problem drinking group (16.3 years) than in the severe dependence group (2.7 years). The non-problem drinking group (the majority of our sample) exhibits slow development of alcohol use. In addition, since MD has very high comorbidity rate with AD (65%, 44%, 33% in classes 1 to 3), we also reported age at onset of MD. The mean age at onset of MD differed between groups: individuals in the dependence severity groups had MD onset significantly (P<0.0001) earlier (25-26 years) than in the non-problem drinking group (31 years).
We also examined personality scores based on revised short-form of neuroticism (N), extroversion (E), and novelty seeking (NS) in different classes. For NS and E, both traits were higher in the two dependence severity groups than in non-problem drinking group (P<0.05) but there was no significant difference between the two dependence severity groups. However, for N (with a maximum sum score of 12), there was a significant difference with dependence severity (both global and pair-wise comparisons, P<0.0001, with moderate Cohen's d effect sizes of 0.23-0.62), with a mean score of 5 in the severe, 3.6 in the moderate, and 2.9 in the non-problem drinking group.
4. Discussion
The primary goal of this study was to assess whether the alcohol dependence criteria in the population could be better characterized by a continuous dimension, a few discrete subgroups, or a combination of the two. Although both factor and latent class models have been previously used to explain the population aggregation of AD symptoms (Allen et al., 1993), no clear structure has emerged. A FA approach seeks to understand the underlying continuous dimensions for symptoms, which is an important initial stage of developing constructs in the use or abuse either of a single substance (Harford and Muthen, 2001; Hasin et al., 1997; Lennox et al., 1996) or of a variety of substance disorders (Nelson et al., 1999) but is more difficult to provide direct clinical applications, such as treatment response and evaluation. While LCA models frequently support a severity-based classification in alcohol problems (Bucholz et al., 1996; Lynskey et al., 2005) or cannabis use (Grant et al., 2006), the symptom profiles from these analyses appear largely parallel, and involve relatively small differences in item endorsement probability. Such minor differentiation between classes can make it difficult to distinguish one class from another, and also problematic to assign class membership to individuals based on their item response pattern. A factor mixture model, which incorporates dimensions within classes, can add to the interpretation and understanding of the differences between classes. Unaccounted for covariation within the class structure can be modeled by the continuous latent variables, and the smaller number of classes is more likely to reflect qualitatively heterogeneous groups in the population. For instance, subgroups obtained from classification analysis have different characteristics and may respond differently in treatment or prognosis (see examples in Muthen et al., 2002 using growth mixture modeling).
In the present study, we illustrated that factor mixture models that combine categorical and continuous latent variables are a promising tool for this kind of phenotypic analyses. Model fitting results showed that a pure FA model was not satisfactory and that the LCA models fit better in general. This indicates a continuous latent construct could not explain the overall covariation among alcohol symptoms and the heterogeneous nature of alcohol problems in the general population. However, the mixture model with one factor and three classes model fit our data well, with one major non-drinking dependence group and two various severity levels of dependence groups. This finding is consistent with a previous study applied mixture models in tobacco dependence (Muthen and Asparouhov, 2006), which also found the FMM fits their data the best. In general, for heterogeneous behavioral traits, the mixture model seems to fit data better than either of the conventional models in both cases of cross-sectional or longitudinal data [see the examples of tobacco dependence and heavy drinking, (Muthen and Asparouhov, 2006; Muthen and Muthen, 2000)]. Other than model-based classification analyses, Cloninger (1987) proposed a neurobiological learning model that split alcohol use disorders into two subtypes (type I and II). This dichotomy has been studied with respect to several aspects of alcohol problems. Results suggest that the two subtypes differ on dependence severity, age-at-onset, or treatment response. Although this scheme provides a way to subgroup individuals with AD, it is largely dependent on existing personality constructs (type I alcoholism had high harm avoidance and low novelty seeking personality). Compared with model-based phenotypic analysis, mapping the current DSM criteria onto the type I/II dichotomy has been more difficult. Future research may be better served by testing for latent classes directly from criteria level data.
