Abstract
The emergence of catheter based ablation therapy for the prevention of recurrent atrial fibrillation has increased interest in the anatomy of the left atrium and pulmonary veins. In this article, we review the magnetic resonance imaging method of imaging the left atrium and the pulmonary veins, normal and variant anatomy, and the utility of imaging before and after atrial fibrillation ablation.
Keywords: Left atrium, Magnetic resonance imaging, Pulmonary veins, Atrial fibrillation
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, affecting more than 2 million people in the United States,1 and is a major cause of morbidity and mortality, accounting for more than 400 000 hospitalizations each year.2 Atrial fibrillation quintuples the risk of stroke3 and is the attributed cause for 15% of all strokes, totalling more than 100 000 per year.2 Although several antiarrhythmic drugs are available for the treatment of AF, maintenance of sinus rhythm is frequently suboptimal,4–6 and all are associated with significant side effects or adverse events.7
While the role of the left atrium in the development of AF has been known for some time, recent evidence has shown that the pulmonary veins also play a critical role in the pathophysiology of AF. The pulmonary veins and left atrium are both derived from the primitive common pulmonary vein8 and therefore have many anatomic similarities. Both are smooth-walled structures that have electrically active myocardium. Approximately 90% of pulmonary veins contain atrial myocardium.9 Although the myocardium in the atrium is uniform, myocardium in the pulmonary veins is frequently discontinuous and fibrotic. Patients with a history of AF uniformly have myocardium in the pulmonary veins and an increased rate of structural abnormalities. These structural abnormalities result in abnormal electrical activation with slow and anisotropic conduction. Proarrhythmic ectopic beats, local re-entry, and sustained focal activity are often observed and can be easily induced.10
A landmark study demonstrated that the proarrhythmic electrical activity in pulmonary veins is directly responsible for the generation of AF in many patients.11 Among those with paroxysmal AF, 94% were found to have ectopic foci in the pulmonary veins that were responsible for the induction of AF. Radiofrequency ablation of these foci resulted in complete suppression of AF in a majority of patients. After the report of these findings, several related procedures were developed for the treatment of AF.11–14 Each of these procedures uses radiofrequency ablation delivered around the pulmonary veins, with or without additional ablation within the left atrium, to either electrically isolate the pulmonary veins from the left atrium or to modify the atrial myocardium around the pulmonary veins. Short-term success rates range from 65 to 85% in patients with paroxysmal AF, with a reduction in morbidity and improved quality of life.15
With the development of radiofrequency ablation for the treatment of AF, there has been increased interest in the accurate determination of left atrial and pulmonary vein anatomy to help plan the procedure and to monitor for post-ablation complications. The left atrium and pulmonary veins can be readily imaged using standard cardiovascular magnetic resonance (CMR) techniques, but contrast-enhanced magnetic resonance angiography (CE-MRA) and high-resolution late gadolinium enhancement (LGE) CMR provide greater anatomic detail and information about the presence of scar after radiofrequency ablation. In this review, we present the methods used to image the left atrium and pulmonary veins, normal and anomalous left atrial and pulmonary venous anatomy, and the utility of imaging before and after AF ablation.
Imaging method and display
The left atrium and pulmonary veins can be identified using standard anatomic and functional CMR imaging sequences. These methods are usually sufficient to identify the anatomic relationship of the left atrium and proximal pulmonary veins to the heart and the other major thoracic structures (Figure 1). More anatomic detail regarding the left atrium and pulmonary veins can be obtained using CE-MRA (Figure 2). A three-dimensional (3D) spoiled gradient echo sequence is acquired during the first-pass of gadolinium contrast.16 Clinical protocols vary but the technique typically uses short repetition times (3–6 ms), a high flip angle (30–60°), and fractional echoes to provide T1-weighting and minimal flow artifacts.17–25 The spatial resolution varies from 1–2 × 1–2 mm in-plane with 2–4 mm slices, before interpolation. A single 3D volume requires a 10–20 s breath-hold to suppress ventilatory motion, but scan time can be shortened using smaller fields of view, shorter repetition times, partial Fourier, lower spatial resolution, or parallel imaging. ECG-triggering is not employed, although it is recognized that the position and shape of the pulmonary veins changes throughout the cardiac cycle.22,26 Images obtained with this method appear to reflect the pulmonary veins at their maximal size.27 Axial slabs are usually acquired, using either sequential or centric k-space filling. For the pulmonary vasculature, the arterial–venous transit time is very short (4–7 s)28 and therefore artery–vein separation is highly challenging and generally not targeted. Contrast is injected with a dose of 0.1–0.2 mmol/kg at a rate of 1–2 mL/s, followed by a saline flush. A pre-contrast mask can be acquired, although mask subtraction is not essential for pulmonary venography since the background signal in the lungs is very low. Often a second time-frame is acquired immediately after the first pass image to ensure acquisition during peak contrast. Timing of the acquisition to the first pass of contrast through the pulmonary veins is critical, and is achieved using either a bolus timing scan29 or with fluoroscopic triggering.30 For either method, imaging is timed to begin with the appearance of contrast in the left atrium.
