Abstract
We have reported previously that thyroid hormone activates the circulating and tissue renin–angiotensin systems without involving the sympathetic nervous system, which contributes to cardiac hypertrophy in hyperthyroidism. This study examined whether the circulating or tissue renin–angiotensin system plays the principal role in hyperthyroidism-induced cardiac hypertrophy. The circulating renin–angiotensin system in Sprague–Dawley rats was fixed by chronic angiotensin II infusion (40 ng/ min, 28 days) via mini-osmotic pumps. Daily i.p. injection of thyroxine (0·1 mg/kg per day, 28 days) was used to mimic hyperthyroidism. Serum free tri-iodothyronine, plasma renin activity, plasma angiotensin II, cardiac renin and cardiac angiotensin II were measured with RIAs. The cardiac expression of renin mRNA was evaluated by semiquantitative reverse transcriptase-polymerase chain reaction. Plasma renin activity and plasma angiotensin II were kept constant in the angiotensin II and angiotensin II+thyroxine groups (0·12 ± 0·03 and 0·15 ± 0·03 μg/h per liter, 126 ± 5 and 130 ± 5 ng/l respectively) (means ± s.e.m.). Despite stabilization of the circulating renin–angiotensin system, thyroid hormone induced cardiac hypertrophy (5·0 ± 0·5 vs 3·5 ± 0·1 mg/g) in conjunction with the increases in cardiac expression of renin mRNA, cardiac renin and cardiac angiotensin II (74 ± 2 vs 48 ± 2%, 6·5 ± 0·8 vs 3·8 ± 0·4 ng/h per g, 231 ± 30 vs 149 ± 2 pg/g respectively). These results indicate that the local renin–angiotensin system plays the primary role in the development of hyperthyroidism-induced cardiac hypertrophy.
Introduction
Cardiac hypertrophy is a serious complication of hyperthyroidism (Shirani et al. 1993). The enhanced hemodynamics produced by increased activity of the sympathetic nervous system (SNS) is a major factor in the cardiac hypertrophy induced by hyperthyroidism (Klein 1990). Increased SNS activity also increases plasma renin activity (PRA) (Hauger-Klevene et al. 1972) following activation of the circulating renin–angiotensin system (RAS). There is evidence that circulating RAS may be involved in the development of cardiac hypertrophy (Morgan & Baker 1991). Angiotensin II (ANGII) exerts a direct physiological effect on the cardiovascular system via specific receptors on the cardiomyocyte plasma membrane that are coupled to guanine nucleotide-binding proteins (Baker et al. 1984, Baker & Singer 1988). The administration of angiotensin I-converting enzyme inhibitors is clinically efficacious in reducing cardiac hypertrophy (Dunn et al. 1984). We therefore hypothesized that activation of the circulating RAS might be involved in the development of the cardiac hypertrophy induced by hyperthyroidism. However, recent reports have shown that high PRA is present in hyperthyroidism but not hypothyroidism (Hauger-Klevene et al. 1972), and that SNS activity is elevated in both conditions (Polikar et al. 1990). While cardiac hypertrophy is induced by hyperthyroidism, cardiac hypertrophy is not induced by hypothyroidism (Heron & Rakusan 1994). These findings suggest that hyperthyroidism-induced cardiac hypertrophy is caused by factors other than changes in circulating RAS or SNS activity. Expression of the Ren-2 gene in the mouse submandibular gland is stimulated by thyroid hormone (Catanzaro et al. 1985, Karen & Morris 1986). In a pituitary cell line, thyroid hormone has been shown to regulate renin gene promoter activity (Gilbert et al. 1994), suggesting that thyroid hormone may regulate the expression of the tissue renin gene. We previously reported that thyroid hormone activates the circulating and tissue RAS without involving the SNS, and this may account for the cardiac hypertrophy observed in hyperthyroidism (Kobori et al. 1997b). However, it is uncertain which RAS dominates. This study examined the roles circulating or tissue RAS play in hyperthyroidism-induced cardiac hypertrophy.
