Abstract
Study Objectives:
To evaluate the amplitude of submentalis muscle EMG activity during sleep in patients with narcolepsy/cataplexy with or without REM sleep behavior disorder (RBD).
Design:
Observational study with consecutive recruitment.
Settings:
Sleep laboratory.
Patients:
Thirty-four patients with narcolepsy/cataplexy and 35 age-matched normal controls.
Measurements and results:
Half the patients (17 subjects) had a clinical and video polysomnographic diagnosis of RBD. The average amplitude of the rectified submentalis muscle EMG signal was used to assess muscle atonia, and the new REM sleep Atonia Index was computed. Chin muscle activations were detected and their duration and interval analyzed. REM sleep Atonia Index was lower in both patient groups (with narcolepsy patients with RBD showing the lowest values) with respect to controls, and it did not correlate with age as it did in controls. The total number of chin EMG activations was significantly higher in both patient groups than controls. No significant differences were found between the two groups of patients, although more chin EMG activations were noted in narcolepsy patients with RBD than those without.
Conclusions:
Elevated muscle activity during REM sleep is the only polysomnographic marker of RBD. This study shows that polysomnographically evident RBD is present in many patients with narcolepsy/cataplexy. This condition might be specific to narcolepsy/cataplexy, reflecting a peculiar form of REM sleep related motor dyscontrol (i.e., status dissociatus), paving the way to enacting dream behaviors, and correlated with the specific neurochemical and neuropathological substrate of narcolepsy/cataplexy.
Citation:
Ferri R; Franceschini C; Zucconi M; Vandi S; Poli F; Bruni O; Cipolli C; Montagna P; Plazzi G. Searching for a marker of REM sleep behavior disorder: submentalis muscle EMG amplitude analysis during sleep in patients with narcolepsy/cataplexy. SLEEP 2008;31(10):1409–1417.
Keywords: Narcolepsy/cataplexy, REM sleep behavior disorder, submentalis EMG, quantitative analysis, polysomnography
REM SLEEP BEHAVIOR DISORDER (RBD), FIRST DESCRIBED AS A CLINICAL ENTITY IN 1986 BY SCHENCK AND COWORKERS,1 HAD BEEN OBSERVED EVEN earlier in narcoleptic patients and termed “ambiguous sleep”2 because of its “low phasic atonia with an extreme abundance of twitches and muscular discharges.” RBD is currently classified as a parasomnia related to REM sleep, characterized by loss of the stage-specific muscle atonia, and a frequent enactment of violent dream content resulting in self or bed-partner injuries. Polygraphically, tonic and phasic electromyographic activity is evident during REM sleep. When not symptomatic, this activity is called REM sleep without atonia (RWA). The importance of this altered sleep stage-dependent muscular activity was stressed in the latest international classification of sleep disorders, the ICSD-2.3 Indeed, this classification advises considering a diagnosis of RBD in the “presence of REM sleep without atonia,” but no quantitative parameters are given.
The prevalence of RBD in narcolepsy/cataplexy seems to be fairly high: according to two recent studies, it is clinically evident in 45% to 61% of patients and polysomnographically detectable in 36% to 43% of them.4,5 Patients with narcolepsy/cataplexy are more frequently affected by RBD than those without cataplexy4 and in many narcolepsy/cataplexy patients RBD can be induced or aggravated by anti-cataplectic treatment (antidepressants).6 RBD may also be an early sign in childhood narcolepsy/cataplexy.7
An increased electromyographic activity during REM sleep has frequently been observed in narcoleptic patients without RBD.8 The prevalence of RWA, phasic EMG activity, and REM density is also higher in these patients than in controls,9 whereas patients with idiopathic RBD have a higher prevalence of RWA and a lower REM density than narcoleptic patients and controls.10 RBD in narcolepsy also differs from the idiopathic form because of its much earlier age of onset5,6 and different sex ratio (in the idiopathic form, RBD mostly affects men).4–6
Despite the crucial relevance of the increased chin EMG activity during REM sleep for the diagnosis of RBD, the reliability of polysomnographic criteria for the identification of RWA is largely unexplored.11 There have been very few systematic attempts to measure submentalis muscle EMG activity during sleep,12 probably because of decades of paper recordings in sleep research. Few literature reports have quantified submentalis muscle EMG activity in RBD patients,13–15 and only one included narcoleptic patients.10
This study aimed to evaluate the quantitative amplitude of submentalis muscle EMG activity during sleep in patients with narcolepsy/cataplexy, without or with RBD, in comparison to normal controls. In addition to a visual quantitative approach following the criteria set by Lapierre and Montplaisir in 1992,13 we adopted a new computer quantitative analysis describing both basal and transient modifications in chin EMG amplitude during sleep in normal controls and idiopathic and symptomatic RBD patients.16
SUBJECTS AND METHODS
Subjects
Thirty-four patients with narcolepsy/cataplexy were consecutively recruited for this study at the Sleep Disorders Center of the Department of Neurological Sciences, University of Bologna, together with 35 age-matched normal controls. Clinical and demographic characteristics of patients are listed in Table 1. The diagnosis of narcolepsy/cataplexy was based on the International Classification of Sleep Disorders (ICSD-2) criteria.3 All patients had ≥ 2 sleep onset REM-sleep episodes upon the multiple sleep latency test (MSLT), cataplexy and excessive daytime sleepiness, reflected by a mean sleep latency at the MSLT ≤ 8 min, and all carried the human leukocyte antigen (HLA) DQB1*0602. Diagnosis of RBD was also based on the ICSD-2 criteria,3 including presence of REM sleep without atonia, sleep related injurious-disruptive behaviors by history—following a semistructured clinical interview described elsewhere,17 administered to the patients and, whenever possible, to their bed partners, evaluating RBD symptomatology and frequency of episodes18—and abnormal sleep behaviors documented during polysomnographic monitoring, absence of EEG epileptiform activity during REM sleep, and sleep disturbance not better explained by another sleep disorder, medical or neurological disorder, mental disorder, medication use, or substance use disorder.
Table 1.
