Abstract
Background and objectives: The 1999 Canadian vascular access guidelines recommend the fistula as the access of choice. The study describes the trends in hemodialysis access use, variation among provinces, and the association with mortality from 2001 to 2004.
Design, setting, participants and measurements: An observational study of adult patients registered in Canadian Organ Replacement Registry on hemodialysis. Access trends were examined among incident and prevalent hemodialysis patients adjusted for age, sex, body mass index, late referral, race, smoking status, province, etiology of end-stage renal disease, and comorbidities. Cox proportional hazard regression analysis was used to analyze risk for death for patients followed to December 31, 2005.
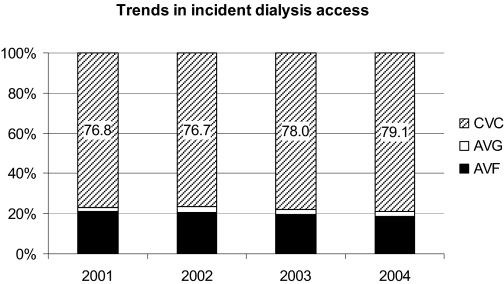
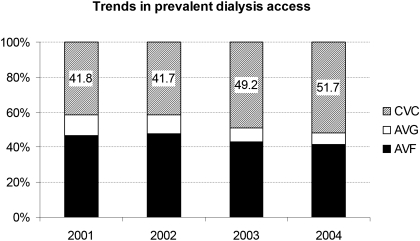
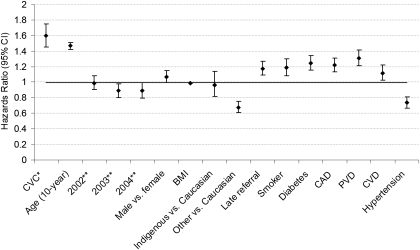
Results: From 2001 to 2004, incident catheter use increased from 76.8% to 79.1%, fistulas decreased from 21.6% to 18.6%, and grafts remained between 2.1% to 2.6%. Prevalent catheter use increased from 41.8% to 51.7%, and fistulas and grafts decreased from 46.8% to 41.6% and 11.4% to 6.7%, respectively. There was significant variation in incident and prevalent fistulae use among the provinces. Adjustment for differences in patient characteristics did not change these trends. Incident catheter use was associated with a 6 times greater risk of death compared with fistula or graft use combined.
Conclusions: In Canada there has been a decrease in fistulae and grafts with a subsequent increase in catheters that is not explained by changes in patient characteristics. Vascular access use varied by province, suggesting differences in practice patterns. Because incident catheter use was associated with increased mortality, urgent measures are needed to develop strategies to decrease catheter use.
In 1999, the Canadian Society of Nephrology vascular access guidelines recommended the arteriovenous fistula (AVF) as the hemodialysis access of choice (1) because of its association with reduced mortality, morbidity, and cost compared with central venous catheters (CVCs) and to a lesser extent compared with arteriovenous grafts (AVGs) (2–5). Despite these advantages and numerous guidelines suggesting higher fistula targets (6), AVF use is not increasing in either the incident or prevalent populations in several countries (7).
Data on Canadian hemodialysis vascular access use have been sparsely reported. The Dialysis Outcomes Practice Patterns Study (DOPPS) reported on a 2003 cross-sectional sample of 118 incident and 524 prevalent hemodialysis patients indicating only 26% of incident and 53% of prevalent patients were dialyzing with a fistula (8). This sample represented only 5% of the total number of patients on hemodialysis. The Canadian Organ Replacement Registry (CORR) is a national registry of all patients on renal replacement therapy (RRT) in Canada and has documented vascular access use since 2001. The aim of this study is to examine trends in vascular access use in Canada between 2001 and 2004, adjusting for factors associated with the type of vascular access, and to examine the association of vascular access type with mortality.
Materials and Methods
The CORR registry records the incidence, prevalence, and outcome of all chronic dialysis and solid organ transplant patients in Canada. Data have been collected by voluntary completion of survey forms for each patient at the start of dialysis and yearly ending December 31st. For this study, all adult patients (age >18 yr at start of RRT), receiving hemodialysis as their first form of RRT, with documentation of vascular access type, between January 1, 2001 and December 31, 2004 were included.
Definitions of Study Cohorts and Vascular Access
Incident Cohorts.
