Abstract
Hendra virus (HeV) is a member of the broadly tropic and highly pathogenic paramyxovirus genus Henipavirus. HeV is enveloped and infects cells by using membrane-anchored attachment (G) and fusion (F) glycoproteins. G possesses an N-terminal cytoplasmic tail, an external membrane-proximal stalk domain, and a C-terminal globular head that binds the recently identified receptors ephrinB2 and ephrinB3. Receptor binding is presumed to induce conformational changes in G that subsequently trigger F-mediated fusion. The stalk domains of other attachment glycoproteins appear important for oligomerization and F interaction and specificity. However, this region of G has not been functionally characterized. Here we performed a mutagenesis analysis of the HeV G stalk, targeting a series of isoleucine residues within a hydrophobic α-helical domain that is well conserved across several attachment glycoproteins. Nine of 12 individual HeV G alanine substitution mutants possessed a complete defect in fusion-promotion activity yet were cell surface expressed and recognized by a panel of conformation-dependent monoclonal antibodies (MAbs) and maintained their oligomeric structure. Interestingly, these G mutations also resulted in the appearance of an additional electrophoretic species corresponding to a slightly altered glycosylated form. Analysis revealed that these G mutants appeared to adopt a receptor-bound conformation in the absence of receptor, as measured with a panel of MAbs that preferentially recognize G in a receptor-bound state. Further, this phenotype also correlated with an inability to associate with F and in triggering fusion even after receptor engagement. Together, these data suggest the stalk domain of G plays an important role in the conformational stability and receptor binding-triggered changes leading to productive fusion, such as the dissociation of G and F.
Hendra virus (HeV) and Nipah virus (NiV) are two newly emergent zoonotic viruses which currently comprise their own genus, Henipavirus, within the family Paramyxoviridae. The principal reservoirs for both viruses appear to be several species of pteropid fruit bats, which as a group cover a broad geographic range over Southeast Asia and the Pacific (reviewed in references 19 and 21). HeV appeared first in Australia in 1994 in two nearly simultaneous yet unrelated episodes of severe respiratory disease in horses and consequent transmissions to three people, two of which resulted in death (reviewed in reference 19). HeV has reemerged in Australia, causing fatal infections of horses in 1999 (20), 2004 (2), 2006 (33), and most recently in 2008 (3). A single human infection occurred in a veterinarian who recovered with seroconversion after conducting the necropsy on the horse in 2004 (25), and as of August 2008 several horses have been confirmed infected along with two people. NiV was first recognized in 1997 to 1998 in an outbreak of encephalitis among pig farmers in Malaysia and Singapore. This outbreak was considerably larger than that of the initial HeV episode, with 265 cases of human infection and 105 deaths, and it was primarily transmitted to humans from infected pigs (reviewed in reference 14). Since then, NiV has also continued to reemerge, causing several deadly spillover events. Most recently, outbreaks of NiV have been associated with an increased case fatality rate (approaching 75%), direct transmission from bat reservoirs, and human-to-human transmission (4, 13, 24, 26). Together, these features of HeV and NiV, along with their broad host ranges and their presence in natural reservoirs, have made them a significant biological threat. There are presently no approved antiviral therapeutics to treat HeV or NiV infection, and they are presently classified as biosafety level 4 pathogens (reviewed in reference 19).
Paramyxoviruses possess two major membrane-anchored glycoproteins in the envelope of the viral particle. One glycoprotein is required for virion attachment to receptors on host cells and is designated as either hemagglutinin-neuraminidase protein (HN) or hemagglutinin protein (H), and the other is glycoprotein (G), which has neither hemagglutination nor neuraminidase activities (28). The attachment glycoproteins are type II membrane proteins, where the molecule's amino (N) terminus is oriented toward the cytoplasm and the protein's carboxy (C) terminus is extracellular. The other major glycoprotein is the fusion (F) glycoprotein, which is a trimeric class I fusogenic envelope glycoprotein containing two heptad repeat (HR) regions and a hydrophobic fusion peptide. HeV and NiV infect cells though a pH-independent membrane fusion process into receptive host cells through the concerted action of their G attachment glycoprotein and F following receptor binding. In nearly all cases, the coexpression of typically its homologous viral species attachment glycoprotein is required along with F for efficient membrane fusion (reviewed in reference 7). Upon triggering, F undergoes significant conformational rearrangements that facilitate the insertion of the fusion peptide into target membranes, bringing the two HR regions together in the formation of the six-helix bundle structure or trimer-of-hairpins during or immediately following fusion of virus and cell membranes (recently reviewed in reference 29). Several molecular details of the substantial conformational change of F upon triggering have been revealed in the recent structural solutions of both post- and prefusion conformations of F (48, 49). The primary function of the paramyxovirus attachment protein is to engage appropriate receptors on the surfaces of host cells, which for the majority of well-characterized paramyxoviruses are sialic acid moieties. However, the HeV and NiV G glycoproteins utilize the host cell protein receptors ephrinB2 and/or ephrinB3 (5, 6, 34, 35).
For some paramyxoviruses, receptor binding is believed to trigger conformational changes in the attachment protein, which in turn is thought to serve as the trigger of the F glycoprotein's fusogenic activity (reviewed in reference 7). This function of the attachment glycoprotein is typically termed its fusion promotion activity. The molecular details of this process have yet to be clarified, and although this is a favored model by many, the influence of receptor binding on the conformation of a paramyxovirus attachment glycoprotein and its role in facilitating F-mediated fusion remains controversial, and these studies have primarily been carried out with HN glycoproteins which employ sialic acid receptors. Conformational changes in the HN glycoprotein were detected in the case of Newcastle disease virus (NDV) HN when its structures alone and in complex with the inhibitor 2-deoxy-2,3-dehydro-N-acetylneuraminic acid (Neu5Ac2en) were solved and compared (41), whereas no major conformational changes in the parainfluenza virus 5 (formerly known as simian virus 5) HN were noted between uncomplexed and receptor-complexed structures (51). In addition to the receptor binding and fusion promotion functions described above, many paramyxovirus attachment proteins also possess hemagglutination or both hemagglutination and neuraminidase activities, classifying them as either H or HN, respectively (reviewed in reference 7).
The HeV and NiV G glycoproteins are similar in structure (11, 47), and both share common features with other paramyxovirus attachment glycoproteins, including the conservation of cysteine residues, a six-bladed β-propeller structure of the globular head domain, and an α-helical stalk or stem domain (46, 50). Further underscoring these basic structural similarities, amino acid residues within the head domain of NiV and HeV G important for receptor binding have been identified through site-directed mutagenesis (5, 23), and contact residues for ephrinB2 and ephrinB3 interaction have been identified through structural analysis (11, 47).
The paramyxovirus attachment glycoproteins are multifunctional molecules. For the HN glycoproteins both receptor binding activity and the neuraminidase active site are localized to the globular head domain, as with human parainfluenza virus 3 (hPIV-3) and NDV HN (10, 16, 30, 52). In addition to receptor binding and specificity, the attachment glycoproteins also possess the fusion promotion activity and specificity for the F glycoprotein. However, elucidation of the domain(s) of the attachment glycoprotein that is directly responsible for F-interaction and/or F-specificity has been less clear, with various studies implicating either the stalk domain (18, 31, 39, 40, 42) or areas in both the stalk domain and the globular head domain (43). In addition, the stalk domain has been shown to be important for dimer formation in the case of measles virus (MeV) H (37), critical for neuraminidase activity for HN (17, 44), and involved in maintenance of the antigenic structure of HN (17).
Within the stalk domain reside a series of hydrophobic isoleucine, leucine, and valine residues which are very well conserved among the various members of the subfamily Paramyxovirinae and which have been hypothesized to form heptad repeat-like structure(s) similar to those found in the F glycoprotein. Previous work by Stone-Hulslander et al. (40) and by Wang et al. (44) found that mutation of some of these residues in the stalk region to alanine impaired NDV HN′s fusion promotion ability and neuraminidase activity, respectively. Another study, by Melanson et al., found that mutation of two residues within this domain of NDV HN, L90 and L94, resulted in decreased fusion and decreased F interaction, without resulting in decreased neuraminidase activity (32). In the present study, we identified analogous residues within the stalk domain of HeV G and assessed the effects of mutation of these residues to alanine on the glycoprotein's various functional activities. Although all of the mutant G glycoproteins were expressed relatively normally and at the cell surface, could bind viral receptors, and were recognized by a panel of conformationally dependent monoclonal antibodies (MAbs), the majority (9 of 12) of mutants had completely lost their ability to promote cell fusion when coexpressed with F. This loss of fusion promotion activity did not correlate to G oligomerization but did correlate to an inability to interact with F. Further analysis revealed that the mutants appeared to adopt a post-receptor-binding conformation in the absence of receptor as measured by differential MAb binding reactivities.
