Abstract
Coronary artery disease (CAD) is common and multi-factorial. Members of the Church of Jesus Christ of Latter-day Saints (LDS, or Mormons) in Utah may have lower cardiac mortality than other Utahns and the US population. While the LDS proscription of smoking likely contributes to lower cardiac risk, it is unknown whether other shared behaviors also contribute. This study evaluated potential CAD-associated effects of fasting. Patients (N1=4,629) enrolled in the Intermountain Heart Collaborative Study registry (1994-2002) were evaluated for association of religious preference with CAD diagnosis (≥70% coronary stenosis on angiography) or no CAD (normal coronaries, <10% stenosis). Consequently, another set of patients (N2=448) were surveyed (2004-2006) for association of behavioral factors with CAD, with the primary variable being routine fasting (i.e., abstinence from food and drink). Secondary survey measures included proscription of alcohol, tea, and coffee, social support, and religious worship patterns. In population 1 (initial), 61% of LDS and 66% of all others had CAD (adjusted [including for smoking]: odds ratio [OR]=0.81; p=0.009). In population 2 (survey), fasting was associated with lower risk of CAD (64% vs. 76% CAD; OR=0.55, CI=0.35, 0.87; p=0.010) and this remained after adjustment for traditional risk factors (OR=0.46, CI=0.27, 0.81; p=0.007). Fasting was also associated with lower diabetes prevalence (p=0.048). In regression models entering other secondary behavioral measures, fasting remained significant with similar effect size. In conclusion, not only proscription of tobacco, but also routine periodic fasting was associated with lower risk of CAD.
Keywords: fasting, coronary artery disease, smoking, behavioral factors
INTRODUCTION
Utah routinely has among the lowest rates of coronary artery disease (CAD) death in the US.(1) Reports from the 1970’s suggest that members of the Church of Jesus Christ of Latter-day Saints (LDS, or Mormons) in Utah have lower cardiac mortality than other Utahns (2) and the general US population.(3) This may be due to the LDS proscription of smoking, but it is unknown whether other behaviors are partially responsible for the lower risk. Additional protective lifestyle behaviors in that population may include routine periodic fasting, proscription of coffee, tea, or alcohol, frequent attendance of worship services, and receiving support from a social network. While some of these factors have been studied,(4-7) routine fasting has not. Fasting one day per month is taught among the LDS population from early youth and its practice often begins as early as the age of 8 years.(8) Given the potential cardiovascular and anti-aging benefits of caloric restriction,(9-12) and the direct effect of fasting on dietary intake over an extended period of time, it was hypothesized that routine periodic fasting could have a beneficial effect on processes such as glucose metabolism.(11,13,14) The objective of this study was to evaluate potential CAD-associated effects of fasting and of other behaviors beyond smoking abstinence.
METHODS
The cardiac catheterization registry of the Intermountain Heart Collaborative Study includes patients from hospitals within Utah-based Intermountain Healthcare. CAD presence was determined from a review of angiograms by the attending cardiologist and was recorded in a database based on the Coronary Artery Surgery Study protocol.(15,16) Patients had no CAD (all coronary arteries free of disease or <10% stenosis), moderate CAD (most severe lesion 10%-69% stenosis), or significant CAD (≥1 lesion of ≥70% stenosis). This study primarily compared the more discordant diagnoses of significant CAD and no CAD, excluding moderate CAD as indeterminate. This study was approved by Intermountain Healthcare’s Urban Central Region Institutional Review Board.
Demographic and health histories were obtained from physicians and hospital records, including age and sex. Smoking was considered present for active smokers or those with a >10 pack-year history. Body mass index (BMI: weight [kg] ÷ height2 [m2]) was computed from measured anthropometrics. History of diabetes, hyperlipidemia, and hypertension were physician-reported from clinical or laboratory findings and current medication use. For laboratory findings, diabetes was defined as a blood sugar ≥126 mg/dL; hypertension as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg; hyperlipidemia as total cholesterol ≥200 mg/dL or low-density lipoprotein cholesterol ≥130 mg/dL. Family history of early CAD was considered positive if a first-order relative suffered cardiovascular death, MI, or coronary revascularization before the age of 65 years for females or 55 years for males.