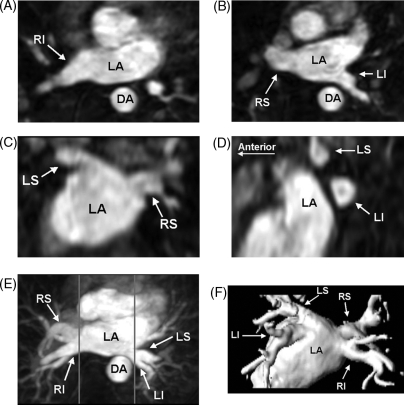
Figure 1.
Axial spin-echo T1 weighted cardiovascular magnetic resonance at the level of the left atrium (LA) and right inferior pulmonary vein (RI). The oesophagus (Eso) is immediately posterior to the left atrium and adjacent to the right inferior pulmonary vein. The oesophagus is compressed between the enlarged left atrium and the spinal column. The ascending aorta (AA), descending aorta (DA), and superior vena cava (SVC) are also shown.
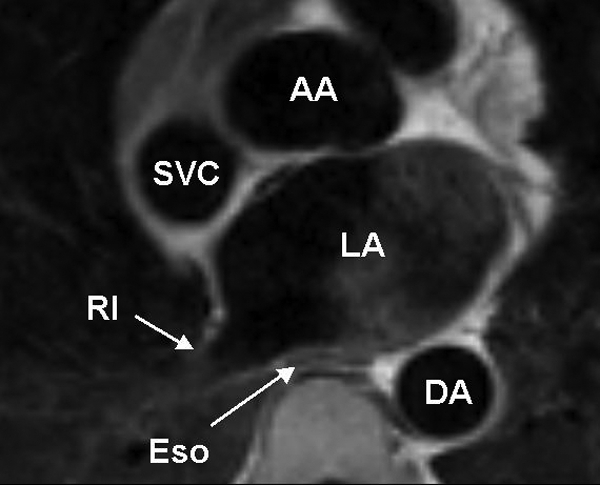
Figure 2.
Pulmonary vein three-dimensional contrast-enhanced magnetic resonance angiography showing the normal anatomy and quantification of pulmonary vein size. These images show the normal complement of four pulmonary veins, along with left atrium (LA) and descending aorta (DA). The right inferior (RI), right superior (RS), and left inferior (LI) pulmonary veins are shown in the axial plane (A and B). The left superior (LS) and right superior pulmonary veins are shown in the coronal plane from the posterior–anterior orientation (C). The left superior (LS) and left inferior (LI) pulmonary veins are shown in the sagittal plane (D, anterior to the left). All of the pulmonary veins are shown in the axial maximal intensity projection (E) and posterior–anterior volume rendered (F) image. The aorta has been removed from the volume rendered image to show all of the pulmonary veins. All of these images were derived from the same three-dimensional magnetic resonance angiography dataset. The gray lines in the maximal intensity projection image (E) correspond to the location in the sagittal plane in which the pulmonary veins separate from the left atrium and from each other. The maximal diameter, perimeter and cross-sectional area can be easily measured in the sagittal images.
Once the 3D CE-MRA dataset is obtained, the images can be transferred to a workstation for further manipulation and analysis (Figure 2). The simplest and often most informative method to display the images is to dynamically view 2D slices within the 3D dataset in the axial, coronal and sagittal planes. The axial images usually provide a good overview of the pulmonary veins and their relationship to the left atrium, but the coronal and sagittal images are frequently required to determine specific anatomic findings, such as a left common or anomalous pulmonary vein.
Although 2D slices are very useful for viewing the individual pulmonary veins, it is difficult to produce a single summary image of the anatomy. Maximal intensity projection and 3D reconstructions displayed as shaded surface or volume rendered images take full advantage of the 3D dataset and provide very good summary images. These are most useful when the displayed volume is limited to the left atrium and pulmonary veins. Because the aorta is directly posterior to the left-sided pulmonary vein, it frequently obscures them from view in the maximal intensity projection images. Three-dimensional reconstructed images are frequently preferred because the aorta can be excluded from the displayed volume. Moving images can also be generated to better display the anatomy. By convention, the left atrium and pulmonary veins are viewed in the posterior–anterior orientation. Some software systems allow integration of the 3D CE-MRA images with results from electro-anatomic mapping to help guide ablation procedures.31
The accurate measurement of pulmonary vein size is essential for serial assessment of pulmonary vein stenosis and to further investigate the role of pulmonary veins in the initiation and maintenance of AF. Most investigators have measured pulmonary vein diameters in a specified plane, usually at the ostia.17,32,33 These measurements tend to have poor reproducibility for several reasons. Identification of the true ostia is very difficult because the pulmonary veins and left atrium are embryologically related with no clear anatomic border between them. The pulmonary vein ostia are not round but ovoid, such that measurements taken at the same location vary significantly with the plane of measurement.17,18 A further complication is that most measurements are derived from non-gated images while the pulmonary vein size varies significantly over the cardiac cycle.22,34 These difficulties were highlighted in a study comparing pulmonary vein diameter measurements performed using computed tomography, intracardiac echocardiography, transoesophageal echocardiography, and venography in the same patients.35 Each of these methods identified different numbers and positions of pulmonary veins with a poor correlation between diameter measurements obtained with each imaging modality.