These data suggest an important role for the stalk domain of the G attachment glycoprotein in maintenance of its conformation and potentially also in the receptor binding-triggered changes leading to productive fusion, such as the dissociation of G and F. The data also demonstrate that conformational changes in the globular head domain of G that are associated with receptor binding can be caused by mutation of certain residues within the stalk and suggest that triggering these conformational changes prematurely can prevent F and G complex formation, resulting in a loss of fusion promotion activity. Our studies highlight a role for receptor-induced conformational changes in the attachment glycoprotein within a model of paramyxovirus fusion protein (F) activity regulated by the G protein.
(K. A. Bishop performed this work as partial fulfillment of the requirements of the Ph.D. program in Emerging Infectious Diseases of the Uniformed Services University of the Health Sciences.)
MATERIALS AND METHODS
Cells and culture conditions.
HeLa-USU cells and PCI-13 cells have been described previously (6, 9). 293T cells were obtained from G. Quinnan (Uniformed Services University). HeLa-USU and 293T cells were maintained in Dulbecco's modified Eagle's medium (Quality Biologicals, Gaithersburg, MD) supplemented with 10% cosmic calf serum (CCS; HyClone, Logan, UT) and 2 mM l-glutamine (DMEM-10). PCI-13 cells were maintained in DMEM-10 plus 100 mM HEPES buffer. All cell cultures were maintained at 37°C in 5% CO2.
Amino acid sequence alignments.
Amino acid sequences for the following proteins were obtained from GenBank and utilized in alignments (accession numbers in parentheses): Sendai virus HN (AB005795), canine distemper virus HN (AF014953, L13194, and L13195), MuV HN (AB040874), MeV H (AB016162), hPIV-3 HN (AB012132), hPIV-2 HN (X57559), hPIV-1 HN (AF457102), and NDV HN (AF309418), along with the amino acid sequences for our HeV and NiV G clones. Global protein alignments were created with Clone Manager software (Scientific and Educational Software, Cary, NC) using a Blosum 62 scoring matrix.
G glycoprotein constructs and mutagenesis.
Conversion of specific residues of HeV G to alanine or glutamine was performed via site-directed mutagenesis using the QuikChange II site-directed mutagenesis kit (Stratagene, Cedar Creek, TX). The template for the reactions consisted of a C-terminal myc epitope-tagged version of HeV G in the vaccinia virus-based plasmid pMCO2 (12). All mutation-containing construct sequences were verified.
Metabolic labeling and immunoprecipitations.
Subconfluent HeLa-USU cells were transfected with the various alanine mutation-containing Gs or wild-type G using the Fugene-6 transfection reagent (Roche, Indianapolis, IN). Cells were transfected with 3 μg total DNA per T-25 flask overnight followed by infection with wild-type vaccinia virus (strain WR) at a multiplicity of infection of 10. At 6 h postinfection, the cells were washed and incubated overnight with methionine- and cysteine-free minimum essential medium (Invitrogen) containing 2.5% dialyzed fetal calf serum (Invitrogen), l-glutamine, and 100 μCi per ml of [35S]methionine-cysteine (Promix; Amersham Pharmacia Biotech, Piscataway, NJ). Approximately 16 h later, the cells were chased with complete medium for 2 h, and cell lysates were prepared using lysis buffer (100 mM Tris-HCl [pH 8.0], 100 mM NaCl, and 1% Triton X-100), clarified by centrifugation, and analyzed by immunoprecipitation and sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) followed by autoradiography. Immunoprecipitated proteins were quantified by spot densitometry using AlphaEase Fc software (Alpha Innotech, San Leandro, CA). For MAb binding, calculations of the percentage of wild-type (WT) reactivity values make use of integrated density values (IDVs) generated from scanned films in the program AlphaEase Fc. The amount of each mutant G immunoprecipitated by a given antibody is measured by determining a ratio that takes into account total expression levels using the following calculation: [(IDV of mutant bands immunoprecipitated with MAb)/(IDV of mutant bands immunoprecipitated with polyclonal antiserum)]/[(IDV of WT bands immunoprecipitated with MAb)/(IDV of WT bands immunoprecipitated with polyclonal antiserum)] × 100.
For coprecipitations of G with receptor, G-containing cell lysates were incubated with 3 μg human ephrinB3/FC (R&D Systems, Minneapolis, MN) or human EFNB2/s-tag (5) followed by precipitation with either protein G-Sepharose (Amersham) or protein S-agarose (EMD Biosciences Inc, Madison, WI), respectively. For immunoprecipitations with G-specific antibodies, 4 μl of a polyclonal antiserum, 3 μg purified MAb, or 5 μl concentrated hybridoma supernatant was incubated with G-containing lysate at 4°C for 1 h or overnight. Samples were washed twice with lysis buffer followed by one wash with 100 mM Tris-HCl (pH 8.0), 100 mM NaCl, 0.1% sodium deoxycholate, and 0.1% SDS (DOC wash buffer). Samples were boiled in sample buffer with 2-mercaptoethanol, analyzed by SDS-PAGE, visualized by autoradiography or Western blotting, and quantified by densitometry.
For coprecipitation assays of G with F glycoproteins, the F- and G-encoding plasmids were cotransfected into HeLa-USU cells. Cells were then infected, and 16 to 18 h later, cell lysates were prepared as described above. Equivalent amounts of each lysate were precleared with protein G-Sepharose for 45 min at room temperature and then incubated at 4°C overnight with 5 μl rabbit polyclonal F1-specific antiserum or 5 μl rabbit polyclonal G-specific antiserum and then precipitated with protein G-Sepharose, washed, and boiled with 2-mercaptoethanol as described above, before being analyzed by SDS-PAGE and Western blotting under reducing conditions with mouse polyclonal G-specific antiserum at 1:20,000.
Cell fusion assays.
Fusion between F and G glycoprotein-expressing effector cells and permissive target cells was measured in a reporter gene assay in which the cytoplasm of one cell population contained vaccinia virus-encoded T7 RNA polymerase and the cytoplasm of the other contained the Escherichia coli lacZ gene linked to the T7 promoter; β-galactosidase (β-Gal) is synthesized only in fused cells (8, 36). Plasmids encoding HeV F and each alanine mutant of G or no DNA (control/mock transfection) were transfected into HeLa-USU cells and allowed to express overnight as described above. 293T cells or PCI-13 cells served as receptor-positive target cells. Vaccinia virus-encoded proteins were produced by infecting cells at a multiplicity of infection of 10 and incubating infected cells at 31°C overnight. Cell fusion reactions were conducted with the various cell mixtures in 96-well plates at 37°C or at 42°C. The ratio of envelope glycoprotein-expressing cells to target cells was 1:1 (2 × 105 total cells per well; 0.2-ml total volume). Cytosine arabinoside (40 μg/ml) was added to the fusion reaction mixture to reduce nonspecific β-Gal production (8). For quantitative analyses, Nonidet P-40 alternative was added (0.5% final) at 2.5 or 3.0 h, and aliquots of the lysates were assayed for β-Gal at ambient temperature with the substrate chlorophenol red-d-galactopyranoside (Roche Diagnostics Corp.). Assays were performed in duplicate, and fusion results were calculated and expressed as rates of β-Gal activity (change in optical density at 570 nm per minute × 1,000) (36) in an MRX microplate reader (Dynatech Laboratories, Chantilly, VA).
Cell surface biotinylation.
HeLa-USU cells were transfected with the various G-encoding plasmids and allowed to express overnight as described above. After overnight incubation, cells were washed three times with ice-cold phosphate-buffered saline (PBS), and then cell surface proteins were biotinylated using 0.25 mg/ml EZ-Link NHS-biotin (Pierce, Rockford, IL) in PBS for 30 min at 4°C. Following surface biotinylation, the cells were washed three times with ice-cold PBS and cell lysates were prepared as described above. One half of each lysate was incubated with 100 μl 20% agarose-avidin D (Vector Laboratories, Inc., Burlingame, CA) in immunoprecipitation (IP) buffer (0.14 M NaCl, 0.1 M Tris, and 0.1% Triton) at 4°C overnight. Samples were then washed twice with lysis buffer followed by one wash with DOC buffer as described above. Precipitated proteins were then boiled in reducing sample buffer and analyzed by 4 to 20% Tris-glycine gradient gel electrophoresis (Invitrogen), followed by transfer to nitrocellulose and probing with G-specific mouse polyclonal antiserum at a concentration of 1:20,000.