Patients who commenced hemodialysis as their first form of RRT were included in one of 4 incident cohorts established for years 2001 (n = 3649), 2002 (n = 3666), 2003 (n = 3728), and 2004 (n = 3766) The incident access was defined as the access in use at the start of dialysis.
Prevalent Cohorts.
Patients on hemodialysis on December 31st of each year were included in the prevalent cohort for years 2001 (n = 8239), 2002 (n = 10,585), 2003 (n = 10,384), and 2004 (n = 11,084). The prevalent access was the access in use on October 31st of each year.
Data Collection
For this study, vascular access is reported as an AVF, AVG, or CVC. All forms of CVCs were combined into one category. Comorbidities present at the start of dialysis were documented by the individual facilities using the CORR survey forms. Information on the presence or absence of coronary artery disease (CAD) (includes angina, myocardial infarction, and coronary artery bypass surgery), peripheral vascular disease (PVD), hypertension, diabetes mellitus, and cerebrovascular disease (CVD) were documented in 3 categories: “yes,” “no,” and “unknown.” The unknowns were combined into the “no” group. All classifications of diabetes were combined. Late referral was defined as first seeing a nephrologist within 3 mo of starting dialysis. Body mass index (BMI) was calculated using the height and weight collected at the start of dialysis. Current smokers were documented as having smoked in the last 3 mo.
Analysis
Patient characteristics were compared across cohorts and access type using χ2 or Kruskal-Wallis tests as appropriate. Univariate analyses of the distribution of access types across each cohort were performed using the χ2 test. Multivariate analyses of access types using binary or multinomial logistic regression, as appropriate, were performed using access type as the independent variable and cohort year as the dependent variable of interest. All regression models were adjusted for the following variables: age, sex, race, BMI, smoking status, late referral, provinces of residence, cause of end-stage renal disease, and comorbidities as listed in Table 1. AVFs and AVGs were combined into one category for the multivariate analyses of incident access because of the limited number of AVGs. Prevalent access was also adjusted for dialysis vintage. Backward variable selection procedure was used to select the variables that were significantly associated with the dependent variable. Results from the final regression models were used to calculate the adjusted probability of each access type by cohort. A two-sided P value of less than 0.05 was considered to be statistically significant. Model estimates are presented with 95% confidence intervals (CIs). Cox proportional hazard regression analysis was used to analyze risk for death for patients followed to December 31, 2005. Patients were censored at times of transplant, permanent switch to peritoneal dialysis, and lost to follow-up. Explanatory variables in the Cox regression are incident year, age, sex, race, BMI, initial access type (CVC versus AVG/AVF combined), late referral, smoking status (current or not), and a history of diabetes, CAD, PVD, CVD, and hypertension. Hazard ratios (HRs) and the 95% CI were estimated from the model. All analyses were conducted using SAS version 9.2 statistical software (SAS Institute, Cary, NC).
Table 1.
Description of hemodialysis patients in the incident cohorts
| Variable | 2001 | 2002 | 2003 | 2004 | Excluded patients |
|---|---|---|---|---|---|
| No. of patients | 3649 | 3666 | 3728 | 3766 | 1190 |
| Age, years (median) | 68.0 | 68.0 | 68.0 | 67.0 | 68.0 |
| Male, % | 58.9 | 57.4 | 60.2 | 59.0 | 60.3 |
| Race, % | |||||
| white | 76.4 | 77.1 | 76.2 | 76.1 | 53.1 |
| indigenous | 4.9 | 4.9 | 4.9 | 5.5 | 4.0 |
| other | 18.7 | 18.0 | 18.9 | 18.5 | 42.9 |
| BMI, kg/m2 (median) | 25.6 | 25.6 | 25.8 | 26.1 | 26.0 |
| Late referral | |||||
| <3 months, % | 36.4 | 35.5 | 32.9 | 33.8 | 34.5 |
| Smoker, % | |||||
| current | 14.4 | 14.8 | 13.7 | 12.8 | 7.5 |
| Cause of ESRD, % | |||||
| glomerulonephritis | 11.8 | 11.6 | 11.7 | 11.9 | 8.4 |
| diabetes mellitus | 34.2 | 35.5 | 35.9 | 35.7 | 21.1 |
| hypertension | 12.3 | 12.1 | 13.4 | 12.7 | 7.4 |
| other | 39.9 | 39.9 | 37.5 | 36.9 | 37.4 |
| unknown | 1.8 | 1.0 | 1.4 | 2.8 | 25. |
| Comorbidities, % | |||||
| diabetes | 43.8 | 45 | 44.3 | 44.7 | 27.7 |
| coronary artery disease | 28.4 | 26.8 | 27.2 | 27.6 | 16.1 |
| peripheral vascular disease | 22.7 | 23.5 | 20.5 | 20 | 13.2 |
| cerebrovascular disease | 15.8 | 14.1 | 13.6 | 14 | 8.9 |
| hypertension | 83.4 | 83.1 | 82.1 | 82.5 | 51.5 |
Results
Incident Cohort
Of 15,999 incident patients, 1190 (8%) did not have a vascular access recorded and thus were ineligible for this study. The distributions of patient characteristics for the study population by year and for those excluded from this study are shown in Table 1. Patients without a documented vascular access also had fewer reported comorbidities and a greater proportion with an unknown cause of end-stage renal disease. Among the population studied, there was a decrease in late referrals, smokers, and those with reported PVD and CVD over time. Figure 1 illustrates the crude rates of access use demonstrating the increase in incident CVCs, the decline in AVFs, and the stability in AVG use between 2001 and 2004.
