Abstract
Objective
To determine the age- and ethnicity-specific prevalence of decreased visual acuity (VA) in White and African-American preschool aged children.
Design
Cross-sectional study.
Participants
The Baltimore Pediatric Eye Disease Study is a population-based evaluation of the prevalence of ocular disorders in children aged 6 through 71 months in Baltimore, Maryland, United States. Among 4,132 children identified, 3,990 eligible children (97%) were enrolled and 2,546 children (62%) were examined. This report focuses on 1,714 of 2,546 examined children (67%) who were aged 30 through 71 months.
Methods
Field staff identified 63,737 occupied dwelling units in 54 census tracts. Parents or guardians of eligible participants underwent an in-home interview and eligible children underwent a comprehensive eye examination including optotype VA in children aged 30 months and older with protocol-specified retesting of children with VA worse than an age-appropriate standard.
Main Outcome Measures
The proportion of children aged 30 through 71 months testable for VA and the proportion with decreased VA as defined by preset criteria.
Results
VA was testable in 1,504 of 1,714 children (87.7%) 30 through 71 months of age. It was decreased at the initial test (wearing glasses if brought to the clinic) in both eyes of 7 of 577 White children (1.21%, 95% Confidence Interval [CI] = 0.49, 2.50) and 13 of 725 African-American children (1.79%, 95% CI = 0.95, 3.08), a difference that is not statistically significant. Decreased VA in both eyes after retesting was found in 3 of 598 White children (0.50%, 95% CI = 0.10, 1.48) and 8 of 757 African-American children (1.06%, 95% CI = 0.45, 2.10), also not statistically significantly different. Uncorrected ametropia explained the decreased VA on initial testing in ten of the twenty children.
Conclusions
Decreased VA in both eyes of children 30 through 71 months of age at presentation in urban Baltimore was 1.2% among White children and 1.8% among African-American children. After re-testing within 60 days of the initial exam and with children wearing best refractive correction, the rate of decreased VA in both eyes was 0.5% among Whites and 1.1% among African-Americans.
Keywords: visual acuity, children, prevalence, risk factors, methods
Introduction
Decreased visual acuity (VA) may affect the quality of life of children. When vision loss is present at a young age, the adverse impact is felt over the many remaining years of life. There is little information on the epidemiology of vision loss and ocular disease among preschool aged children (<72 months of age) in the United States. Previous studies of VA and vision impairment in young children have been clinic-based,1,2,3,4 included only school-aged children,5 performed in selected high-risk populations,6 imputed from claims data,7 or used surveys such as the National Health and Nutrition Examination Survey of 1971−1972 which were limited to older children.8 These studies have not permitted accurate estimation of population prevalence of decreased VA or the severity of eye disease among preschool aged children.
To address this lack of information about the prevalence and causes of visual impairment in the preschool population of the United States, we assessed VA in an urban population-based sample of non-Hispanic Whites and African-American children six months through 71 months of age.
Methods
Study Design
The Baltimore Pediatric Eye Disease Study (BPEDS) was designed to estimate and compare the prevalence of decreased VA, strabismus, amblyopia, and refractive error in a population-based sample of non-Hispanic White (hereafter called White) and African-American children 6 through 71 months of age living in Baltimore. All study activities were approved by the Committee on Human Subjects Research at the Johns Hopkins Bloomberg School of Public Health, the Battelle Centers for Public Health Research and Evaluation Institutional Review Board (IRB), and the IRB of the Maryland Department of Health and Mental Hygiene.
The study enrolled subjects from 54 contiguous census tracts in northeastern and eastern Baltimore City and adjacent portions of Baltimore County. Prior to contacting the households, an introductory letter was mailed to all residential dwelling units along with a BPEDS brochure. Households were identified through a door-to-door census. In the first 10 census tracts we performed the initial screening for eligible children by telephone. Parental response to phone calls was poor. Therefore, we converted screening to door-to-door canvassing in each neighborhood. A household resident was defined as anyone who considered the household his or her permanent residence, lived and slept at the residence most of the time, or lived in the household at least six months of the year. Using this definition, eligibility criteria were: (1) age five to 70 months on the day of the household screening, and (2) parent or legal guardian confirmation that the participant resided in one of the selected BPEDS census tracts. For those houses with eligible children, an adult resident answered a questionnaire about basic demographic and socioeconomic characteristics of the household as well as the eye health of each eligible child. All phone and field interviewers were trained and certified by the investigators. A minimum of 5 attempts was made to contact the occupants of each eligible dwelling unit in the study area, with these spread over different days and time periods (daytime and early evening of weekdays and weekends).
All enrolled subjects were invited to attend the study clinic for a detailed interview and ophthalmic examination. At the clinic the parent/guardian of the enrolled child participated in a detailed interview covering: (1) health care coverage and utilization; (2) basic medical history; (3) ocular history; (4) pregnancy and neonatal history; (5) tobacco and alcohol use during pregnancy; (6) presence or absence of developmental delay; (7) motor milestones; (8) socioeconomic status; and (9) quality of life (using the age-appropriate Pediatric Quality of Life Inventory (PedsQoL).9 The PedsQoL is a 23-item generic health status instrument that assesses five domains: physical functioning, emotional functioning, psychosocial functioning, social functioning, and school functioning.
The clinical examination was performed by study-certified personnel including an ophthalmic technician and a pediatric-trained optometrist. Testing included the following procedures performed in the listed order:
The Randot Preschool Stereoacuity test (Stereo Optical Company, 3539 N. Kenton Avenue, Chicago, IL) measuring random dot stereoacuity from 800 to 40 arc seconds at near. Administered to all participants 30 months of age or older.