Tomographic imaging of the pulmonary veins using CMR has several advantages. All of the anatomic information is obtained in a single 3D dataset that can be manipulated in numerous ways. This allows for anatomic measurements in any desired plane, including determination of the perimeter and cross-sectional area that may be more meaningful measures of pulmonary vein size. A simple method for determining pulmonary vein size in the sagittal plane is highly reproducible and provides these additional measures.18 The maximal diameter, perimeter, and cross-sectional area are measured at the location in the sagittal plane at which the pulmonary veins separate from the left atrium and from each other (Figure 2). This is easily determined by scrolling through a reconstruction of the 3D dataset in the sagittal plane. Because the measurements are made in a standard plane and location, reproducibility is greatly improved compared to standard diameter measurements.18 This allows for more accurate determination of inter-study differences in pulmonary vein size and increased statistical power in research studies. Even in the absence of severe stenosis, this method can identify small changes in pulmonary vein size after AF ablation that may be due to hemodynamic changes related to the restoration of sinus rhythm.19 The determination of the cross-sectional area is also advantageous. Patients with larger summed total pulmonary vein cross-sectional area are more likely to have recurrent AF after ablation independent of the type of AF or left atrial size.36 Diameter measurements do not have predictive value.15
One of the advantages of CMR is the ability to characterize myocardial scarring and fibrosis using LGE.37–39 Gadolinium contrast remains concentrated in the regions of scar, compared with normal myocardium or blood, due to reduced clearance and the large contrast volume of distribution in fibrotic regions.37 Imaging with a strongly T1-weighed sequence can then be performed 10–20 min after the CE-MRA to detect these areas of left atrial and pulmonary vein and scarring and fibrosis.39 While this technique has generally been used to identify myocardial scar in the left ventricle in patients with myocardial infarction,38 it has also been adapted to identify scar in the left atrium and pulmonary veins after AF ablation (Figure 3).40 The standard method is modified to achieve higher spatial resolution (1.3 × 1.3 × 5 mm) by acquiring a 3D volume during free-breathing with ventilatory motion compensated imaging.
Figure 3.
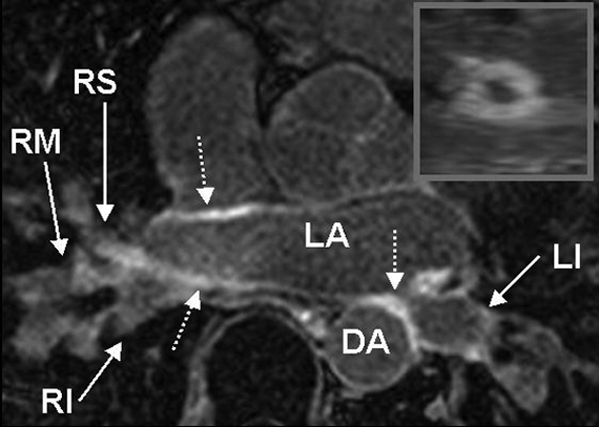
Axial late gadolinium enhancement image of the left atrium and pulmonary veins. These images show the left atrial and pulmonary vein scar 6 weeks after atrial fibrillation ablation. After ablation there is evidence of pulmonary vein scar (bright area indicated by the dashed arrows) in the wall of the left atrium and the pulmonary veins. The inset shows a reformatted image of the left inferior pulmonary vein that shows circumferential scar.
Normal and variant left atrial and pulmonary venous anatomy
The left atrium is located posteriorly in the chest, adjacent to the descending aorta. There are usually four pulmonary veins that enter the left atrium: right superior, right inferior, left superior, and left inferior (Figure 1). Each of the veins is directed laterally, with the inferior veins directed posteriorly and the superior veins directed anteriorly. The left superior pulmonary vein frequently has a cranial angulation and may appear to arise from the superior portion of the left atrium.
While there is very little variation in the normal left atrial anatomy, non-pathologic variations in the pulmonary vein anatomy are very common, present in ∼40% of patients.17,41 Although numerous variations have been described, the most common are the presence of a single left common pulmonary vein or an additional right middle pulmonary vein (Figure 4).18 These variations occur due to more or less incorporation of the primitive common pulmonary vein into the body of the left atrium. Less incorporation leads to apparent fusion of pulmonary veins prior to entering the left atrium, while more incorporation results in additional pulmonary veins (Figure 5).42 Because the right-sided pulmonary veins form first and have more developmental time to be incorporated into the left atrium, it is more common to have additional veins on the right. Conversely, the left-sided pulmonary veins form later and are more likely to have a common trunk. These variations in pulmonary venous anatomy have not yet been identified as a cause of pathology.