Figure 1.
Distribution (%) of vascular access type among incident hemodialysis patients (unadjusted).
Late referral (adjusted odds ratio [AOR] = 18.06; 95% CI [14.80 to 22.05], P < 0.001), age (> 60) (AOR = 1.11; [1.02, 1.21], P = 0.04), a history of diabetes (AOR = 1.29; [1.17, 1.44], P < 0.001), CAD (AOR = 1.39; [1.23 to 1.55], P < 0.001), and PVD (AOR = 1.29; [1.13 to 1.46], P = 0.001) were associated with increased CVC use. Male sex (AOR = 0.63; [0.57 to 0.70], P < 0.001), higher BMI (AOR = 0.98; [0.97 to 0.99], P < 0.001), and a history of hypertension (AOR = 0.76; [0.65 to 0.89], P = 0.01) was associated with lower CVC use. Compared with the 2001 cohort, CVC use was similar to the 2002 cohort (AOR = 1.08; [0.94 to 1.24], P = 0.31) but progressively higher in the 2003 cohort (AOR = 1.23; [1.07 to 1.44], P = 0.004) and 2004 cohort (AOR = 1.38; [1.20 to 1.58], P < 0.001). Crude and adjusted proportions of AVF/AVG and CVC are as shown in Table 2.
Table 2.
Type of vascular access in use (unadjusted and risk-adjusted expected percentage) by cohort
| Incident cohorts | N | AVF/AVG, %
|
CVC, %
|
||||
|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | ||||
| 2001 | 3623 | 23.3 | 23.9 | 76.7 | 76.1 | ||
| 2002 | 3638 | 23.4 | 23.7 | 76.6 | 76.3 | ||
| 2003 | 3698 | 22.1b | 22.7b | 77.9b | 77.3b | ||
| 2004 | 3748 | 21.0b | 21.1b | 79.0b | 78.9b | ||
| Prevalent cohorts | N | AVF, %
|
AVG, %
|
CVC, %
|
|||
|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedc | Unadjusted | Adjustedc | Unadjusted | Adjustedc | ||
| 2001 | 8239 | 46.9 | 45.6 | 11.4 | 9.0 | 41.8 | 45.4 |
| 2002 | 10585 | 47.7 | 45.0 | 10.6 | 9.0 | 41.7 | 46.0 |
| 2003 | 10384 | 43.2 | 44.7 | 7.7 | 8.9 | 49.1b | 46.4 |
| 2004 | 11084 | 41.6 | 44.5 | 6.7 | 8.9 | 51.7b | 46.6 |
Adjusted for age, sex, race, body mass index, late referral, smoking status, etiology of end-stage renal disease, history of diabetes, coronary artery disease, peripheral vascular disease, cerebrovascular disease, and hypertension.
P < 0.05 vs. 2001.
Adjusted for age, sex, race, body mass index, late referral, smoking status, etiology of end-stage renal disease, history of diabetes, coronary artery disease, peripheral vascular disease, cerebrovascular disease, hypertension, and dialysis vintage.