Cover/uncover testing (unilateral cover test) at distance and near. If there was a previously prescribed spectacle correction, it was worn for the initial measurement and then the cover test was repeated without correction.
Simultaneous prism and cover test (SPCT) measurement if a strabismus was present during cover/uncover testing. If there was a previously prescribed spectacle correction, it was worn for the initial measurement and then the SPCT was repeated without correction.
Prism and alternate cover test measurement if a strabismus or phoria was present during cover/uncover testing. If there was a previously prescribed spectacle correction, it was worn for the initial measurement and then the test was repeated without correction.
Assessment of versions and ductions.
Prism and alternate cover test in side gazes for assessment of comitancy.
Hirschberg and modified Krimsky tests (if required): The Hirschberg test was performed if the examiner (1) was unable to perform cover/uncover testing at near to determine the presence, direction, and/or laterality of strabismus, or (2) as a precursor to the modified Krimsky test, when it was not possible to obtain an SPCT measurement at near. If a strabismus was present, the modified Krimsky test was performed to measure the strabismus.
Fixation preference testing using a 12 prism diopter base-down prism at near 0.3 meter. Fixation was graded as “normal” if there was spontaneous alternation between the right and left eyes or if a fixation preference reversed after switching the prism to the fellow eye. Fixation was graded as “likely normal” if fixation with the non-preferred eye was held for ≥ 3 seconds OR during a smooth pursuit movement OR through a blink before refixation to the preferred eye occurred. It was graded as “momentary” if fixation with the non-preferred eye was held for 1 to < 3 seconds or not through a pursuit or blink. It was graded as “no fixation” if refixation with the preferred eye occurred in < 1 second when the occluder was removed from the preferred eye. Patients with momentary or no fixation were considered to have reduced vision in that eye.
Monocular VA was tested using single optotypes (HOTV) surrounded with bars on the Electronic Visual Acuity (EVA) system and the Amblyopia Treatment Study (ATS) protocol.3, 10 VA testing included a pretest to assess testability, a rapid screening phase to obtain an approximation of the acuity threshold, threshold testing, a rest and a second attempt to establish threshold. We prospectively defined VA to be decreased if the better of the two threshold values obtained was worse than 20/40 in children 4 to <6 years of age, and if worse than 20/50 in children < 4 years of age.
Anterior segment and pupillary evaluations. The anterior segment was evaluated using a handheld or stand-mounted slit lamp. A direct ophthalmoscope was used when slit evaluation was not possible. Pupillary responses were tested with a handlight.
Cycloplegia was attained by administering one drop of 0.5% proparacaine, one drop of cyclopentolate (0.5% if child was 1 year of age or younger and 1.0% if child was older than 1 year), and one drop of 2.5% phenylephrine. One additional drop of cyclopentolate (concentration dependent on age as above) was administered after waiting 5 minutes. The presence of cycloplegia was confirmed 30 minutes after the second drop with dynamic retinoscopy. A third drop was administered to those children with persistent accommodation.
Height and weight measurements. Height or length was measured using a Shorr length board/stadiometer (Shorr Productions, Olney, MD). Length was measured in children less than 24 months of age and height was measured in children 24 months and older. Weight was measured using a Seca 4802 digital floor scale (Scale-tronix, White Plains, NY).
Lensometry was performed if the child was wearing spectacles.
Axial length measurement was conducted using the IOLMaster (Carl Zeiss Meditec, Dublin, CA), for children 30 months of age or older.
Cycloplegic autorefraction and keratometry was measured using the Retinomax autorefractor (Nikon, Inc, Melville, NY). A confidence interval of 8, 9, or 10 derived by the instrument was required for the measurement to be considered reliable. If the reliability measure was less than 8, autorefraction was repeated up to three times.
Cycloplegic streak retinoscopy was performed, if a reliable cycloplegic autorefraction measurement could not be obtained.
Noncycloplegic streak retinoscopy was performed if cycloplegic drops could not be administered or were refused.
Examination of the fundus through a dilated pupil.
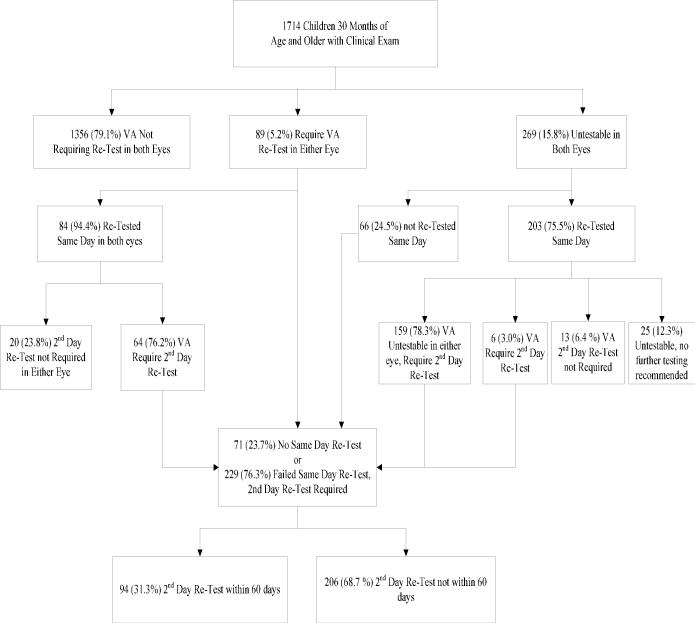
VA was retested during the same visit for children who met at least one of the following criteria: (1) Any child with 20/32 or worse (including “unables”) in one eye and two lines or greater interocular difference in VA, (2) VA in one or both eyes of: 20/60 or worse (including “unables”) when < 4 years of age or 20/50 or worse (including “unables”) when ≥ 4 years of age. VA retesting was performed with the child wearing full refractive error correction identified with cycloplegic autorefraction (or streak retinoscopy if the autorefraction reliability with the Retinomax was less than 8) (Figure 1).