Figure 4.
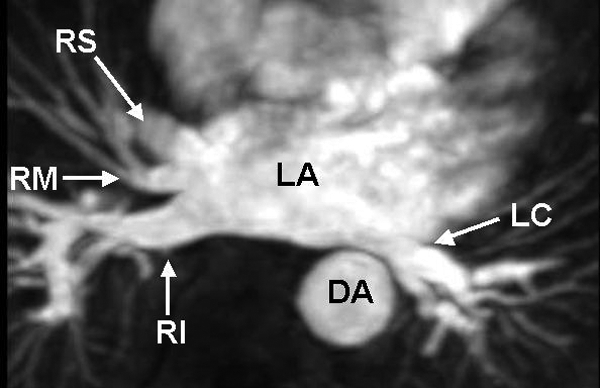
Three-dimensional contrast-enhanced magnetic resonance angiography of variant pulmonary venous anatomy. This image was obtained from a patient with right middle (RM) and left common (LC) pulmonary veins.
Figure 5.
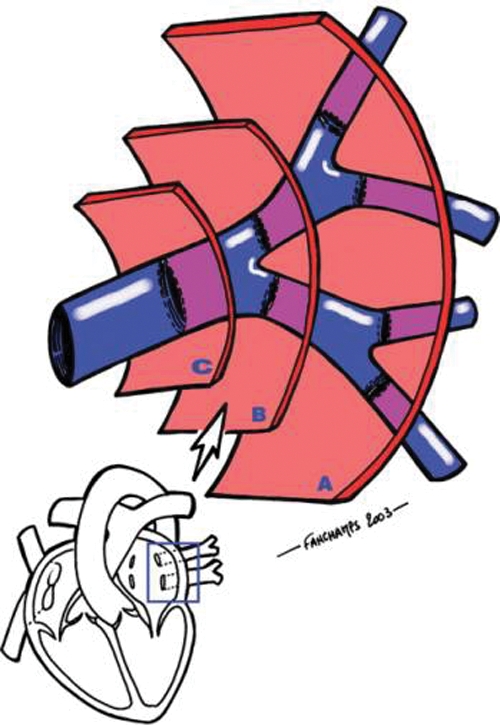
Incorporation of the primitive common pulmonary vein into the left atrium. The incorporation of the primitive common pulmonary vein is variable and results in non-pathological variations in the normal anatomy. This figure shows the results of variable incorporation of the left-sided pulmonary veins. The most common pattern is two left-sided pulmonary veins (B). With less incorporation of the common pulmonary vein into the left atrium, there is only a single left common pulmonary vein (C). With more incorporation, there are additional pulmonary veins (A). From Ghaye et al.42 (used with permission).
Imaging before and after atrial fibrillation ablation
Imaging is usually performed before AF ablation to determine the left atrial and pulmonary vein anatomy and after the procedure to screen for stenosis. Late gadolinium enhancement imaging for the detection of left atrial and pulmonary vein scar is able to identify scar from the ablation and may provide important information about the completeness of ablation and atrial remodelling after the procedure.
Cardiovascular magnetic resonance is able to identify the relationship of the left atrium to other major thoracic structures, particularly the oesophagus (Figure 1). The formation of an atrial-oesophageal fistula is a rare but catastrophic complication of radiofrequency ablation procedures for the treatment of AF that is caused by excessive heating of the posterior left atrial wall and the adjacent oesophagus.43,44 The oesophagus is almost always directly behind the left atrium and is usually closer to the left-sided pulmonary veins, but the location is highly variable.45,46 The oesophagus is frequently within 5 mm of the pulmonary veins at a location that probably increases the risk for the formation of an atrial-oesophageal fistula.47,48 The risk of causing an atrial-oesophageal fistula may be reduced by avoiding ablation in the region of the left atrium closest to the oesophagus, but this may be difficult as the oesophagus is mobile and may move during the course of the procedure.49
The accurate determination of pulmonary vein anatomy is critical for the planning and execution of AF ablation. To achieve success, the operator must place a series of radiofrequency lesions that encircle the pulmonary veins. Using the most common ablation strategy, most operators use electrical isolation of the pulmonary veins from the left atrium as the endpoint of ablation.50 This necessarily requires that the pulmonary vein anatomy be determined prior to the procedure. In the initial development of the procedure the pulmonary veins were identified using invasive contrast venography.33 Although this can be done successfully, it greatly increases the procedure time and only provides projection images of the pulmonary veins. Most centres now use magnetic resonance angiography or multi-detector computed tomography to determine the pulmonary vein anatomy prior to the procedure. Both techniques provide high-resolution 3D tomographic images of the pulmonary veins and other mediastinal structures. These images can also be imported into the 3D electrophysiological mapping systems that are an integral part of the procedure to combine anatomic and functional information during the procedure.51
The pulmonary veins are imaged after the procedure to screen for pulmonary vein stenosis. Pulmonary vein stenosis is an uncommon but severe complication of AF ablation.17,32,33,41,52–57 The application of radiofrequency energy to the pulmonary veins causes intimal proliferation and myocardial necrosis that can result in stenosis or occlusion.58 Severe stenosis occurs in up to 5% of patients after the procedure and results in pulmonary hypertension and decreased perfusion of the affected lung segments.59,60 Patients frequently present with cough or dyspnea, but a significant proportion are asymptomatic.54 Stenosis is most likely to occur in smaller pulmonary veins in which the ablation lesions were placed further into the pulmonary vein trunk and with greater extent of ablation.32,57 If stenosis does occur, pulmonary vein angioplasty is usually successful in restoring normal flow and alleviating symptoms.61 Newer techniques that have emphasized placing ablation lesions within the left atrium under intra-cardiac echocardiographic guidance have reduced the rate of pulmonary vein stenosis,53 but screening is still recommended for all patients.