Sucrose gradient density ultracentrifugation.
Oligomeric characteristics of the various G alanine mutants were assessed essentially as described before (9). In short, the various alanine substitution mutants or WT HeV G were expressed in HeLa-USU cells, which were metabolically labeled, chased, and lysed as described above. One half of each lysate was layered onto a continuous 5 to 20% sucrose gradient and centrifuged at 40,000 rpm for 20 h at 4°C, and then each gradient was fractionated into fractions of about 1 to 1.2 ml. Fractions were immunoprecipitated with 2 μl G-specific rabbit polyclonal antisera overnight at 4°C and then analyzed by SDS-PAGE on 4 to 20% Tris-glycine gels under reducing and nonreducing conditions.
Deglycosylation assays.
G alanine mutants or WT HeV G were expressed in HeLa-USU cells and lysates were prepared as described above. G-containing lysates were incubated overnight at 4°C with 5 μl G-specific rabbit polyclonal antiserum, precipitated with 100 μl protein G-Sepharose, and washed as described above. The protein G beads were then boiled for 10 min in 45 μl 1× glycoprotein denaturing buffer (New England Biolabs, Beverly, MA) and centrifuged at maximum speed for 4 min, and the supernatant was removed to new tubes in which the deglycosylation reaction was conducted using 3 μl of peptide-N-glycosidase F (PNGase F; New England Biolabs) or 3 μl of endoglycosidase Hf (Endo Hf; New England Biolabs) for either 0, 10, or 60 min at 37°C. The reaction mixtures were mixed with reducing sample buffer, analyzed by SDS-PAGE, transferred to nitrocellulose, and probed with G-specific mouse polyclonal antiserum at 1:10,000.
dMM treatment.
Various mutants and the WT G glycoprotein were expressed in HeLa-USU cells in the presence versus absence of 1-deoxymannojirimycin, HCl (dMM; EMD Biosciences, Inc., Madison, WI), in order to prevent the conversion of high mannose to complex oligosaccharides. Cell culture conditions were essentially the same as described above except for the addition of 0.5 mm dMM and 200 mM HEPES (Quality Biologicals) to the medium 2 h postinfection with WR vaccinia virus. Following overnight incubation with dMM, cell surfaces expressing the mutants or WT G were washed and biotinylated as described above. Surface-expressed glycoproteins were precipitated with avidin D-agarose and analyzed by SDS-PAGE followed by Western blotting with mouse polyclonal G-specific antiserum at 1:20,000. The mutants and WT G glycoprotein produced in the presence and absence of dMM were also subjected to immunoprecipitation with several MAbs, followed by SDS-PAGE and Western blotting.
RESULTS
Expression and fusion promotion activity of HeV G stalk domain mutants.
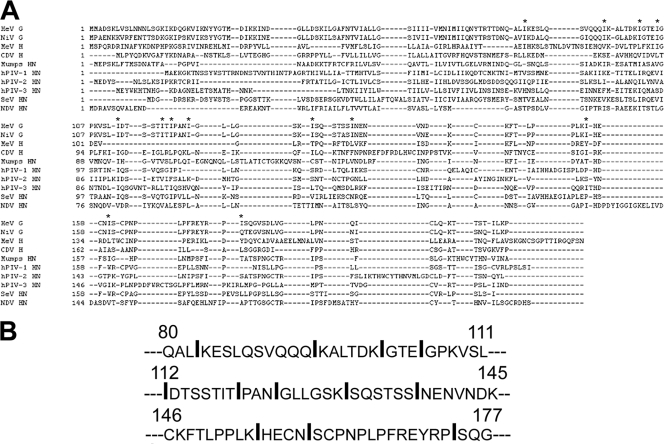
An isoleucine-rich stretch of amino acid residues in the HeV G glycoprotein stalk domain was identified that is also 100% conserved in NiV G and well conserved, with either isoleucine, leucine, or valine residues at analogous positions, among several other paramyxoviruses, including the HN glycoprotein of NDV, Sendai virus, hPIV-1 and hPIV-3, and the H glycoprotein of MeV and canine distemper virus. An amino acid sequence alignment of the stalk region of the N-terminal part of HeV G with that of other paramyxovirus attachment proteins is shown in Fig. 1A. Earlier work suggested that these residues within NDV HN could form two heptad repeat-like structures similar to those within the F glycoprotein (40) and that this stalk region was important for interaction between the attachment glycoprotein and F and in determining F-virus species fusion specificity (18, 22, 32, 42, 43). Molecular modeling of HeV G shows this region of the protein stalk as an α-helical stretch, and in some modeled configurations the domain possesses a kink. To explore whether this domain in HeV G possesses any similar functional importance, we individually mutated 12 of 13 isoleucine residues, shown in Fig. 1B, to alanine in HeV G from amino acid position 83 to 174 and assessed the mutant G glycoproteins for their fusion promotion activities.
FIG. 1.
Sequence alignment of the stalk regions in selected paramyxovirus attachment proteins. (A) Partial sequence alignment of the HeV G stalk domain with that of other paramyxovirus attachment proteins. Asterisks indicate the motif of conserved isoleucine, leucine, and valine residues. (B) That particular motif in the stalk of HeV G consisting solely of isoleucines. Large, boldfaced residues are those which were mutated to alanine and subsequently assessed for fusion promotion activity in the current study. The I118 residue that we were unable to mutate is shown in plain, unbolded text and underlined.
Each of these HeV G mutant constructs or WT HeV G was coexpressed with HeV F in an effector cell population and then tested for fusion promotion activity along with a receptor-bearing target cell population, and the results are shown in Fig. 2. This analysis revealed that 9 of 12 G glycoprotein, single amino acid-substituted, stalk mutants had completely lost the ability to promote membrane fusion. Notably, all 9 of these 12 isoleucine residues were better conserved overall among the majority of the attachment glycoproteins analyzed by sequence alignment than were the 3 isoleucine residues (I83, I94, and I174), which had no effect on the G glycoprotein's fusion promotion activity when altered and which were located at both ends of the domain of interest (Fig. 1). These single amino acid substitutions in G were profoundly defective in supporting fusion, but the nature of this defect was unknown. Relative temperature has been shown to affect viral glycoprotein-mediated cell-cell fusion (29); however, the block in fusion caused by these mutations could not be overcome by increasing the temperature at which the fusion assay was conducted from 37°C to 42°C (data not shown).
FIG. 2.
Fusion promotion activity of HeV G glycoprotein stalk mutants. The various HeV G alanine mutants or WT HeV G were coexpressed with HeV F and assayed for their ability to promote cell-cell fusion when mixed with receptor-positive 293T or PCI-13 cells in a quantitative, vaccinia virus-based fusion assay as described in Materials and Methods. HeLa-USU cells, which are receptor-negative for henipaviruses, served as a negative control. The means of two independent experiments are shown. Error bars represent the ranges. This experiment has been conducted more than five times, and a representative result is shown.
Although it seemed unlikely that these individual alanine substitutions would globally disrupt an important overall structure possessed by this stalk domain, we next sought to determine whether the observed fusion defect could be due to gross misfolding of the mutant glycoproteins and thus significantly reducing expression levels at the cell surface. Nevertheless, subtle changes in cell surface expression levels of viral membrane glycoproteins that are involved in membrane fusion can have measurable effects on the fusion process. In order to assess cell surface expression of these mutants, the surfaces of cells transiently expressing either each mutant or WT HeV G were biotinylated at 4°C. After washing to remove excess biotin, cells were lysed and surface-expressed proteins were then precipitated using avidin beads. Under these conditions, only two of the mutants (I155A and I160A) exhibited decreased levels of cell surface expression in comparison to wild-type HeV G, although they were readily detected in the cell lysates (Fig. 3). Thus, the defect in fusion promotion ability conveyed by the majority of the mutants (seven of nine) could not be attributed to gross misfolding of the protein or a resultant defect in cell surface expression. It was also observed that the nine fusion-defective mutants exhibited an altered electrophoretic species, consisting of a G species with an apparent molecular weight equivalent to WT HeV G and a slightly larger species that was more predominant in the cell surface HeV G material.
FIG. 3.

Cell surface expression of HeV G glycoprotein stalk mutants. Proteins on the surfaces of HeLa-USU cells transiently expressing HeV G alanine mutants or WT HeV G were biotin labeled at 4°C. Lysates were prepared, and biotin-labeled proteins were immunoprecipitated with avidin-agarose beads, subjected to SDS-PAGE, and immunoblotted with G-specific antisera as described in Materials and Methods. Total cell lysates were also probed with polyclonal G-specific antisera for comparison (control). Arrows point to the two species of HeV G.
