Abstract
The present study examined associations among dimensions of suicidality and psychopathology in a sample of 428 homeless adolescents (56.3% female). Confirmatory factor analysis results provided support for a three-factor model in which suicidality (measured with lifetime suicidal ideation and suicide attempts), internalizing disorders (assessed with lifetime diagnoses of major depressive episode and post-traumatic stress disorder), and externalizing disorders (indicated by lifetime diagnoses of conduct disorder, alcohol abuse, and drug abuse) were positively intercorrelated. The findings illustrate the utility of a dimensional approach that integrates suicidality and psychopathology into one model.
Keywords: Psychopathology, Suicidality, Internalizing, Externalizing, Homeless adolescents
Dimensions of adolescent suicidality and psychopathology are of increased concern to clinicians and researchers (Bridge et al. 2006; Verona et al. 2004). This interest can be attributed to the relatively high prevalence of adolescent suicidal ideation and suicide attempts (Evans et al. 2005) and to suicide being the third leading cause of death among youths ages 15-24 in the USA (Hoyert et al. 2006). Research also indicates both suicidal ideation and suicide attempts increase the risk for completed suicide (Brown et al. 2000). This pattern of increased liability for suicide risk has led to a broader conceptualization of a suicide spectrum ranging from suicidal ideation to attempted and completed suicide (Lewinsohn et al. 1996).
Moreover, psychiatric disorders are among the strongest correlates of adolescent suicidality (Bridge et al. 2006). Mood disorders are robust correlates, but post-traumatic stress disorder, conduct disorder, and substance use disorders are also associated with suicidality (Bridge et al. 2006; Evans et al. 2004). Krueger (1999), informed by the work of Achenbach (Achenbach and McConaughy 1997), developed a dimensional model of psychopathology and clustered psychiatric diagnoses into internalizing and externalizing disorders. As specific psychiatric disorders from both clusters are related to suicidal ideation and attempts, there is interest in linking the suicide spectrum to these broader dimensions of psychopathology (Hills et al. 2005; Verona et al. 2004).
Our study expands on this work by including the internalizing and externalizing dimensions of psychopathology in a structural model of adolescent suicidality using a sample of homeless adolescents. Suicidality is measured with lifetime suicidal ideation and suicide attempts, internalizing psychopathology with lifetime diagnoses of major depressive episode and post-traumatic stress disorder, and externalizing psychopathology with lifetime diagnoses of conduct disorder, alcohol abuse, and drug abuse. We use confirmatory factor analysis to examine covariances among dimensions of suicidality, internalizing, and externalizing disorders.
Internalizing and Externalizing Disorders
Achenbach used an empirical approach to derive two broad dimensions (internalizing and externalizing) of child and adolescent problem behaviors (Achenbach and McConaughy 1997). The syndromes of the internalizing dimension (e.g., depression, anxiety, somatic complaints) are characterized by inner distress and those of the externalizing dimension (e.g., aggression, delinquent behaviors) are characterized by conflicts with others or society (Achenbach and McConaughy 1997). Krueger (1999) extended Achenbach's conceptualization in his analyses of data from a large epidemiologic sample of individuals aged 15 to 64 years old.
Krueger (1999) used confirmatory factor analysis to explicitly model comorbidity among psychiatric disorders that were indicators for each of the latent dimensions of internalizing and externalizing. In this model, within-dimension comorbidity is indicated by substantial covariance shared by the syndromes within each common underlying latent dimension and is modeled by the factor loadings for each manifest disorder on its respective latent dimension. For example, there is substantial covariance both within internalizing and within externalizing syndromes. Between-dimension comorbidity is suggested by the more modest covariance between the two latent dimensions of internalizing and externalizing. Similar findings have been replicated by analyses of data from other large samples (Krueger and Markon 2006; Lahey et al. 2004). Confirmatory factor analysis is appropriate to study adolescent psychopathology as pure psychiatric disorders are rare and clusters of disorders often co-occur at rates greater than chance (Angold et al. 1999).
Suicidality
Researchers increasingly advocate a suicide dimension that varies along a continuum of increased intention to die from ideation to attempts and completed suicide (Lewinsohn et al. 1996; Van Heeringen 2001). Given the low base rate and methodological difficulties associated with studying completed suicide, researchers have focused attention on the more common suicidal ideation and attempts, which might aid in preventive efforts (Lewinsohn et al. 1996). Indeed, suicidal ideation increases the likelihood of a suicide attempt (Bridge et al. 2006), and past suicide attempts are predictors of completed suicide (Brown et al. 2000).
Suicidal ideation and attempts occur in a range of psychiatric disorders, although few individuals diagnosed with any psychiatric disorder attempt or commit suicide (Lewinsohn et al. 1996). Consequently, it has been argued that psychopathology is a necessary, but not sufficient, condition for suicidal behavior (Apter and Ofek 2001). It has also been suggested that suicidal behavior is itself a valid clinical syndrome that co-occurs with other forms of psychopathology (Ahrens and Linden 1996; Leboyer et al. 2005). Moreover, family genetic studies that suggest that suicidality is transmitted independent of psychopathology (Brent and Mann 2005; Turecki 2001).