Radiofrequency ablation for the treatment of AF results in scarring of the pulmonary vein and left atrium.58 Late gadolinium enhancement imaging to identify this scar has the potential to non-invasively assess the completeness of ablation by providing a precise anatomic map of the ablation lines (Figure 3). This could be useful either after the procedure to assess patient outcomes or as a real-time tool to guide ablation during interventional CMR. In addition, the extent of left atrial scar is associated with decreased left atrial contractile function after AF ablation, a finding that may have important implications for risk of thrombo-embolic events even in the absence of AF.62
Summary
Cardiovascular magnetic resonance readily images left atrial and pulmonary vein anatomy. Contrast-enhanced magnetic resonance angiography provides a comprehensive assessment of the anatomy that is very useful to define normal and variant anatomy. Imaging is usually performed before ablation to plan for the procedure and after to screen for pulmonary vein stenosis. Quantification of pulmonary vein size is important for the comparison of serial studies and is easily accomplished by examining images in the sagittal plane. Late gadolinium enhancement imaging of the left atrium and pulmonary veins is a new technique that may be useful to define the extent of ablation and clinical success.
Conflict of interest: none declared.
Funding
Supported by grants from the American Heart Association (AHA SDG 0530061N) and the National Institutes of Health (NIBIB K01 EB004434-01A1).
References
- 1.Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995;155:469–73. [PubMed] [Google Scholar]
- 2.Heart Disease and Storke Statistics—2004 Update. Dallas, TX: American Heart Association; 2004. [Google Scholar]
- 3.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 4.Hauser TH, Pinto DS, Josephson ME, Zimetbaum P. Early recurrence of arrhythmia in patients taking amiodarone or class 1C agents for treatment of atrial fibrillation or atrial flutter. Am J Cardiol. 2004;93:1173–6. doi: 10.1016/j.amjcard.2004.01.051. [DOI] [PubMed] [Google Scholar]
- 5.Singh BN, Singh SN, Reda DJ, et al. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861–72. doi: 10.1056/NEJMoa041705. [DOI] [PubMed] [Google Scholar]
- 6.Roy D, Talajic M, Dorian P, et al. Amiodarone to prevent recurrence of atrial fibrillation. Canadian Trial of Atrial Fibrillation Investigators. N Engl J Med. 2000;342:913–20. doi: 10.1056/NEJM200003303421302. [DOI] [PubMed] [Google Scholar]
- 7.Hauser TH, Pinto DS, Josephson ME, Zimetbaum P. Safety and feasibility of a clinical pathway for the outpatient initiation of antiarrhythmic medications in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2003;91:1437–41. doi: 10.1016/s0002-9149(03)00395-3. [DOI] [PubMed] [Google Scholar]
- 8.Moore KL. Philadelphia: W.B. Saunders Co; 1988. The Developing Human. [Google Scholar]
- 9.Hassink RJ, Aretz HT, Ruskin J, Keane D. Morphology of atrial myocardium in human pulmonary veins: a postmortem analysis in patients with and without atrial fibrillation. J Am Coll Cardiol. 2003;42:1108–14. doi: 10.1016/s0735-1097(03)00918-5. [DOI] [PubMed] [Google Scholar]
- 10.Arora R, Verheule S, Scott L, et al. Arrhythmogenic substrate of the pulmonary veins assessed by high-resolution optical mapping. Circulation. 2003;107:1816–21. doi: 10.1161/01.CIR.0000058461.86339.7E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 12.Pappone C, Rosanio S, Oreto G, et al. Circumferential radiofrequency ablation of pulmonary vein ostia. A new anatomic approach for curing atrial fibrillation. Circulation. 2000;102:2619–28. doi: 10.1161/01.cir.102.21.2619. [DOI] [PubMed] [Google Scholar]
- 13.Arentz T, von Rosenthal J, Blum T, et al. Feasibility and safety of pulmonary vein isolation using a new mapping and navigation system in patients with refractory atrial fibrillation. Circulation. 2003;108:2484–90. doi: 10.1161/01.CIR.0000097118.75179.83. [DOI] [PubMed] [Google Scholar]
- 14.Oral H, Knight BP, Ozaydin M, et al. Segmental ostial ablation to isolate the pulmonary veins during atrial fibrillation: feasibility and mechanistic insights. Circulation. 2002;106:1256–62. doi: 10.1161/01.cir.0000027821.55835.00. [DOI] [PubMed] [Google Scholar]