To exclude the effect of late referral, the analysis of incident patients was restricted to only patients seen by a nephrologist at least 3 mo before initiating hemodialysis. Consistent with the previous analysis, there was a significant and clinically important trend toward increased CVC use from 2001 to 2004.
Prevalent Cohorts
Of 56,072 prevalent patients, 15,780 (28.1%) did not have a vascular access recorded and were ineligible for this study. The distributions of patient characteristics for the study population by prevalent cohort and for those excluded from this study are shown in Table 3. Among the study patients, there was a significant increase in age, obesity, and proportion with diabetes, hypertension, and on dialysis for >24 mo over time. Figure 2 depicts the decrease in the crude rates of prevalent AVF and AVG use with an increase in CVC use over time.
Table 3.
Characteristics of hemodialysis patients by prevalent cohort
| Variable | 2001 | 2002 | 2003 | 2004 | Excluded patients |
|---|---|---|---|---|---|
| No. of patients | 8239 | 10,585 | 10,384 | 11,084 | 15,780 |
| Age, years (median) | 66.0 | 67.0 | 67.0 | 67.0 | 64.0 |
| Male | 58.7 | 57.5 | 57.6 | 57.9 | 60.2 |
| Race | |||||
| white | 71.5 | 71.8 | 71.9 | 72.3 | 63.2 |
| indigenous | 5.8 | 5.7 | 5.9 | 6.1 | 3.6 |
| other | 22.7 | 22.5 | 22.2 | 21.7 | 33.2 |
| BMI, kg/m2 (median) | 25.5 | 25.6 | 25.9 | 26.0 | 25.5 |
| Late referral | |||||
| <3 months, % | 34.2 | 32.6 | 30.8 | 29.7 | 30.5 |
| Smoker, % | |||||
| current | 13.1 | 13.3 | 13.2 | 13.3 | 9.9 |
| Time on dialysis, % | |||||
| <24 months | 49.8 | 46.7 | 47.8 | 45.2 | 25.0 |
| 24-47 months | 21.1 | 22.1 | 23.8 | 25.9 | 26.7 |
| 48-72 months | 11.3 | 12.5 | 11.1 | 11.1 | 19.8 |
| >72 months | 17.4 | 18.5 | 17.1 | 17.5 | 27.6 |
| Cause of ESRD (%) | |||||
| glomerulonephrities | 15.8 | 15.3 | 14.6 | 14.4 | 19.8 |
| diabetes mellitus | 30.0 | 31.5 | 33.0 | 34.0 | 26.6 |
| hypertension | 12.6 | 12.2 | 12.8 | 12.2 | 10.2 |
| other | 40.8 | 40.1 | 38.5 | 37.6 | 40.3 |
| unknown | 0.9 | 0.9 | 1.1 | 1.7 | 3.4 |
| Comorbidities, % | |||||
| diabetes mellitus | 37.7 | 39.2 | 40.8 | 41.6 | 33.02 |
| coronary artery disease | 22.2 | 21.8 | 22.7 | 22.8 | 17.6 |
| peripheral vascular disease | 16.5 | 17.1 | 17.0 | 17.0 | 13.5 |
| cerebrovascular disease | 11.1 | 11.1 | 11.7 | 12.0 | 7.8 |
| hypertension | 76.1 | 77.2 | 78.7 | 79.5 | 70.0 |
Figure 2.
Distribution (%) of vascular access type among prevalent hemodialysis patients (unadjusted).
In the multivariate analysis, variables associated with increased CVC compared with AVF use included age (AOR = 1.08 per 10 yr; [1.04 to 1.12]; P < 0.001), late referral (AOR 2.99; [2.64 to 3.4], P < 0.001), history of diabetes (AOR 1.39; [1.24 to 1.57], P < 0.001), CVD (AOR 1.24; [1.08 to 1.42], P < 0.001), and PVD (AOR = 1.28; [1.10 to 1.48], P < 0.001). Male sex (AOR = 0.49; [0.43 to 0.55], P < 0.001), indigenous (versus white) (AOR = 0.77; [0.60 to 0.98], P < 0.03) was associated with lower CVC use. Compared with patients using an AVF, increased use of AVG was associated with CAD (AOR = 1.41 [1.07 to 1.385]; P < 0.02), whereas male gender (AOR = 0.45; [0.35 to 0.56]; P = 0.03) was associated with greater AVF use. Dialysis vintage (length of time on dialysis) was associated with decreased CVC use. Adjustment for patient characteristics did not significantly change the trends in access use, as shown in Table 2.