Specific Psychiatric Disorders and Suicidality
A consistent finding is the relationship between a diagnosis of major depression and suicidality in community samples of adolescents (Bridge et al. 2006; Evans et al. 2004; Lewinsohn et al. 1996). A diagnosis of post-traumatic stress disorder has also been related to suicidality in samples of adolescents (e.g., Brezo et al. 2006; Giaconia et al. 1995). It is also established that conduct and substance use disorders have a relationship with suicidality in community samples of adolescents (Bridge et al. 2006; Evans et al. 2004; Lewinsohn et al. 1996).
Internalizing and Externalizing Disorder Categories and Suicidality
Moreover, studies of adolescents (Breton et al. 2002; Esposito and Clum 2003) and adults (Hills et al. 2005; Verona et al. 2004) have examined the relationship between suicidality and broadly-defined internalizing and externalizing disorders. Three studies reported a significant relationship between suicidality and both disorder categories (Breton et al. 2002; Hills et al. 2005; Verona et al. 2004), and one study reported a significant relationship between suicidality and the internalizing disorder category only (Esposito and Clum 2003).
Contributions of the Present Study
Our study makes a contribution by using a sample of homeless adolescents. This is an appropriate sample as research has shown that both suicidality and psychological disorders are more common among homeless adolescents than among community-dwelling youths (Kamieniecki 2001; Whitbeck et al. 2004a). For homeless adolescents, lifetime suicide attempt rates have ranged from 18% (Yates et al. 1988) to 53% (Smart and Ogborne 1994), and lifetime suicidal ideation rates have been as high as 28% (Booth and Zhang 1996) to 62% (Unger et al. 1997). Also, the lifetime rate of one (or more) psychiatric disorders ranges from 78% (Sleegers et al. 1998) to 90% (Feitel et al. 1992).
Our review also suggests where research on suicidality and internalizing and externalizing disorders can be improved. No previous studies on suicidality and that defines internalizing and externalizing disorders broadly have used confirmatory factor analysis (CFA; Breton et al. 2002; Esposito and Clum 2003; Hills et al. 2005; Verona et al. 2004). Yet, this method of analysis provides both general and specific advantages over other techniques such as exploratory factor analysis (EFA) that will improve on previous research. General advantages of CFA over EFA are that this approach is: (a) appropriate for testing a priori hypothesized models, and (b) a more parsimonious method of modeling of comorbidity and core psychopathological processes (Brown 2006; Fabrigar et al. 1999; Krueger 1999).
Specific advantages of CFA for examining suicidality and dimensions of psychopathology are that it is possible to: (a) account for between- and within-category comorbidity and (b) incorporate multiple aspects of suicidality. As previous studies did not use CFA, the focus was largely on observed diagnoses. Without the use of CFA it was simply not possible to model these as latent internalizing or externalizing dimensions across their respective forms of psychopathology. Moreover, the use of CFA is consistent with current conceptualizations of suicide both as separate from, but related to, the dimensions of internalizing and externalizing (e.g., Lewinsohn et al. 1996; Van Heeringen 2001). Our study is also one of the few that uses both suicidal ideation and suicide attempts as indicators of suicidality. Three of the previous cited studies focused only on one aspect of suicidality - suicidal ideation (Esposito and Clum 2003) or suicide attempts (Hills et al. 2005; Verona et al. 2004).
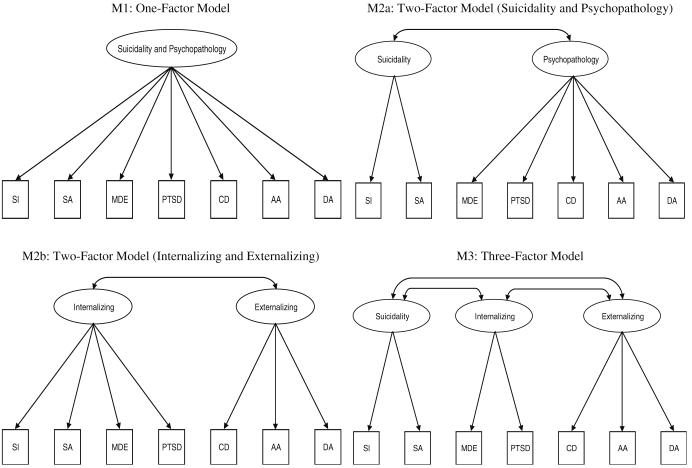
Four CFA models will be tested in this study (see Fig. 1). The one-factor model (M1) indicates that the suicidality items [lifetime measures of suicidal ideation (SI) and suicide attempts (SA)] and all psychopathology indicators [lifetime diagnoses of major depressive episode (MDE), post-traumatic stress disorder (PTSD), conduct disorder (CD), alcohol abuse (AA), and drug abuse (DA)] will load on one latent factor. M1 is useful for comparative purposes but does not have empirical support (e.g., Turecki 2001). The first two-factor model (M2a) posits that the indicators for suicidality (SI and SA) load on one latent factor, that the indicators for psychopathology (MDE, PTSD, CD, AA, and DA) load on another latent factor, and that the latent factors are correlated. M2a has merit as there is evidence for comorbidity among psychiatric disorders (e.g., Angold et al. 1999). The second two-factor model (M2b) suggests that the indicators for suicidality and internalizing (SI, SA, MDE, and PTSD) load on one latent factor, and it is related to an externalizing latent factor comprised of three indicators (CD, AA, and DA). M2b is plausible because it has been argued that internalizing disorders are a necessary component of suicidality (e.g., Isacsson 2006). We predict that the three-factor model (M3) will be the best fit to the data, as this has been supported by previous research (Breton et al. 2002; Esposito and Clum 2003). M3 has separate sets of indicators for suicidality (SI and SA), internalizing (MDE and PTSD), and externalizing (CD, AA, and DA) that comprise three related latent factors.