Those children who continued to meet the criteria for decreased vision after the same-day VA retest were asked to return on another day for a final VA measure. Testing was performed with full cycloplegia-determined correction for myopic children and with cycloplegic-determined correction for hypermetropic children cut symmetrically by 1.50D with a minimum correction of plano. We prospectively stipulated that this test had to take place within 60 days of the initial examination to be included in the final VA assessment. Some children who were untestable after same-day testing were testable on a subsequent day. Thus the total number of testable children increased when the results of all tests are included in the analyses. The 151 children who had home-visit examinations had all of the testing above except for axial length measurement and lensometry.
Figure 1.
Flow of Visual Acuity (VA) Examination in the Baltimore Pediatric Eye Disease Study
For analysis of VA we considered each eye separately. We are reporting the VA: 1) At presentation (“Presenting VA”); 2) The better VA on day one (the better of the presenting acuity or the same day retest if the child met the criteria for retest described above, “Best Same-Day VA”), and; 3) The best measured VA within 60 days of the initial clinical examination (best of presenting acuity, retest on the same day if required, and retest within 60 days if required, “Best Measured VA”). The latter data set includes the results of the additional retesting of children with reduced vision in either eye, but not all subjects were able to be re-tested. In cases where same day repeat testing and/or repeat testing on a separate day were not performed the single best measured VA was used.
Statistical Analysis
SAS Version 9.1.3 (SAS Institute, Cary, NC) was used for all statistical analyses. Statistically significant differences in participation rates by socioeconomic, demographic and health status were assessed with chi-square tests. Logistic regression was used to assess whether testability of VA was associated with age, race and sex. The Poisson distribution was used to construct 95% confidence intervals for the prevalence estimates.
Results
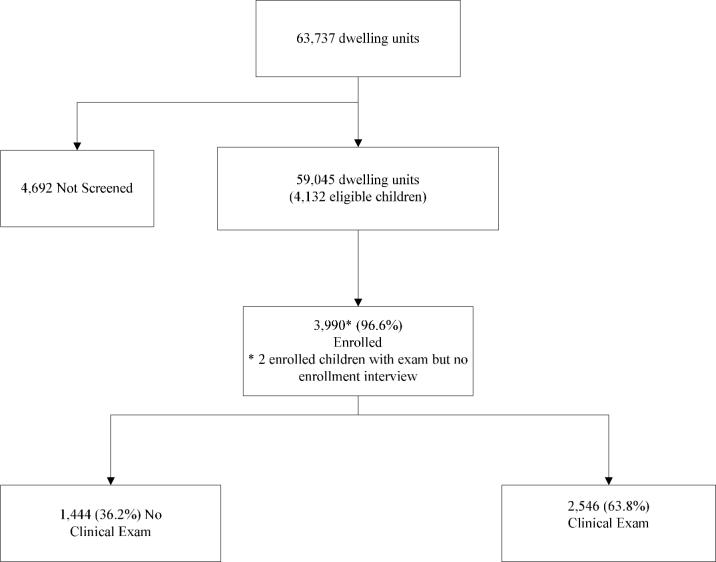
A total of 63,737 occupied dwelling units were identified in 54 census tracts, of which 59,045 (93%) responded to household screening for eligible children. Occupants of 3% of the units refused the household screening and an additional 4% were unable to be contacted despite a minimum of 5 visits to the housing unit. Data collection was conducted between November 2003 and May 2007. We enrolled 3,990 (97%) of the 4,132 eligible children (Figure 2) and examined a total of 2,546 children (151 of whom were examined in their homes) with an overall response rate of 64% (62% of all eligible subjects). Based on data obtained during the enrollment interview, children who received a clinic or home visit examination were similar to those who were not examined on the following characteristics: race/ethnicity, sex, parent-rated eye health of the child, the proportion of parents reporting that the child had difficulty seeing in the past year, the proportion of parents reporting that the child had a prior diagnosis of an eye problem, and parent-rated general health of the child (Table 1). However, response rates to the clinical examination (in the clinic or at home) varied by a number of other characteristics. Children 13 to 24 months of age were less likely to have a clinical examination than children in other age groups. Those with reported health problems at birth were more likely to undergo a clinical evaluation (13.2% of attendees versus 12.0% of non-attendees, p < 0.05), and the primary care giver was less likely to be working, (35.8% working versus 38.4%, p < 0.05) and was more likely to have a college education among attendees versus those not attending a clinical examination (16.8% versus 14.7%, p < 0.05).
Figure 2.
Enrollment of Children in the Baltimore Pediatric Eye Disease Study
Table 1.