Materials and Methods
Preparation of animals
The experiments were approved by the University Committee on Animal Care and Use of Keio University. Fifteen 6-week-old male Sprague–Dawley rats (Charles River, Kanagawa, Japan), 150−200 g, were used. They had free access to standard laboratory chow, containing 110 μmol/g sodium (Oriental Yeast, Tokyo, Japan), and tap water. They were individually housed in a room with a 12 h darkness–light cycle. Animals were divided into a control group, an ANGII group and an ANGII+thyroxine (T4) group. Continuous s.c. administration of ANGII (40 ng/min) for 28 days was given to the ANGII group and the ANGII+T4 group via mini-osmotic pumps (Alzet Model 2004, Alza Corporation, Palo Alto, CA, USA) to fix the circulating RAS. Saline was infused in the same manner in the control group. Daily i.p. injection of T4 (0·1 mg/kg per day) for 28 days was used to mimic hyperthyroidism in the ANGII+T4 group as we have previously described (Kobori et al. 1997a). Systolic blood pressure and heart rate were measured weekly using the tail-cuff method. Body weight was also determined weekly. Rats were killed by decapitation at day 28. Blood was collected, divided between two tubes with or without EDTA, separated into plasma and serum by centrifugation at 4 °C and stored at −20 °C. After blood was collected, the heart was removed immediately, washed in water free of ribonucleases, weighed, frozen in liquid nitrogen and stored at −20 °C until assayed.
Hormone measurements in serum and plasma
A commercially available RIA kit (Amarex-MAB Free T3, Ortho-Clinical Diagnostics, Tokyo, Japan) was used to determine the serum level of free tri-iodothyronine (T3). One half of the plasma was used to determine PRA with a commercially available RIA kit, according to the manufacturer's instructions (Renin-Riabead, Dainabot, Tokyo, Japan). The remaining plasma was used to determine the level of ANGII with a commercially available RIA kit, according to the manufacturer's instructions (Angiotensin II Radioimmunoassay Kit, Nichols Institute Diagnostics, San Juan Capistrano, CA, USA).
Hormone measurements in cardiac tissue
Frozen hearts were dissected into the four chambers. One-third of each chamber was used for each of the following measurements.
The first portion of each chamber was used to measure the cardiac level of renin as described previously (Kobori et al. 1997b). In brief, the heart was thawed and homogenized with a Polytron (Kinematica, Littau, Switzerland) in 10 ml buVer containing 2·6 mmol/l EDTA, 1·6 mmol/l dimercaprol, 3·4 mmol/l 8-hydroxyquinoline sulfate, 0·2 mmol/l phenylmethylsulfonyl fluoride and 5 mmol/l ammonium acetate. The homogenate was frozen and thawed four times, centrifuged at 20 000 g for 30 min at 4 °C and the supernatant removed. An aliquot of the supernatant was diluted 1:10. In addition, 0·5 ml plasma obtained from nephrectomized male rats was added to the same volume of diluted solution as a substrate for the enzymatic reaction. Renin activity was determined as in our previous study (Ichihara et al. 1995) using the Renin-Riabead assay. The cardiac level of renin was calculated using the formula: cardiac level of renin (ng of angiotensin I/h per g of heart)=renin activity (ng of angiotensin I/h per ml) × dilution rate (10 × 2=20) × volume of the buffer (10 ml)/weight of the aliquot of the heart assayed (g).
The second piece of each chamber was used for determination of the cardiac ANGII level as described previously (Kobori et al. 1997b). In brief, the heart was thawed and homogenized with a Polytron in 10 ml buffer that contained 0·1 mol/l HCl, which would inactivate endogenous tissue proteases. The homogenate was centrifuged at 20 000 g for 30 min at 4 °C and 1 ml of the supernatant was immediately applied to an octadecasilyl-silica solid phase extraction column (Sep-Pak Plus C18 cartridge, Millipore, Bedford, MA, USA). The concentration of ANGII in the sample was determined as described above. The cardiac level of ANGII was calculated using the formula: cardiac level of ANGII (pg/g of heart)=ANGII concentration (pg/ml) × volume of the buffer (10 ml)/weight of the aliquot of the heart assayed (g).
Semiquantitative reverse transcriptase-polymerase chain reaction (RT-PCR)
Semiquantitative RT-PCR was carried out as previously described (Kobori et al. 1997a,b, Ichihara et al. 1998). In brief, total RNA was extracted from the last piece of each heart chamber according to the manufacturer's instructions using the Total RNA Separator Kit (Clontech, Palo Alto, CA, USA). The extracted RNA was suspended in ribonuclease-free water and quantified by measuring the absorbance at 260 nm.