Between 1993 and 2002, all patients presenting for coronary angiography were asked their religious preference via a free-text query: “Do you have a religious/spiritual preference? If yes, please list.” A cohort of N1=4,629 patients (27% of total) responded and differences in CAD based on religious preference were evaluated by the Chi-square test. Multivariable logistic regression was used to determine covariable-adjusted odds ratios (OR) and 95% confidence intervals (CI). Regressions initially used a conditional stepwise approach and final models utilized forced variable entry, with covariables including age, sex, hypertension, hyperlipidemia, BMI, diabetes, smoking, and family history. Analyses were performed with SPSS (version 15.0) and two-tailed p values≤0.05 were nominally significant.
Consequently, a second population was studied to determine which lifestyle behaviors may contribute to the risk difference observed in population 1. From 2004-2006, a survey was administered to all patients prior to angiography to assess adherence to behaviors that may account for health outcome differences (N2=448). From a review of the potentially-shared behaviors among those of the LDS faith, the primary hypothesis was developed that routine fasting may be associated with a lower risk of CAD since obesity, diabetes, and metabolic syndrome are strong risk factors for CAD,(11,17) fasting directly influences caloric intake, and the other potentially-shared behaviors were unlikely candidates for reducing the risk of CAD. To assess fasting behavior, patients were asked, “Do you routinely abstain from food and drink (i.e., fast) for extended periods of time.”
Beyond smoking, other potentially shared behaviors of LDS patients (see Supplemental Table 1) included levels of social support,(7) proscription of tea, coffee, and alcohol,(18) weekly observance of a day of rest,(19) and attendance of worship services.(19) Questions for alcohol, tea, coffee, and social support incorporated components of questions from the National Health and Nutrition Examination Survey. The survey was validated by serial administration to 20 individuals at 0, 3, and 30 days, with follow-up interviews. For alcohol, primary modeling compared any use vs. none, while further evaluation examined 1-7 drinks/week and >7 drinks/week vs. none for beer and for liquor, and wine was evaluated as any vs. none (almost no patients reported >7 drinks/week). For religious worship and observing a day of rest, frequency of once a month or more was classified as adherence and compared to non-adherence.
Although not available for all patients, physical activity-related caloric expenditure (kilocalories per week) was calculated based on survey data collected via the Paffenbarger physical activity questionnaire and divided into quintiles for modeling purposes.(20) Socioeconomic measures of income and educational attainment were also surveyed (see Supplemental Table 2), although only about two-thirds of patients (n=306) completed the income question. Education was categorized into five groups based on attainment of high school graduation or less, some college or vocational school experience, college graduation, some graduate school or a masters degree, or a doctoral degree. Income was categorized into three groups post hoc based on levels of CAD risk: low income (<$30,000), intermediate ($30,000-$69,999), and high income (≥$70,000).
Associations with CAD for fasting and other behaviors were tested using the Chi-square test or Fisher’s Exact Test and each metric was subsequently evaluated by multivariable logistic regression. Regression models adjusted for age, sex, smoking, diabetes, hyperlipidemia, hypertension, BMI, and family history of early CAD. Because diabetics may be instructed not to fast due to their medical condition, subanalyses of fasting were performed for diabetic and non-diabetic strata. Stratified analyses were also performed by religious preference and smoking, and by the other cardiac risk factors. Effect modification on fasting by each other variable was tested using a regression interaction y = β0 + β1*X1 + β2*X2 + β3*(X1*X2), where y is CAD status, βi is the i regression coefficient, X1 is reported fasting status, and X2 is one of the covariables. For the secondary behavioral measures, additional models were evaluated entering fasting as a covariable to assess confounding.
RESULTS
Baseline characteristics are shown in Table 1 for population 1 (N=4,629) and Table 2 for population 2 (survey population, N=448). In population 1, 61% of LDS preference patients and 66% of others had CAD (OR=0.81, CI= 0.70, 0.93; p=0.002) and this was significant after adjustment (OR=0.81, CI=0.69, 0.95; p=0.009). A similar effect size was found in population 2 (univariable: OR=0.80, CI=0.50, 1.28; p=0.35; multivariable: OR=0.78, CI=0.45, 1.35; p=0.37), although sample size was much smaller.