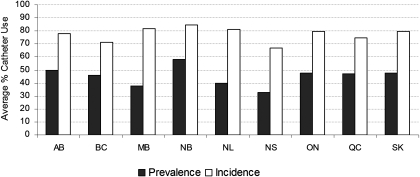
There was significant variability in the use of both incident and prevalent catheters among the provinces (Figure 3). Incident catheter use ranged from 83% in New Brunswick to 68% in Nova Scotia. Prevalent catheter use ranged from 58% in New Brunswick to 32% in Nova Scotia. After adjusting for differences in demographic and comorbid factors, these differences persisted as shown in Table 4. The odds of starting dialysis with a catheter were 49% lower in Nova Scotia with 67% lower prevalent catheter use compared with Ontario.
Figure 3.
Average percentage catheter use between 2001 and 2004 by province (unadjusted). AB, Alberta; BC, British Columbia; MB, Manitoba; NB, New Brunswick; NS, Nova Scotia; ON, Ontario; QC, Quebec; SK, Saskatchewan.
Table 4.
Incident and prevalent catheter use by province for the whole cohort
| Province | Incident catheter use, aOR (95% CI)a | Prevalent catheter use, aOR (95% CI)b |
|---|---|---|
| Ontario (as reference) | 1.0 | 1.0 |
| Alberta | 0.85 (0.72-1.0) | 0.88 (0.73-1.00) |
| British Columbia | 0.63 (0.52-0.77) | 0.87 (0.70-1.09) |
| Manitoba | 1.12 (0.88-1.42) | 0.65 (0.51-0.83) |
| New Brunswick | 1.37 (0.99-1.90) | 1.58 (1.08-2.30) |
| Newfoundland | 1.16 (0.85-1.57) | 1.22 (0.85-1.74) |
| Nova Scotia | 0.51 (0.40-0.65) | 0.33 (0.24-0.44) |
| Quebec | 0.62 (0.55-0.71) | 0.84 (0.73-0.97) |
| Saskatchewan | 0.80 (0.63-1.01) | 0.59 (0.46-0.77) |
Adjusted for age, gender, body mass index, late referral, diabetes mellitus, coronary artery disease, and peripheral vascular disease.
Adjusted for age, gender, body mass index, late referral, diabetes mellitus, coronary artery disease, peripheral vascular disease, and time on dialysis.
HRs for patient survival are shown in Figure 4. Use of a CVC as the incident access had a 1.6 times greater risk of death compared with use of an AVF or AVG combined (HR, 1.60; [1.45 to 1.75], P < 0.001). Other variables associated with increased risk of death were increasing age (per year) (HR, 1.47; [1.42 to 1.51], P < 0.001), late referral (versus early) (HR, 1.18; [1.09 to 1.27], P < 0.001), smokers (versus quit or nonsmoker) (HR, 1.19; [1.08 to 1.30], P < 0.003), history of diabetes (HR, 1.25; [1.16 to 1.34], P < 0.001), CAD (HR, 1.22; [1.13 to 1.31], P < 0.001), PVD (HR, 1.31; [1.21 to 1.41], P < 0.001), and CVD (HR, 1.12; [1.03 to 1.22], P = 0.01). This association persisted when late referrals were excluded from the analysis.
Figure 4.
Hazard ratios for death by Cox regression. •, point estimate (with 95% confidence interval represented by the bars). *Central venous catheter compared with AVF and AVG combined. **Compared with 2001. CAD, coronary artery disease; PVD, peripheral vascular disease.
Discussion
This study reports a number of concerning findings about vascular access use in the Canadian hemodialysis population after the introduction of national guidelines recommending the fistula as the preferred access (9). Most importantly, we identified a significant mortality risk associated with initiation of dialysis with a catheter in a large cohort of incident hemodialysis patients. We also confirmed the high and increasing use of CVCs and declining use of AVFs and AVGs with significant differences in vascular access use among provinces. Adjustment for patient characteristics and demographics did not change the significance of these trends suggesting differences in unidentified practice patterns, attitudes, or patient preference.