Total RNA from each heart was reverse transcribed using the GeneAmp RNA PCR Core Kit (Perkin Elmer, Norwalk, CT, USA) according to the manufacturer's instructions.
Oligonucleotide primers were designed from the published cDNA sequences of renin (Tada et al. 1988) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (Tso et al. 1985). GAPDH was used as an internal standard. The sequences of the renin primers were sense 5′-TGCCACCTTGTTGTGTGAGG-3′ (exon 7 bases 851−870) and antisense 5′-ACCCGATGCGATTGTTA TGCCG-3′ (exon 9 bases 1203−1224). The sequences of the GAPDH primers were sense 5′-TCCCTCAAGA TTGTCAGCAA-3′ (bases 492−511) and antisense 5′-AGATCCACAACGGATACATT-3′ (bases 780−799). The expected sizes of the amplified renin and GAPDH PCR products are 374 and 308 bp respectively. The sense primers in each reaction were radiolabeled with [γ-32P]ATP (Amersham, Amersham, Bucks, UK) and T4 polynucleotide kinase using the Kination Kit (Toyobo, Osaka, Japan).
Five μl of the RT mixture were used for amplification. Each reaction contained 25 nmol MgCl2, 1000 nmol KCl, 200 nmol Tris–HCl (pH 8·3), 3·75 pmol and 106 c.p.m. of each sense primer, 3·75 pmol of each antisense primer and 0·625 U AmpliTaq DNA polymerase. To minimize nonspecific amplification, we used a ‘hot start’ procedure in which PCR samples were placed in a thermocycler (DNA Thermal Cycler 480, Perkin Elmer) prewarmed to 94 °C. After 2 min, PCR was performed for 35 cycles using a 30 s denaturation step at 94 °C, a 1 min annealing step at 57 °C and a 1 min 15 s extension step at 72 °C. We added a final 5 min extension step at 72 °C. After completion of RTPCR, DNA was electrophoresed on an 8% (weight/volume) polyacrylamide gel. Gels were dried on filter paper and then exposed to a BAS 2000 imaging plate (Fuji Film, Tokyo, Japan) for 1 min and quantified with a BAS 2000 Laser Image Analyzer (Fuji Film) (Amemiya & Miyahara 1988, Itohara et al. 1990). Renin mRNA expression was evaluated as the renin/GAPDH ratio, because the levels of GAPDH did not differ between the groups.
Statistical analysis
The data are presented as mean ± s.e.m. To compare multiple groups, we used one-way factorial ANOVA with post hoc Scheffe's F test to evaluate the significance of the differences. P<0·01 was considered statistically significant.
Results
Effects of administration of saline and ANGII
As shown in Table 1, ANGII infusion increased the ratio of heart weight to body weight, systolic blood pressure, plasma ANGII and cardiac ANGII. PRA, cardiac renin mRNA (Fig. 1) and cardiac renin were suppressed by chronic ANGII administration. As shown in Table 1, there was no difference in serum free T3 level and heart rate between the control group and the ANGII group.
Table 1.
Changes in parameters produced by ANGII and T4 treatment. The data are expressed as mean ± S.E.M., n=5
|
Control |
ANGII |
ANGII +T4 |
|
|---|---|---|---|
| Parameters/groups | |||
| Serum free T3 (ng/l) | 2·1 ± 0·1 | 2·3 ± 0·2 | 6·6 ± 0·3† |
| Heart weight/body weight (mg/g) | 2·9 ± 0·2 | 3·5 ± 0·1* | 5·0 ± 0·5† |
| Systolic blood pressure (mmHg) | 106 ± 3 | 176 ± 6* | 180 ± 4 |
| Heart rate (beats/min) | 324 ± 21 | 348 ± 12 | 446 ± 13† |
| PRA (μg angiotensin I/h/l) | 5·48 ± 1·17 | 0·12 ± 0·03* | 0·15 ± 0·03 |
| Plasma ANGII (ng/l) | 37 ± 3 | 126 ± 5* | 130 ± 5 |
| Renin/GAPDH mRNA (% ratio) | 61 ± 2 | 48 ± 2* | 74 ± 2† |
| Cardiac renin (ng angiotensin I/h/g) | 10·0 ± 0·8 | 3·8 ± 0·4* | 6·5 ± 0·8† |
| Cardiac ANGII (pg/g) | 83 ± 13 |
149 ± 2* |
231 ± 30† |
P<0·01 vs control group;
P<0·01 vs ANGII group.