Table 1.
Baseline characteristics for the initial population 1 and for strata defined by religious preference. Statistical comparisons are of each factor by religious preference
| Characteristic | Overall (N = 4,629) | LDS Preference (n = 3,162) | Other Religious Preference (n = 1,467) | p-value |
|---|---|---|---|---|
| Age (years) | 63.6±13.0 | 64.5±12.8 | 61.5±13.2 | <0.001 |
| Men | 64% | 63% | 65% | 0.09 |
| Diabetes Mellitus | 18% | 19% | 17% | 0.07 |
| Hypertension | 51% | 52% | 50% | 0.23 |
| Body Mass Index (kg/m2) | 28.3±5.8 | 28.5±5.9 | 27.9±5.6 | 0.002 |
| Hyperlipidemia* | 43% | 41% | 46% | 0.008 |
| Family History of Early Coronary Disease† | 29% | 29% | 29% | 0.97 |
| Smoker | 18% | 12% | 31% | <0.0001 |
Total cholesterol≥200 mg/dL, low-density lipoprotein cholesterol≥130 mg/dL, or current medication use;
First-order relative suffered cardiovascular death, myocardial infarction, or coronary revascularization before the age of 65 years for females or 55 years for males.
Table 2.
Baseline characteristics in the second (survey) population 2. For physical activity and annual income, sample size was lower due to missing data
| Characteristic | Overall (N=448) | Fasting (n=122) | Non-fasting (n=326) | p-value | LDS Preference (n=297) | Other Religious Preferences (n=151) | p-value |
|---|---|---|---|---|---|---|---|
| Age (years) | 63.8±11.9 | 62.8±11.1 | 64.2±12.1 | 0.28 | 64.2±12.1 | 62.7±11.5 | 0.23 |
| Men | 69% | 68% | 69% | 0.97 | 66% | 73% | 0.15 |
| Diabetes Mellitus | 18% | 12% | 20% | 0.048 | 20% | 13% | 0.07 |
| Hypertension | 58% | 53% | 60% | 0.17 | 57% | 59% | 0.69 |
| Body Mass Index (kg/m2) | 28.7±6.0 | 28.1±5.4 | 28.9±6.3 | 0.27 | 28.9±6.2 | 28.1±5.7 | 0.25 |
| Hyperlipidemia* | 57% | 62% | 56% | 0.25 | 58% | 57% | 0.87 |
| Family History of Early Coronary Disease† | 39% | 42% | 38% | 0.45 | 39% | 39% | 0.98 |
| Smoker | 13% | 3% | 17% | <0.001 | 7% | 24% | <0.001 |
| LDS Preference | 66% | 92% | 57% | <0.001 | ----- | ----- | ----- |
| Physical Activity (caloric expenditure: kCal/week, N=330) | |||||||
| Quintile 1 | 20% | 8% | 25% | 21% | 16% | ||
| Quintile 2 | 19% | 20% | 18% | 20% | 17% | ||
| Quintile 3 | 22% | 18% | 25% | 21% | 25% | ||
| Quintile 4 | 19% | 27% | 15% | 20% | 16% | ||
| Quintile 5 | 20% | 26% | 18% | 0.001 | 18% | 26% | 0.26 |
| Annual Income (N=306) | |||||||
| <$30,000 | 30% | 21% | 33% | 32% | 25% | ||
| $30K-$69,999 | 46% | 50% | 45% | 47% | 45% | ||
| ≥$70,000 | 24% | 29% | 22% | 0.13 | 21% | 30% | 0.23 |
| Education | |||||||
| ≤12 years | 29% | 21% | 32% | 28% | 29% | ||
| Some college | 32% | 32% | 32% | 31% | 35% | ||
| College graduate | 17% | 12% | 20% | 16% | 20% | ||
| Masters degree/Some graduate school | 13% | 22% | 9% | 15% | 8% | ||
| Doctoral degree | 9% | 13% | 7% | <0.001 | 9% | 8% | 0.29 |
Total cholesterol≥200 mg/dL, low-density lipoprotein cholesterol≥130 mg/dL, or current medication use
First-order relative suffered cardiovascular death, myocardial infarction, or coronary revascularization before the age of 65 years for females or 55 years for males.