Fig. 1.
Alternative confirmatory factor analysis models (SI suicidal ideation, SA suicide attempt, MDE major depressive episode, PTSD post-traumatic stress disorder, CD conduct disorder, AA alcohol abuse, and DA drug abuse)
Method
Participants
Interviewers
The data come from the baseline sample of 444 participants in the Midwest Longitudinal Study of Homeless Adolescents (MLSHA). Full-time interviewers were placed in outreach agencies in eight Midwestern cities (Des Moines, Cedar Rapids, and Iowa City, Iowa; Lincoln and Omaha, Nebraska; St. Louis and Kansas City, Missouri; and Wichita, Kansas). The interviewers held at least a Bachelor's degree, had social service experience, had previously worked with homeless youths, and were already familiar with the local street culture. The interviewers underwent one week of intensive training for procedures regarding computer-assisted personal interviewing and psychiatric diagnostic interviewing. They then returned to their outreach agencies and completed several practice interviews with staff members and other respondents ages 20 years or older. After administering the practice interviews, the interviewers returned to the university for a second week of training.
Eligibility and Protocol
The interviewers approached potential participants whom they believed would meet eligibility criteria for the study. In particular, youths were eligible to participate if they were ages 16 to 19 and homeless. Consistent with federal guidelines and previous research (Haber and Toro 2004; Whitbeck and Hoyt 1999), youth homelessness was assessed in terms of housing situation and/or absence of a legal guardian. More specifically, homelessness was defined as living in a shelter, on the street, or on their own (with friends or in a transitional living situation) as a result of being pushed out by—or running away from—their families of origin. Similar to the strategy employed by Kipke et al. (1998), potential interviewees were recruited in shelters and in other areas where homeless adolescents congregated (e.g., outreach and drop-in centers, parks, homeless camps). In order to maximize diversity in terms of service use and duration of homelessness, locations were checked repeatedly at various times of the day and days of the week over the course of one year.
Of those who met eligibility criteria, about 90% agreed to participate. Participants were informed that the study was longitudinal, and the interviewers explained the tracking protocols. The adolescents were assured that refusing to participate, refusing to answer individual questions, or stopping the interview at any time would have no effect on current or future service provision by outreach agencies. The baseline interview was conducted in two parts that were administered within two days of each other. The first part contained the bulk of the survey, and the second part consisted of psychiatric diagnostic interviews. Participants were interviewed in shelter interview rooms, outreach vans, quiet corners of restaurants, apartments, or outside. The youths were paid $25 at the completion of each part of the interview. All interviews were conducted on laptop computers, and the data were downloaded electronically to a special secure university server.
Consent
The project was approved by the Institutional Review Board (IRB) at the University of Nebraska-Lincoln (#2001-07-333 FB), and a National Institute of Mental Health Certificate of Confidentiality was obtained to protect the participants if they made statements about potentially illegal activities. Adolescents signed a statement of informed consent, and as mandated by the IRB, they were asked if the interviewers could contact their parents. When parents were contacted, they were asked to provide verbal consent to interview the adolescents, which was granted in every case. The parents were also asked to participate in a telephone interview. Requiring parental consent did not affect recruitment and retention of participants.
Moreover, the interviewers did not disclose specific information about the adolescents to the parents. If the parents requested details about the adolescent's location or well-being, the interviewers stated that they had spoken to the adolescent, indicated that the adolescent was all right, and offered to relay the parent's inquiry to the adolescent. Among adolescents living in shelters, the interviewers followed shelter policies of parental permission for placement and guidelines for granting such permissions. These policies were based on state laws. In the few cases where adolescents were under 18 years old, not in a shelter, and refused permission to contact their parents, the adolescents were treated as emancipated minors according to National Institutes of Health guidelines (U.S. Department of Health and Human Services 2001).
Measures
Suicidality
Two measures were used to assess suicidality. First, suicidal ideation (SI) consisted of eight items (Cronbach's α=0.91) described in Yoder et al. (2007). Adolescents rated (on a scale of 0=none of the time, 1=some of the time, and 2=all of the time) their lifetime thoughts about being dead or committing suicide. Sample questions (all with the stem “in your whole life, how often have you”) include: (1) wished that our life would end? (2) thought about killing yourself? (3) had plans to kill yourself? The items were coded and averaged so that higher values of the scale indicated more suicidal ideation. Second, suicide attempt (SA) consisted of responses to the question “during your whole life, how many times have you tried to kill yourself?” A negative reciprocal root transformation (Newton and Rudestam 1999) was used to reduce skewness (from 3.35 to 0.99) and kurtosis (from 12.11 to −0.56) in the suicide attempt variable.