Receptor binding properties of HeV G stalk domain mutants.
Loss or defects in receptor binding ability would be expected to have a significant adverse effect on the G glycoprotein's fusion promotion activity. Therefore, we next tested each of the G mutants for the ability to bind the henipavirus receptors ephrinB2 and ephrinB3 in a coprecipitation-based assay (5, 6). With this assay, each of the HeV G mutants, including I155A and I160A, which were poorly surface expressed, were coprecipitated with soluble, epitope-tagged human ephrinB2 and ephrinB3 to levels equivalent to WT HeV G, including the slightly higher-molecular-weight species. The results, shown in Fig. 4, demonstrate that the defect in fusion promotion activity caused by these stalk domain mutations is not attributable to lack of receptor binding competence by the HeV G mutants.
FIG. 4.

Receptor binding by HeV G glycoprotein stalk mutants. The various alanine mutants or WT HeV G were transiently expressed in HeLa-USU cells and subjected to coprecipitation with s-tagged human ephrinB2 followed by S-agarose beads or Fc-tagged human ephrinB3 followed by protein G beads. Each lysate was also directly precipitated with polyclonal G-specific antiserum followed by protein G beads for comparison (control). Precipitated proteins were analyzed by SDS-PAGE followed by Western blotting with polyclonal G-specific antiserum.
Oligomerization of HeV G stalk domain mutants.
Previous work has demonstrated that like other paramyxovirus attachment glycoproteins, HeV G appears to be a disulfide-linked dimer and that the native configuration appears to be a dimer of dimers or tetrameric (9). In addition, the stalk domain of MeV H is a critical determinant of H oligomerization (37), and thus the possibility that the HeV G stalk mutants generated here could be defective in oligomerization and as a result defective in their fusion promotion activity needed to be examined. Therefore, we analyzed several of the HeV G glycoprotein stalk mutants for their ability to form the dimeric and tetrameric species similar to that of WT HeV G. We selected several of the completely fusion-defective mutants and one fusion-competent stalk mutant, along with WT HeV G, each was transiently expressed and metabolically labeled, and cell lysates were prepared and subjected to sucrose density ultracentrifugation, fractionation, and immunoprecipitation with G-specific antisera. The immunoprecipitated G glycoproteins in each fraction of the gradient were analyzed by SDS-PAGE under reducing and nonreducing conditions, and these results are shown in Fig. 5. This analysis revealed that each HeV G mutant examined was observed to form oligomers with an identical pattern as that exhibited by the WT HeV G glycoprotein, and both tetrameric and dimeric species were observed under nonreducing conditions which were resolved to monomeric forms of G under reducing conditions (Fig. 5), essentially identical to prior observations (9). Thus, the conclusion from this analysis is that the observed fusion promotion defect caused by the isoleucine-to-alanine mutations in the stalk domain cannot be attributed to a failure of these mutant G glycoproteins to form native oligomeric complexes.
FIG. 5.

Oligomerization of HeV G glycoprotein stalk mutants. Various alanine mutants or WT HeV G were transiently expressed in HeLa-USU cells, metabolically labeled, and chased as described in Materials and Methods. Each lysate was layered onto a continuous 5 to 20% sucrose gradient and centrifuged at 40,000 rpm for 20 h at 4°C. Then, each gradient was fractionated and immunoprecipitated with polyclonal G-specific antiserum and analyzed by SDS-PAGE under reducing and nonreducing conditions followed by autoradiography. The last two fractions of the I112A mutant are not shown for the sake of organizational clarity. The different species of G, monomer (m), dimer (d), and tetramer, are indicated on the right.
Glycosylation of HeV G stalk domain mutants.
Because of the observation that the nine fusion promotion-defective stalk domain mutants of HeV G all exhibited slightly higher molecular weight species upon SDS-PAGE analysis in addition to a species that comigrated with WT HeV G, we sought to characterize the nature of this alteration. The apparent difference in molecular mass between both HeV G species was approximately 4 to 5 kDa and could potentially be attributable to an additional posttranslational N-glycosylation modification of the molecule. Therefore, we examined whether this higher molecular weight species could be due to an additional glycosylation in the protein that was somehow brought about through the introduction of the stalk domain point mutations. We selected two representative HeV G mutants near the middle of the stalk domain of interest that were completely defective in fusion promotion activity along with WT HeV G and subjected them to PNGase or Endo Hf treatment for 0, 10, and 60 min followed by SDS-PAGE and Western blot analysis; the results are shown in Fig. 6A. While PNGase is an enzyme which will remove multiple types of N-glycans, Endo Hf is specific for high-mannose oligosaccharides, and once high-mannose oligosaccharides are converted to the complex form, they are no longer susceptible to digestion by Endo Hf. After either 10 or 60 min of incubation with PNGase at 37°C, there was an apparent shift in molecular weight for the two mutants and the WT HeV G, indicating the successful removal of N-glycans from G. Importantly, after N-glycan removal, there was no longer any difference in the apparent molecular weight or migratory properties between the HeV G mutants or WT HeV G, indicating that the observed difference in migratory properties at time zero is due to N-glycosylation. Interestingly, for both the HeV G mutants examined and the WT HeV G, there was a shift in electrophoretic mobility following treatment with Endo Hf as well, although for both there was still a subfraction of the protein which migrated as if unaffected by Endo Hf treatment (Fig. 6A). This suggested that both the HeV G mutants and the WT HeV G contain some high-mannose and some complex-type oligosaccharides.
FIG. 6.
Complex oligosaccharide addition to HeV G glycoprotein stalk mutants. The apparent higher-molecular-weight species of fusion-defective G stalk mutants was explored. (A) G alanine mutants or WT HeV G were expressed in HeLa-USU cells and lysates were prepared as described in Materials and Methods. G-containing lysates were immunoprecipitated with polyclonal G-specific antiserum followed by protein G beads. Precipitated proteins were treated with PNGase F or Endo HF at 37°C for 0, 10, or 60 min, and the reactions were analyzed by SDS-PAGE and Western blotting with polyclonal G-specific antiserum. (B) Schematic of the HeV G glycoprotein, illustrating the location of eight potential N-linked glycosylation sites (asterisks) in reference to the stalk domain of G. (C) Effect of individual glycosylation site deletions on fusion promotion ability of G, assessed in a quantitative, vaccinia virus-based cell fusion assay as described in Materials and Methods. The reactions were conducted in duplicate wells using receptor-positive 293T cells and receptor-negative HeLa-USU cells. Error bars illustrate the ranges. The inset panel illustrates essentially unaltered electrophoretic mobility observed when the resulting double mutants were tested for expression. HeLa-USU cells were transiently transfected, metabolically labeled, and chased as described in Materials and Methods. Resulting cell lysates were immunoprecipitated with several different monoclonal and polyclonal antibodies, and the results obtained with m101 are shown as an example. (D) Several mutants and the WT G were expressed in HeLa-USU cells in the presence (+) or absence (−) of dMM, which inhibits the conversion of high-mannose to complex oligosaccharides. Mutant or WT G glycoproteins on the cell surface were biotinylated, precipitated with avidin D-agarose, and analyzed by SDS-PAGE followed by Western blotting with G-specific antiserum.
It has been reported that addition of N-glycans to paramyxovirus F or G glycoproteins can result in decreased fusion (1, 31, 45). Therefore, we questioned whether this apparent extraneous glycosylation, associated with the fusion-promotion-defective phenotype, could be masking an important domain of G involved in the fusion promotion process. The full-length HeV G glycoprotein has seven potential N-linked glycosylation sites in the extracellular domain. One site located in the extracellular region is proximal to the predicted transmembrane anchor and likely not modified. The other six sites are located at various positions along the extracellular portion of G and are conserved between HeV and NiV. A recently completed structural analysis of NiV G has shown that N306, N378, N481, and N529 were modified, N417 was not (47), and N159 was not included in that structure. The location of these sites in relation to the rest of the protein is diagrammed in Fig. 6B. We speculated that if the presence of an extra or differentially modified N-glycan were occluding an important domain of G required for its fusion-promoting activity, then its removal by mutation might prevent this interference and restore its fusion promotion activity. To examine this possibility we individually mutated the asparagine residue at each site to glutamine in the context of one of the HeV G mutants (I124A) as a representative example and tested the resulting double mutants for expression. Surprisingly, none of the glycosylation site deletions resulted in any change in electrophoretic mobility pattern, although for some of the HeV G mutants, the slightly higher molecular weight species was slightly decreased in intensity (Fig. 6C, inset), and simultaneous analysis of all eight additional HeV G double mutants for fusion promotion activity upon coexpression with F (Fig. 6C) revealed that none was rescued in its ability to promote fusion. Together, these results demonstrated that although it is was not apparent which N-glycosylation site was being altered in comparison to WT HeV G, this posttranslational modification by itself was not likely to be obscuring an important domain of G resulting in the observed fusion promotion defect.