Use of CVCs among incident patients in Canada is associated with the same increased risk of mortality as identified by others (5,10), although not as great an association as identified in the Australian/New Zealand population (4). Some may suggest that, with more frequent use of catheters, management of complications would be improved, with subsequent improved outcomes. This is not the case in Canada. Catheters are associated with increased mortality even with late referrals excluded. Nephrology programs must review their process of care to identify opportunities to decrease the use of catheters and its associated complications. The biologic plausibility to explain this increased risk is not explored in this study. It is well documented that infections are more common in CVC-dependent patients than in those using a permanent access (11), and it is postulated that use of catheters increase inflammation, which has been associated with increased cardiovascular risk (12).
Canada has had one of the highest rates of CVC use, trailing only behind Belgium in prevalent use and even higher than the 70% incident use and 33% prevalent use (13) reported in the 2003 Canadian DOPPS cohort (6). The use of CVCs has increased over time despite national guidelines (9) and initiatives, such as Fistula First (14). Differences in patient characteristics and comorbidities did not explain the vascular access usage patterns, in either the overall Canadian trends or with the provincial variation. This is similar to data recently reported from Australia, which showed an increase in catheter use, not influenced by changes in patient characteristics (7) and suggests that differences in practice patterns or patient preference are contributing to the decrease in fistulae and grafts and the increase in catheters.
The type of vascular access at the first dialysis has been used as a marker of predialysis care (15–17). Late referrals to nephrology had a greater than 18-fold risk of starting dialysis with a CVC, and this association persisted in the prevalent cohort, highlighting its role as a potentially modifiable risk factor. More importantly, late referral was independently associated with increased mortality; however, the association between increased mortality and CVC use persisted even when the late referrals were excluded from the analysis. Although we note a decrease in the number of late referrals over the time period studied, data from DOPPS suggest that, in Canada, patients wait an average of 61.7 d from the time of referral to creation of a permanent vascular access; thus, patients referred <3 mo by necessity must start hemodialysis with a CVC or AVG (8). As well, there are fewer vascular surgeons per 100 hemodialysis patients in Canada compared with either Europe or the United States and Canadian surgeons devote fewer hours to access surgery, all of which may be contributing to the increased use of incident catheters, but it does not explain the persistent use of catheters among prevalent patients. Starting dialysis with a catheter is a strong predictor of subsequent catheter use, as indicated by the Nova Scotia data from this study.
Earlier referral to the nephrologist and timely access to a surgeon may improve the rate of AVF creation, but this does not necessarily equate to an increase in functioning AVFs. Fistulas that fail to mature (FTM) are increasingly more common with rates between 9% and 70% (18,19) and the highest FTM rates among the elderly, diabetics, and those with vascular disease (19), the same group that represents the largest growth in dialysis. When this early fistula failure is considered in cumulative patency analysis, there is little difference compared with graft patency (20,21). The role of a graft needs to be reconsidered given the conquerable patency and the trade off between interventions required to get a fistula to maturation versus intervention to maintain patency in a graft (22), and the shortened time from creation to use.
In this study, it is important to note that the use of both AVGs and AVFs decreased among the prevalent population with a subsequent increase in the rate of CVCs. The evidence associating AVG use with increased mortality compared with AVF use is perhaps less convincing and certainly not at the same risk level as use of a CVC (5,10,23). In prevalent patients, AVG use has only been associated with a greater risk of mortality among patients with diabetes (24). Prospective studies of incident patients and their accesses have demonstrated no difference in mortality between those using AVF and AVG (10,25). The higher rates of FTM in fistulae with subsequent use of a CVC and the lower mortality of grafts compared with CVC identify the need to reexamine the role of the AVG. Studies comparing outcomes between grafts and CVCs are needed particularly among patients with previous failed attempts at a fistula or where there is insufficient time for the fistula to mature. Adopting a philosophy of “lines last” may complement the “fistula first” initiative along with an aggressive program to convert existing catheters to a permanent access.
Several authors have identified changes in the process of care to improve the rate of AVF use among incident patients (22,26,27), and one author suggests financial incentive based on the cost-effectiveness of the AVF (28). Understanding patient preference, beliefs, values, and reasons for refusal will be necessary to appropriately address this significant proportion of eligible patients who simply refuse a permanent access. Several authors have also highlighted the role of vascular access education to patients and staff, use of vascular mapping, salvage of early AVF failures, and thrombectomy of clotted fistulae as possible measures to reduce the use of CVCs (20,27,29).