Clinical and Demographic Characteristics of Patients
| Patient | Sex | Age | Age at onset, years |
SP | HH | AB | DNS | Therapy withdraw one month before admission, daily dose | Therapy at PSG time, daily dose | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| EDS | Cataplexy | RBD | |||||||||
| 1 | M | 36 | 10 | 18 | − | + | + | + | + | Valproic Acid 1,250 mg; Citalopram 20 mg | |
| 2 | M | 41 | 33 | 33 | − | + | − | − | + | drug naive | |
| 3 | F | 52 | 49 | 50 | − | − | − | − | − | Paroxetine 20 mg | |
| 4 | M | 35 | 13 | 15 | − | − | − | − | + | drug naive | |
| 5 | M | 44 | 33 | 33 | − | + | + | + | + | drug naive | |
| 6 | F | 33 | 18 | n.a. | − | + | + | + | − | drug naive | |
| 7 | F | 20 | 12 | 12 | − | + | + | − | + | drug naive | |
| 8 | F | 73 | 45 | 44 | − | − | − | − | + | Enalapril 10 mg | Thyroxine sodium 50 mg; Furosemide 25 mg |
| 9 | F | 18 | 10 | 16 | − | + | + | + | − | Modafinil 100 mg | |
| 10 | F | 23 | 9 | 22 | − | − | + | − | + | drug naive | |
| 11 | M | 31 | 18 | 18 | − | − | − | + | − | drug naive | |
| 12 | F | 37 | 29 | 29 | − | + | + | + | + | Modafinil 100 mg; Venlafaxine 75 mg | |
| 13 | M | 59 | 48 | n.a. | − | − | − | − | − | Fluoxetine 60 mg | |
| 14 | M | 67 | 13 | 13 | − | − | − | + | + | drug naive | Nifedipine 40 mg; Perindopril 2 mg |
| 15 | M | 44 | 40 | n.a. | − | − | − | − | − | drug naive | |
| 16 | M | 35 | 15 | 15 | − | + | − | − | + | drug naive | |
| 17 | F | 34 | 19 | 19 | − | + | + | − | + | drug naive | |
| 18 | M | 66 | 10 | 40 | 50 | − | − | − | − | Sertraline 50 mg; Flurazepam 15 mg | Metformin 500 mg; Alfuzosin 10 mg |
| 19 | F | 36 | 24 | 24 | 24 | + | + | − | + | drug naive | |
| 20 | M | 25 | 10 | 10 | 15 | − | − | + | + | Imipramine 30 mg | |
| 21 | M | 32 | 11 | 11 | 12 | − | + | − | − | Modafinil 100 mg | |
| 22 | F | 41 | 15 | 16 | 20 | − | + | + | + | Modafinil 100 mg | |
| 23 | F | 59 | 45 | 47 | 50 | + | + | + | + | Modafinil 200 mg; Clomipramine 50 mg | |
| 24 | M | 75 | 18 | 20 | 22 | − | − | − | + | Modafinil 100 mg | |
| 25 | M | 31 | 15 | 26 | 28 | + | + | + | + | drug naive | |
| 26 | M | 55 | 44 | 44 | 50 | − | + | + | + | drug naive | |
| 27 | M | 38 | 17 | 20 | 20 | + | + | + | + | drug naive | |
| 28 | M | 24 | 7 | n.a. | 16 | − | − | − | − | drug naive | |
| 29 | M | 44 | 22 | 22 | 19 | − | + | + | + | drug naive | |
| 30 | M | 50 | 16 | 15 | 18 | − | + | − | + | drug naive | |
| 31 | M | 30 | 18 | 20 | 24 | + | + | + | + | Modafinil 200 mg | |
| 32 | F | 35 | 14 | 14 | 25 | + | + | + | − | drug naive | |
| 33 | M | 36 | 28 | n.a. | 30 | − | − | − | − | drug naive | |
| 34 | M | 20 | 18 | 19 | 19 | − | − | − | − | drug naive | |
EDS = Excessive daytime sleepiness; SP = sleep paralysis; HH = hypnagogic/hypnopompic hallucinations; AB = automatic behaviors; DNS = disturbed nocturnal sleep; n.a. = not available; + = present; − = absent.
Patients were recorded on average within 18.6 years (SD 2.81, range 2–57 years) from the beginning of narcolepsy clinical symptoms, and all had been drug-free ≥ 3 weeks at the time of the polysomnographic recording.
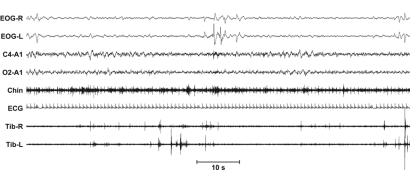
None of the 35 normal subjects had any physical, neurological or psychiatric disorder or history of sleep problems, and none was taking medication at the time of recording. Exclusion criteria included (a) a sleep disorder diagnosis (including sleep apnea); (b) a major mental illness; (c) a significant history of cognitive difficulties; (d) prior (within one year) or current use of a neuroleptic agent or SSRIs, venlafaxine; and (e) history of alcohol or other substance abuse.
Nocturnal Polysomnography
Nocturnal polysomnography was carried out after a night of adaptation in a standard sound-attenuated (noise level to a maximum of 30 dB nHL) sleep laboratory room, under video recording monitoring. Subjects were not allowed caffeinated beverages the afternoon preceding the recording and were allowed to sleep until they awoke spontaneously in the morning. Lights-out time was based on individual habitual bedtime and ranged between 21:30 and 23:30. The following signals were recorded: EEG (at least 2 channels, one central and one occipital, referred to the contralateral earlobe); electrooculogram (electrodes placed 1 cm above the right outer cantus and 1 cm below the left outer cantus and referred to A1), electromyogram (EMG) of the submentalis muscle (bipolar derivations with 2 electrodes placed 3 cm apart and affixed using a collodion-soaked gauze pad), impedance was kept less than 10 KΩ (typically <5 KΩ), EMG of the right and left tibialis anterior muscles, and ECG (one derivation). Sleep signals were sampled at 200 or 256 Hz and stored on hard disk in European data format (EDF)19 for further analysis. The sleep respiratory pattern of each patient was monitored using oral and nasal airflow thermistors and/or nasal pressure cannula, thoracic and abdominal respiratory effort strain gauge, and by monitoring oxygen saturation (pulse-oximetry). This had been performed in all subjects in a previous recording (within one week) by means of a portable cardiorespiratory monitor or during the study recording; patients with an apnea/hypopnea index ≥ 5 were not included. Sleep stages were scored following standard criteria20 on 30-sec epochs; since muscle atonia can be absent in RBD, REM sleep was scored without submental EMG atonia, using electroencephalogram and electrooculogram only. According to a method specifically developed for RBD,10,13 onset of a REM sleep period was defined as the occurrence of the first rapid eye movement in the presence of an EEG signal characteristic of REM sleep (low amplitude mixed frequencies, absence of sleep spindles and K complexes). Offset of a REM sleep period was determined by the occurrence of a specific EEG feature indicative of another stage (K complex, sleep spindle, or EEG signs of arousal) or absence of rapid eye movements during 3 consecutive minutes. Figure 1 shows an example of REM sleep without atonia scored following these criteria. Epochs containing technical artifact or extremely elevated muscle activity causing saturation of amplifiers were carefully detected and marked for exclusion from the subsequent quantitative EMG analysis.