Figure 1.
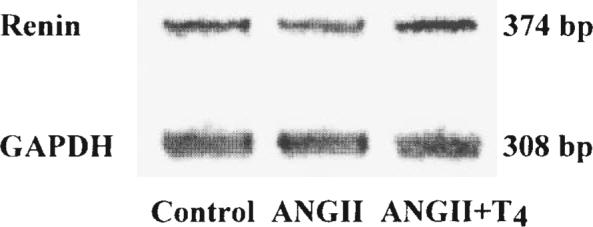
A representative electrophoretogram showing the effect of ANGII and T4 on renin and GAPDH mRNA levels.
Effects of administration of ANGII and T4
As shown in Table 1, PRA and plasma ANGII were fixed in the ANGII group and the ANGII+T4 group. Serum free T3 levels rose significantly after i.p. administration of T4 in the ANGII+T4 group vs the ANGII group.
Table 1 shows that the ratio of heart weight to body weight increased significantly in the ANGII+T4 group compared with the ANGII group. As shown in Table 1, there was no difference in systolic blood pressure between the ANGII group and the ANGII+T4 group. Heart rate increased significantly in the ANGII+T4 group compared with the ANGII group.
As shown in Table 1 and Fig. 1, semiquantitative RT-PCR of total heart RNA showed that renin mRNA levels were elevated in rats treated with T4.
Table 1 shows that the cardiac levels of renin and ANGII were increased significantly in the ANGII+T4 group compared with the ANGII group.
Discussion
Similar to the findings of Von Thun et al. (1994b), chronic infusion of ANGII significantly increased systolic blood pressure, plasma ANGII and tissue ANGII. In contrast, PRA, tissue levels of renin and tissue expression of renin mRNA were suppressed by ANGII administration, and this is also consistent with previous work (Von Thun et al. 1994a,b). In spite of the suppression in cardiac expression of renin mRNA and cardiac renin, cardiac hypertrophy was induced by ANGII infusion in conjunction with the increase in cardiac ANGII. These results imply that chronic ANGII infusion induces cardiac hypertrophy through renin-independent augmentation of cardiac ANGII. However, in vitro studies are needed for the clarification of the more precise mechanism by which ANGII administration induces cardiac hypertrophy.
Administration of T4 for 28 days significantly increased the serum level of free T3 and was considered effective in mimicking hyperthyroidism in this model. Administration of ANGII for 28 days reduced PRA to lower limits in both groups, and plasma ANGII was not different between the two groups. In our previous study, T4 administration increased PRA and plasma ANGII (Kobori et al. 1997b). Therefore, administration of ANGII was effective in stabilizing PRA and plasma ANGII and removing circulating RAS as a variable in this model.
Systolic blood pressure was not different between the two groups; however, cardiac hypertrophy was observed only in the ANGII+T4 group in accord with the increase in expression of cardiac renin mRNA, cardiac renin and cardiac ANGII. These results indicate that thyroid hormone activates the cardiac RAS independently of the circulating RAS via enhancement of renin mRNA expression.
Since the RAS was first described, it has been characterized as a circulating neuroendocrine system (Davis & Freeman 1976). Recent cardiovascular research has determined that the RAS is more complicated than originally thought, and that it is a local tissue system as well as a circulating endocrine system (Dzau 1993, Raman et al. 1995). Some studies showed that activation of the cardiac RAS, and not the circulating RAS, produced cardiac hypertrophy in a pressure-overload model (Bruckschlegel et al. 1995) and in a volume-overload model (Ruzicka et al. 1993). In our model, the local RAS was found to play the primary role in cardiac hypertrophy.
Bedotto et al. (1989) and Garcia del Rio et al. (1997) demonstrated that an angiotensin I-converting enzyme inhibitor, captopril, inhibited circulating RAS and failed to prevent cardiac hypertrophy in T4-induced hyper-thyroid rats. These results apparently conflict with our hypothesis. In other words, captopril suppressed circulating RAS; however, it did not completely inhibit cardiac RAS. Because the activation of local RAS is important in T4-induced cardiac hypertrophy, captopril does not prevent cardiac hypertrophy in a T4-induced model. However, we cannot assess the more precise mechanism because we did not use captopril in this present study.