In our sample, 96.1% of individuals in severe dependence group met diagnosis of AD, compared to 76.4% in moderate dependence group and 4.8% in non-problem drinking group; the average numbers of AD symptoms were 5.3, 3.1, and 0.2, respectively. Although many individuals in the moderate dependence group endorsed symptoms like TOL, MORE, CUT, and TIME (see Figure 4 a,b), a quarter of them did not meet the present DSM-IV AD diagnosis. From a clinical point of view, failure to detect these sub-clinical individuals or so-called ‘diagnostic orphans’, who may be in an earlier stage of development of drinking dependence problems, may hamper an effective treatment or intervention (Note: The moderate dependence group has relatively younger average age, three years younger than severe dependence group). In addition, although model-fitting results supported a unidimensional factor structure for AD symptoms, factor loadings were not consistent across three classes. The factor loadings were high for all symptoms in the severe dependence and non-problem drinking groups, but were low for several symptoms in the moderate dependence group (< 0.2 for TOL, CUT, and TIME among females and <0.3 for TOL and MORE among males). The TOL criterion factor loading was especially low in both genders, implying that, relative to the other AD criteria; TOL was less endorsed and poorly discriminated in the moderate dependence group.
The mixture of AD and non-AD individuals in the moderate drinking group may explain why the two models based on DSM-IV diagnostic system fit the data very poorly. In addition, we fitted mixture models with the DSM-IV diagnostic system. Including dimensionality (one latent factor) into the DSM-IV framed models improves model fit (data not shown) but is still much worse than the freely estimated mixture 1-factor 3-class models. That finding in turn provides empirical evidence for the heterogeneity in AD diagnosis and suggests the reconsidering of the diagnostic system to classify according to, e.g., the three-class system found here. Presumably individuals in severe or moderate drinking groups may vary in their clinical course, treatment response, or prognosis. In a predictive model, given a certain symptom profile, individuals could be best predicted to fall into one of the classes. From a clinical point of view, this refinement of grouping approach could help clinical workers to provide a suitable treatment or intervention for other comorbid disorders in more homogenous subgroups. We are developing a small web-based application that gives the likelihood for particular patterns of responses. This will provide a way to classify individuals based on different combinations of symptoms and also report the corresponding features of those exogenous variables that were tested in our study, including alcohol-related behavioral problems, comorbid psychiatric disorders, age at onset for alcohol-related events, and personality features.
The class membership probability for the non-problem drinking group was higher for females (82.6%) than males (67.4%), while class probabilities for other problematic drinking groups (class 1 & 2) in males was nearly twice of those in females, which is consistent with the well-recognized gender differences in the prevalence of drinking problems (Green et al., 2004; Kessler et al., 1994). However, in other respects males and females were remarkably similar. First, the symptom endorsement probabilities among individuals diagnosed with AD are almost the same in males and females (Figure 2b). Second, the age at onset of AD distributions are similar with a peak of 18-20 years in this sample for both genders (Kuo et al., 2006). Third, we calculated the class membership agreement within twin pairs. The agreement did not differ between females and males (weighted Kappa = 0.21, 95% CI =0.13-0.29 for female twins and 0.17, 95% CI =0.12-0.22 for male twins). However, the agreement was substantially greater in monozygotic (MZ) compared to dizygotic (DZ) twins (weighted Kappa = 0.31, 95% CI =0.25-0.37 for MZ and 0.13, 95% CI =0.09-0.17 for DZ twins). If restricted to two alcohol problem groups, the tetrachoric correlations between twins were 0.53 for MZ and 0.02 for DZ twins, implying a moderate genetic component for class assignment of alcohol problematic use. Additional differences were found between groups. Those classified in the more severe alcohol problem groups reported more alcohol-caused behavioral problems, had higher risk of having comorbid psychiatric disorders, exhibited a faster development of alcohol problems from regular drinking to AD diagnosis, and higher score of personality trait neuroticism.
The results presented in this report should be considered in the light of three potential limitations. First, the results are based on Caucasian twins born in Virginia and may not generalize to individuals from other ethnic backgrounds or geographical regions. Second, as we mentioned in the method section, we did not directly model the correlation between twins in order to avoid further complicating the models. We expect the consequences of non-independence for the model-fitting results to be negligible due to the small group size (i.e., here two for the twins). We refit our models to data where one twin was randomly selected from each pair (N=4460) and found similar model fitting results. According to AIC and sBIC, the fmm-1f3c and fmm-1f2c models fit the single record data the best, respectively. This concurs with our general experience that confidence intervals are only modestly affected when models fit to non-independent (paired) data but that parameter point estimates typically are not. Third, we used outcome measures based solely on DSM-IV AD binary diagnostic symptoms; there may be other measures or instruments that could capture the distribution of alcohol problems better but were not included in the present study.
