Abstract
Micropapillary carcinoma is an uncommon variant of urothelial carcinoma with high metastatic potential. The presence of micropapillary carcinoma component in bladder biopsies should alert urologists to its aggressive behaviour. We report the case of a 70-year-old man who presented with macroscopic hematuria lasting 2 weeks. Magnetic resonance imaging revealed a bladder tumour in the dome area extended to perivascular adipose. The transurethral biopsy showed a high-grade micropapillary carcinoma with muscle invasion. Radical cystectomy with lymph node dissection was then performed. The pathological examination revealed a high-grade purely micropapillary carcinoma invading the perivesical adipose. No tumour recurrence or metastasis were reported at the 6-month follow-up.
Introduction
Micropapillary carcinoma (MPC) of the bladder was established as a distinct pathological entity by Amin and colleagues.1 It is an uncommon but aggressive variant of urothelial carcinoma. We report a new case of bladder MPC.
Case report
A 70-year-old man presented with macroscopic hematuria lasting 2 weeks. On urine analysis, red blood cells were 20/high-power field and white blood cells were 1/high-power field. Urine cytology was noncontributive. Cystoscopy showed a solitary nonpapillary tumour in the dome area. A transurethral biopsy demonstrated a high-grade micropapillary carcinoma invading the muscle. Magnetic resonance imaging showed that the tumour extended to the perivesical tissue (Fig. 1). Cystoprostatectomy with pelvic lymph node dissection was performed.
Fig. 1.
Pelvic sagittal magnetic resonance imaging section spin-echo T1-weighted after gadolinium administration showing a tumour of the bladder dome area with perivesical tissue infiltration.
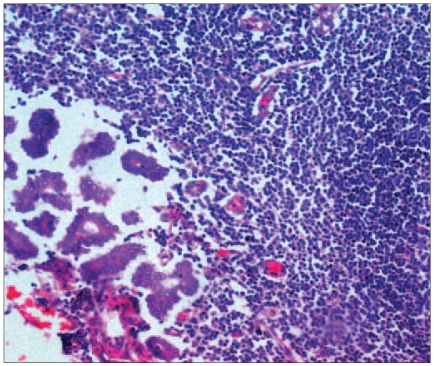
Macroscopic findings demonstrated a 40-mm solid tumour in the dome area infiltrating the perivesical adipose tissue. Microscopically, the malignant cells were arranged in small papillary clusters lying in clear spaces (Fig. 2). These cells were of irregular nuclear outline and high mitotic activity (Fig. 3). These tumour cells invaded the perivesical adipose tissue. The surface epithelium exhibited a transitional cell carcinoma in situ. Conventional transitional cell carcinoma elements were not found. There was lymph node metastasis in 1 of the 5 nodes (Fig. 4). There was no visceral metastasis, and the patient did not receive adjuvant chemotherapy. Adjuvant chemotherapy would not have been efficacious as there was lymph node metastasis without visceral metastasis. No tumour recurrence or metastasis were reported at the 6-month follow-up.
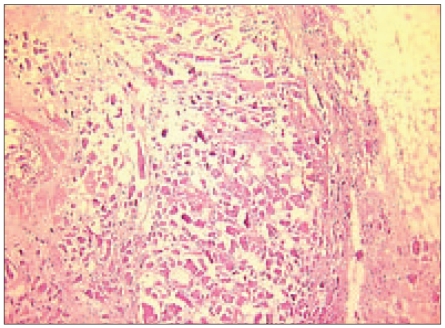
Fig. 2.
Histopathological section showing small papillary clusters lying in clear spaces (hematoxylin–eosin stain, original magnification ×25).
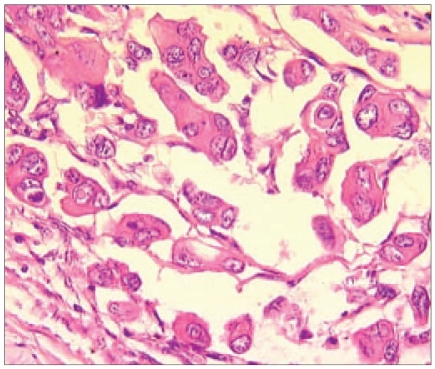
Fig. 3.