Characteristics of Children Attending the Exam in the Baltimore Pediatric Eye Disease Study*
| Age (years)** | Clinic Attendees | Total Enrolled |
|---|---|---|
| n (% response) | ||
| < 1 | 214 (64.7) | 331 |
| 1 | 449 (59.4) | 756 |
| 2 | 480 (63.7) | 754 |
| 3 | 504 (67.3) | 749 |
| 4 | 497 (65.4) | 760 |
| 5 | 400 (62.8) | 638 |
| Ethnic Group | ||
| White | 1030 (64.1) | 1607 |
| Black | 1268 (63.7) | 1990 |
| Other | 218 (64.5) | 338 |
| Sex | ||
| Female | 1237 (65.2) | 1898 |
| Male | 1309 (62.6) | 2092 |
| Eyesight Both Eyes | ||
| Excellent | 1481 (63.5) | 2334 |
| Very good | 623 (62.7) | 993 |
| Good | 330 (66.5) | 496 |
| Fair | 67 (72.8) | 92 |
| Poor | 13 (56.5) | 23 |
| Blind | 4 (100.0) | 4 |
| Difficulty Seeing in the Past Year | ||
| No | 2415 (63.7) | 3793 |
| Yes | 92 (66.7) | 138 |
| Ever Diagnosed with Eye Problem | ||
| No | 2417 (64.1) | 3773 |
| Yes | 103 (61.0) | 169 |
| Born with Health Problems* | ||
| No | 2194 (62.8) | 3492 |
| Yes | 333 (70.3) | 474 |
| Primary Caregiver Working* | ||
| No | 1631 (66.5) | 2451 |
| Yes | 908 (59.4) | 1528 |
| Primary Caregiver Education* | ||
| < 6 yrs | 2 (66.7) | 3 |
| 6 − 8 yrs | 45 (64.3) | 70 |
| 9 − 11 yrs | 367 (60.8) | 604 |
| 12 yrs | 1038 (62.5) | 1662 |
| 13 − 15 yrs | 652 (62.5) | 1043 |
| >= 16 yrs | 426 (73.3) | 581 |
| General Health | ||
| Excellent | 1548 (63.1) | 2452 |
| Very Good | 633 (63.7) | 994 |
| Good | 297 (67.5) | 440 |
| Fair | 39 (65.0) | 60 |
| Poor | 3 (75.0) | 4 |
Based on parent/guardian report
p < 0.05 comparing attendees to non-attendees
2 (0.05%) enrolled (2 of whom are attendees) missing age
55 (1.4%) enrolled (30 of whom are attendees) missing ethnicity
48 (1.2%) enrolled (28 of whom are attendees) missing eye health
59 (1.5%) enrolled (39 of whom are attendees) missing difficulty seeing
48 (1.2%) enrolled (26 of whom are attendees) missing eye diagnosis
24 (0.6%) enrolled (19 of whom are attendees) missing health problems
11 (0.3%) enrolled (7 of whom are attendees) missing caregiver work status
27 (0.7%) enrolled (16 of whom are attendees) missing caregiver education
40 (1.0%) enrolled (26 of whom are attendees) missing general health
Visual Acuity
Children younger than 30 months of age were tested using a standardized fixation preference protocol. We found this test to be unreliable for detecting decreased vision among children 30 through 71 months of age (see companion paper).11 Therefore we are uncertain of its validity for classifying VA for the age group less than 30 months of age and thus do not report acuity based on fixation preference testing in that group.
The Amblyopia Treatment Study VA testing protocol was administered to all children aged 30 months and older.3 Testability improved with age (Table 2). Testability was 67.2% for those 30 to less than 48 months of age compared to 97.2% for those 48 to less than 72 months of age (p < 0.0001, Table 2). Testability was lower among African-Americans compared to Whites after adjusting for age and sex (Odds Ratio [OR] = 0.72 (95% CI: 0.53, 0.98), p < 0.04). Boys less than 48 months of age were less testable than girls less than 48 months of age after adjusting for age and race (OR = 0.49 (95% CI: 0.34, 0.71).
Table 2.
Presenting Visual Acuity in the Better Seeing Eye among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 5 (10.6) | 5 (11.1) | 24 (28.9) | 18 (22.0) | 30 (29.4) | 35 (38.5) | 44 (42.7) | 34 (42.0) | 69 (50.4) | 66 (60.6) | 70 (57.4) | 64 (64.6) | 75 (61.5) | 50 (71.4) |
| 20/25 | 12 (25.5) | 20 (44.4) | 21 (25.3) | 34 (41.5) | 33 (32.4) | 34 (37.4) | 34 (33.0) | 26 (32.1) | 52 (38.0) | 27 (24.8) | 31 (25.4) | 24 (24.2) | 28 (23.0) | 10 (14.3) |
| 20/32 | 28 (59.6) | 17 (37.8) | 27 (32.5) | 27 (32.9) | 30 (29.4) | 20 (22.0) | 20 (19.4) | 17 (21.0) | 14 (10.2) | 14 (12.8) | 19 (15.6) | 7 (7.1) | 14 (11.5) | 5 (7.1) |
| 20/40 | 2 (4.3) | 2 (4.4) | 3 (3.6) | 2 (2.4) | 4 (3.9) | 2 (2.2) | 3 (2.9) | 2 (2.5) | 1 (0.7) | 2 (1.8) | 2 (1.6) | 2 (2.0) | 2 (1.6) | 3 (4.3) |
| <20/40 | 0 (0.0) | 1 (2.2) | 7 (8.4) | 1 (1.2) | 5 (4.9) | 0 (0.0) | 2 (1.9) | 2 (2.5) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 2 (2.0) | 3 (2.5) | 2 (2.9) |
| Total Testable | 47 | 45 | 82 | 82 | 102 | 91 | 113 | 81 | 137 | 109 | 122 | 99 | 122 | 70 |
| Decreased VA* | 0 (0.0) | 1 (2.2) | 5 (6.1) | 0 (0.0) | 2 (2.0) | 0 (0.0) | 2 (1.8) | 2 (2.5) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 2 (2.0) | 3 (2.5) | 2 (2.9) |
| Untestable (n, % of all tested) | 80 (63.0) | 46 (50.5) | 38 (31.7) | 27 (24.8) | 18 (15.0) | 10 (9.9) | 5 (4.2) | 5 (5.8) | 6 (4.2) | 6 (5.2) | 1 (0.8) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
A decrease in optotype VA was diagnosed based on an age-dependent set of prospectively defined criteria (see Methods). Data presented here are for testable children. Twelve White (1.8%) and 14 African-American (1.6%) children presented with glasses and thus, by protocol, were tested using that correction. Presenting VA was decreased in both eyes of 7 of 577 White children (1.21%, 95% CI = 0.49, 2.50) and 13 of 725 African-American children (1.79%, 95% CI = 0.95, 3.08, Table 2). The age- and sex-adjusted relative odds of decreased Presenting VA in White compared to African-American children was 0.66 (95% CI = 0.26, 1.66), which was not statistically significant. The prevalence of decreased Same-Day VA in both eyes (after retesting with spectacle correction) was lower for Whites with 3 of 586 (0.51%, 95% CI = 0.10, 1.50), but nearly identical for African-Americans with 12 of 739 (1.62%, 95% CI = 0.84, 2.84, Table 3). The age- and sex-adjusted relative odds of decreased Same-Day VA in White compared to African-American children was 0.27 (95% CI = 0.08, 0.97), a statistically significant finding.