In population 2, fasting was associated (Figure 1) with lower risk of CAD (64% vs. 76% CAD for fasting vs. non-fasting, respectively; OR=0.55, CI=0.35, 0.87; p=0.010), and this effect remained after multivariable adjustment for age, sex, BMI, hypertension, hyperlipidemia, diabetes, smoking, and family history (OR=0.46, CI=0.27, 0.81; p=0.007). Among the 74% of patients with data on physical activity, fasting results were similar in univariable analysis (OR=0.55, CI=0.32, 0.93; p=0.025) and when adjusting for physical activity and the other cardiac risk factors listed above (OR=0.50, CI=0.26, 0.95; p=0.035). For the 68% with income and education data (n=306), effect size was similar but power was reduced (fasting: OR=0.59, p=0.06), but adjustment for income and education did not alter the effect size of fasting (OR=0.57, p=0.11). Adjusting for fasting and cardiac risk factors, physical activity (OR=0.78 per quintile, p=0.043) and income (vs. <$30,000/year; $30,000-$69,999: OR=0.43, p=0.046; ≥$70,000; OR=0.31, p=0.016), but not education (OR=1.03 per category, p=0.082) were associated with CAD.
Figure 1.
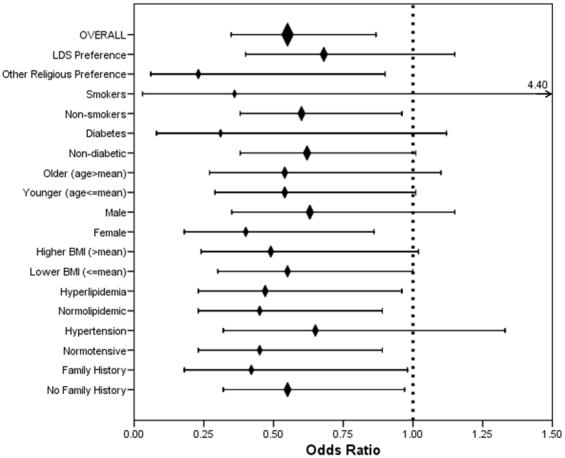
Univariable association of fasting with CAD, both overall and in subgroups. No effect modification was found for any covariable on the association of fasting with CAD (all p-interaction>0.15).
Most secondary behaviors differed by fasting status (Table 3), but only religious worship was associated with CAD although some other trends were present (Table 4). Evaluation of alcohol use (any vs. none) showed a trend toward increased CAD risk (Table 4), and evaluation by type and quantity showed a similar outcome for wine (any vs. none: OR=1.70, CI=0.91, 3.19; p=0.10), beer (1-7 drinks/week vs. none: OR=1.20, CI=0.60, 2.40; p=0.60; >7 drinks/week vs. none: OR=1.56, CI=0.43, 5.64; p=0.50), and liquor (1-7 drinks/week vs. none: OR=1.81, CI=0.85, 3.87; p=0.12; >7 drinks/week vs. none: OR=4.08, CI=0.52, 32.26; p=0.18). In analyses of fasting and the secondary behaviors, though, only fasting was significant in each model (Table 4) and in multivariable analysis (data not shown).
Table 3.
Comparison of secondary behavioral measures to fasting status
| Characteristic | Overall | Fasting | Non-fasting | p-value |
|---|---|---|---|---|
| LDS-proscribed Beverages | ||||
| Alcohol | 28% | 6% | 35% | <0.001 |
| Tea | 31% | 13% | 38% | <0.001 |
| Coffee | 37% | 10% | 47% | <0.001 |
| Religious Observance | ||||
| Religious Worship | 76% | 97% | 68% | <0.001 |
| Day of Rest | 81% | 93% | 77% | <0.001 |
| Receipt of Social Support | ||||
| Talk about Health | 98% | 97% | 98% | 0.55 |
| Talk about Personal Problems | 95% | 94% | 95% | 0.58 |
| Financial Support | 53% | 56% | 52% | 0.54 |
Table 4.