Figure 1.
Example of polysomnographic recording of REM sleep without atonia.
Quantification of Submentalis Muscle EMG Amplitude
For visual quantitative analysis, we first quantified the 2 parameters proposed by Lapierre and Montplaisir,13 adapted to our recordings, in REM sleep of all groups. First, each 30-sec epoch was scored as tonic or atonic, depending on whether tonic chin EMG activity was present for > 50% of the epoch; then, we calculated the percentage of total REM epochs scored as tonic. Second, we evaluated phasic EMG density as the percentage of the total number of 2-sec mini-epochs of REM sleep containing phasic EMG events (defined as any burst of EMG activity lasting 0.1–5 s, with an amplitude exceeding 4 times the background EMG activity).
For computer quantitative analysis, the submentalis muscle EMG signal was digitally band-pass filtered at 10–100 Hz, with a notch filter at 50 Hz and rectified. Subsequently, each sleep epoch included in the analysis was divided into 30 1-sec mini-epochs. The average amplitude of the rectified submentalis muscle EMG signal was then obtained for each mini-epoch. The values of the submentalis muscle EMG signal amplitude in each mini-epoch were used to draw normalized distribution histograms for each sleep stage (REM, S1, S2, and SWS) of the percentage of values in the following 20 amplitude (amp) classes (expressed in μV): amp ≤ 1, 1 < amp ≤ 2, …, 18 < amp ≤ 19, amp > 19. In these graphs, muscle atonia is expected to be reflected by high values of the first left column while phasic and tonic activations are expected to increase the value of the other columns.16 As proposed in our recent validation study,16 an index summarizing the degree of preponderance of the first column in these graphs in a single value was used in REM sleep:
Sleep Atonia Index = amp ≤ 1 /(100 − 1<amp ≤ 2).
Mathematically, this index can vary from 0 (absence of mini-epochs with amp ≤ 1), i.e., complete absence of EMG atonia, to 1 (all mini-epochs with amp ≤ 1) or stable EMG atonia in the epoch.
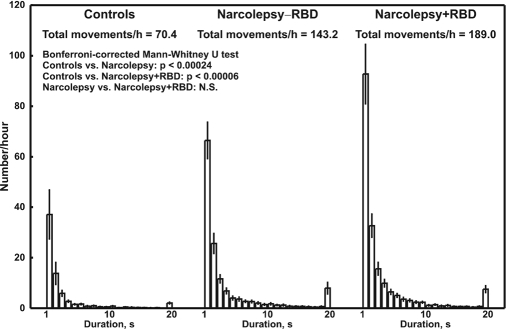
Finally, we also counted all sequences of consecutive mini-epochs exceeding the value of 2 μV and calculated their number per hour for REM sleep. These data were also used to draw normalized distribution histograms within the following 20 duration (dur) classes (expressed in s): dur = 1, dur = 2, …, dur = 19, dur > 19.
Statistical Data Analysis
All data were coded and analyzed blind to the subject group upon completion of recruitment. Comparisons between groups were carried out using the nonparametric Mann-Whitney test for independent data sets, with the Bonferroni correction for multiple comparisons when needed. The correlation between REM sleep Atonia Index and age of subjects was evaluated by the nonparametric Spearman rank correlation coefficient. Finally, the Chi-square test was used for the comparison of the gender composition of the groups and the nonparametric Kruskal-Wallis ANOVA for the comparison of their age. Differences and correlations were considered significant when P < 0.05. The data analysis software system STATISTICA (StatSoft, Inc. 2004, version 6. www.statsoft.com) was used for statistical analysis.
RESULTS
After the application of the current criteria for the diagnosis of RBD3 and the analysis of the video-polysomnographic recordings, 17 of the 34 patients with narcolepsy/cataplexy were diagnosed with RBD (Narcolepsy+RBD) and 17 were not (Narcolepsy−RBD). Table 2 shows the details of the RBD signs observed at videopolysomnography, in each Narcolepsy+RBD patient; the complete narcolepsy symptom tetrad was present in 3 patients with Narcolepsy−RBD (21.4%) and in 4 Narcolepsy+RBD (28.6%) patients. All subsequent statistical analyses were carried out taking into account these 2 subgroups.
Table 2.