- 15.Pappone C, Rosanio S, Augello G, et al. Mortality, morbidity, and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol. 2003;42:185–97. doi: 10.1016/s0735-1097(03)00577-1. [DOI] [PubMed] [Google Scholar]
- 16.Prince MR, Narasimham DL, Stanley JC, et al. Breath-hold gadolinium-enhanced MR angiography of the abdominal aorta and its major branches. Radiology. 1995;197:785–92. doi: 10.1148/radiology.197.3.7480757. [DOI] [PubMed] [Google Scholar]
- 17.Wittkampf FH, Vonken EJ, Derksen R, et al. Pulmonary vein ostium geometry: analysis by magnetic resonance angiography. Circulation. 2003;107:21–3. doi: 10.1161/01.cir.0000047065.49852.8f. [DOI] [PubMed] [Google Scholar]
- 18.Hauser TH, Yeon SB, McClennen S, et al. A method for the determination of proximal pulmonary vein size using contrast-enhanced magnetic resonance angiography. J Cardiovasc Magn Reson. 2004;6:927–36. doi: 10.1081/jcmr-200037474. [DOI] [PubMed] [Google Scholar]
- 19.Hauser TH, Yeon SB, McClennen S, et al. Subclinical pulmonary vein narrowing after ablation for atrial fibrillation. Heart. 2005;91:672–3. doi: 10.1136/hrt.2004.039347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mansour M, Holmvang G, Sosnovik D, et al. Assessment of pulmonary vein anatomic variability by magnetic resonance imaging: implications for catheter ablation techniques for atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15:387–93. doi: 10.1046/j.1540-8167.2004.03515.x. [DOI] [PubMed] [Google Scholar]
- 21.Mlcochova H, Tintera J, Porod V, Peichl P, Cihak R, Kautzner J. Magnetic resonance angiography of pulmonary veins: implications for catheter ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2005;28:1073–80. doi: 10.1111/j.1540-8159.2005.00228.x. [DOI] [PubMed] [Google Scholar]
- 22.Syed MA, Peters DC, Rashid H, Arai AE. Pulmonary vein imaging: comparison of 3D magnetic resonance angiography with 2D cine MRI for characterizing anatomy and size. J Cardiovasc Magn Reson. 2005;7:355–60. doi: 10.1081/jcmr-200053458. [DOI] [PubMed] [Google Scholar]
- 23.Tamborero D, Mont L, Nava S, et al. Incidence of pulmonary vein stenosis in patients submitted to atrial fibrillation ablation: a comparison of the selective segmental ostial ablation vs the circumferential pulmonary veins ablation. J Interv Card Electrophysiol. 2005;14:21–5. doi: 10.1007/s10840-005-4513-6. [DOI] [PubMed] [Google Scholar]
- 24.Tsao HM, Wu MH, Huang BH, et al. Morphologic remodeling of pulmonary veins and left atrium after catheter ablation of atrial fibrillation: insight from long-term follow-up of three-dimensional magnetic resonance imaging. J Cardiovasc Electrophysiol. 2005;16:7–12. doi: 10.1046/j.1540-8167.2005.04407.x. [DOI] [PubMed] [Google Scholar]
- 25.Vonken EP, Velthuis BK, Wittkampf FH, Rensing BJ, Derksen R, Cramer MJ. Contrast-enhanced MRA and 3D visualization of pulmonary venous anatomy to assist radiofrequency catheter ablation. J Cardiovasc Magn Reson. 2003;5:545–51. doi: 10.1081/jcmr-120025229. [DOI] [PubMed] [Google Scholar]
- 26.Lickfett L, Dickfeld T, Kato R, et al. Changes of pulmonary vein orifice size and location throughout the cardiac cycle: dynamic analysis using magnetic resonance cine imaging. J Cardiovasc Electrophysiol. 2005;16:582–8. doi: 10.1046/j.1540-8167.2005.40724.x. [DOI] [PubMed] [Google Scholar]
- 27.Hauser TH, Yeon SB, McClennen S, et al. Variability in Pulmonary Vein Anatomy During the Cardiac Cycle. Society for Cardiovascular Magnetic Resonance; 2005. [Google Scholar]
- 28.Schoenberg SO, Bock M, Floemer F, et al. High-resolution pulmonary arterio- and venography using multiple-bolus multiphase 3D-Gd-mRA. J Magn Reson Imaging. 1999;10:339–46. doi: 10.1002/(sici)1522-2586(199909)10:3<339::aid-jmri16>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 29.Earls JP, Rofsky NM, DeCorato DR, Krinsky GA, Weinreb JC. Breath-hold single-dose gadolinium-enhanced three-dimensional MR aortography: usefulness of a timing examination and MR power injector. Radiology. 1996;201:705–10. doi: 10.1148/radiology.201.3.8939219. [DOI] [PubMed] [Google Scholar]