Association of fasting and secondary behavioral measures with coronary artery disease. Models entering fasting with each measure demonstrated that none of the secondary measures was significant, while fasting retained significance at p<0.05 in all models
| Univariable | Modeled with Fasting | |||
|---|---|---|---|---|
| Characteristic | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Fasting | 0.55 (0.35, 0.87) | 0.010 | ----- | ----- |
| LDS-proscribed Beverages | ||||
| Alcohol | 1.63 (0.98, 2.72) | 0.06 | 1.40 (0.82, 2.39) | 0.22 |
| Tea | 1.44 (0.87, 2.38) | 0.15 | 1.23 (0.73, 2.08) | 0.43 |
| Coffee | 1.42 (0.88, 2.28) | 0.15 | 1.14 (0.68, 1.90) | 0.62 |
| Religious Observance | ||||
| Religious Worship | 0.54 (0.31, 0.93) | 0.027 | 0.63 (0.35, 1.13) | 0.12 |
| Day of Rest | 0.92 (0.51, 1.65) | 0.78 | 1.05 (0.58, 1.93) | 0.87 |
| Receipt of Social Support | ||||
| Talk about Health | 0.90 (0.18, 4.53) | 0.90 | 0.84 (0.16, 4.29) | 0.83 |
| Talk about Personal Problems | 1.40 (0.55, 3.56) | 0.48 | 1.36 (0.53, 3.50) | 0.53 |
| Financial Support | 0.87 (0.55, 1.39) | 0.56 | 0.88 (0.55, 1.41) | 0.60 |
In exploratory subgroup analyses (Figure 1), a >30% lower risk of CAD was found in all subgroups although not all achieved significance. Formal interaction tests found no covariable modified fasting’s effect (all p-interaction>0.15). Notably, the effect of fasting on CAD was present among patients of religious preferences other than LDS (44% vs. 78% CAD; OR=0.23, CI=0.06, 0.90; p=0.037).
Finally, an exploratory evaluation was performed with inclusion of n=67 patients with moderate CAD who had been excluded as indeterminate from all other analyses, bringing the population 2 sample size to N=515. Diabetes prevalence was lower (11% vs. 20% for fasting vs. non-fasting, respectively, p=0.019) and trends to lower BMI (27.9±5.3 vs. 29.1±6.2, p=0.051) and less hypertension (52% vs. 61%, p=0.07) were found. A step-wise trend in CAD (p-trend=0.038) was found with 34%, 26%, and 24% fasting reported among patients with no CAD, moderate CAD, and significant CAD, respectively.
DISCUSSION
The Utah population consistently has one of the lowest rates of death due to cardiovascular disease,(1) and this low-risk status has been linked to the lifestyle of people with an LDS religious preference.(2,3) The most likely source of such risk differences is the proscription of tobacco smoking since smoking is a well-described risk factor for CAD development and conveys a substantial increase in risk,(1,17) but it is improbable that smoking alone could account for such a profound effect.
This study confirmed an additional CAD risk difference based on routine fasting behavior and is the first to evaluate the association of routine fasting with angiographically-defined CAD. Fasting was defined in the study as abstinence from food and drink for an extended time period. This was designed to include the LDS definition and a broader set of other fasting definitions while retaining the periodic and routine aspects. Many religions encourage occasional fasting for purification and improving self-discipline,(21,22) and some contemporary wellness philosophies advocate prolonged fasting for bodily cleansing. LDS teachings provide for a once-monthly fast wherein adherents do not eat or drink for two consecutive meals (i.e., 24 hours) and children are encouraged to fast as early as the age of eight years, thus potentially establishing a pattern of fasting behavior early in life prior to the development of CAD.(8)
The lower risk of CAD herein may have occurred because fasting, or a behavior arising from it, is causally related to lower CAD risk. It may be that fasting improves an individual’s self-control over bodily appetites and desires,(8) which could translate to better discipline regarding daily caloric intake. Since this study did not evaluate caloric intake (i.e., diet), it is not clear whether diet or some dietary factor (e.g., vitamin, nutrient, or nutraceutical intake) may account for the finding. Since fasting-derived behavioral discipline (i.e., a “state of mind”) may account for the lower risk of CAD associated with fasting in this population, future investigation should evaluate dietary factors and self-discipline.