In other experimental models, local RAS has been shown to play a more prominent role than circulating RAS. Zou et al. (1996) recently reported that renal accumulation of circulating ANGII induces hypertension in ANGII-infused rats. Sigmund et al. (1997) recently demonstrated in transgenic mice that selective activation of an intrinsic intrarenal RAS results in hypertension via a renal ANGII-dependent but plasma ANGII-independent mechanism. In the same manner, the activation of local RAS generates cardiac hypertrophy in our hyperthyroid rat model. Development of a more specific inhibitor of local RAS will help clarify these mechanisms.
It is obvious that cardiac hypertrophy in the ANGII+T4 group is modulated by ANGII-induced hypertension and tachycardia. Strictly speaking, cardiac hypertrophy in the ANGII+T4 group may be different from hyperthyroidism-induced cardiac hypertrophy. However, thyroid hormone has an independent effect on cardiac hypertrophy, since the ratio of heart weight to body weight increased significantly in the ANGII+T4 group compared with the ANGII group.
Segal (1990) reported that thyroid hormone induced uptake of calcium by the heart as an acute effect, which would then increase myocardial contractility. Ojamaa et al. (1992) demonstrated that thyroid hormone upregulated the expression of the myosin heavy chain genes. Thomas et al. (1993) showed that insulin-like growth factor-I produced cardiac hypertrophy, as well as endocrine and cardiac paracrine effects, during hyperthyroidism. Based on these previous literature reports, it seems likely that the animal model of hyperthyroidism-induced cardiac hypertrophy is in fact multi-factorial in its mechanistic nature.
In conclusion, the present study showed that thyroid hormone directly enhances the cardiac expression of renin mRNA independent of the circulating RAS. The cardiac levels of renin and ANGII both increased, and cardiac hypertrophy developed. It appears that thyroid hormone enhances the cardiac RAS via an increase in the expression of renin mRNA. Our findings indicate that hyper-thyroidism leads to cardiac hypertrophy via the activation of the cardiac RAS rather than by activation of the circulating RAS. The local RAS contributes to hyperthyroidism-induced cardiac hypertrophy.
Acknowledgements
This work was supported in part by Grant(s)-in-Aid for Scientific Research from the Ministry of Education, Science and Culture, Japan (Nos 08770511, 09770500), a Grant-in-Aid from Keio University for the Promotion of Science and a Young Investigator Prize for Encouragement from Keio University.
References
- Amemiya Y, Miyahara J. Imaging plate illuminates many fields. Nature. 1988;336:89–90. doi: 10.1038/336089a0. [DOI] [PubMed] [Google Scholar]
- Baker KM, Singer HA. Identification and characterization of guinea pig angiotensin II ventricular and atrial receptors: coupling to inositol phosphate production. Circulation Research. 1988;62:896–904. doi: 10.1161/01.res.62.5.896. [DOI] [PubMed] [Google Scholar]
- Baker KM, Campanile CP, Trachte GJ, Peach MJ. Identification and characterization of the rabbit angiotensin II myocardial receptor. Circulation Research. 1984;54:286–293. doi: 10.1161/01.res.54.3.286. [DOI] [PubMed] [Google Scholar]
- Bedotto JB, Gay RG, Graham SD, Morkin E, Goldman S. Cardiac hypertrophy induced by thyroid hormone is independent of loading conditions and beta adrenoceptor blockade. Journal of Pharmacology and Experimental Therapeutics. 1989;248:632–636. [PubMed] [Google Scholar]
- Bruckschlegel G, Holmer SR, Jandeleit K, Grimm D, Muders F, Kromer EP, Riegger GA, Schunkert H. Blockade of the renin–angiotensin system in cardiac pressure-overload hypertrophy in rats. Hypertension. 1995;25:250–259. doi: 10.1161/01.hyp.25.2.250. [DOI] [PubMed] [Google Scholar]