We have identified significant regional differences in vascular access practice patterns across the provinces in Canada, which persisted after adjustment for patient characteristics. This is similar to regional differences in Australia (23) and the United States (30). These differences in practice patterns are likely multifactorial and cannot be described using these data. As highlighted by Polkinghorne et al. (23), physician and nursing attitudes may play a role (31), as well as surgical wait times, surgical expertise, and patient preferences. These differences in practice pattern afford an opportunity to examine in detail the practice in those provinces with a higher fistula rates to identify opportunities for improvement in centers with lower rates of AVF use. These health outcomes studies will address the questions raised but not answered in this study of registry data.
The limitations of our study are those inherent with the use of observational data. AVFs and AVGs were combined in the incident cohorts because of the small number of patients using an AVG. The CORR registry only collects the access in use at the end of the survey period, so we were unable to examine whether another access had failed during the survey period or was present but not in use. Therefore, we could not describe access attempts, FTM rates, access to vascular surgery, practice preferences, and other explanatory variables. Data on mortality and comorbidities as reported to CORR have not been validated. The unique value of our study is the ability to trend access use in an industrialized multiethnic country that provides universal health care and underscores the consistent mortality increase in CVC use. These data should clearly dispel any thoughts that more frequent use of CVCs leads to better management and outcomes. It should engender a sense of urgency to ensure provision of timely predialysis care with a focus on dialysis initiation with a functioning permanent access, the close examination of practice patterns, and the reevaluation of strategies to limit CVC use.
Conclusion
We have demonstrated that patients initiating hemodialysis with a catheter have a significant increase in associated risk of death compared with those using a fistula or graft. We have demonstrated an increasing reliance on catheters in all patients with a subsequent decline in the use of fistula and grafts. There are significant regional differences in patterns of vascular access use, which are not explained by differences in patient characteristics. These data provide strong evidence for the urgent examination and change in practice to ensure timely predialysis care to enable dialysis initiation with a functioning permanent access, adequate resources, and ongoing processes to attain high prevalent permanent access, to limit patient morbidity and mortality by achieving “lines last.”
Disclosures
None.
Acknowledgments
The authors thank the staff of the renal units throughout Canada submitting information to CORR and the staff at CORR for maintaining the database.
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Jindal K, Ethier D, Lindsay RM, Barre P, Kappel JE, Carlisle EJ, Common A: Clinical practice guidelines for vascular access. J Am Soc Nephrol 10[Suppl]: S287–S305, 1999 [PubMed] [Google Scholar]
- 2.Hirth RA, Turenne MN, Woods JD, Young EW, Port FK, Pauly MV, Held PJ: Predictors of type of vascular access in hemodialysis patients. JAMA 276: 1303–1308, 1996 [PubMed] [Google Scholar]
- 3.Manns B, Tonelli M, Yilmaz S, Lee H, Laupland K, Klarenbach S, Radkevich V, Murphy B: Establishment and maintenance of vascular access in incident hemodialysis patients: a prospective cost analysis. J Am Soc Nephrol 16: 201–209, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vascular access and all-cause mortality: a propensity score analysis. J Am Soc Nephrol 15: 477–486, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Xue JL, Dahl D, Ebben JP, Collins AJ: The association of initial hemodialysis access type with mortality outcomes in elderly Medicare ESRD patients. Am J Kidney Dis 42: 1013–1019, 2003 [DOI] [PubMed] [Google Scholar]
- 6.K-DOQI: Clinical practice guidelines for vascular access. Am J Kidney Dis 48[Suppl]: S248–S273, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Moist LM, Chang SH, Polkinghorne KR, McDonald SP: Trends in hemodialysis vascular access from the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) 2000 to 2005. Am J Kidney Dis 50: 612–621, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Mendelssohn DC, Ethier J, Elder SJ, Saran R, Port FK, Pisoni RL: Haemodialysis vascular access problems in Canada: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS II). Nephrol Dial Transplant 21: 721–728, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF: Vascular access. J Am Soc Nephrol 17[Suppl 1]: S16–S23, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J: Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Allon M, Depner TA, Radeva M, Bailey J, Beddhu S, Butterly D, Coyne DW, Gassman JJ, Kaufman AM, Kaysen GA, Lewis JA, Schwab SJ: Impact of dialysis dose and membrane on infection-related hospitalization and death: results of the HEMO Study. J Am Soc Nephrol 14: 1863–1870, 2003 [DOI] [PubMed] [Google Scholar]
- 12.van Leuven SI, Franssen R, Kastelein JJ, Levi M, Stroes ES, Tak PP: Systemic inflammation as a risk factor for atherothrombosis. Rheumatology (Oxf). 47: 3–7, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Port FK, Pisoni RL, Bommer J, Locatelli F, Jadoul M, Eknoyan G, Kurokawa K, Canaud BJ, Finley MP, Young EW: Improving outcomes for dialysis patients in the International Dialysis Outcomes and Practice Patterns Study. Clin J Am Soc Nephrol 1: 246–255, 2006 [DOI] [PubMed] [Google Scholar]
- 14.Fistula First National Vascular Access Improvements Initiative. Available at http://www.fistulafirst.org. Accessed January 19, 2007.