- 30.Wilman AH, Riederer SJ, King BF, Debbins JP, Rossman PJ, Ehman RL. Fluoroscopically triggered contrast-enhanced three-dimensional MR angiography with elliptical centric view order: application to the renal arteries. Radiology. 1997;205:137–46. doi: 10.1148/radiology.205.1.9314975. [DOI] [PubMed] [Google Scholar]
- 31.Dong J, Dickfeld T, Dalal D, et al. Initial experience in the use of integrated electroanatomic mapping with three-dimensional MR/CT images to guide catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2006;17:459–66. doi: 10.1111/j.1540-8167.2006.00425.x. [DOI] [PubMed] [Google Scholar]
- 32.Dill T, Neumann T, Ekinci O, et al. Pulmonary vein diameter reduction after radiofrequency catheter ablation for paroxysmal atrial fibrillation evaluated by contrast-enhanced three-dimensional magnetic resonance imaging. Circulation. 2003;107:845–50. doi: 10.1161/01.cir.0000048146.81336.1d. [DOI] [PubMed] [Google Scholar]
- 33.Lin WS, Prakash VS, Tai CT, et al. Pulmonary vein morphology in patients with paroxysmal atrial fibrillation initiated by ectopic beats originating from the pulmonary veins: implications for catheter ablation. Circulation. 2000;101:1274–81. doi: 10.1161/01.cir.101.11.1274. [DOI] [PubMed] [Google Scholar]
- 34.Bowman AW, Kovacs SJ. Prediction and assessment of the time-varying effective pulmonary vein area via cardiac MRI and Doppler echocardiography. Am J Physiol Heart Circ Physiol. 2005;288:H280–H286. doi: 10.1152/ajpheart.00713.2004. [DOI] [PubMed] [Google Scholar]
- 35.Wood MA, Wittkamp M, Henry D, et al. A comparison of pulmonary vein ostial anatomy by computerized tomography, echocardiography, and venography in patients with atrial fibrillation having radiofrequency catheter ablation. Am J Cardiol. 2004;93:49–53. doi: 10.1016/j.amjcard.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 36.Hauser TH, Essebag V, Baldessin F, et al. Larger pulmonary vein cross-sectional area is associated with recurrent atrial fibrillation after pulmonary vein isolation. Circulation. 2005;112:II-555. [Google Scholar]
- 37.Judd RM, Lugo-Olivieri CH, Arai M, et al. Physiological basis of myocardial contrast enhancement in fast magnetic resonance images of 2-day-old reperfused canine infarcts. Circulation. 1995;92:902–10. doi: 10.1161/01.cir.92.7.1902. [DOI] [PubMed] [Google Scholar]
- 38.Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–53. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 39.Simonetti OP, Kim RJ, Fieno DS, et al. An improved MR imaging technique for the visualization of myocardial infarction. Radiology. 2001;218:215–23. doi: 10.1148/radiology.218.1.r01ja50215. [DOI] [PubMed] [Google Scholar]
- 40.Peters DC, Wylie JV, Hauser TH, et al. Detection of pulmonary vein and left atrial scar after catheter ablation with three-dimensional navigator-gated delayed enhancement MR imaging: initial experience. Radiology. 2007;243:690–5. doi: 10.1148/radiol.2433060417. [DOI] [PubMed] [Google Scholar]
- 41.Kato R, Lickfett L, Meininger G, et al. Pulmonary vein anatomy in patients undergoing catheter ablation of atrial fibrillation: lessons learned by use of magnetic resonance imaging. Circulation. 2003;107:2004–10. doi: 10.1161/01.CIR.0000061951.81767.4E. [DOI] [PubMed] [Google Scholar]
- 42.Ghaye B, Szapiro D, Dacher JN, et al. Percutaneous ablation for atrial fibrillation: the role of cross-sectional imaging. Radiographics. 2003;23:S19–33. doi: 10.1148/rg.23si035513. discussion: S48–50. [DOI] [PubMed] [Google Scholar]
- 43.Scanavacca MI, D'Avila A, Parga J, Sosa E. Left atrial-esophageal fistula following radiofrequency catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15:960–2. doi: 10.1046/j.1540-8167.2004.04083.x. [DOI] [PubMed] [Google Scholar]
- 44.Cummings JE, Schweikert RA, Saliba WI, et al. Assessment of temperature, proximity, and course of the esophagus during radiofrequency ablation within the left atrium. Circulation. 2005;112:459–64. doi: 10.1161/CIRCULATIONAHA.104.509612. [DOI] [PubMed] [Google Scholar]
- 45.Lemola K, Sneider M, Desjardins B, et al. Computed tomographic analysis of the anatomy of the left atrium and the esophagus: implications for left atrial catheter ablation. Circulation. 2004;110:3655–60. doi: 10.1161/01.CIR.0000149714.31471.FD. [DOI] [PubMed] [Google Scholar]