Lifetime Psychiatric Diagnoses
Five lifetime psychiatric diagnoses (each coded as 0=absent, 1=present) were measured. Conduct Disorder (CD) was assessed using the Diagnostic Interview Schedule for Children-Revised (DISC-R; Shaffer et al. 1993), and Major Depressive Episode (excluding the death- and suicide-related criteria; MDE), Post-Traumatic Stress Disorder (PTSD), Alcohol Abuse (AA), and Drug Abuse (DA) were assessed using the University of Michigan version of the Composite International Diagnostic Interview (UM-CIDI; Wittchen and Kessler 1994). The DISC-R and UM-CIDI were based on criteria in the revised third edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association 1987), and both were intended for use by interviewers without clinical training. Researchers have reported good to excellent interrater and test-retest reliability and satisfactory validity on the DISC-R (Piacentini et al. 1993; Schwab-Stone et al. 1993; Shaffer et al. 1993) and on the CIDI, from which the UM-CIDI was derived (Wittchen 1994). In this study, practice interviews were checked for accuracy, but statistical measures of reliability were not calculated.
Analytic Strategy
The analyses were conducted in two steps. First, a correlation matrix was calculated using PRELIS 2 (Jöreskog and Sörbom 2002). Three types of correlations were estimated: Pearson (between suicidal ideation and suicide attempt), tetrachoric (among the dichotomous psychiatric diagnoses), and biserial (between the diagnoses and suicide-related variables). Tetrachoric and biserial correlations are computed assuming that normally-distributed variables underlie each of the psychiatric diagnosis variables (Jöreskog and Sörbom 2002). Second, confirmatory factor analysis models were estimated using the Weighted Least Squares (WLS) procedure in LISREL 8.71 (Jöreskog and Sörbom 2001). WLS is appropriate for models that contain dichotomous variables, and it can accommodate a mixture of Pearson, tetrachoric, and biserial correlations (Jöreskog and Sörbom 2001, 2002).
One-, two-, and three-factor models (see Fig. 1) were estimated, and the χ2 statistic and descriptive goodness-of-fit indices were used to select the best-fitting model. Criteria for a good-fitting model include a χ2 statistic p value>0.05; RMSEA<0.06; SRMR<0.08; MOC>0.90; and GFI*, NNFI, IFI, and CFI>0.95. Criteria for selecting between two good-fitting nested models include a significant difference between the model χ2 statistics (p<0.05); smaller RMSEA, AIC, and SRMR; and larger MOC, GFI*, NNFI, IFI, and CFI (Marsh et al. 2005). The two-factor models (M2a and M2b) are not nested; however, they can be compared using the AIC (Brown 2006) and both can be compared to the one- and three-factor models.
Results
Missing Cases
Sixteen participants (3.6% of the total) did not complete the psychiatric diagnostic portion of the interview, and they were excluded from the analyses. The remaining 428 respondents were used in the analyses, and of these youths, 427 had complete information on all of the study variables. One participant did not answer one of the suicidal ideation questions, and mean value substitution was used to impute a value for the missing item. When compared to those who were included in the analyses, excluded adolescents were older, on average, when they first ran away from home (Ms of 14.8 and 13.4 years, t(19)=3.23, p=0.004, Hedge's g=0.46). The included and excluded youths did not differ on other sociodemographic variables or on the suicidality measures.
Sample Characteristics
Among the 428 participants included in the analyses, 241 (56.3%) were female. Over half (58.4%) self-identified as white (non-Hispanic), 21.5% as African-American, 4.4% as Hispanic, 3.3% as American Indian, 0.7% as Asian or Pacific Islander, and 11.0% as bi- or multi-racial. The youths ranged in age from 16 to 19 years (M=17.3), and they ran away from home for the first time when they were an average of 13.4 years old (range=2 to 18 years). When asked where they had stayed the night before the interview, 40.2% stated a shelter or mission, 16.8% the home of a friend or acquaintance, 16.1% a foster or group home, 11.7% the home of a relative, 6.3% their own apartment (paying rent), 2.6% on the street or under a bridge, 1.4% in an abandoned house or squat, and 4.9% other.
Descriptive Statistics and Bivariate Correlations
Table 1 presents descriptive statistics and bivariate correlations for the study variables. The mean value for the suicidal ideation scale falls between “none” and “some of the time” (M=0.61, SD=0.48). Descriptive statistics for the transformed suicide attempt variable are difficult to interpret (M=−0.81, SD=0.26), but based on the untransformed version, adolescents made an average of nearly 2 lifetime suicide attempts (M=1.98, SD=4.46). Many of these youths met lifetime criteria for the five psychiatric diagnoses: major depressive episode (30.4%), PTSD (36.0%), conduct disorder (75.7%), alcohol abuse (43.7%), and drug abuse (40.4%). Finally, the correlations provide preliminary evidence for the three-factor model because the within-construct correlations are moderate to large (ranging from 0.45 to 0.68) and are higher than the between-construct correlations (ranging from 0.14 to 0.38).
Table 1.