Table 3.
Best Same Day Visual Acuity in the Better Seeing Eye among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 5 (9.4) | 6 (12.5) | 24 (27.6) | 18 (21.7) | 30 (29.1) | 35 (37.6) | 55 (48.3) | 34 (41.5) | 69 (50.4) | 66 (59.5) | 70 (56.9) | 64 (64.7) | 76 (62.3) | 50 (71.4) |
| 20/25 | 13 (24.5) | 22 (45.8) | 22 (25.3) | 34 (41.0) | 34 (29.8) | 35 (37.6) | 34 (29.8) | 28 (34.2) | 53 (38.7) | 27 (24.3) | 31 (25.2) | 25 (25.3) | 30 (24.6) | 12 (17.1) |
| 20/32 | 30 (56.6) | 17 (35.4) | 27 (31.0) | 28 (33.7) | 30 (29.1) | 21 (22.6) | 21 (18.4) | 17 (20.7) | 14 (10.2) | 17 (15.3) | 21 (17.1) | 7 (7.1) | 12 (9.8) | 5 (7.1) |
| 20/40 | 3 (5.7) | 2 (4.2) | 4 (4.6) | 2 (2.4) | 6 (5.8) | 2 (2.2) | 3 (2.6) | 2 (2.4) | 1 (0.7) | 1 (0.9) | 1 (0.8) | 2 (2.0) | 3 (2.5) | 3 (4.3) |
| <20/40 | 2 (3.8) | 1 (2.1) | 10 (11.5) | 1 (1.2) | 3 (2.9) | 0 (0.0) | 1 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 1 (0.8) | 0 (0.0) |
| Total Testable | 53 | 48 | 87 | 83 | 103 | 93 | 114 | 82 | 137 | 111 | 123 | 99 | 122 | 70 |
| Decreased VA* | 2 (3.8) | 1 (2.1) | 8 (9.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 1 (0.8) | 0 (0.0) |
| Untestable (n, % of all tested) | 74 (58.3) | 43 (47.3) | 33 (37.9) | 26 (23.9) | 17 (14.2) | 8 (7.9) | 4 (3.4) | 4 (4.7) | 6 (4.2) | 4 (3.5) | 0 (0.0) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Children with reduced vision were asked to return for an additional test of VA on a separate day. No active treatment (e.g., patching, spectacles) was prescribed during the interim. Testing at that visit was performed with appropriate correction in trial frames (see Methods, Best Measured VA). Best Measured VA was decreased in both eyes of 3 of 594 White children (0.51%, 95% CI = 0.10, 1.48) and 8 of 753 African-American children (1.06%, 95% CI = 0.45, 2.10, Table 4). The age- and sex-adjusted relative odds of decreased Best Measured VA in White compared to African-American children was 0.44 (95% CI = 0.12, 1.66), which is not statistically significant.
Table 4.