Histopathological section showing that the cells were of high-grade nuclear atypia (hematoxylin–eosin stain, original magnification ×400).
Fig. 4.
Histopathological section showing metastasis of the lymph node (hematoxylin–eosin stain, original magnification ×200).
Discussion
MPC of the bladder is considered a rare variant of transitional cell carcinoma; the incidence is about 0.7% among bladder tumours.2 MPC of the bladder occurs in elderly patients, mostly in men.3
The histological features are distinctive: a surface component is composed of slender and delicate filiforme processes or small papillary clusters lined by uniform transitional cells. The invasive component consists of tightly cohesive nests and conglomeration of micropapillary cells.3 These clusters lay in small clear spaces that lack endothelial lining.3 Marked cytologic atypia with irregular nuclear outline and high mitotic activity are usually evident.3 Carcinoma in situ and a conventional transitional cell carcinoma are occasionally found.3,4
The biphasic pattern of micropapillary carcinoma, with high-grade elements in the deeper portion, can be a potential source of underdiagnosis in superficial transurethral resection specimens.3
The immunohistochemical profile (positivity for cytokeratin 7, cytokeratin 20 and epithelial membrane antigen) of MPC suggests that it is a variant of bladder adenocarcinoma.5
MPC of the bladder must be distinguished from metastatic carcinoma, especially pulmonar and peritoneal origins.4 However, the presence of transitional cell carcinoma in situ and the cell positivity for cytokeratin 7 and cytokeratin 20 supported a urothelial origin.6
Even the focal presence of micropapillary pattern in an otherwise conventional bladder carcinoma is associated with advanced tumour stage and poor prognosis.1
Similar to that occurring in the urinary bladder, carcinoma with a micropapillary pattern has also been described in the ovary, lung and peritoneum. Most of these tumours show a high propensity for lymph node metastasis. The possibility of urothelial origin should also be considered if micropapillary pattern is found on metastatic deposits.3 Treatment is not codified on radical cystectomy associated with chemotherapy, particularly if there is visceral metastasis.4 In our case, there was no visceral metastasis, and adjuvant chemotherapy was not indicated because it seemed non-efficacious if there was lymph node metastasis without visceral metastasis. The optimal treatment remains to be defined in multicentre studies.2
The presence of an MPC component in bladder biopsies should alert the urologists to this unusual but aggressive disease and deep-muscle biopsies should be recommended.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
References
- 1.Amin MB, Ro JY, el-Sharkawy T, et al. Micropapillary variant of transitional cell carcinoma of the urinary bladder: hisotologic patter resembling ovarian papillary serous carcinoma. Am J Surg Pathol. 1994;18:1224–32. doi: 10.1097/00000478-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Johansson SL, Borghed G, Holmang S. Micropapillary bladder carcinoma: a clinico–pathological study of 20 cases. J Urol. 1999;161:1798–802. doi: 10.1016/s0022-5347(05)68807-6. [DOI] [PubMed] [Google Scholar]
- 3.Chan GS, Ng WK, Nicholls JM, et al. Micropapillary transitional cell carcinoma of urinary bladder: pathologic quiz case. Arch Pathol Lab Med. 2004;129:e53–4. doi: 10.5858/2005-129-e53-PQC. [DOI] [PubMed] [Google Scholar]
- 4.Sugino Y, Negoro H, Iwamura H, et al. Micropapillary variant of transitional cell carcinoma of the bladder. Int J Urol. 2004;11:792–4. doi: 10.1111/j.1442-2042.2004.00880.x. [DOI] [PubMed] [Google Scholar]
- 5.Samaratunga H, Khoo K. Micropapillary variant of urothelial carcinoma of the urinary bladder; a clinicopathological and immunohistochemical study. Histopathology. 2004;45:55–64. doi: 10.1111/j.1365-2559.2004.01895.x. [DOI] [PubMed] [Google Scholar]
- 6.Oh YL, Kim KR. Micropapillary variant of transitional cell carcinoma of the ureter. Pathol Int. 2000;50:52–6. doi: 10.1046/j.1440-1827.2000.00997.x. [DOI] [PubMed] [Google Scholar]