Descriptive statistics and Pearson, tetrachoric, and biserial correlations for the study variables (N=428)
| M or % | (SD) | SI | SA | MDE | PTSD | CD | AA | DA | |
|---|---|---|---|---|---|---|---|---|---|
| SI Suicidal ideation, SA suicide attempt, MDE major depressive episode, PTSD post-traumatic stress disorder, CD conduct disorder, AA alcohol abuse, DA drug abuse | |||||||||
| SI | 0.61 | (0.48) | 1.00 | ||||||
| SA | −0.81a | (0.26) | 0.68 | 1.00 | |||||
| MDE | 30.4% | 0.35 | 0.28 | 1.00 | |||||
| PTSD | 36.0% | 0.38 | 0.31 | 0.45 | 1.00 | ||||
| CD | 75.7% | 0.21 | 0.21 | 0.14 | 0.15 | 1.00 | |||
| AA | 43.7% | 0.23 | 0.21 | 0.20 | 0.18 | 0.58 | 1.00 | ||
| DA | 40.4% | 0.19 | 0.20 | 0.14 | 0.22 | 0.46 | 0.58 | 1.00 | |
Based on transformed count of suicide attempts. For the untransformed variable, M=1.98 (SD=4.46).
Confirmatory Factor Analysis Models
Tables 2 and 3 present the goodness-of-fit indices for the null model of independent variables and the one-, two-, and three-factor models. The three-factor model provides the best fit to the data as indicated by superior fit index values [χ2(11)=5.41; p=0.91; RMSEA=0.00; SRMR=0.02; MOC=1.01; and GFI*, NNFI, IFI, and CFI=1], the smallest AIC value (39.41), and significantly better fit than both two-factor models (M2a: Δχ2(2)=49.93, p<0.001; M2b: Δχ2(2)=21.24, p<0.001).
Table 2.
Goodness-of-fit indices for confirmatory factor analysis models (N=428)
| Models | Chi-square statistics | RMSEA and 90% confidence interval | Absolute fit indices | Incremental fit indices | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p value | RMSEA | Lower | Upper | AIC | SRMR | MOC | GFI* | NNFI | IFI | CFI | |
| Analyses based on Weighted Least Squares estimation with tetrachoric, biserial, and Pearson correlations. | |||||||||||||
| M0: null | 10,667.52 | 21 | 0.00 | 1.09 | 1.07 | 1.11 | 10,691.52 | 0.30 | 0.00 | 0.12 | 0.00 | 0.00 | 0.00 |
| M1: one-factor | 156.87 | 14 | 0.00 | 0.15 | 0.13 | 0.18 | 184.87 | 0.15 | 0.85 | 0.91 | 0.98 | 0.99 | 0.99 |
| M2a: two-factor | 55.34 | 13 | 0.00 | 0.09 | 0.06 | 0.11 | 85.34 | 0.12 | 0.95 | 0.97 | 0.99 | 1.00 | 1.00 |
| (suicidality and psychopathology) | |||||||||||||
| M2b: two-factor | 26.65 | 13 | 0.01 | 0.05 | 0.02 | 0.08 | 56.65 | 0.06 | 0.98 | 0.99 | 1.00 | 1.00 | 1.00 |
| (internalizing and externalizing) | |||||||||||||
| M3: three-factor | 5.41 | 11 | 0.91 | 0.00 | 0.00 | 0.02 | 39.41 | 0.02 | 1.01 | 1.00 | 1.00 | 1.00 | 1.00 |
Table 3.
Comparison of models
| Model comparisons | Chi-square statistics | ||
|---|---|---|---|
| Δχ2 | Δdf | p value | |
| M0 vs. M1 | 10,520.65 | 7 | 0.00 |
| M1 vs. M2a | 101.53 | 1 | 0.00 |
| M1 vs. M2b | 130.22 | 1 | 0.00 |
| M2a vs. M3 | 49.93 | 2 | 0.00 |
| M2b vs. M3 | 21.24 | 2 | 0.00 |
Table 4 presents the results for the three-factor model. The unstandardized factor loadings and factor correlations are all positive and statistically significant, and the standardized factor loadings indicate a good factor structure (values range from 0.66 to 0.88). The suicidality and internalizing factors are highly correlated (0.61), but the correlation is not large enough to suggest that both factors are measuring one concept. The correlations of externalizing with both suicidality and internalizing (0.35 and 0.37) provide evidence for comorbidity among the latent dimensions.
Table 4.
Three-factor confirmatory factor analysis results (N=428)
| Unstandardized solution | (Standard error) | Standardized solution | |
|---|---|---|---|
| Analyses based on Weighted Least Squares estimation with tetrachoric, biserial, and Pearson correlations. | |||
| SI Suicidal ideation, SA suicide attempt, MDE major depressive episode, PTSD post-traumatic stress disorder, CD conduct disorder, AA alcohol abuse, DA drug abuse, NT not tested (unstandardized factor loading was set equal to 1 for identification) | |||
| Factor loadings | |||
| Suicidality | |||
| SI | 1.00NT | - | 0.88 |
| SA | 0.88* | (0.06) | 0.78 |
| Internalizing | |||
| MDE | 1.00NT | - | 0.66 |
| PTSD | 1.07* | (0.14) | 0.70 |
| Externalizing | |||
| CD | 1.00NT | - | 0.72 |
| AA | 1.15* | (0.13) | 0.83 |
| DA | 0.96* | (0.11) | 0.69 |
| Factor correlations | |||
| Suicidality and internalizing | 0.35* | (0.04) | 0.61 |
| Suicidality and externalizing | 0.22* | (0.03) | 0.35 |
| Internalizing and externalizing | 0.17* | (0.05) | 0.37 |
Statistically significant at p<0.001 (two-tailed test).