In contrast, the hypothesis that fasting may influence metabolic health is the more likely explanation based on evidence from the scientific literature. Decreased β-cell sensitivity to glucose (derangement of insulin secretion) and decreased sensitivity to insulin by peripheral tissues (insulin resistance) are well-established pathways in type II diabetes.(13,14) Desensitization of receptors to a stimulus is a well-known phenomenon that may occur quickly or after prolonged exposure to the stimulus.(13) Because it periodically eliminates such exposure, routine fasting may represent a behavioral approach to temporarily eliminate receptor stimulation and reset cellular sensitivity to glucose and/or insulin by periodically resting the system.(11) If so, fasting would be associated not only with lower risk of CAD but also with lower prevalence of diabetes, and this study found such associations. Because 18% of diabetics reported that they routinely fast and had a lower risk of CAD compared to non-fasting diabetics, this suggests that fasting may reduce diabetes risk and this should be further investigated.
Regarding glucose metabolism, Panowski and colleagues found that expression of the Caenorhabditis elegans PHA-4 gene was increased more than 80% due to fasting and, in separate experiments, that over-expression of PHA-4 increased longevity.(23) The murine and human FOXA genes are orthologous to the C. elegans PHA-4 gene. FOXA is a family of transcription factors that, among other things, regulate glucagon expression and glucose homeostasis, and do so to a greater degree in response to fasting.(24) Other transporter and metabolic enzyme genes are also differentially expressed due to fasting,(25) and new evidence suggests that fasting (termed “short-term starvation”) may activate a self-protective cellular stress-resistance mechanism.(26) Such direct impacts of fasting on longevity and homeostasis provide biologically plausible mechanisms that may explain how routine fasting behavior across the life span could reduce age-related chronic diseases such as CAD.
It may be instructive to also consider other populations where fasting behavior may be linked to diabetes or metabolic syndrome. It is increasingly evident that several ethnic populations whose ancestors historically experienced more frequent and severe feast-famine cycles than Caucasians did are today enduring higher rates of diabetes and metabolic syndrome.(27) The higher rates of disease among those ethnic groups is the result of both modern environmental factors and a shared genetic ability to withstand extended periods without food,(27) which may also be described as the inherited ability to endure more frequent periods of fasting or caloric restriction.
Several reports indicate that limiting caloric intake (i.e., “caloric restriction”) may have anti-aging (13) and cardio-protective effects.(9-11) It is expected that caloric restriction will lead to improved cardiac risk profiles.(9) While fasting was associated with lower diabetes prevalence, only small and not statistically-significant differences in BMI and hypertension were found based on fasting behavior. Evidence suggests that multiple calorie-deprivation pathways may exist that improve health,(23) thus any direct connection between fasting and caloric restriction requires further exploration.
Finally, evidence herein also suggests that fasting is associated with other behaviors common to this population. Patients who fasted were also more likely to not smoke, be more physically active, follow beverage proscriptions, engage in religious worship, and observe a day of rest. This allows for the possibility that fasting may simply be the best surrogate for a cluster of low-risk behaviors, including unmeasured factors. Fasting behavior was, however, reported by some with religious preferences other than LDS and, among these participants, an association of large effect size was found (a 77% lower risk of CAD). This suggests that the observed benefit arises from fasting and not from a cluster of religion-associated behaviors. Further, it is also unlikely that the other behaviors (at least the measured ones) account for the fasting benefit since they were all eliminated when statistical modeling included them along with fasting.
This study is potentially susceptible to various problems faced by all observational studies, including uncontrolled confounding, reverse causation, and self-selection in survey response. The association of religious preference with CAD was similar in both populations, though, and adjustment for various potential confounders did not eliminate or appreciably attenuate the association of fasting. Confirmatory studies in other populations are required since uncontrolled confounding may remain, including due to patient self-selection for survey response in this study’s hospital care setting.