Best Measured Visual Acuity in the better eye among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 7 (11.3) | 7 (13.2) | 26 (27.4) | 18 (20.2) | 30 (28.0) | 35 (37.2) | 55 (48.3) | 35 (42.7) | 69 (50.4) | 66 (59.5) | 70 (56.9) | 64 (64.7) | 76 (62.3) | 50 (71.4) |
| 20/25 | 16 (25.8) | 22 (41.5) | 24 (25.3) | 37 (41.6) | 36 (33.6) | 36 (38.3) | 34 (29.8) | 27 (32.9) | 54 (39.4) | 27 (24.2) | 31 (25.2) | 25 (25.3) | 30 (24.6) | 12 (17.1) |
| 20/32 | 34 (54.8) | 19 (35.8) | 30 (31.6) | 30 (33.7) | 32 (29.9) | 21 (22.3) | 22 (19.3) | 17 (20.7) | 13 (9.5) | 18 (15.3) | 22 (18.9) | 8 (8.1) | 12 (9,8) | 5 (7.1) |
| 20/40 | 3 (4.8) | 3 (5.7) | 8 (8.4) | 2 (2.2) | 6 (5.6) | 2 (2.1) | 2 (1.8) | 2 (2.4) | 1 (0.7) | 1 (0.9) | 0 (0.0) | 1 (1.0) | 3 (2.5) | 3 (4.3) |
| <20/40 | 2 (3.2) | 2 (3.8) | 7 (7.4) | 2 (2.2) | 3 (2.8) | 0 (0.0) | 1 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 1 (0.8) | 0 (0.0) |
| Total Testable | 62 | 53 | 95 | 89 | 107 | 94 | 114 | 82 | 137 | 111 | 123 | 99 | 122 | 70 |
| Decreased VA* | 2 (3.2) | 1 (1.9) | 4 (4.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 1 (0.8) | 0 (0.0) |
| Untestable (n, % of all tested) | 65 (51.2) | 38 (41.8) | 25 (20.8) | 20 (18.3) | 13 (10.8) | 7 (6.9) | 4 (3.4) | 4 (4.7) | 6 (4.2) | 4 (3.5) | 0 (0.0) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Six girls younger than 48 months of age (1.7%) had decreased Best Measured VA versus one boy (0.3%, p = 0.04). There were no differences in the prevalence of decreased Best Measured VA between boys and girls in the 48 through 71 month age range (Table 5).
Table 5.
Best Measured Visual Acuity in the Better Seeing Eye among Children 30−71 months of age by sex in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| F N=128 | M N=116 | F N=110 | M N=139 | F N=114 | M N=132 | F N=98 | M N=131 | F N=130 | M N=148 | F N=127 | M N=120 | F N=110 | M N=111 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 8 (10.5) | 7 (13.7) | 20 (20.6) | 27 (26.5) | 34 (32.4) | 42 (38.5) | 43 (45.7) | 59 (46.8) | 60 (47.2) | 87 (61.7) | 65 (51.2) | 83 (70.3) | 72 (65.5) | 77 (69.4) |
| 20/25 | 24 (31.5) | 17 (33.3) | 29 (29.9) | 39 (38.2) | 37 (35.2) | 43 (37.4) | 32 (34.0) | 36 (28.6) | 47 (37.0) | 39 (27.7) | 40 (31.5) | 22 (18.6) | 21 (19.1) | 25 (22.5) |
| 20/32 | 36 (47.4) | 23 (45.1) | 36 (37.1) | 28 (27.5) | 28 (26.7) | 29 (22.0) | 17 (18.1) | 24 (19.1) | 18 (14.2) | 14 (9.9) | 21 (16.5) | 11 (9.3) | 14 (12.7) | 5 (4.5) |
| 20/40 | 5 (6.6) | 3 (5.9) | 5 (5.2) | 6 (5.9) | 4 (3.8) | 4 (2.2) | 1 (1.1) | 5 (3.0) | 2 (1.6) | 1 (0.7) | 1 (0.8) | 1 (0.9) | 3 (2.7) | 3 (2.7) |
| <20/40 | 3 (4.0) | 1 (2.0) | 7 (7.2) | 2 (2.0) | 2 (1.9) | 1 (0.0) | 1 (1.1) | 2 (1.6) | 9 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.9) | 0 (0.0) | 1 (0.9) |
| Total Testable | 76 | 51 | 97 | 102 | 105 | 119 | 94 | 126 | 127 | 141 | 127 | 118 | 110 | 111 |
| Decreased VA* | 3 (3.9) | 0 (0.0) | 3 (3.1) | 1 (1.0) | 0 (0.0) | 0 (0.0) | 1 (1.1) | 2 (1.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 1 (0.9) |
| Untestable (n, % of all tested) | 52 (40.6) | 65 (56.0) | 13 (11.8) | 37 (26.6) | 9 (7.9) | 13 (9.8) | 4 (4.1) | 5 (3.8) | 3 (2.3) | 7 (4.7) | 0 (0.0) | 2 (1.7) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those > = 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Four of the 7 White children with decreased Presenting VA in both eyes (or reduced in one eye and the other eye not testable) had refractive error as the cause (Table 6). The other three White children with bilateral decreased Presenting VA had other causes for decreased acuity; one with bilateral amblyopia (Best Measured VA = 20/100), one with oculocutaneous albinism (Best Measured VA = 20/63), and one with no explanation for decreased vision (Best Measured VA = 20/50). Six of the 13 African-American children with bilateral decreased Presenting VA had refractive error as the primary cause, while three improved on retesting with no explanation for decreased VA at presentation (i.e., there was no reason for decreased vision on the first test). The final four African American children with bilateral decreased Presenting VA had decreased VA after all testing (Best Measured VA). Two of these four had bilateral amblyopia (best measured vision 20/50 and 20/63) and the other two had no explanation for decreased vision (best measured vision of 20/63 and 20/800).
Table 6.