In order to further explore the altered glycosylation phenotype, we selected three of the seven (surface-expressed) HeV G mutants as representatives along with WT HeV G and expressed each in HeLa-USU cells in the presence and absence of dMM, which was added to the cell culture medium, in order to prevent conversion of high-mannose to complex-type oligosaccharides, and these results are shown in Fig. 6D. Indeed, the inclusion of dMM in the cell culture medium resulted in a notable shift in the electrophoretic mobility of the slightly higher molecular weight species of the HeV G mutants and the WT HeV G, consistent with those results obtained upon Endo Hf digestion (Fig. 6A). Importantly, however, when expressed in the presence of dMM, these HeV G mutants and the WT HeV G had a similar electrophoretic mobility, indicating that the difference in apparent molecular weights of the HeV G mutants and WT HeV G in the absence of dMM is due to the conversion of high-mannose to complex-type oligosaccharides.
Finally, we examined whether treatment with dMM and thus prevention of complex oligosaccharide formation would restore the fusion promotion activity of a defective HeV G mutant. Here, the same selected HeV G mutants along with WT HeV G were each cotransfected along with HeV F and expressed in the presence and absence of dMM. These resulting effector cell populations were then mixed with either receptor-positive or -negative target cells in the cell-cell fusion assay. These results revealed that effector cells expressing HeV F and WT HeV G were able to mediate fusion with receptor-positive 293T cells in the presence or absence of dMM treatment, while those effector cell populations expressing HeV F along with a HeV G mutant remained fusion promotion defective even in the presence of dMM (Fig. 7). This result, along with the results in Fig. 6C, strongly suggest that the apparent conversion of high-mannose to complex oligosaccharides observed in the stalk mutants is not the cause of the fusion-promotion-defective phenotype of these stalk domain HeV G mutants.
FIG. 7.
dMM treatment does not restore fusion promotion activity to mutant G. Representative HeV G mutants and WT HeV G were cotransfected with HeV F and tested for fusion promotion activity in the presence and absence of 0.5 mM dMM. Error bars represent standard deviations.
HeV F interaction with HeV G stalk domain mutants.
As discussed above, previous work carried out with attachment glycoproteins of other paramyxoviruses containing mutations in the stalk domain has implicated this region as an important determinant of F engagement and/or F species specificity. To examine this possibility in the case of the fusion-promotion-defective HeV G mutants, we selected three of the seven (surface-expressed) stalk domain HeV G mutants as before to examine in a previously developed coprecipitation-based biotin labeling assay for F-G interaction (5) and assessed whether their defective fusion promotion activity could be correlated to a decreased ability to interact with their partner glycoprotein, HeV F. We found that each HeV G mutant and the WT HeV G were comparably expressed (Fig. 8A) and present on the cell surface as expected (Fig. 8B); however, the slightly higher molecular weight species that was observed to be the predominant species at the cell surface (Fig. 3) was not found complexed with and coprecipitated by F, and only the HeV G species (predominantly intracellular) that had a similar apparent molecular weight in comparison to WT HeV G was coprecipitated with F (Fig. 8C).
FIG. 8.

F interaction ability of HeV G glycoprotein stalk mutants. Representative HeV G mutants or WT HeV G were coexpressed in the presence and absence of HeV F as described in Materials and Methods and biotin labeled at 4°C. Cell lysates were prepared and immunoprecipitated with different reagents. Gels show immunoprecipitation with polyclonal G-specific antiserum (A), avidin (B), and polyclonal F-specific antiserum (C). The samples were all processed and analyzed by 4 to 20% gradient SDS-PAGE and Western blotting with G-specific antiserum.
Characterization of HeV G stalk domain mutants by MAb reactivity.
The HeV G stalk domain mutants that were completely defective in fusion promotion activity were cell surface expressed and competent for receptor binding and retained their oligomeric structure, but were apparently defective in F interaction. A favored model of paramyxovirus membrane fusion suggests that receptor binding triggers changes in the attachment glycoprotein (in this case, G), resulting in its dissociation from F. As a further approach to characterize the nature and effects of the stalk domain mutations within HeV G, such as whether these mutations may be causing any measurable conformation changes in the molecule, we made use of a panel of G-specific MAbs, including those which compete for receptor (ephrinB2), such as m101 and m102, and others that do not, such as m106 (5, 46, 53). We first examined the MAb binding reactivities of WT HeV G in both the presence and absence of ephrinB2 in a coprecipitation assay, and these results are shown in Fig. 9. Three types of relative MAb reactivity were observed: MAbs that could bind and precipitate G to equivalent levels in the presence or absence of receptor (hAH1.3 and 8H4), those that bound less because they compete for receptor (nAH22.4 and m102.4), and interestingly, MAbs that bound and precipitated HeV G better after ephrinB2 binding (nAH23.4, nAH24.4, hAH2.1, and m106.3). This latter MAb binding phenotype was suggestive of a conformational change in the G glycoprotein following receptor engagement. The MAb m106.3 is an affinity-matured derivative of the human Fab, m106, and m106 was also found to exhibit enhanced binding to receptor-bound HeV G (data not shown).
FIG. 9.

MAbs recognize receptor-induced conformational changes in HeV G. Several MAbs were assessed for their ability to recognize and immunoprecipitate HeV G glycoprotein following a 1-h preincubation of G protein with either s-tagged human ephrinB2 or an equal amount of PBS at 37°C. +, incubation with ephrinB2; −, incubation with PBS as a control. (A) HeV G was precipitated with various mouse MAbs and analyzed by SDS-PAGE followed by Western blotting with polyclonal G-specific antiserum. (B) Metabolically labeled HeV G was precipitated with human MAbs and analyzed by SDS-PAGE followed by autoradiography.
In this assay, cell lysates containing the various HeV G stalk domain mutants or WT HeV G were immunoprecipitated with each of these MAbs in the absence of receptor, and the levels of precipitated G glycoprotein were then quantitated by densitometry. A representative result obtained using the three conformation-dependent human MAbs is shown in Fig. 10, and a summary of all the MAb reactivity data obtained with the HeV G mutants is presented in Table 1. All of the HeV G mutants were recognized by all conformation-dependent MAbs tested, which together with the cell surface expression data provided further evidence that the HeV G mutants are not grossly misfolded. However, an interesting pattern in MAb reactivity emerged during this analysis, in that those MAbs that were capable of detecting conformational changes in HeV G following receptor binding, as measured by an increased binding reactivity to HeV G-receptor complexes, also exhibited a similar increased binding phenotype to the fusion-promotion-defective stalk domain mutants of HeV G, yet did so in the absence of any bound ephrinB2 receptor (i.e., m106, hAH2.1, nAH23.4, and nAH24.4). These data suggested that the stalk domain HeV G mutations were causing conformational alterations in G that were associated with receptor binding.
FIG. 10.

Human MAb reactivities to HeV G glycoprotein stalk mutants. (A) Alanine substitution mutants of HeV G were transiently expressed in HeLa-USU cells, metabolically labeled, and chased as described in Materials and Methods. Cell lysates were prepared and divided equally into four parts, which were immunoprecipitated with human MAbs 101, 102.4, and 106 or rabbit polyclonal G-specific antiserum (control). The precipitated proteins were analyzed by SDS-PAGE followed by autoradiography. (B) Autoradiographs were used to quantify the relative amounts of precipitated protein by spot densitometry, and the results are expressed as the percentage of WT reactivity.
TABLE 1.