RBD Video-Polysomnographic Features of Narcolepsy+RBD Subjects Included in this Study
| Patient | Sex | Age | Age at onset, years |
Vocalizations | Simple and Complex Behaviors | ||
|---|---|---|---|---|---|---|---|
| EDS | Cataplexy | RBD | |||||
| 18 | M | 66 | 10 | 40 | 50 | talking | upper limb movements |
| 19 | F | 36 | 24 | 24 | 24 | talking, crying | reaching, crawling |
| 20 | M | 25 | 10 | 10 | 15 | talking | lower limb movements |
| 21 | M | 32 | 11 | 11 | 12 | talking | |
| 22 | F | 41 | 15 | 16 | 20 | talking | Grabbing |
| 23 | F | 59 | 45 | 47 | 50 | shouting | |
| 24 | M | 75 | 18 | 20 | 22 | laughing | Grabbing |
| 25 | M | 31 | 15 | 26 | 28 | talking | reaching, grabbing |
| 26 | M | 55 | 44 | 44 | 50 | shouting | arm flailing, gesturing, crawling |
| 27 | M | 38 | 17 | 20 | 20 | reaching, grabbing | |
| 28 | M | 24 | 7 | n.a. | 16 | laughing, shouting | upper/lower limb movements, sitting |
| 29 | M | 44 | 22 | 22 | 19 | laughing, shouting | upper/lower limb movements, arm flailing, reaching, crawling |
| 30 | M | 50 | 16 | 15 | 18 | arm flailing, reaching | |
| 31 | M | 30 | 18 | 20 | 24 | talking | grabbing, punching, kicking, attempts to jump out of bed |
| 32 | F | 35 | 14 | 14 | 25 | laughing, talking | Crawling |
| 33 | M | 36 | 28 | n.a. | 30 | laughing, talking | Grabbing |
| 34 | M | 20 | 18 | 19 | 19 | grabbing, gesturing, crawling | |
Age and Sex
Table 3 reports age and gender composition of the groups; only the Narcolepsy+RBD group is male predominant, with the other 2 groups having almost equal gender composition. This was due to the consecutive character of the recruitment that prevented us forming gender-balanced groups; however, the group differences in gender composition did not reach statistical significance (Chi-square test = 5.209, 0.1 > P > 0.05). The age of the subjects in the 3 groups was not statistically different at the nonparametric Kruskal-Wallis ANOVA.
Table 3.
Subjects Included in this Study
| total, n | males | females | Age, years ± SD (range) | |
|---|---|---|---|---|
| 1. Normal Controls | 35 | 15 | 20 | 40.2 ± 16.72 (24.5–76) |
| 2. Narcolepsy–RBD | 17 | 9 | 8 | 40.1 ± 15.35 (18–73) |
| 3. Narcolepsy+RBD | 17 | 13 | 4 | 41.0 ± 15.36 (20–75) |
Sleep Architecture
Table 4 shows the comparison between the different sleep scoring parameters obtained in the 3 groups of subjects. Both groups of patients showed the expected changes with respect to controls: namely longer time in bed, sleep period time, and total sleep time, shorter REM sleep latency, smaller percentage of sleep stage 2 and higher percentages of sleep stage 1 and REM sleep. No significant differences were found in sleep architecture between the 2 groups of patients with narcolepsy/cataplexy.
Table 4.
Comparison Between Sleep Scoring Parameters in the 3 Groups of Subjects
| 1. Controls (n=35) |
2. Narcolepsy−RBD (n=17) |
3. Narcolepsy+RBD (n=17) |
Mann-Whitney U test* |
||||||
|---|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | 1 vs. 2 P< |
1 vs. 3 P< |
2 vs. 3 P< |
|
| TIB, min | 457.4 | 63.19 | 508.4 | 79.72 | 521.0 | 73.47 | 0.021 | 0.006 | NS |
| SPT, min | 429.9 | 52.11 | 496.6 | 75.12 | 498.6 | 84.49 | 0.005 | 0.007 | NS |
| TST, min | 367.4 | 69.50 | 423.9 | 70.69 | 436.6 | 70.70 | 0.03 | 0.007 | NS |
| SOL, min | 20.1 | 24.01 | 6.2 | 2.77 | 16.8 | 33.13 | NS | NS | NS |
| FRL, min | 98.0 | 76.49 | 31.2 | 31.29 | 39.2 | 42.71 | 0.0009 | 0.006 | NS |
| SE% | 81.4 | 16.91 | 83.9 | 10.22 | 84.1 | 9.93 | NS | NS | NS |
| WASO, % | 14.1 | 15.65 | 14.1 | 9.82 | 12.3 | 7.63 | NS | NS | NS |
| S1, % | 4.1 | 4.07 | 12.6 | 6.71 | 12.9 | 5.81 | 0.00002 | 0.00001 | NS |
| S2, % | 46.5 | 10.50 | 32.6 | 7.93 | 34.7 | 8.25 | 0.00009 | 0.0006 | NS |
| SWS, % | 17.3 | 9.92 | 18.3 | 6.73 | 17.0 | 8.68 | NS | NS | NS |
| REM, % | 18.1 | 6.93 | 22.4 | 5.57 | 23.0 | 6.17 | NS | NS | NS |
TIB = Time in bed; SPT = sleep period time; TST = total sleep time; SOL = sleep onset latency; FRL = 1st REM latency; SE%= sleep efficiency; WASO = wakefulness after sleep onset; S1 = NREM sleep stage 1; S2 = NREM sleep stage 2; SWS = slow wave sleep; REM = rapid eye movement sleep.
Bonferroni corrected P values.
Visual Analysis of Submentalis EMG Amplitude
The comparison between the chin EMG amplitude visual analysis parameters obtained in the 3 groups of subjects is reported in Table 5. Both groups of patients with narcolepsy/cataplexy showed an increased percentage of REM sleep mini-epochs containing phasic EMG events (defined as any burst of EMG activity lasting 0.1–5 s, with an amplitude exceeding 4 times the background EMG activity).13 No significant difference was found between the 2 patient groups for this parameter or among all groups for the percentage of tonic REM sleep epochs.
Table 5.
Comparison Between Chin EMG Amplitude Visual Analysis Parameters Obtained in the 3 Groups of Subjects
| 1. Controls (n=35) |
2. Narcolepsy−RBD (n=17) |
3. Narcolepsy+RBD (n=17) |
Mann-Whitney U test* |
||||||
|---|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | 1 vs. 2 P< |
1 vs. 3 P< |
2 vs. 3 P< |
|
| Phasic REM mini-epochs, % | 1.5 | 0.96 | 6.5 | 2.79 | 8.0 | 3.51 | 0.000003 | 0.000003 | NS |
| Tonic REM epochs,% | 10.1 | 13.04 | 7.6 | 8.01 | 6.5 | 5.80 | NS | NS | NS |
Data expressed as a percentages of the total.
Bonferroni corrected P values.