Discussion
Summary
This study examined associations among dimensions of suicidality and psychopathology in a sample of 428 homeless adolescents. Confirmatory factor analysis results provided support for a three-factor model in which suicidality (measured with lifetime suicidal ideation and suicide attempts), internalizing disorders (assessed with lifetime diagnoses of major depressive episode and post-traumatic stress disorder), and externalizing disorders (indicated by lifetime diagnoses of conduct disorder, alcohol abuse, and drug abuse) were positively intercorrelated. These results are consistent with previous research that examined suicidality and broadly-defined internalizing and externalizing disorders (Breton et al. 2002; Hills et al. 2005; Verona et al. 2004). That the suicidal ideation and suicide attempt variables loaded on one factor also supports current conceptualizations of a suicide spectrum (e.g., Lewinsohn et al. 1996; Van Heeringen 2001). In addition, the correlation between the suicidality and internalizing factors was relatively large (0.61), but it was not large enough to suggest that both factors are measuring the same concept. This finding is consistent with the perspective that suicidal behavior is itself a valid clinical syndrome that cooccurs with other forms of psychopathology (Ahrens and Linden 1996; Leboyer et al. 2005).
Furthermore, the strong factor loadings for the internalizing and externalizing factors provide evidence for substantial within-dimension comorbidity, and the more modest correlation between the internalizing and externalizing factors provides evidence for between-dimension comorbidity. These findings are consistent with those of Krueger (1999), and they agree with research conducted on other adolescent and adult samples (Krueger and Markon 2006; Lahey et al. 2004). Also, the magnitude of the factor loadings for major depressive episode and post-traumatic stress disorder is consistent with the findings of Cox et al. (2002) and Slade and Watson (2006), who extended Krueger's dimensional model to include PTSD as part of the internalizing factor. In sum, the results of this study illustrate the utility of modeling suicidality based on Krueger's (1999) approach and integrating psychopathology and suicidality into one model (Hills et al. 2005; Verona et al. 2004).
Weaknesses
Some weaknesses of our study should be acknowledged. First, we used lifetime reports of suicidality and psychopathology, and the results might be affected by recall biases (Angold et al. 1999; Foley et al. 2006). Also, lifetime reports of suicidality and psychiatric diagnoses, when compared to current or past-year measures, yield higher prevalence rates for individual and comorbid problems (Angold et al. 1999; Foley et al. 2006), which might strengthen the correlations (cf. Bonett and Price 2005). Second, the correlations could be further inflated due to the high-risk nature of the sample (cf. Shahar et al. 2006) and single-reporter biases (e.g., Bank et al. 1990). Third, the results may not generalize to other adolescent populations or to other homeless youths. Although participants were selected from several Midwestern cities, research suggests that characteristics of homeless youths differ by region of the country (Thompson et al. 2003).
Fourth, the data are from a non-probability convenience sample, and statistically speaking, a probability sample is preferable. However, the population of interest is highly unstable and not very well defined (Whitbeck and Hoyt 1999), which makes it impossible to create a sampling frame and to determine a probability of selection. Fifth, due to concerns about participant fatigue and time constraints, the number of psychiatric diagnoses was limited to those that were expected to be most prevalent (Whitbeck et al. 2004b). Consequently, this study could not exactly replicate Krueger's (1999) dimensional model. Finally, the nature of the latent dimensions is not well specified. Fergusson et al. (2006) suggest three possible interpretations for these latent dimensions (individual predisposition, genetic and environmental influences, and underlying continuum of severity), and they note that empirical evidence does not support any one interpretation.
Conclusion
While the results should be interpreted with appropriate caution, they have practical implications for people working with homeless adolescents. The dimensional approach and its emphasis on core psychopathological processes (Krueger 1999) indicates that screening and treatment should be broad-based rather than narrowly focused. Youths should be screened across the spectrum of suicidality (from thoughts of death and suicide to plans and attempted suicide) and both internalizing and externalizing problems. Although conduct disorder and substance abuse are relatively common among homeless adolescents (e.g., Whitbeck et al. 2004a), these externalizing problems should not be overlooked because they might be indicators of suicidality. These young people should be offered appropriate therapeutic interventions that are comprehensive and draw on their strengths (Karabanow and Clement 2004).
The limitations of this study indicate potential directions for future research using a dimensional approach to understanding the relationship between suicidality and psychopathology. First, additional research is needed in psychiatric and general adolescent and adult populations. Second, lifetime measures cannot distinguish concurrent from successive comorbidity (Angold et al. 1999) and the relative timing of suicidality versus psychopathology (Foley et al. 2006), which limits the practical implications that can be drawn from the results. Consequently, future studies should use prospective data or current measures of suicidality and psychopathology. Finally, studies should include a broader array of psychiatric disorders such as dysthymia, generalized anxiety disorder, social phobia, agoraphobia, specific phobia, panic disorder, and obsessive-compulsive disorder (Krueger 1999; Krueger and Markon 2006; Slade and Watson 2006). The inclusion of more psychiatric disorders will better illuminate the relationships among dimensions of suicidality and internalizing and externalizing disorders.
Acknowledgments
Thank you to the editor and anonymous reviewers for comments and help on earlier drafts of this paper. The Midwest Longitudinal Study of Homeless Adolescents was supported by the National Institute of Mental Health (MH57110), Les B. Whitbeck, principal investigator.
Footnotes
Kevin A. Yoder and Susan L. Longley made equal contributions to this paper.