MAb reactivities to G glycoprotein mutantsa
| G mutation | MAb reactivity in category:
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 1
|
2
|
3
|
||||||
| 102.4 | 101 | nAH22.4 | 8H4 | hAH2.1 | 106 | nAH23.4 | nAH24.4 | |
| I83A | NC | NC | NT | NC | NC | − | − | NC |
| I94A | NC | NC | NT | NC | NC | NC | − | NC |
| I101A | + | NC | NT | NC | NC | + | NC | + |
| I105A | NC | NC | ++ | NC | ++ | + | + | ++ |
| I112A | NC | NC | ++ | NC | ++ | + | + | ++ |
| I120A | NC | NC | NT | NC | + | + | + | ++ |
| I124A | NC | NC | NC | NC | ++ | + | + | ++ |
| I131A | NC | NC | ++ | NC | + | + | NC | + |
| I138A | NC | NC | NT | NC | + | + | + | ++ |
| I155A | NC | NC | NT | NC | + | + | + | + |
| I160A | NC | NC | NT | NC | + | + | + | + |
| I174A | NC | NC | NT | NC | NC | + | − | NC |
Selected MAbs were assessed for their reactivities to the various alanine mutants versus WT HeV G in immunoprecipitations followed by SDS-PAGE and either Western blotting or autoradiography. The results were quantitated via spot densitometry, and the results are summarized here. −, 50 to 75% of WT reactivity; NC, virtually no change or 76 to 125% of WT reactivity; +, 126 to 175% of WT reactivity; ++, 176% of WT reactivity or higher; NT, not tested. For the reader's convenience, MAbs in the chart are divided into three categories based on their detection profile of WT G in the presence versus absence of soluble ephrinB2: MAbs in category 1 immunoprecipitate less WT G in the presence of receptor, MAbs in category 2 show no detectable change in the amount of WT G they immunoprecipitate in the presence of receptor, and MAbs in category 3 immunoprecipitate more WT G in the presence of receptor.
Although the possibility that these differential binding reactivities were due to actual epitope alterations seemed unlikely, for example, the fact that nAH23.4 and nAH24.4 are Western blot-reactive MAbs (data not shown), prompted us to further explore whether it was the MAbs' epitopes or G's conformation that had been altered. In order to do so, we conducted a simple boiling experiment. We hypothesized that if indeed our mutations had altered a shared epitope of these antibodies and the epitope was completely linear in nature, a boiled HeV G mutant would remain better recognized by the antibody than the boiled WT HeV G. Conversely, if the antibodies had an epitope that was partially conformation dependent, and if the antibodies were indeed recognizing a conformational difference between the HeV G mutants and the WT HeV G, then it would be expected that preboiling the mutant and the WT G prior to immunoprecipitation with these antibodies would remove the difference between the amount of mutant G recognized versus the amount of WT G. Therefore, we preboiled lysates containing the HeV G mutants or WT HeV G for 5 min and then subjected them to immunoprecipitation with one of the MAbs in question, nAH23.4. Under these conditions, the mutants and the WT G were all immunoprecipitated to similar levels; the apparent difference in MAb nAH23.4 reactivity to the HeV G mutants versus WT HeV G had disappeared (data not shown). This observation supported the suggestion that the stalk domain mutations had not simply altered a MAb epitope, but rather altered the conformation of G, and denaturing the protein first eliminated the conformational difference between mutant and WT G. For these reasons and because the mutations causing the identical fusion-promotion-defective phenotype span a relatively large area of the protein, encompassing a stretch of at least 55 amino acid residues, it seems plausible that the fusion-defective phenotype and increased MAb reactivity by those antibodies which preferentially bind receptor-complexed HeV G are related to an altered conformation of the protein.
Finally, since the fusion-defective stalk domain HeV G mutants displayed an altered electrophoretic mobility which was apparently due to a more complex oligosaccharide modification compared to the WT HeV G, which could be prevented by addition of dMM to the cell culture medium, we also examined whether the reactivity of these MAbs to the G mutants would be affected if dMM were used during their expression and thus prevented the conversion of high-mannose to complex oligosaccharides. We selected the same three of the seven (surface-expressed) HeV G mutants as representatives along with WT HeV G, expressed each in the presence and absence of dMM as described in Materials and Methods, and then subjected each to immunoprecipitation with several MAbs followed by SDS-PAGE and Western blot analysis. We observed that the reactivities of MAbs m102.4, m106, and nAH24.4 to the HeV G mutants and WT HeV G were unaffected (data not shown), further indicating that the apparent glycosylation phenotype was also not the cause of the increased reactivities of these MAbs.
DISCUSSION
Using site-directed alanine-scanning mutagenesis, we examined the importance of the stalk domain of the HeV G attachment glycoprotein in its various structural and functional characteristics by targeting a series of well-conserved isoleucine residues within this domain. We found that a single amino acid substitution mutation to alanine of 9 out of 12 isoleucine residues between positions 83 and 174 resulted in completely defective fusion promotion activity, results consistent with observations made with other paramyxovirus attachment glycoproteins (15, 18, 32, 40, 42, 43). Although mutation of HeV G isoleucine stalk residues to alanine abrogated its fusion promotion activity in 9 of 12 cases, the G glycoprotein mutants were all cell surface expressed, retained their oligomeric structure, were recognized by conformation-dependent MAbs, and were capable of binding the two known viral receptors, ephrinB2 and ephrinB3.
The series of isoleucine residues in the HeV G stalk targeted in the present study is similar to other hydrophobic residues that have been examined using mutagenesis within the H and HN glycoproteins of several other paramyxoviruses. In particular, homologous amino acids in NDV HN, hypothesized to form two heptad repeat-like structures, were shown to be important for HN-F interaction (40), and targeting this region by mutagenesis has clearly demonstrated its importance in modulating HN-F-mediated fusion as well the interaction between the two proteins (32). In contrast, mutations made in the analogous region of MeV H were also observed to decrease its fusion promotion activity yet did so without effecting the H-F interaction (15). For HeV G stalk domain mutants, we found a direct correlation between defects in G glycoprotein interaction with F and a lack of fusion promotion activity, similar to those observations with NDV HN-F. Together, these data indicate that this stalk region within HeV G is also critically important role for its fusion promotion activity.
Unlike several prior studies involving stalk domain mutagenesis in other paramyxovirus systems, we found that mutation of those HeV G isoleucine stalk domain residues that abrogated its fusion promotion activity also resulted in an apparent different N-glycosylation pattern and the appearance of a slightly higher-molecular-weight species. The individual elimination by further mutagenesis of all eight potential N-glycosylation sites within G in the context of a stalk domain mutant was unable to delineate which site was involved and also did not alter the fusion-promotion-defective phenotype. We then determined that this observed difference in glycosylation of the HeV G mutants versus WT G was related to an increased conversion of high-mannose to complex oligosaccharides. Previous studies carried out on other paramyxovirus fusion and attachment proteins demonstrated that additional glycosylation can lead to decreased fusion or failure to interact with the partner glycoprotein (1, 31, 45). Similarly, we observed with the differentially N-glycosylated HeV G mutants that the slightly higher-molecular-weight species that was expressed on cell surfaces was incapable of interacting with F. At least two possibilities exist to account for the defect in F interaction. First, the addition of complex oligosaccharides interferes with the G-F interaction directly, and second, the stalk domain mutations cause a conformational alteration in G that disrupts F engagement that is also associated with the appearance of the altered glycosylated species of HeV G. One finding that provides evidence for this latter possibility is that expression of the HeV G mutants and WT HeV G in the presence versus absence of dMM, which prevented conversion of high-mannose to complex oligosaccharides and eliminated the formation of the higher-molecular-weight species, did not restore the fusion promotion activity of the HeV G stalk domain mutants.
Perhaps of greater interest was that further characterization of the HeV G stalk domain mutants revealed that receptor binding could facilitate a measurable conformational change in G, as detected by several conformation-dependent and -independent MAbs. In nearly all cases, efficient paramyxovirus-mediated fusion requires the participation of both an attachment and fusion glycoprotein (reviewed in reference 29). For many paramyxoviruses, a physical interaction between F and its homologous attachment glycoprotein partner has been detected, including HeV (5), and a favored model for fusion suggests that upon receptor binding, the attachment glycoprotein triggers F-mediated fusion, presumably through receptor-induced conformational changes of its own (reviewed in references 7 and 27). The data here on HeV G are the first demonstration of a protein receptor-induced conformational change in a paramyxovirus attachment glycoprotein that uses a protein receptor, as measured by MAb binding reactivities. These findings, along with the observations that those same MAbs could preferentially bind to the fusion promotion-defective HeV G stalk domain mutants, also support the speculation that these conformational changes in HeV G appear to correlate with both receptor binding and G-F nonassociation (release). These data are in agreement with the work of Takimoto et al. (41), who demonstrated alternative conformations in NDV HN depending on whether it was bound with 2-deoxy-2, 3-dehydro-N-acetylneuraminic acid (sialic acid). Taken together, we speculate that these HeV G stalk domain mutants are assuming a receptor binding conformation, in the absence of receptor, and thus are already “triggered” upon expression at the cell surface, not associated with F, and hence unable to execute their fusion-promoting activity even after subsequent receptor binding.
Our findings suggest an important role for the stalk domain of HeV G in maintenance of its conformation and potentially also in the receptor binding-triggered changes leading to productive fusion perhaps related to the dissociation of G and F. This notion is similar to the findings of Wang et al., who found that the stalk domain of NDV HN was essential for neuraminidase activity, even though the neuraminidase active site is located in the globular head region (44), those of Deng et al., who observed that the stalk domain was important for maintenance of antigenic structures within the globular head domain as well as neuraminidase activity in HN (17), and the findings by Melanson et al., who found some mutations within the stalk of NDV HN could prevent F engagement and thereby prevent fusion (32).