Computer Quantitative Analysis of the Submentalis EMG Amplitude
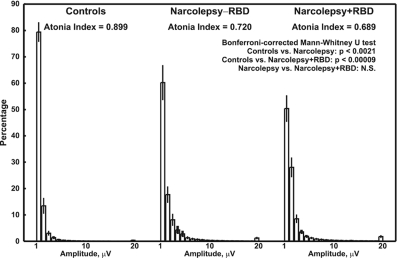
Figure 2 shows the normalized distribution histograms of mini-epoch amplitude for each subject group. Small but clear differences can be seen among the 3 groups. The graph pertaining to normal controls (on the left) was characterized by a very high and prominent first column indicating that approximately 80% of mini-epochs during this sleep stage have amp ≤ 1. The amplitude of the same column was lower in the Narcolepsy−RBD and lower still in the Narcolepsy+RBD group, with a shift of the respective graphs towards the other columns representing higher values of amp.
Figure 2.
Normalized distribution histograms of mini-epochs amplitude for each subject group. (The percentage of values in 20 amplitude (amp) classes are shown (1 = amp ≤ 1, 2 = 1 < amp ≤ 2, …, 19 = 18 < amp ≤ 19, 20 = amp > 19. All values are shown as means and standard errors (whiskers). The statistical analysis of the differences in REM sleep Atonia Index is also shown.
The REM sleep Atonia Index, which summarizes the distribution of these graphs, was significantly lower in both patient groups than controls. Again, no significant differences were found in REM sleep Atonia Index between the 2 groups of patients.
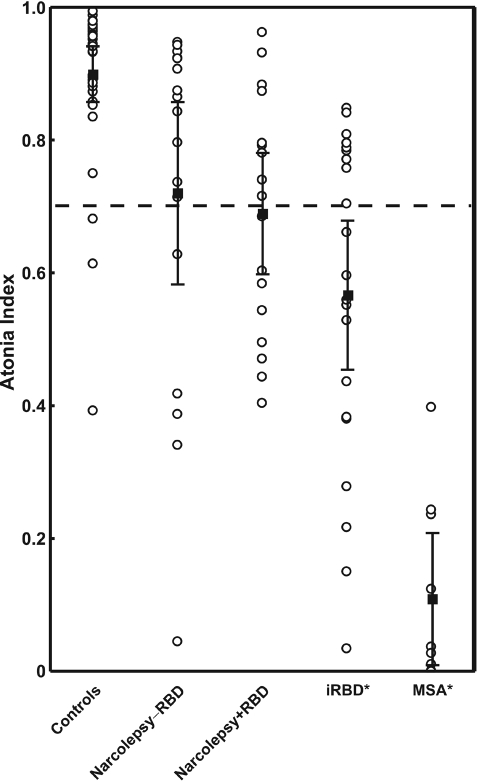
Figure 3 shows the individual values of the REM sleep Atonia Index in the different subject groups. Both patient groups showed a wide distribution of their individual values, largely overlapping with those of normal controls, but more often below the arbitrary threshold of 0.7 (Chi-square test = 10.006, P < 0.01), indicated with a dotted line in this figure and already indicated as a possible supporting criterion for the diagnosis of RBD.16 Also in this figure it is possible to note that REM sleep Atonia Index did not differ between the 2 groups of patients. Figure 2 also demonstrates data from a recent study in idiopathic and symptomatic RBD (multiple system atrophy), carried out by our group;16 this shows that both narcolepsy subgroups seem to show mean values of REM sleep Atonia Index between those of young normal controls and idiopathic RBD patients, with multiple system atrophy patients showing the lowest average value.
Figure 3.
REM sleep Atonia Index in the 3 groups of subjects in this study and in patients with idiopathic RBD (iRBD) and multiple system atrophy (MSA) (*data from Ferri et al.16): values are shown as means (black-filled squares) and 95% confidence intervals (whiskers). Individual values are also shown (circles).
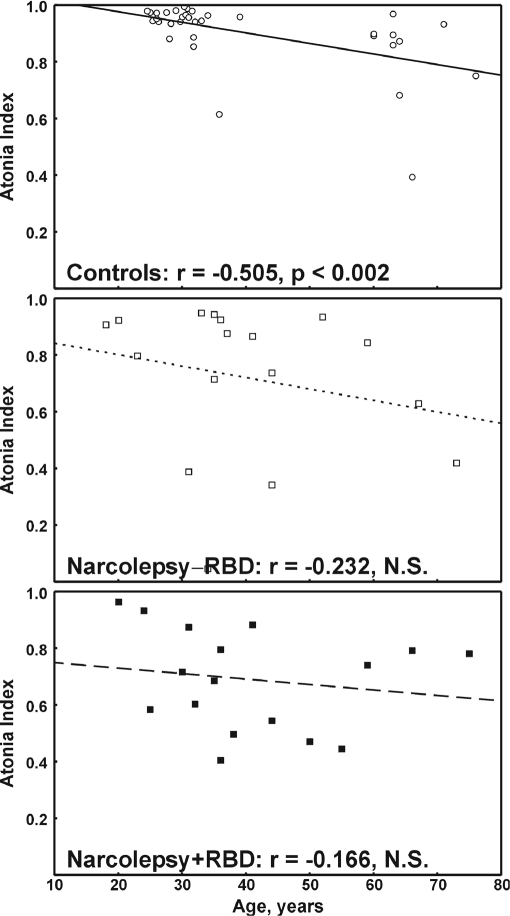
Figure 4 reports the relationship of REM sleep Atonia Index and age in the 3 groups of subjects. Even if this index tended to decrease with age in all graphs, the correlation coefficient reached statistical significance only for normal controls who showed individual values less scattered around the linear regression line than those of the patient groups. This result was confirmed also by the analysis reported in Table 6 in which 2 age subgroups (≤ 40 years and > 40 years) were obtained in each subject group; a statistically significant difference was found only in normal controls. The same table reports the comparison between gender subgroups in each subject group; none of these comparisons reached statistical significance.
Figure 4.
Correlation between REM sleep Atonia Index and age in normal controls (top graph), patients with narcolepsy−RBD (middle graph), and patients with narcolepsy+RBD (bottom graph). The Spearman correlation coefficient is also reported for each graph together with its statistical significance and the linear regression line.