References
- Achenbach TM, McConaughy SH. Empirically based assessment of child and adolescent psychopathology: Practical applications. 2nd ed. Sage; Thousand Oaks, CA: 1997. [Google Scholar]
- Ahrens B, Linden M. Is there a suicidality syndrome independent of specific major psychiatric disorder? Results of a split half multiple regression analysis. Acta Psychiatrica Scandinavica. 1996;94:79–86. doi: 10.1111/j.1600-0447.1996.tb09829.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed., revised American Psychiatric Association; Washington, DC: 1987. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Apter A, Ofek H. Personality constellations and suicidal behaviour. In: Van Heeringen K, editor. Understanding suicidal behaviour: The suicidal process approach to research, treatment, and prevention. Wiley; Chichester, England: 2001. pp. 94–119. [Google Scholar]
- Bank L, Dishion T, Skinner M, Patterson GR. Method variance in structural equation modeling: Living with “glop”. In: Patterson GR, editor. Depression and aggression in family interaction. Lawrence Erlbaum; Hillsdale, NJ: 1990. pp. 247–279. [Google Scholar]
- Bonett DG, Price RM. Inferential methods for the tetrachoric correlation coefficient. Journal of Educational and Behavioral Statistics. 2005;30:213–225. [Google Scholar]
- Booth RE, Zhang Y. Severe aggression and related conduct problems among runaway and homeless adolescents. Psychiatric Services. 1996;47:75–80. doi: 10.1176/ps.47.1.75. [DOI] [PubMed] [Google Scholar]
- Brent DA, Mann JJ. Family genetic studies, suicide, and suicidal behavior. American Journal of Medical Genetics Part C. 2005;133:13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- Breton J-J, Tousignant M, Bergeron L, Berthiaume C. Informant-specific correlates of suicidal behavior in a community survey of 12- to 14-year-olds. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:723–730. doi: 10.1097/00004583-200206000-00012. [DOI] [PubMed] [Google Scholar]
- Brezo J, Paris J, Tremblay R, Vitaro F, Zoccolillo M, Hérbert M, et al. Personality traits as correlates of suicide attempts and suicidal ideation in young adults. Psychological Medicine. 2006;36:191–202. doi: 10.1017/S0033291705006719. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford; New York: 2006. [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Esposito CL, Clum GA. The relative contribution of diagnostic and psychosocial factors in the prediction of adolescent suicidal ideation. Journal of Clinical Child and Adolescent Psychology. 2003;32:386–395. doi: 10.1207/S15374424JCCP3203_07. [DOI] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: A systematic review of population-based studies. Clinical Psychology Review. 2004;24:957–979. doi: 10.1016/j.cpr.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K, Deeks J. The prevalence of suicidal phenomena in adolescents: A systematic review of population-based studies. Suicide and Life-Threatening Behavior. 2005;35:239–250. doi: 10.1521/suli.2005.35.3.239. [DOI] [PubMed] [Google Scholar]
- Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4:272–299. [Google Scholar]
- Feitel B, Margetson N, Chamas J, Lipman C. Psychosocial background and behavioral and emotional disorders of homeless and runaway youth. Hospital and Community Psychiatry. 1992;43:155–159. doi: 10.1176/ps.43.2.155. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM. Structure of internalising symptoms in early adulthood. British Journal of Psychiatry. 2006;189:540–546. doi: 10.1192/bjp.bp.106.022384. [DOI] [PubMed] [Google Scholar]
- Foley DL, Goldston DB, Costello EJ, Angold A. Proximal psychiatric risk factors for suicidality in youth. Archives of General Psychiatry. 2006;63:1017–1024. doi: 10.1001/archpsyc.63.9.1017. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- Haber MG, Toro PA. Homelessness among families, children, and adolescents: An ecological-developmental perspective. Clinical Child and Family Psychology Review. 2004;7:123–164. doi: 10.1023/b:ccfp.0000045124.09503.f1. [DOI] [PubMed] [Google Scholar]
- Hills AL, Cox BJ, McWilliams LA, Sareen J. Suicide attempts and externalizing psychopathology in a nationally representative sample. Comprehensive Psychiatry. 2005;46:334–339. doi: 10.1016/j.comppsych.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Hoyert DL, Heron MP, Murphy SL, Kung H-C. Deaths: Final data for 2003. National Vital Statistics Report, 54. National Center for Health Statistics; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- Isacsson G. Depression is the core of suicidality—its treatment is the cure. Acta Psychiatrica Scandinavica. 2006;114:149–150. doi: 10.1111/j.1600-0447.2006.00871.x. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User's reference guide. Scientific Software International; Lincolnwood, IL: 2001. [Google Scholar]
- Jöreskog KG, Sörbom D. PRELIS 2: User's reference guide. Scientific Software International; Lincolnwood, IL: 2002. [Google Scholar]
- Kamieniecki GW. Prevalence of psychological distress and psychiatric disorders among homeless youth in Australia: A comparative review. Australian and New Zealand Journal of Psychiatry. 2001;35:352–358. doi: 10.1046/j.1440-1614.2001.00910.x. [DOI] [PubMed] [Google Scholar]
- Karabanow J, Clement P. Interventions with street youth: A commentary on the practice-based research literature. Brief Treatment and Crisis Intervention. 2004;4:93–108. [Google Scholar]