It has been suggested that the fusion mechanism of paramyxoviruses that make use of sialic acid moieties as receptors proceeds by a different process than that of the protein receptor-utilizing paramyxoviruses (the henipaviruses and morbilliviruses) (reviewed in reference 27). Here, our data on the HeV G stalk domain are consistent with those of Melanson and Iorio (32), who demonstrated that the fusion activity of NDV HN and F is directly proportional to the extent of the HN-F interaction. Thus, although HeV makes use of cellular proteins as opposed to sialic acid moieties as its receptor, the G-F interaction also appears proportional to their fusion activity. This is in contrast to those observations on MeV, which like HeV makes use of protein receptors, where the strength of the MeV H-F interaction is inversely related to their fusion activity (38). Nevertheless, the apparent similarities between NDV and HeV with regard to their attachment and fusion glycoprotein interactions and fusion activity are at least consistent with the recent NiV and HeV G and ephrinB2 and -B3 structures (11, 47), revealing similar locations within their attachment glycoproteins for receptor recognition, suggesting that these two viral fusion processes brought about by quite different types of receptor triggering could be more similar than previously anticipated.
Finally, our data here also reveal conformational alterations in G that appear related to receptor binding as measured by MAb binding. The recent structural analysis of NiV G both alone and in complex with receptor has shown that receptor-mediated rearrangements in G are relatively small and localized to the G-ephrinB3 interface (47). However, it should be pointed out that the studies conducted here are in the context of full-length G, whereas only a globular head and monomer G structure have been characterized, and the possibility that receptor engagement could induce more significant conformational changes in full-length G, such as between pairs of dimers, cannot be ruled out and such alterations could be readily detected by specific MAb reactivities. Future experiments aimed at defining the epitopes recognized by some of the MAbs used here, along with additional structural studies, will facilitate a better understanding of the rearrangements that take place in G following receptor binding and help define the neutralization mechanisms of different classes of antibodies, such as those that do not block receptor binding. Such findings should aid our understanding of the paramyxovirus fusion process in general and could potentially lead to the design of new classes of antiviral drugs and vaccines.
Acknowledgments
We thank Michael Flora and all his staff at the Biomedical Instrumentation Center (BIC) of the Uniformed Services University (USU) for primer synthesis and sequencing. We also thank John White (CSIRO) for monoclonal antibodies and Erica Ollman Saphire (Scripps) and Rebecca Dutch (University of Kentucky) for helpful discussions.
This work was supported by NIH grant AI054715 to C.C.B. This study was also supported by the NIH intramural biodefense program (D.S.D.). This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract N01-CO-12400. This research was supported in part by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The views expressed in the manuscript are solely those of the authors, and they do not represent official views or opinions of the Department of Defense or The Uniformed Services University of the Health Sciences.
Footnotes
Published ahead of print on 17 September 2008.
REFERENCES
- 1.Aguilar, H. C., K. A. Matreyek, C. M. Filone, S. T. Hashimi, E. L. Levroney, O. A. Negrete, A. Bertolotti-Ciarlet, D. Y. Choi, I. McHardy, J. A. Fulcher, S. V. Su, M. C. Wolf, L. Kohatsu, L. G. Baum, and B. Lee. 2006. N-glycans on Nipah virus fusion protein protect against neutralization but reduce membrane fusion and viral entry. J. Virol. 804878-4889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymous. 2004. Hendra virus—Australia (Queensland) ProMED archive no. 20041214.3307. International Society for Infectious Diseases.
- 3.Anonymous. 2008. Hendra virus, human, equine—Australia (04): (Queensland) ProMED archive no. 20080725.2260. International Society for Infectious Diseases.
- 4.Anonymous. 2004. Person-to-person transmission of Nipah virus during outbreak in Faridpur District, 2004. Health Sci. Bull. 25-9. [Google Scholar]
- 5.Bishop, K. A., T. S. Stantchev, A. C. Hickey, D. Khetawat, K. N. Bossart, V. Krasnoperov, P. Gill, Y. R. Feng, L. Wang, B. T. Eaton, L. F. Wang, and C. C. Broder. 2007. Identification of Hendra virus G glycoprotein residues that are critical for receptor binding. J. Virol. 815893-5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonaparte, M. I., A. S. Dimitrov, K. N. Bossart, G. Crameri, B. A. Mungall, K. A. Bishop, V. Choudhry, D. S. Dimitrov, L. F. Wang, B. T. Eaton, and C. C. Broder. 2005. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc. Natl. Acad. Sci. USA 10210652-10657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bossart, K. N., and C. C. Broder. Paramyxovirus entry. In S. Pöhlmann and G. Simmons (ed.), Viral entry into host cells, in press. Landes Bioscience, Austin, TX.
- 8.Bossart, K. N., and C. C. Broder. 2004. Viral glycoprotein-mediated cell fusion assays using vaccinia virus vectors. Methods Mol. Biol. 269309-332. [DOI] [PubMed] [Google Scholar]
- 9.Bossart, K. N., G. Crameri, A. S. Dimitrov, B. A. Mungall, Y. R. Feng, J. R. Patch, A. Choudhary, L. F. Wang, B. T. Eaton, and C. C. Broder. 2005. Receptor binding, fusion inhibition, and induction of cross-reactive neutralizing antibodies by a soluble G glycoprotein of Hendra virus. J. Virol. 796690-6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bousse, T. L., G. Taylor, S. Krishnamurthy, A. Portner, S. K. Samal, and T. Takimoto. 2004. Biological significance of the second receptor binding site of Newcastle disease virus hemagglutinin-neuraminidase protein. J. Virol. 7813351-13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bowden, T. A., A. R. Aricescu, R. J. Gilbert, J. M. Grimes, E. Y. Jones, and D. I. Stuart. 2008. Structural basis of Nipah and Hendra virus attachment to their cell-surface receptor ephrin-B2. Nat. Struct. Mol. Biol. 15567-572. [DOI] [PubMed] [Google Scholar]
- 12.Carroll, M. W., and B. Moss. 1995. E. coli beta-glucuronidase (GUS) as a marker for recombinant vaccinia viruses. BioTechniques 19352-356. [PubMed] [Google Scholar]
- 13.Chadha, M. S., J. A. Comer, L. Lowe, P. A. Rota, P. E. Rollin, W. J. Bellini, T. G. Ksiazek, and A. Mishra. 2006. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg. Infect. Dis. 12235-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chua, K. B. 2003. Nipah virus outbreak in Malaysia. J. Clin. Virol. 26265-275. [DOI] [PubMed] [Google Scholar]
- 15.Corey, E. A., and R. M. Iorio. 2007. Mutations in the stalk of the measles virus hemagglutinin protein decrease fusion but do not interfere with virus-specific interaction with the homologous fusion protein. J. Virol. 819900-9910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crennell, S., T. Takimoto, A. Portner, and G. Taylor. 2000. Crystal structure of the multifunctional paramyxovirus hemagglutinin-neuraminidase. Nat. Struct. Biol. 71068-1074. [DOI] [PubMed] [Google Scholar]
- 17.Deng, R., A. M. Mirza, P. J. Mahon, and R. M. Iorio. 1997. Functional chimeric HN glycoproteins derived from Newcastle disease virus and human parainfluenza virus-3. Arch. Virol. Suppl. 13115-130. [DOI] [PubMed] [Google Scholar]
- 18.Deng, R., Z. Wang, A. M. Mirza, and R. M. Iorio. 1995. Localization of a domain on the paramyxovirus attachment protein required for the promotion of cellular fusion by its homologous fusion protein spike. Virology 209457-469. [DOI] [PubMed] [Google Scholar]
- 19.Eaton, B. T., C. C. Broder, D. Middleton, and L. F. Wang. 2006. Hendra and Nipah viruses: different and dangerous. Nat. Rev. Microbiol. 423-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Field, H. E., P. C. Barratt, R. J. Hughes, J. Shield, and N. D. Sullivan. 2000. A fatal case of Hendra virus infection in a horse in north Queensland: clinical and epidemiological features. Aust. Vet. J. 78279-280. [DOI] [PubMed] [Google Scholar]