Table 6.
Comparison Between REM Sleep Atonia Index Obtained in 2 Age Subgroups (≤40 Years and >40 Years), in Normal Controls, Patients with Narcolepsy–RBD, and Patients with Narcolepsy+RBD; Comparison Between Genders is also Reported in the Same Subject Groups
| Age ≤40 years |
Age >40 years |
Mann-Whitney U test* | |||||
|---|---|---|---|---|---|---|---|
| n | mean | SD | n | mean | SD | P < | |
| Controls | 24 | 0.937 | 0.077 | 10 | 0.815 | 0.170 | 0.006 |
| Narcolepsy−RBD | 10 | 0.747 | 0.300 | 7 | 0.681 | 0.229 | NS |
| Narcolepsy+RBD | 10 | 0.706 | 0.187 | 7 | 0.666 | 0.175 | NS |
| Males |
Females |
||||||
| n | mean | SD | n | mean | SD | P < | |
| Controls | 15 | 0.940 | 0.045 | 20 | 0.869 | 0.151 | NS |
| Narcolepsy−RBD | 9 | 0.710 | 0.221 | 8 | 0.731 | 0.327 | NS |
| Narcolepsy+RBD | 13 | 0.692 | 0.179 | 4 | 0.679 | 0.201 | NS |
Bonferroni corrected P values.
Figure 5 contains the normalized distribution histograms of consecutive mini-epoch sequences exceeding 2 μV for each subject group. These graphs show a similar type of distribution for all groups, with a tendency for patients with Narcolepsy−RBD and those with Narcolepsy+RBD to show higher values mostly for columns in the left part of the graphs (shorter activations). The same figure shows the differences in the total number of chin EMG activations detected in the 3 groups of subjects; this is significantly higher in both patient groups than controls. No significant differences were found in the total number of chin EMG activations between the 2 groups of patients.
Figure 5.
Normalized distribution histograms of consecutive mini-epoch sequences exceeding 2 μV for each subject group. The number per hour of sleep stage in 20 duration (dur) classes is shown (20 = dur>20 s). All values are shown as means and standard errors (whiskers). The statistical analysis of the differences in total number of movements per hour of REM sleep is also shown.
DISCUSSION
To our knowledge, this is the first computerized quantitative study of the EMG signal in narcolepsy, designed to evaluate polysomnographically signs of RBD in narcolepsy patients. RBD is prevalent in narcolepsy,4,6 but it has an even higher prevalence in narcolepsy-cataplexy.4,5 The percentage found in our narcolepsy/cataplexy patients fits with previous data. Interestingly, several findings suggest that narcoleptic patients without clinical RBD also frequently have increased electromyographic activity during REM sleep8 and have a higher prevalence of RWA, phasic EMG activity, and REM density than controls.10 Previous studies suggest that although it is frequent, RBD is not an every night phenomenon in narcolepsy/cataplexy4,5 and is more frequently disclosed by questionnaires or by clinical interview than by (video)polysomnography. This finding is peculiar, and differentiates narcolepsy/cataplexy from neurodegenerative diseases (i.e., multiple system atrophy) in which the typical RBD dream enacting is easily documented by videopolysomnography.21 In this light, the availability of a tool to detect subclinical signs of RBD on polysomnographic tracings might be of great interest not only for research but also for clinical decision making.
The recent availability of more quantitative and computerized methods of analysis of the EMG signal, especially designed for the evaluation of the chin motor phenomena accompanying RBD22,23 prompted us to apply this new approach to the study of RBD in narcolepsy/cataplexy.
The main finding of this study is the confirmation and quantification of polysomnographic signs of motor dyscontrol in the chin EMG of patients with narcolepsy/cataplexy. This allowed us to discover an abnormal quantity of motor activity in patients without a clear clinical complaint of RBD, as specified by the current diagnostic criteria.3 Although these signs were always more evident in subjects with clinically evident RBD, the difference from those without was not statistically significant. If we consider REM sleep Atonia Index ≤0.7 as a cut-off for RWA, 13 of our 34 (38%) narcolepsy/cataplexy patients had RWA, a figure similar to that found by others using visual scoring.10 As shown above, both narcolepsy subgroups seem to show mean values of REM sleep Atonia Index intermediate between those of young normal controls and idiopathic RBD patients, with multiple system atrophy patients showing the lowest average value; for this reason, the degree of motor dyscontrol expected in narcoleptic patients should be expected to be somewhat milder than that of idiopathic or symptomatic RBD. The increased index of motor dyscontrol in REM sleep in the 2 groups of patients with narcolepsy/cataplexy can thus be considered an intrinsic finding of the disease and a sort of “status dissociatus” (a condition characterized by ambiguous, multiple, or rapid oscillation of state-determining variables which can be observed in a wide variety of experimental and clinical situations),24,25 opening the way to acting out dream contents (i.e., RBD).
Another important finding of this study is that the altered REM sleep atonia index in all patients with narcolepsy/cataplexy was mostly caused by an increase in short-lasting EMG activity (approximately from 0 to 5 s), as shown in Figure 4. This phenomenon, already described by Geisler et al.,9 is also consistent with the increased limb phasic EMG activity in NREM sleep,26 and might differentiate patients with narcolepsy/cataplexy and RBD from patients with other forms of secondary RBD (i.e., multiple system atrophy), if confirmed by additional studies.