- Kipke MD, O'Connor S, Nelson B, Anderson JE. A probability sampling for assessing the effectiveness of outreach for street youth. In: Greenberg JB, Neumann MS, editors. What we have learned from the AIDS evaluation of street outreach projects: A summary document. Centers for Disease Control and Prevention; Atlanta, GA: 1998. pp. 17–28. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psycho-pathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Leboyer M, Slama F, Siever L, Bellivier F. Suicidal disorders: A nosological entity per se? American Journal of Medical Genetics Part C. 2005;133:3–7. doi: 10.1002/ajmg.c.30040. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: Prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3:25–46. [Google Scholar]
- Marsh HW, Hau K-T, Grayson D. Goodness of fit in structural equation models. In: Maydeu-Olivares A, McArdle JJ, editors. Contemporary psychometrics: A festschrift for Roderick P. McDonald. Lawrence Erlbaum; Mahwah, NJ: 2005. pp. 275–340. [Google Scholar]
- Newton RR, Rudestam KE. Your statistical consultant: Answers to your data analysis questions. Sage; Thousand Oaks, CA: 1999. [Google Scholar]
- Piacentini J, Shaffer D, Fisher P, Schwab-Stone M, Davies M, Gioia P. The diagnostic interview schedule for children—Revised version (DISC-R): III. Concurrent criterion validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:658–665. doi: 10.1097/00004583-199305000-00025. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone M, Fisher P, Piacentini J, Shaffer D, Davies M, Briggs M. The diagnostic interview schedule for children—Revised version (DISC-R): II. Test-retest reliability. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:651–657. doi: 10.1097/00004583-199305000-00024. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Schwab-Stone M, Fisher P, Cohen P, Piacentini J, Davies M, et al. The diagnostic interview schedule for children—Revised version (DISC-R): I. Preparation, field testing, interrater reliability, and acceptability. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:643–650. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- Shahar G, Bareket L, Rudd MD, Joiner TE. In severely suicidal young adults, hopelessness, depressive symptoms, and suicidal ideation constitute a single syndrome. Psychological Medicine. 2006;36:913–922. doi: 10.1017/S0033291706007586. [DOI] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Sleegers J, Spijker J, van Limbeek J, van Engeland H. Mental health problems among homeless adolescents. Acta Psychiatrica Scandinavica. 1998;97:253–259. doi: 10.1111/j.1600-0447.1998.tb09996.x. [DOI] [PubMed] [Google Scholar]
- Smart RG, Ogborne AC. Street youth in substance abuse treatment: Characteristics and treatment compliance. Adolescence. 1994;29:733–745. [PubMed] [Google Scholar]
- Thompson SJ, Maguin E, Pollio DE. National and regional differences among runaway youth using federally-funded crisis services. Journal of Social Science Research. 2003;30:1–17. [Google Scholar]
- Turecki G. Suicidal behavior: Is there a genetic predisposition? Bipolar Disorders. 2001;3:335–349. doi: 10.1034/j.1399-5618.2001.30608.x. [DOI] [PubMed] [Google Scholar]
- Unger JB, Kipke MD, Simon TR, Montgomery SB, Johnson CJ. Homeless youths and young adults in Los Angeles: Prevalence of mental health problems and the relationship between mental health and substance abuse disorders. American Journal of Community Psychology. 1997;25:371–394. doi: 10.1023/a:1024680727864. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Code of Federal Regulations (45 CFR § 46 et seq.) National Institutes of Health, Office of Protection from Research Risks; 2001. Protection of human subjects. [Google Scholar]
- Van Heeringen K. The suicidal process and related concepts. In: Van Heeringen K, editor. Understanding suicidal behaviour: The suicidal process approach to research, treatment, and prevention. Wiley; Chichester, England: 2001. pp. 3–14. [Google Scholar]
- Verona E, Sachs-Ericsson N, Joiner TE. Suicide attempts associated with externalizing psychopathology in an epidemiological sample. American Journal of Psychiatry. 2004;161:444–451. doi: 10.1176/appi.ajp.161.3.444. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Hoyt DR. Nowhere to grow: Homeless and runaway adolescents and their families. Aldine de Gruyter; New York: 1999. [Google Scholar]
- Whitbeck LB, Johnson KD, Hoyt DR, Cauce AM. Mental disorder and comorbidity among runaway and homeless adolescents. Journal of Adolescent Health. 2004a;35:132–140. doi: 10.1016/j.jadohealth.2003.08.011. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Johnson KD, Hoyt DR, Cauce AM. The missing psychotic disorders: Response. Journal of Adolescent Health. 2004b;35:433. [Google Scholar]
- Wittchen H-U. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Kessler RC. Modifications of the CIDI in the National Comorbidity Survey: The development of the UMCIDI (NCS Working Paper #2) Institute for Social Research, The University of Michigan; Ann Arbor: 1994. [Google Scholar]
- Yates GL, MacKenzie R, Pennbridge J, Cohen E. A risk profile comparison of runaway and non-runaway youth. American Journal of Public Health. 1988;78:820–821. doi: 10.2105/ajph.78.7.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder KA, Whitbeck LB, Hoyt DR. Social Indicators Research. 2007. Dimensionality of thoughts of death and suicide: Evidence from a study of homeless adolescents. (in press) DOI 10.1007/s11205-007-9095-5. [Google Scholar]