- 21.Field, H. E., J. S. Mackenzie, and P. Daszak. 2007. Henipaviruses: emerging paramyxoviruses associated with fruit bats. Curr. Top. Microbiol. Immunol. 315133-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gravel, K. A., and T. G. Morrison. 2003. Interacting domains of the HN and F proteins of Newcastle disease virus. J. Virol. 7711040-11049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guillaume, V., H. Aslan, M. Ainouze, M. Guerbois, T. F. Wild, R. Buckland, and J. P. Langedijk. 2006. Evidence of a potential receptor-binding site on the Nipah virus G protein (NiV-G): identification of globular head residues with a role in fusion promotion and their localization on an NiV-G structural model. J. Virol. 807546-7554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gurley, E. S., J. M. Montgomery, M. J. Hossain, M. Bell, A. K. Azad, M. R. Islam, M. A. Molla, D. S. Carroll, T. G. Ksiazek, P. A. Rota, L. Lowe, J. A. Comer, P. Rollin, M. Czub, A. Grolla, H. Feldmann, S. P. Luby, J. L. Woodward, and R. F. Breiman. 2007. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg. Infect. Dis. 131031-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanna, J. N., W. J. McBride, D. L. Brookes, J. Shield, C. T. Taylor, I. L. Smith, S. B. Craig, and G. A. Smith. 2006. Hendra virus infection in a veterinarian. Med. J. Aust. 185562-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsu, V. P., M. J. Hossain, U. D. Parashar, M. M. Ali, T. G. Ksiazek, I. Kuzmin, M. Niezgoda, C. Rupprecht, J. Bresee, and R. F. Breiman. 2004. Nipah virus encephalitis reemergence, Bangladesh. Emerg. Infect. Dis. 102082-2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iorio, R. M., and P. J. Mahon. 2008. Paramyxoviruses: different receptors-different mechanisms of fusion. Trends Microbiol. 16135-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lamb, R. A., and G. D. Parks. 2007. Paramyxoviridae: the viruses and their replication, p. 1449-1496. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 5th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 29.Lamb, R. A., R. G. Paterson, and T. S. Jardetzky. 2006. Paramyxovirus membrane fusion: lessons from the F and HN atomic structures. Virology 34430-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lawrence, M. C., N. A. Borg, V. A. Streltsov, P. A. Pilling, V. C. Epa, J. N. Varghese, J. L. McKimm-Breschkin, and P. M. Colman. 2004. Structure of the haemagglutinin-neuraminidase from human parainfluenza virus type III. J. Mol. Biol. 3351343-1357. [DOI] [PubMed] [Google Scholar]
- 31.Melanson, V. R., and R. M. Iorio. 2006. Addition of N-glycans in the stalk of the Newcastle disease virus HN protein blocks its interaction with the F protein and prevents fusion. J. Virol. 80623-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melanson, V. R., and R. M. Iorio. 2004. Amino acid substitutions in the F-specific domain in the stalk of the newcastle disease virus HN protein modulate fusion and interfere with its interaction with the F protein. J. Virol. 7813053-13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murray, G. 2006. Hendra virus findings in Queensland, Australia, Vol. 19, no.26. World Organisation for Animal Health (OIE), Paris, France. [Google Scholar]
- 34.Negrete, O. A., E. L. Levroney, H. C. Aguilar, A. Bertolotti-Ciarlet, R. Nazarian, S. Tajyar, and B. Lee. 2005. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 436401-405. [DOI] [PubMed] [Google Scholar]
- 35.Negrete, O. A., M. C. Wolf, H. C. Aguilar, S. Enterlein, W. Wang, E. Muhlberger, S. V. Su, A. Bertolotti-Ciarlet, R. Flick, and B. Lee. 2006. Two key residues in ephrinB3 are critical for its use as an alternative receptor for Nipah virus. PLoS Pathog. 2e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nussbaum, O., C. C. Broder, and E. A. Berger. 1994. Fusogenic mechanisms of enveloped-virus glycoproteins analyzed by a novel recombinant vaccinia virus-based assay quantitating cell fusion-dependent reporter gene activation. J. Virol. 685411-5422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Plemper, R. K., A. L. Hammond, and R. Cattaneo. 2000. Characterization of a region of the measles virus hemagglutinin sufficient for its dimerization. J. Virol. 746485-6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Plemper, R. K., A. L. Hammond, D. Gerlier, A. K. Fielding, and R. Cattaneo. 2002. Strength of envelope protein interaction modulates cytopathicity of measles virus. J. Virol. 765051-5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stone-Hulslander, J., and T. G. Morrison. 1997. Detection of an interaction between the HN and F proteins in Newcastle disease virus-infected cells. J. Virol. 716287-6295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stone-Hulslander, J., and T. G. Morrison. 1999. Mutational analysis of heptad repeats in the membrane-proximal region of Newcastle disease virus HN protein. J. Virol. 733630-3637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takimoto, T., G. L. Taylor, H. C. Connaris, S. J. Crennell, and A. Portner. 2002. Role of the hemagglutinin-neuraminidase protein in the mechanism of paramyxovirus-cell membrane fusion. J. Virol. 7613028-13033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tanabayashi, K., and R. W. Compans. 1996. Functional interaction of paramyxovirus glycoproteins: identification of a domain in Sendai virus HN which promotes cell fusion. J. Virol. 706112-6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsurudome, M., M. Kawano, T. Yuasa, N. Tabata, M. Nishio, H. Komada, and Y. Ito. 1995. Identification of regions on the hemagglutinin-neuraminidase protein of human parainfluenza virus type 2 important for promoting cell fusion. Virology 213190-203. [DOI] [PubMed] [Google Scholar]
- 44.Wang, Z., and R. M. Iorio. 1999. Amino acid substitutions in a conserved region in the stalk of the Newcastle disease virus HN glycoprotein spike impair its neuraminidase activity in the globular domain. J. Gen. Virol. 80749-753. [DOI] [PubMed] [Google Scholar]
- 45.Wang, Z., A. M. Mirza, J. Li, P. J. Mahon, and R. M. Iorio. 2004. An oligosaccharide at the C-terminus of the F-specific domain in the stalk of the human parainfluenza virus 3 hemagglutinin-neuraminidase modulates fusion. Virus Res. 99177-185. [DOI] [PubMed] [Google Scholar]
- 46.White, J. R., V. Boyd, G. S. Crameri, C. J. Duch, R. K. van Laar, L. F. Wang, and B. T. Eaton. 2005. Location of, immunogenicity of and relationships between neutralization epitopes on the attachment protein (G) of Hendra virus. J. Gen. Virol. 862839-2848. [DOI] [PubMed] [Google Scholar]
- 47.Xu, K., K. R. Rajashankar, Y. P. Chan, J. P. Himanen, C. C. Broder, and D. B. Nikolov. 2008. Host cell recognition by the henipaviruses: crystal structures of the Nipah G attachment glycoprotein and its complex with ephrin-B3. Proc. Natl. Acad. Sci. USA 1059953-9958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yin, H. S., R. G. Paterson, X. Wen, R. A. Lamb, and T. S. Jardetzky. 2005. Structure of the uncleaved ectodomain of the paramyxovirus (hPIV3) fusion protein. Proc. Natl. Acad. Sci. USA 1029288-9293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yin, H. S., X. Wen, R. G. Paterson, R. A. Lamb, and T. S. Jardetzky. 2006. Structure of the parainfluenza virus 5 F protein in its metastable, prefusion conformation. Nature 43938-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu, M., E. Hansson, J. P. Langedijk, B. T. Eaton, and L. F. Wang. 1998. The attachment protein of Hendra virus has high structural similarity but limited primary sequence homology compared with viruses in the genus Paramyxovirus. Virology 251227-233. [DOI] [PubMed] [Google Scholar]
- 51.Yuan, P., T. B. Thompson, B. A. Wurzburg, R. G. Paterson, R. A. Lamb, and T. S. Jardetzky. 2005. Structural studies of the parainfluenza virus 5 hemagglutinin-neuraminidase tetramer in complex with its receptor, sialyllactose. Structure (Cambridge) 13803-815. [DOI] [PubMed] [Google Scholar]
- 52.Zaitsev, V., M. von Itzstein, D. Groves, M. Kiefel, T. Takimoto, A. Portner, and G. Taylor. 2004. Second sialic acid binding site in Newcastle disease virus hemagglutinin-neuraminidase: implications for fusion. J. Virol. 783733-3741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhu, Z., A. S. Dimitrov, K. N. Bossart, G. Crameri, K. A. Bishop, V. Choudhry, B. A. Mungall, Y. R. Feng, A. Choudhary, M. Y. Zhang, Y. Feng, L. F. Wang, X. Xiao, B. T. Eaton, C. C. Broder, and D. S. Dimitrov. 2006. Potent neutralization of Hendra and Nipah viruses by human monoclonal antibodies. J. Virol. 80891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]