- 46.Tsao HM, Wu MH, Higa S, et al. Anatomic relationship of the esophagus and left atrium: implication for catheter ablation of atrial fibrillation. Chest. 2005;128:2581–7. doi: 10.1378/chest.128.4.2581. [DOI] [PubMed] [Google Scholar]
- 47.Sanchez-Quintana D, Cabrera JA, Climent V, Farre J, Mendonca MC, Ho SY. Anatomic relations between the esophagus and left atrium and relevance for ablation of atrial fibrillation. Circulation. 2005;112:1400–5. doi: 10.1161/CIRCULATIONAHA.105.551291. [DOI] [PubMed] [Google Scholar]
- 48.Monnig G, Wessling J, Juergens KU, et al. Further evidence of a close anatomical relation between the oesophagus and pulmonary veins. Europace. 2005;7:540–5. doi: 10.1016/j.eupc.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 49.Good E, Oral H, Lemola K, et al. Movement of the esophagus during left atrial catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2005;46:2107–10. doi: 10.1016/j.jacc.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 50.Marine JE, Dong J, Calkins H. Catheter ablation therapy for atrial fibrillation. Prog Cardiovasc Dis. 2005;48:178–92. doi: 10.1016/j.pcad.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 51.Calkins H. Three dimensional mapping of atrial fibrillation: techniques and necessity. J Interv Card Electrophysiol. 2005;13:53–9. doi: 10.1007/s10840-005-2624-8. [DOI] [PubMed] [Google Scholar]
- 52.Moak J, Moore H, Lee S, et al. Case report: pulmonary vein stenosis following RF ablation of paroxysmal atrial fibrillation: successful treatement with balloon dilation. J Interv Card Electrophysiol. 2000;4:621–31. doi: 10.1023/a:1026573816874. [DOI] [PubMed] [Google Scholar]
- 53.Saad EB, Rossillo A, Saad CP, et al. Pulmonary vein stenosis after radiofrequency ablation of atrial fibrillation: functional characterization, evolution, and influence of the ablation strategy. Circulation. 2003;108:3102–7. doi: 10.1161/01.CIR.0000104569.96907.7F. [DOI] [PubMed] [Google Scholar]
- 54.Saad EB, Marrouche NF, Saad CP, et al. Pulmonary vein stenosis after catheter ablation of atrial fibrillation: emergence of a new clinical syndrome. Ann Intern Med. 2003;138:634–8. doi: 10.7326/0003-4819-138-8-200304150-00010. [DOI] [PubMed] [Google Scholar]
- 55.Scanvacca M, Kajita L, Vieira M, Sosa E. Pulmonary vein stenosis complicating catheter ablation of focal atrial fibrillation. J Cardiovasc Electrophysiol. 2000;1:677–81. doi: 10.1111/j.1540-8167.2000.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 56.Yang M, Akbari H, Reddy GP, Higgins CB. Identification of pulmonary vein stenosis after radiofrequency ablation for atrial fibrillation using MRI. J Comput Assist Tomagr. 2001;25:34–5. doi: 10.1097/00004728-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Arentz T, Jander N, von Rosenthal J, et al. Incidence of pulmonary vein stenosis 2 years after radiofrequency catheter ablation of refractory atrial fibrillation. Eur Heart J. 2003;24:963–9. doi: 10.1016/s0195-668x(03)00002-2. [DOI] [PubMed] [Google Scholar]
- 58.Taylor GW, Kay GN, Zheng X, Bishop S, Ideker RE. Pathological effects of extensive radiofrequency energy applications in the pulmonary veins in dogs. Circulation. 2000;101:1736–42. doi: 10.1161/01.cir.101.14.1736. [DOI] [PubMed] [Google Scholar]
- 59.Kluge A, Dill T, Ekinci O, et al. Decreased pulmonary perfusion in pulmonary vein stenosis after radiofrequency ablation: assessment with dynamic magnetic resonance perfusion imaging. Chest. 2004;126:428–37. doi: 10.1378/chest.126.2.428. [DOI] [PubMed] [Google Scholar]
- 60.Arentz T, Weber R, Jander N, et al. Pulmonary haemodynamics at rest and during exercise in patients with significant pulmonary vein stenosis after radiofrequency catheter ablation for drug resistant atrial fibrillation. Eur Heart J. 2005;26:1410–4. doi: 10.1093/eurheartj/ehi279. [DOI] [PubMed] [Google Scholar]
- 61.Qureshi AM, Prieto LR, Latson LA, et al. Transcatheter angioplasty for acquired pulmonary vein stenosis after radiofrequency ablation. Circulation. 2003;108:1336–42. doi: 10.1161/01.CIR.0000086322.21781.6A. [DOI] [PubMed] [Google Scholar]
- 62.Wylie J, Peters D, Essebag V, Manning W, Josephson M, Hauser T. Left atrial function and scar after catheter ablation of atrial fibrillation. Heart Rhythm. 2008;5:656–62. doi: 10.1016/j.hrthm.2008.02.008. [DOI] [PubMed] [Google Scholar]