- 15.Lorenzo V, Martn M, Rufino M, Hernandez D, Torres A, Ayus JC: Predialysis nephrologic care and a functioning arteriovenous fistula at entry are associated with better survival in incident hemodialysis patients: an observational cohort study. Am J Kidney Dis 43: 999–1007, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton J: The timely construction of arteriovenous fistulae: a key to reducing morbidity and mortality and to improving cost management. Nephrol Dial Transplant 20: 598–603, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Stehman-Breen CO, Sherrard DJ, Gillen D, Caps M: Determinants of type and timing of initial permanent hemodialysis vascular access. Kidney Int 57: 639–645, 2000 [DOI] [PubMed] [Google Scholar]
- 18.Dixon BS: Why don’t fistulas mature? Kidney Int 70: 1413–1422, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D: Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas. J Am Soc Nephrol 17: 3204–3212, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Allon M, Lockhart ME, Lilly RZ, Gallichio MH, Young CJ, Barker J, Deierhoi MH, Robbin ML: Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis patients. Kidney Int 60: 2013–2020, 2001 [DOI] [PubMed] [Google Scholar]
- 21.Oliver MJ, McCann RL, Indridason OS, Butterly DW, Schwab SJ: Comparison of transposed brachiobasilic fistulas to upper arm grafts and brachiocephalic fistulas. Kidney Int 60: 1532–1539, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Lok CE: Fistula first initiative: advantages and pitfalls. Clin J Am Soc Nephrol 2: 1043–1053, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Epidemiology of vascular access in the Australian hemodialysis population. Kidney Int 64: 1893–1902, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK: Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 60: 1443–1451, 2001 [DOI] [PubMed] [Google Scholar]
- 25.Allon M, Ornt DB, Schwab SJ, Rasmussen C, Delmez JA, Greene T, Kusek JW, Martin AA, Minda S: Factors associated with the prevalence of arteriovenous fistulas in hemodialysis patients in the HEMO study: Hemodialysis (HEMO) Study Group. Kidney Int 58: 2178–2185, 2000 [DOI] [PubMed] [Google Scholar]
- 26.Allon M, Robbin ML: Increasing arteriovenous fistulas in hemodialysis patients: problems and solutions. Kidney Int 62: 1109–1124, 2002 [DOI] [PubMed] [Google Scholar]
- 27.Lok CE, Oliver MJ: Overcoming barriers to arteriovenous fistula creation and use. Semin Dial 16: 189–196, 2003 [DOI] [PubMed] [Google Scholar]
- 28.Schon D, Blume SW, Niebauer K, Hollenbeak CS, de Lissovoy G: Increasing the use of arteriovenous fistula in hemodialysis: economic benefits and economic barriers. Clin J Am Soc Nephrol 2: 268–276, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Lenz O, Sadhu S, Fornoni A, Asif A: Overutilization of central venous catheters in incident hemodialysis patients: reasons and potential resolution strategies. Semin Dial 19: 543–550, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Reddan D, Klassen P, Frankenfield DL, Szczech L, Schwab S, Coladonato J, Rocco M, Lowrie EG, Owen WF Jr: National profile of practice patterns for hemodialysis vascular access in the United States. J Am Soc Nephrol 13: 2117–2124, 2002 [DOI] [PubMed] [Google Scholar]
- 31.Young EW, Dykstra DM, Goodkin DA, Mapes DL, Wolfe RA, Held PJ: Hemodialysis vascular access preferences and outcomes in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 61: 2266–2271, 2002 [DOI] [PubMed] [Google Scholar]