The LDS proscription of alcohol is notable since non-use is associated in many studies with higher CAD risk compared to moderate levels of consumption.(4) If so, CAD risk would be expected to increase among LDS adherents, but this study suggests that abstinence from alcohol is not associated with higher CAD risk. While contrary to a commonly-held belief, this finding is supported by reports that the benefits of moderate alcohol consumption may arise from residual confounding due to socioeconomic and other factors,(28-30) an issue that only a randomized clinical trial could resolve. The current study appears to be the first wherein the majority of participants were non-drinkers, thus the social and behavioral risk profiles of drinkers and non-drinkers herein may be at variance with previously-studied populations.
This population is unique because of the aforementioned behaviors and the primarily Caucasian ethnic composition, thus the study findings may not be generalizable to other populations. Further study of fasting in other geographic locations and among other ethnicities is indicated.
A strength of the study was the CAD outcome that was determined from coronary angiography, the gold-standard assessment of CAD status. Cases had clinically-significant coronary stenoses. Controls, although not a random population sample, were definitively free from coronary lesions.
Supplementary Material
Acknowledgments
This study was funded in part by grants from the Deseret Foundation and NIH grant HL071878.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Heart Association . Heart disease and stroke statistics—2007 update. American Heart Association; Dallas, TX: 2007. p. e79. [Google Scholar]
- 2.Lyon JL, Wetzler HP, Gardner JW, Klauber MR, Williams RR. Cardiovascular mortality in Mormons and non-Mormons in Utah, 1969-1971. Am J Epidemiol. 1978;108:357–366. doi: 10.1093/oxfordjournals.aje.a112632. [DOI] [PubMed] [Google Scholar]
- 3.Williams RR, Lyon JL, Brockert JE, Maness AT. In: Havlik RJ, Feinleib M, editors. Decline in coronary mortality rates: Utah vs. United States; Proceedings of the Conference on the Decline in CHD Mortality; Washington, D.C.: U.S. Department of Health and Human Services. 1979:48-57; NIH publication No. 79-1610. [Google Scholar]
- 4.Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, Jr, Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997;337:1705–1714. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- 5.Lopez-Garcia E, van Dam RM, Willett WC, Rimm EB, Manson JE, Stampfer MJ, Rexrode KM, Hu FB. Coffee consumption and coronary heart disease in men and women: a prospective cohort study. Circulation. 2006;113:2045–2053. doi: 10.1161/CIRCULATIONAHA.105.598664. [DOI] [PubMed] [Google Scholar]
- 6.Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health. A critical review of the evidence for biological pathways. Am Psychol. 2003;58:53–63. doi: 10.1037/0003-066x.58.1.53. [DOI] [PubMed] [Google Scholar]
- 7.Berkman L, Glass T. Social integration, social networks, social support, and health. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford University Press; New York, NY: 2000. pp. 137–73. [Google Scholar]
- 8.Gospel principles. Intellectual Reserve, Inc.; Salt Lake City, UT: 1997. The Church of Jesus Christ of Latter-day Saints; pp. 165–169. Fasting. [Google Scholar]
- 9.Fontana L, Meyer T, Klein S, Holloszy JO. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A. 2004;101:6659–6663. doi: 10.1073/pnas.0308291101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cefalu WT, Wang ZQ, Bell-Farrow AD, Collins J, Morgan T, Wagner JD. Caloric restriction and cardiovascular aging in cynomolgus monkeys (Macaca fascicularis): metabolic, physiologic, and atherosclerotic measures from a 4-year intervention trial. J Gerontol A Biol Sci Med Sci. 2004;59:1007–1014. doi: 10.1093/gerona/59.10.b1007. [DOI] [PubMed] [Google Scholar]
- 11.DeFronzo RA. Insulin resistance, hyperinsulinemia, and coronary artery disease: a complex metabolic web. J Cardiovasc Pharmacol. 1992;20(Suppl 11):S1–S16. doi: 10.1097/00005344-199200111-00002. [DOI] [PubMed] [Google Scholar]