Finally, further work is needed. A larger sample (e.g. a national representative sample) could provide more power to distinguish and help choose among models. Including more symptoms/items and using ordinal or continuous measures which provide greater information to sub-classify and quantify individuals' patterns of drinking behavior would also be useful. Longitudinal data would provide an opportunity to examine the degree to which individual's transition between classes, or change on the dimension within a class, or both. For instance, subgroups obtained from classification analysis have different characteristics and may respond differently in treatment or prognosis (see examples in Muthen et al., 2002 using growth mixture modeling).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
When included, the 226 abstainers were all found to occupy the non-problem drinking class (their class- membership probabilities were all > 0.99). Excluding them from the analyses did not change the overall model fitting results. Alternatively, one can treat them as missing data in the analysis.
The mixture models allow for multidimensional structure. Because of previously suggested unitary construct of AD, we only consider mixture models with 1 factor in our analytic diagram.
The AIC index obtained from Mx uses the formula: −2lnL − 2df, which calculates the number of statistics from the raw data observations. For AIC/sBIC indexes, models with lower (larger negative) values are better models.
References
- Aggen SH, Neale MC, Kendler KS. DSM criteria for major depression: evaluating symptom patterns using latent-trait item response models. Psychol Med. 2005;35:475–487. doi: 10.1017/s0033291704003563. [DOI] [PubMed] [Google Scholar]
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- Allen JP, Fertig JB, Towle LH, Bryant K, Altshuler VB, Vrublevsky AG, Valentik YV. Structure And Correlates Of Alcohol Dependence In Clinical-Samples In The United-States And Russia. Addiction. 1993;88:1535–1543. doi: 10.1111/j.1360-0443.1993.tb03139.x. [DOI] [PubMed] [Google Scholar]
- Barrett P. Structural equation modelling: Adjudging model fit. Personality And Individual Differences. 2007;42:815–824. [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JIJ, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Madden PAF. Transitions in drinking in adolescent females: Evidence from the Missouri Adolescent Female Twin Study. Alcoholism-Clinical And Experimental Research. 2000;24:914–923. [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JI, Schuckit MA. Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcoholism-Clinical And Experimental Research. 1996;20:1462–1471. doi: 10.1111/j.1530-0277.1996.tb01150.x. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. Springer; New York: 2002. [Google Scholar]
- Chung T, Martin CS. Classification and course of alcohol problems among adolescents in addictions treatment programs. Alcoholism-Clinical And Experimental Research. 2001;25:1734–1742. [PubMed] [Google Scholar]
- Dolan CV, Van der Maas HLJ. Fitting multivariage normal finite mixtures subject to structural equation modeling. Psychometrika. 1998;63:227–253. [Google Scholar]
- Everitt BS. A Finite Mixture Model For The Clustering Of Mixed-Mode Data. Statistics & Probability Letters. 1988;6:305–309. [Google Scholar]
- Grant JD, Scherrer JF, Neuman RJ, Todorov AA, Price RK, Bucholz KK. A comparison of the latent class structure of cannabis problems among adult men and women who have used cannabis repeatedly. Addiction. 2006;101:1133–1142. doi: 10.1111/j.1360-0443.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Polen MR. Gender differences in the relationships between multiple measures of alcohol consumption and physical and mental health. Alcoholism-Clinical and Experimental Research. 2004;28:754–764. doi: 10.1097/01.alc.0000125342.28367.a1. [DOI] [PubMed] [Google Scholar]
- Harford TC, Muthen BO. The dimensionality of alcohol abuse and dependence: a multivariate analysis of DSM-IV symptom items in the National Longitudinal Survey of Youth. J Stud Alcohol. 2001;62:150–157. doi: 10.15288/jsa.2001.62.150. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant B, Endicott J. The Natural-History Of Alcohol-Abuse - Implications For Definitions Of Alcohol-Use Disorders. American Journal Of Psychiatry. 1990;147:1537–1541. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Alcohol Abuse and Dependence in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Van Rossem R, McCloud S, Endicott J. Differentiating DMS-IV alcohol dependence and abuse by course: Community heavy drinkers. Journal Of Substance Abuse. 1997;9:127–135. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Jedidi K, Jagpal HS, Desarbo WS. Finite-mixture structural equation models for response-based segmentation and unobserved heterogeneity. Marketing Science. 1997;16:39–59. [Google Scholar]