A third important finding is that the visual analysis of the same signal, following criteria established in the past,13 yielded results similar to those of the automatic analysis only for the count of short-duration (phasic) EMG activations, whereas analysis of the tonic REM epochs failed to disclose differences among our 3 groups of subjects. This is only partially in agreement with our previous study16 in idiopathic and symptomatic RBD and with the results reported in another study in a different group of symptomatic RBD patients using another quantitative method.22
The results of this study need to be compared with those obtained in idiopathic RBD patients.16 RBD in patients with narcolepsy differs from idiopathic RBD: patients with idiopathic RBD have a higher prevalence of RWA than narcolepsy subjects, with smaller REM density,10 and RBD in narcolepsy has a much earlier age at onset and a different sex ratio (in the idiopathic form, RBD mostly affects men).4,6 The present study clearly shows that the pattern of motor dyscontrol found in our narcoleptic subjects is less severe than that found in idiopathic RBD and also different from that of symptomatic RBD in patients with multiple system atrophy. MSA patients present a very high number of RWA epochs compared to idiopathic RBD. Thus, this new quantitative approach seems to be not only able to disclose differences between normal controls and patients, but also among nosologically different groups of patients who might present a different type of REM sleep motor dyscontrol (which is currently referred to as RBD in all cases). These differences might indicate different neurochemical and neurophysiological mechanisms underlying an apparently similar sleep disturbance, from a strictly clinical point of view, occurring in different conditions such as narcolepsy, idiopathic RBD, and MSA.21,27 Besides these conditions, RBD has been reported to occur in neurological diseases such as Parkinson disease,28,29 spinocerebellar ataxia,30 supranuclear palsy,31 Lewy body disease,28 Alzheimer disease,32 amyotrophic lateral sclerosis,33 multiple sclerosis,34,35 and Tourette syndrome.36 Lastly, RBD can be induced by medications, especially the tricyclic antidepressants and serotonin-specific reuptake inhibitors.33,37 For this reason, the new quantitative approach proposed in the present study may also yield insights into the specific patterns of chin EMG activation during REM sleep in these disorders.
This study also provided further evidence of a significant effect of age on our REM sleep Atonia Index in normal controls, an effect which was mild and statistically nonsignificant in both groups of patients. This seems to indicate that the age of subjects is a critical factor to take into account in these studies, and that there is a significant interaction between disease and age, with the pathological condition masking the effects of age.
In conclusion, a certain degree of polysomnographically evident RBD is present in many patients with narcolepsy/cataplexy. This disorder might be specific and correlated to the specific neurochemical and neuropathological substrate of narcolepsy/cataplexy. Our approach represents an improvement over previous visual methods of analysis of chin EMG during REM sleep and yields useful and practical indices for the quantitative and nonsubjective evaluation of EMG atonia during REM sleep, and EMG activations. The combination of atonia and activation indices allows investigation of different clinical conditions characterized by abnormal chin EMG activation during sleep. Our proposed REM sleep Atonia Index is an additional useful parameter to be used in conjunction with the other criteria for the diagnosis of RBD. Future research is now needed to verify this new method in evaluating the clinical effects of drugs for RBD treatment.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9:293–308. doi: 10.1093/sleep/9.2.293. [DOI] [PubMed] [Google Scholar]
- 2.de Barros-Ferreira M, Lairy GC. Ambiguous sleep in narcolepsy. In: Guilleminault C, Dement WC, Passouant P, editors. Narcolepsy; Proceedings of the First international symposium on narcolepsy; July 1975; Montpellier, France. New York: Spectrum publications; 1976. pp. 57–75. [Google Scholar]
- 3.American Academy of Sleep Medicine. Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. International Classification of Sleep Disorders. [Google Scholar]
- 4.Nightingale S, Orgill JC, Ebrahim IO, de Lacy SF, Agrawal S, Williams AJ. The association between narcolepsy and REM behavior disorder (RBD) Sleep Med. 2005;6:253–8. doi: 10.1016/j.sleep.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Mattarozzi K, Bellucci C, Campi C, et al. Clinical, behavioural and polysomnographic correlates of cataplexy in patients with narcolepsy/cataplexy. Sleep Med. 2008 doi: 10.1016/j.sleep.2007.05.006. in press. [DOI] [PubMed] [Google Scholar]
- 6.Schenck CH, Mahowald MW. Motor dyscontrol in narcolepsy: rapid-eye-movement (REM) sleep without atonia and REM sleep behavior disorder. Ann Neurol. 1992;32:3–10. doi: 10.1002/ana.410320103. [DOI] [PubMed] [Google Scholar]
- 7.Nevsimalova S, Prihodova I, Kemlink D, Lin L, Mignot E. REM behavior disorder (RBD) can be one of the first symptoms of childhood narcolepsy. Sleep Med. 2007;8:784–6. doi: 10.1016/j.sleep.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 8.Mayer G, Meier-Ewert K. Motor dyscontrol in sleep of narcoleptic patients (a lifelong development?) J Sleep Res. 1993;2:143–8. doi: 10.1111/j.1365-2869.1993.tb00078.x. [DOI] [PubMed] [Google Scholar]
- 9.Geisler P, Meier-Ewert K, Matsubayshi K. Rapid eye movements, muscle twitches and sawtooth waves in the sleep of narcoleptic patients and controls. Electroencephalogr Clin Neurophysiol. 1987;67:499–507. doi: 10.1016/0013-4694(87)90051-4. [DOI] [PubMed] [Google Scholar]