- 12.Ingram DK, Young J, Mattison JA. Calorie restriction in nonhuman primates: assessing effects on brain and behavioral aging. Neuroscience. 2007;145:1359–1364. doi: 10.1016/j.neuroscience.2006.10.031. [DOI] [PubMed] [Google Scholar]
- 13.Rustenbeck I, Wienbergen A, Bleck C, Jörns A. Desensitization of insulin secretion by depolarizing insulin secretagogues. Diabetes. 2004;53:S140–S150. doi: 10.2337/diabetes.53.suppl_3.s140. [DOI] [PubMed] [Google Scholar]
- 14.Liang CP, Han S, Senokuchi T, Tall AR. The macrophage at the crossroads of insulin resistance and atherosclerosis. Circ Res. 2007;100:1546–1555. doi: 10.1161/CIRCRESAHA.107.152165. [DOI] [PubMed] [Google Scholar]
- 15.Anonymous Myocardial infarction and mortality in the coronary artery surgery study (CASS) randomized trial. N Engl J Med. 1984;310(12):750–8. doi: 10.1056/NEJM198403223101204. [DOI] [PubMed] [Google Scholar]
- 16.Taylor GS, Muhlestein JB, Wagner GS, Bair TL, Li P, Anderson JL. Implementation of a computerized cardiovascular information system in a private hospital setting. Am Heart J. 1998;136:792–803. doi: 10.1016/s0002-8703(98)70123-1. [DOI] [PubMed] [Google Scholar]
- 17.D’Agostino RB, Sr., Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care. The Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 18.The Lord’s law of health . Gospel principles. Intellectual Reserve, Inc.; Salt Lake City, UT: 1997. The Church of Jesus Christ of Latter-day Saints; pp. 192–196. [Google Scholar]
- 19.The Sabbath day . Gospel principles. Intellectual Reserve, Inc.; Salt Lake City, UT: 1997. The Church of Jesus Christ of Latter-day Saints; pp. 159–164. [Google Scholar]
- 20.Paffenbarger R, Wing A, Hyde R. Paffenbarger physical activity questionnaire. Med Sci Sports Exerc. 1997;29:S83–S88. [Google Scholar]
- 21.Hallak MH, Nomani MZ. Body weight loss and changes in blood lipid levels in normal men on hypocaloric diets during Ramadan fasting. Am J Clin Nutr. 1988;48:1197–1210. doi: 10.1093/ajcn/48.5.1197. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan M, Eidelman AI, Aboulafia Y. Fasting and the precipitation of labor. The Yom Kippur effect. JAMA. 1983;250:1317–1318. [PubMed] [Google Scholar]
- 23.Panowski SH, Wolff S, Aguilaniu H, Durieux J, Dillin A. PHA-4/Foxa mediates diet-restriction-induced longevity of C. elegans. Nature. 2007;447:550–556. doi: 10.1038/nature05837. [DOI] [PubMed] [Google Scholar]
- 24.Zhang L, Rubins NE, Ahima RS, Greenbaum LE, Kaestner KH. Foxa2 integrates the transcriptional response of the hepatocyte to fasting. Cell Metab. 2005;2:141–148. doi: 10.1016/j.cmet.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Van den Bosch HM, Bünger M, de Groot PJ, van der Meijde J, Hooiveld GJEJ, Müller M. Gene expression of transporters and phase I/II metabolic enzymes in murine small intestine during fasting. BMC Genomics. 2007;8:267–278. doi: 10.1186/1471-2164-8-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raffaghello L, Lee C, Safdie FM, Wei M, Madia F, Bianchi G, Longo VD. Starvartion-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc Natl Acad Sci U S A. 2008 doi: 10.1073/pnas.0708100105. March 31, Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egede LE, Dagogo-Jack S. Epidemiology of type 2 diabetes: focus on ethnic minorities. Med Clin North Am. 2005;89:949–975. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Mortensen EL, Jensen HH, Sanders SA, Reinisch JM. Better psychological functioning and higher social status may largely explain the apparent health benefits of wine. Arch Intern Med. 2001;161:1844–1848. doi: 10.1001/archinte.161.15.1844. [DOI] [PubMed] [Google Scholar]
- 29.Naimi TS, Brown DW, Brewer RD, Wells S. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 30.Jackson R, Broad J, Connor J, et al. Alcohol and ischaemic heart disease: probably no free lunch. Lancet. 2005;366:1911–1912. doi: 10.1016/S0140-6736(05)67770-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