- Kahler CW, Strong DR. A Rasch model analysis of DSM-IV alcohol abuse and dependence items in the National Epidemiological Survey on Alcohol and Related Conditions. Alcoholism-Clinical And Experimental Research. 2006;30:1165–1175. doi: 10.1111/j.1530-0277.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Nichol PE, Hicks BM, Markon KE, Patrick CJ, Iacono WG, McGue M. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychological Assessment. 2004;16:107–119. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- Kuo PH, Gardner CO, Kendler KS, Prescott CA. The temporal relationship of the onsets of alcohol dependence and major depression: using a genetically informative study design. Psychol Med. 2006:1–10. doi: 10.1017/S0033291706007860. [DOI] [PubMed] [Google Scholar]
- Lazarsfeld PF, Henry NW. Latent structure analysis. Houghton Mifflin Company; Boston: 1968. [Google Scholar]
- Lennox RD, Zarkin GA, Bray JW. Latent variable models of alcohol-related constructs. Journal Of Substance Abuse. 1996;8:241–250. doi: 10.1016/s0899-3289(96)90282-5. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Nelson EC, Neuman RJ, Bucholz KK, Madden PA, Knopik VS, Slutske W, Whitfield JB, Martin NG, Heath AC. Limitations of DSM-IV operationalizations of alcohol abuse and dependence in a sample of Australian twins. Twin Res Hum Genet. 2005;8:574–584. doi: 10.1375/183242705774860178. [DOI] [PubMed] [Google Scholar]
- McLachlan GJ, Peel D. Finite mixture models. Wiley; New York: 2000. [Google Scholar]
- Moustaki I. A latent trait and latent class model for mixed observed variables. British Journal of Mathematical and Statistical Pscyhology. 1996;49:313–334. [Google Scholar]
- Muthen B. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006;101:6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- Muthen B, Asparouhov T. Item response mixture modeling: application to tobacco dependence criteria. Addict Behav. 2006;31:1050–1066. doi: 10.1016/j.addbeh.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Muthen B, Brown CH, Masyn K, Jo B, Khoo ST, Yang CC, Wang CP, Kellam SG, Carlin JB, Liao J. General growth mixture modeling for randomized preventive interventions. Biostatistics. 2002;3:459–475. doi: 10.1093/biostatistics/3.4.459. [DOI] [PubMed] [Google Scholar]
- Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism-Clinical And Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Muthen B, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical Modeling, VCU Box 900126. Department of Psychiatry; Richmond, VA 23298: 2003. [Google Scholar]
- Nelson CB, Rehm J, Ustun TB, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO reliability and validity study. Addiction. 1999;94:843–855. doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Structural Equation Modeling. in press. [Google Scholar]
- Pickles A, Angold A. Natural categories or fundamental dimensions: on carving nature at the joints and the rearticulation of psychopathology. Dev Psychopathol. 2003;15:529–551. doi: 10.1017/s0954579403000282. [DOI] [PubMed] [Google Scholar]
- Proudfoot H, Baillie AJ, Teesson M. The structure of alcohol dependence in the community. Drug Alcohol Depend. 2006;81:21–26. doi: 10.1016/j.drugalcdep.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Rebollo I, de Moor MHM, Dolan CV, Boomsma DI. Phenotypic factor analysis of family data: Correction of the bias due to dependency. Twin Research And Human Genetics. 2006;9:367–376. doi: 10.1375/183242706777591326. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-III-R (SCID) New York State Psychiatric Institute. Biometrics Research Department; New York: 1985. [Google Scholar]
- Sullivan PF, Prescott CA, Kendler KS. The subtypes of major depression in a twin registry. J Affect Disord. 2002;68:273–284. doi: 10.1016/s0165-0327(00)00364-5. [DOI] [PubMed] [Google Scholar]
- Waller NG, Meehl PE. Multivariate taxometric procedures: Distinguishing types from continua. SAGE University Press; 1997. [Google Scholar]
- Yung YF. Finite mixtures in confirmatory factor-analysis models. Psychometrika. 1997;62:297–330. [Google Scholar]