Causes of Bilaterally Decreased Presenting Visual Acuity in Children 30 - <72 Months of Age
| Age (months) | Presenting VA (20/*) | Best-Measured VA (20/*) | Explanation |
|---|---|---|---|
| White Children who Improved | |||
| 67 | 63 | 32 | hyperopia |
| 61 | 63 | 32 | myopia |
| 68 | 50 | 40 | astigmatism |
| 49 | 50 | 25 | astigmatism |
| White Children with Decreased Vision after All Testing | |||
| 48 | 50 | No Improvement | no explanation |
| 64 | 125 | 100 | amblyopia |
| 32 | 63 | No Improvement | albinism |
| African American Children Who Improved | |||
| 58 | 63 | 25 | myopia |
| 68 | 63 | 40 | myopia |
| 68 | 63 | 25 | myopia |
| 45 | 63 | 40 | myopia |
| 31 | unable | 20 | testability |
| 50 | 50 | 32 | astigmatism |
| 39 | 320 | 20 | testability |
| 45 | 200 | 40 | testability |
| 37 | 63 | 25 | myopia |
| 37 | unable | 25 | testability |
| 36 | 63 | 32 | testability |
| African American Children with Decreased Vision after Testing | |||
| 36 | 800 | 800 | no explanation |
| 38 | 63 | 63 | no explanation |
| 66 | 50 | 50 | amblyopia |
| 50 | 63 | 63 | amblyopia |
| 36 | unable | 800 | no explanation |
| 36 | unable | 800 | nystagmus |
| 31 | unable | 160 | no explanation |
| 32 | unable | 125 | no explanation |
VA = visual acuity
In addition to these children who were defined as having decreased Presenting VA, an additional four African-American children who were untestable at presentation were testable on retesting and had decreased VA with best measured vision of 20/800 (2 children), 20/160, and 20/125. There was no explanation for three of these children, while one child with 20/800 vision had manifest nystagmus. The two African-American children with unexplained vision loss of 20/800 (retinas appeared normal) were twins and had been born prematurely with very low birth weight.
Decreased VA in one or both eyes was seen in 20 of 577 White children at presentation (3.5%, 95% CI = 2.0, 5.0, available at http://aaojournal.org), 22 of 586 White children after retesting on the first day (“Same Day VA” = 3.8%, 95% CI = 2.2, 5.3, Table 8, available at http://aaojournal.org), and 22 of 598 White children after repeat testing on a subsequent day (“Best Measured VA” =3.7%, 95% CI 2.2, 5.2, Table 9, available at http://aaojournal.org). Decreased VA in one or both eyes was found in 32 of 725 African-American children at presentation (4.4%, 95% CI = 2.9, 5.9, Table 7), 39 of 739 after retesting on the first day (5.3%, 95% CI = 3.7, 6.9, Table 8), and 41 of 757 (5.4%, 95% CI =3.7, 6.9, Table 9) after repeat testing on a separate day. None of these differences in prevalence rates of decreased vision in one or both eyes when comparing African American children to White children were statistically significant.
Table 8.
Worse Eye Same Day Visual Acuity among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 1 (1.9) | 1 (1.2) | 11 (12.6) | 8 (9.6) | 15 (14.6) | 21 (22.6) | 32 (28.1) | 16 (19.5) | 44 (32.1) | 41 (36.9) | 47 (38.2) | 41 (41.4) | 54 (44.3) | 36 (51.4) |
| 20/25 | 8 (15.1) | 14 (29.2) | 18 (20.7) | 22 (26.5) | 33 (32.0) | 33 (35.5) | 37 (32.5) | 32 (39.0) | 47 (34.3) | 33 (29.7) | 28 (22.8) | 37 (37.4) | 27 (22.1) | 18 (25.7) |
| 20/32 | 29 (54.7) | 23 (47.9) | 35 (40.2) | 45 (54.2) | 35 (34.0) | 31 (33.3) | 36 (31.6) | 23 (28.1) | 34 (24.8) | 26 (23.4) | 36 (29.3) | 11 (11.1) | 30 (24.6) | 8 (11.4) |
| 20/40 | 13 (24.5) | 8 (16.7) | 12 (13.8) | 6 (7.2) | 12 (11.7) | 8 (8.6) | 5 (4.4) | 7 (8.5) | 6 (4.4) | 7 (6.3) | 5 (4.1) | 4 (4.0) | 4 (3.3) | 2 (2.9) |
| <20/40 | 2 (3.8) | 2 (4.2) | 11 (12.6) | 2 (2.4) | 8 (7.8) | 0 (0.0) | 4 (3.5) | 4 (4.9) | 6 (4.4) | 4 (3.6) | 7 (5.7) | 6 (6.1) | 7 (5.7) | 6 (8.6) |
| Total Testable | 53 | 48 | 87 | 83 | 103 | 93 | 114 | 82 | 137 | 111 | 123 | 99 | 122 | 70 |
| Decreased VA* | 2 (3.8) | 2 (4.2) | 9 (10.3) | 0 (0.0) | 4 (3.9) | 0 (0.0) | 4 (3.5) | 4 (4.9) | 6 (4.4) | 4 (3.6) | 7 (5.7) | 6 (6.1) | 7 (5.7) | 6 (8.6) |
| Untestable (n, % of all tested) | 74 (58.3) | 43 (47.3) | 33 (37.9) | 26 (23.9) | 17 (14.2) | 8 (7.9) | 4 (3.4) | 4 (4.7) | 6 (4.2) | 4 (3.5) | 0 (0.0) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Table 9.