- 10.Dauvilliers Y, Rompre S, Gagnon JF, Vendette M, Petit D, Montplaisir J. REM sleep characteristics in narcolepsy and REM sleep behavior disorder. Sleep. 2007;30:844–9. doi: 10.1093/sleep/30.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walters AS, Lavigne G, Hening W, et al. The scoring of movements in sleep. J Clin Sleep Med. 2007;3:155–67. [PubMed] [Google Scholar]
- 12.Brunner DP, Dijk DJ, Borbely AA. A quantitative analysis of phasic and tonic submental EMG activity in human sleep. Physiol Behav. 1990;48:741–8. doi: 10.1016/0031-9384(90)90219-t. [DOI] [PubMed] [Google Scholar]
- 13.Lapierre O, Montplaisir J. Polysomnographic features of REM sleep behavior disorder: development of a scoring method. Neurology. 1992;42:1371–4. doi: 10.1212/wnl.42.7.1371. [DOI] [PubMed] [Google Scholar]
- 14.Consens FB, Chervin RD, Koeppe RA, et al. Validation of a polysomnographic score for REM sleep behavior disorder. Sleep. 2005;28:993–7. doi: 10.1093/sleep/28.8.993. [DOI] [PubMed] [Google Scholar]
- 15.Bliwise DL, He L, Ansari FP, Rye DB. Quantification of electromyographic activity during sleep: a phasic electromyographic metric. J Clin Neurophysiol. 2006;23:59–67. doi: 10.1097/01.wnp.0000192303.14946.fc. [DOI] [PubMed] [Google Scholar]
- 16.Ferri R, Manconi M, Plazzi G, et al. A quantitative statistical analysis of the submentalis muscle EMG amplitude during sleep in normal controls and patients with REM sleep behavior disorder. J Sleep Res. 2008;17 doi: 10.1111/j.1365-2869.2008.00631.x. in press. [DOI] [PubMed] [Google Scholar]
- 17.Bologna Genova Parma and Pisa Universities group for the study of REM Sleep Behaviour Disorder (RBD) in Parkinson's Disease. Interobserver reliability of ICSD-R criteria for REM sleep behaviour disorder. J Sleep Res. 2003;12:255–7. doi: 10.1046/j.1365-2869.2003.00359.x. [DOI] [PubMed] [Google Scholar]
- 18.Scaglione C, Vignatelli L, Plazzi G, et al. REM sleep behaviour disorder in Parkinson's disease: a questionnaire-based study. Neurol Sci. 2005;25:316–21. doi: 10.1007/s10072-004-0364-7. [DOI] [PubMed] [Google Scholar]
- 19.Kemp B, Varri A, Rosa AC, Nielsen KD, Gade J. A simple format for exchange of digitized polygraphic recordings. Electroencephalogr Clin Neurophysiol. 1992;82:391–3. doi: 10.1016/0013-4694(92)90009-7. [DOI] [PubMed] [Google Scholar]
- 20.Rechtschaffen A, Kales A, editors. A manual of standardized terminology, techniques, and scoring system for sleep stages of human subjects. Washington, DC: US Government Printing Office; 1968. [Google Scholar]
- 21.Plazzi G, Corsini R, Provini F, et al. REM sleep behavior disorders in multiple system atrophy. Neurology. 1997;48:1094–7. doi: 10.1212/wnl.48.4.1094. [DOI] [PubMed] [Google Scholar]
- 22.Burns JW, Consens FB, Little RJ, Angell KJ, Gilman S, Chervin RD. EMG variance during polysomnography as an assessment for REM sleep behavior disorder. Sleep. 2007;30:1771–8. doi: 10.1093/sleep/30.12.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayer G, Penzel T, Kesper K, Leonhardt E. New findings on the pathogenesis and pathophysiology of REM sleep behaviour disorder (RBD) J Sleep Res. 2006;15(Suppl 1):29. [Google Scholar]
- 24.Mahowald MW, Schenck CH. Evolving concepts of human state dissociation. Arch Ital Biol. 2001;139:269–300. [PubMed] [Google Scholar]
- 25.Mahowald MW, Schenck CH. Status dissociatus--a perspective on states of being. Sleep. 1991;14:69–79. doi: 10.1093/sleep/14.1.69. [DOI] [PubMed] [Google Scholar]
- 26.Ferri R, Zucconi M, Manconi M, et al. Different periodicity and time structure of leg movements during sleep in narcolepsy/cataplexy and restless legs syndrome. Sleep. 2006;29:1587–94. doi: 10.1093/sleep/29.12.1587. [DOI] [PubMed] [Google Scholar]
- 27.Vetrugno R, Provini F, Cortelli P, et al. Sleep disorders in multiple system atrophy: a correlative video-polysomnographic study. Sleep Med. 2004;5:21–30. doi: 10.1016/j.sleep.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Boeve BF, Silber MH, Ferman TJ. REM sleep behavior disorder in Parkinson's disease and dementia with Lewy bodies. J Geriatr Psychiatry Neurol. 2004;17:146–57. doi: 10.1177/0891988704267465. [DOI] [PubMed] [Google Scholar]
- 29.Onofrj M, Thomas A, D'Andreamatteo G, et al. Incidence of RBD and hallucination in patients affected by Parkinson's disease: 8-year follow-up. Neurol Sci. 2002;23(Suppl 2):S91–S94. doi: 10.1007/s100720200085. [DOI] [PubMed] [Google Scholar]
- 30.Friedman JH. Presumed rapid eye movement behavior disorder in Machado-Joseph disease (spinocerebellar ataxia type 3) Mov Disord. 2002;17:1350–3. doi: 10.1002/mds.10269. [DOI] [PubMed] [Google Scholar]
- 31.Arnulf I, Merino-Andreu M, Bloch F, et al. REM sleep behavior disorder and REM sleep without atonia in patients with progressive supranuclear palsy. Sleep. 2005;28:349–54. [PubMed] [Google Scholar]
- 32.Gagnon JF, Petit D, Fantini ML, et al. REM sleep behavior disorder and REM sleep without atonia in probable Alzheimer disease. Sleep. 2006;29:1321–5. doi: 10.1093/sleep/29.10.1321. [DOI] [PubMed] [Google Scholar]
- 33.Thomas A, Bonanni L, Onofrj M. Symptomatic REM sleep behaviour disorder. Neurol Sci. 2007;28(Suppl 1):S21–S36. doi: 10.1007/s10072-007-0735-y. [DOI] [PubMed] [Google Scholar]
- 34.Plazzi G, Montagna P. Remitting REM sleep behavior disorder as the initial sign of multiple sclerosis. Sleep Med. 2002;3:437–9. doi: 10.1016/s1389-9457(02)00042-4. [DOI] [PubMed] [Google Scholar]
- 35.Tippmann-Peikert M, Boeve BF, Keegan BM. REM sleep behavior disorder initiated by acute brainstem multiple sclerosis. Neurology. 2006;66:1277–9. doi: 10.1212/01.wnl.0000208518.72660.ff. [DOI] [PubMed] [Google Scholar]
- 36.Trajanovic NN, Voloh I, Shapiro CM, Sandor P. REM sleep behaviour disorder in a child with Tourette's syndrome. Can J Neurol Sci. 2004;31:572–5. doi: 10.1017/s031716710000384x. [DOI] [PubMed] [Google Scholar]
- 37.Mahowald MW, Schenck CH, Bornemann MA. Pathophysiologic mechanisms in REM sleep behavior disorder. Curr Neurol Neurosci Rep. 2007;7:167–72. doi: 10.1007/s11910-007-0013-7. [DOI] [PubMed] [Google Scholar]