- Catanzaro DF, Mesterovic N, Morris BJ. Studies of the regulation of mouse renin genes by measurement of renin messenger ribonucleic acid. Endocrinology. 1985;117:872–878. doi: 10.1210/endo-117-3-872. [DOI] [PubMed] [Google Scholar]
- Davis JO, Freeman RH. Mechanisms regulating renin release. Physiological Reviews. 1976;56:1–56. doi: 10.1152/physrev.1976.56.1.1. [DOI] [PubMed] [Google Scholar]
- Dunn FG, Oigman W, Ventura HO, Messerli FH, Kobrin I, Frohlich ED. Enalapril improves systemic and renal hemodynamics and allows regression of left ventricular mass in essential hypertension. American Journal of Cardiology. 1984;53:105–108. doi: 10.1016/0002-9149(84)90692-1. [DOI] [PubMed] [Google Scholar]
- Dzau VJ. Tissue renin–angiotensin system in myocardial hypertrophy and failure. Archives of Internal Medicine. 1993;153:937–942. [PubMed] [Google Scholar]
- Garcia del Rio C, Moreno MR, Osuna A, de Dios Luna J, Garcia-Estan J, Vargas F. Role of the renin–angiotensin system in the development of thyroxine-induced hypertension. European Journal of Endocrinology. 1997;136:656–660. doi: 10.1530/eje.0.1360656. [DOI] [PubMed] [Google Scholar]
- Gilbert MT, Sun J, Yan Y, Oddoux C, Lazarus A, Tansey WP, Lavin TN, Catanzaro DF. Renin gene promoter activity in GC cells is regulated by cAMP and thyroid hormone through Pit-1-dependent mechanisms. Journal of Biological Chemistry. 1994;269:28049–28054. [PubMed] [Google Scholar]
- Hauger-Klevene JH, Brown H, Zavaleta J. Plasma renin activity in hyper- and hypothyroidism: effect of adrenergic blocking agents. Journal of Clinical Endocrinology and Metabolism. 1972;34:625–629. doi: 10.1210/jcem-34-4-625. [DOI] [PubMed] [Google Scholar]
- Heron MI, Rakusan K. Geometry of coronary capillaries in hyperthyroid and hypothyroid rat heart. American Journal of Physiology. 1994;267:H1024–H1031. doi: 10.1152/ajpheart.1994.267.3.H1024. [DOI] [PubMed] [Google Scholar]
- Ichihara A, Suzuki H, Murakami M, Naitoh M, Matsumoto A, Saruta T. Interactions between angiotensin II and norepinephrine on renin release by juxtaglomerular cells. European Journal of Endocrinology. 1995;133:569–577. doi: 10.1530/eje.0.1330569. [DOI] [PubMed] [Google Scholar]
- Ichihara A, Kobori H, Miyashita Y, Hayashi M, Saruta T. Differential effects of thyroid hormone on renin secretion, content, and mRNA in juxtaglomerular cells. American Journal of Physiology. 1998;274:E224–E231. doi: 10.1152/ajpendo.1998.274.2.e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itohara S, Farr AG, Lafaille JJ, Bonneville M, Takagaki Y, Haas W, Tonegawa S. Homing of a gamma delta thymocyte subset with homogeneous T-cell receptors to mucosal epithelia. Nature. 1990;343:754–757. doi: 10.1038/343754a0. [DOI] [PubMed] [Google Scholar]
- Karen P, Morris BJ. Stimulation by thyroid hormone of renin mRNA in mouse submandibular gland. American Journal of Physiology. 1986;251:E290–E293. doi: 10.1152/ajpendo.1986.251.3.E290. [DOI] [PubMed] [Google Scholar]
- Klein I. Thyroid hormone and the cardiovascular system. American Journal of Medicine. 1990;88:631–637. doi: 10.1016/0002-9343(90)90531-h. [DOI] [PubMed] [Google Scholar]
- Kobori H, Ichihara A, Suzuki H, Miyashita Y, Hayashi M, Saruta T. Thyroid hormone stimulates renin synthesis in rats without involving the sympathetic nervous system. American Journal of Physiology. 1997a;272:E227–E232. doi: 10.1152/ajpendo.1997.272.2.E227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Ichihara A, Suzuki H, Takenaka T, Miyashita Y, Hayashi M, Saruta T. Role of the renin–angiotensin system in cardiac hypertrophy induced in rats by hyperthyroidism. American Journal of Physiology. 1997b;273:H593–H599. doi: 10.1152/ajpheart.1997.273.2.H593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan HE, Baker KM. Cardiac hypertrophy: mechanical, neural, and endocrine dependence. Circulation. 1991;83:13–25. doi: 10.1161/01.cir.83.1.13. [DOI] [PubMed] [Google Scholar]
- Ojamaa K, Samarel AM, Kupfer JM, Hong C, Klein I. Thyroid hormone eVects on cardiac gene expression independent of cardiac growth and protein synthesis. American Journal of Physiology. 1992;263:E534–E540. doi: 10.1152/ajpendo.1992.263.3.E534. [DOI] [PubMed] [Google Scholar]
- Polikar R, Kennedy B, Ziegler M, O'Connor DT, Smith J, Nicod P. Plasma norepinephrine kinetics, dopamine-beta-hydroxylase, and chromogranin-A, in hypothyroid patients before and following replacement therapy. Journal of Clinical Endocrinology and Metabolism. 1990;70:277–281. doi: 10.1210/jcem-70-1-277. [DOI] [PubMed] [Google Scholar]
- Raman VK, Lee YA, Lindpaintner K. The cardiac renin–angiotensin–aldosterone system and hypertensive cardiac hypertrophy. American Journal of Cardiology. 1995;76:18D–23D. doi: 10.1016/s0002-9149(99)80487-1. [DOI] [PubMed] [Google Scholar]
- Ruzicka M, Yuan B, Harmsen E, Leenen FH. The renin–angiotensin system and volume overload-induced cardiac hypertrophy in rats. EVects of angiotensin converting enzyme inhibitor versus angiotensin II receptor blocker. Circulation. 1993;87:921–930. doi: 10.1161/01.cir.87.3.921. [DOI] [PubMed] [Google Scholar]
- Segal J. Calcium is the first messenger for the action of thyroid hormone at the level of the plasma membrane: first evidence for an acute eVect of thyroid hormone on calcium uptake in the heart. Endocrinology. 1990;126:2693–2702. doi: 10.1210/endo-126-5-2693. [DOI] [PubMed] [Google Scholar]
- Shirani J, Barron MM, Pierre-Louis ML, Roberts WC. Congestive heart failure, dilated cardiac ventricles, and sudden death in hyperthyroidism. American Journal of Cardiology. 1993;72:365–368. doi: 10.1016/0002-9149(93)90691-5. [DOI] [PubMed] [Google Scholar]
- Sigmund CD, Ding Y, Hardy DO, Zhu L, Catterall JF, Davisson RL. Selective activation of an intrinsic intrarenal renin–angiotensin system results in hypertension via a renal Ang-II-dependent but plasma Ang-II-independent mechanism in transgenic mice. Journal of the American Society of Nephrology. 1997;8:308. [Google Scholar]
- Tada M, Fukamizu A, Seo MS, Takahashi S, Murakami K. Nucleotide sequence of rat renin cDNA. Nucleic Acids Research. 1988;16:3576. doi: 10.1093/nar/16.8.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas MR, Miell JP, Taylor AM, Ross RJ, Arnao JR, Jewitt DE, McGregor AM. Endocrine and cardiac paracrine actions of insulin-like growth factor-I (IGF-I) during thyroid dysfunction in the rat: is IGF-I implicated in the mechanism of heart weight/body weight change during abnormal thyroid function? Journal of Molecular Endocrinology. 1993;10:313–323. doi: 10.1677/jme.0.0100313. [DOI] [PubMed] [Google Scholar]
- Tso JY, Sun XH, Kao TH, Reece KS, Wu R. Isolation and characterization of rat and human glyceraldehyde-3-phosphate dehydrogenase cDNAs: genomic complexity and molecular evolution of the gene. Nucleic Acids Research. 1985;13:2485–2502. doi: 10.1093/nar/13.7.2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Thun AM, El-Dahr SS, Vari RC, Navar LG. Modulation of renin–angiotensin and kallikrein gene expression in experimental hypertension. Hypertension. 1994a;23:I131–I136. doi: 10.1161/01.hyp.23.1_suppl.i131. [DOI] [PubMed] [Google Scholar]
- Von Thun AM, Vari RC, El-Dahr SS, Navar LG. Augmentation of intrarenal angiotensin II levels by chronic angiotensin II infusion. American Journal of Physiology. 1994b;266:F120–F128. doi: 10.1152/ajprenal.1994.266.1.F120. [DOI] [PubMed] [Google Scholar]
- Zou L-X, Hymel A, Imig JD, Navar LG. Renal accumulation of circulating angiotensin II in angiotensin II-infused rats. Hypertension. 1996;27:658–662. doi: 10.1161/01.hyp.27.3.658. [DOI] [PubMed] [Google Scholar]