Best Measured Visual Acuity in the worse eye among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 2 (3.2) | 1 (1.9) | 12 (12.6) | 8 (9.0) | 15 (14.0) | 21 (22.3) | 32 (28.1) | 16 (19.5) | 44 (38.2) | 41 (36.9) | 47 (38.2) | 41 (41.4) | 54 (44.3) | 36 (51.4) |
| 20/25 | 10 (16.1) | 15 (28.3) | 18 (18.9) | 24 (27.0) | 35 (32.7) | 34 (36.2) | 37 (32.5) | 32 (39.0) | 28 (22.8) | 33 (29.7) | 28 (22.8) | 37 (27.4) | 27 (22.1) | 18 (25.7) |
| 20/32 | 33 (53.2) | 25 (47.2) | 37 (38.9) | 48 (53.9) | 37 (34.6) | 31 (33.0) | 36 (31.6) | 23 (28.1) | 36 (29.3) | 26 (23.4) | 36 (29.3) | 11 (11.1) | 30 (24.6) | 8 (11.4) |
| 20/40 | 13 (21.0) | 9 (17.0) | 16 (16.8) | 6 (6.7) | 12 (11.2) | 8 (8.5) | 5 (4.4) | 7 (8.5) | 5 (4.1) | 7 (6.3) | 5 (4.1) | 4 (4.0) | 4 (3.3) | 2 (2.9) |
| <20/40 | 4 (6.5) | 3 (5.7) | 12 (12.6) | 3 (3.4) | 8 (7.5) | 0 (0.0) | 4 (3.5) | 4 (4.9) | 7 (5.7) | 4 (3.6) | 7 (5.7) | 6 (6.1) | 7 (5.7) | 6 (8.6) |
| Total Testable | 62 | 53 | 95 | 89 | 107 | 94 | 114 | 82 | 137 | 111 | 123 | 99 | 122 | 70 |
| Decreased VA* | 4 (6.5) | 2 (3.8) | 9 (9.6) | 0 (0.0) | 4 (3.7) | 0 (0.0) | 4 (3.5) | 4 (4.9) | 6 (4.4) | 4 (3.6) | 7 (5.7) | 6 (6.1) | 7 (5.7) | 6 (8.6) |
| Untestable (n, % of all tested) | 65 (51.2) | 38 (41.8) | 25 (20.8) | 20 (18.3) | 13 (10.8) | 7 (6.9) | 4 (3.4) | 4 (4.7) | 6 (4.2) | 4 (3.5) | 0 (0.0) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Table 7.
Presenting Visual Acuity in the Worse Seeing Eye among Black and White Children 30−71 months of age in the Baltimore Pediatric Eye Disease Study
| Visual Acuity | Age in Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30−35 | 36−41 | 42−47 | 48−53 | 54−59 | 60−65 | 66−71 | ||||||||
| B N=127 | W N=91 | B N=120 | W N=109 | B N=120 | W N=101 | B N=118 | W N=86 | B N=143 | W N=115 | B N=123 | W N=101 | B N=122 | W N=70 | |
| n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | n (Prev %) | |
| ≥20/20 | 1 (2.1) | 1 (2.2) | 11 (13.3) | 8 (9.8) | 15 (14.7) | 21 (23.1) | 32 (31.4) | 16 (19.8) | 44 (32.1) | 41 (37.6) | 47 (38.5) | 41 (41.4) | 54 (44.3) | 37 (52.9) |
| 20/25 | 8 (17.0) | 12 (26.7) | 18 (21.7) | 22 (26.8) | 33 (32.4) | 32 (35.2) | 36 (35.0) | 32 (39.5) | 47 (34.3) | 33 (30.3) | 28 (23.0) | 37 (37.4) | 27 (22.1) | 18 (25.7) |
| 20/32 | 27 (57.4) | 22 (48.9) | 25 (30.1) | 44 (53.7) | 35 (34.3) | 30 (33.0) | 36 (35.0) | 22 (27.2) | 34 (24.8) | 25 (22.9) | 36 (29.5) | 11 (11.1) | 30 (24.6) | 8 (11.4) |
| 20/40 | 11 (23.4) | 8 (17.8) | 11 (13.3) | 6 (7.3) | 12 (11.8) | 8 (8.8) | 5 (4.9) | 7 (8.6) | 6 (4.4) | 7 (6.4) | 5 (4.1) | 4 (4.0) | 4 (3.3) | 2 (2.9) |
| <20/40 | 0 (0.0) | 2 (4.4) | 7 (8.4) | 2 (2.4) | 7 (6.9) | 0 (0.0) | 4 (3.9) | 4 (4.9) | 6 (4.4) | 3 (2.9) | 6 (4.9) | 6 (6.1) | 7 (5.7) | 5 (7.1) |
| Total Testable | 47 | 45 | 82 | 82 | 102 | 91 | 113 | 81 | 137 | 109 | 122 | 99 | 122 | 70 |
| Decreased VA* | 0 (0.0) | 2 (4.4) | 6 (7.3) | 0 (0.0) | 3 (2.9) | 0 (0.0) | 4 (3.5) | 4 (4.9) | 6 (4.4) | 3 (2.8) | 6 (4.9) | 6 (6.1) | 7 (5.7) | 5 (7.1) |
| Untestable (n, % of all tested) | 80 (63.0) | 46 (50.5) | 38 (31.7) | 27 (24.8) | 18 (15.0) | 10 (9.9) | 5 (4.2) | 5 (5.8) | 6 (4.2) | 6 (5.2) | 1 (0.8) | 2 (2.0) | 0 (0.0) | 0 (0.0) |
Prev % = Prevalence defined as the proportion of persons in visual acuity category among those who were testable.
Decreased visual acuity was defined as VA worse than 20/50 for children < 4 years and VA worse than 20/40 for those >= 4 years, out of all those who were testable
B = African American; W = White, Prev = prevalence; VA = visual acuity
Discussion
The prevalence of decreased VA in both eyes of children 30 through 71 months of age at presentation in urban Baltimore was low. The prevalence of bilateral decreased Presenting VA was 1.2% among White children and 1.8% among African-American children, which are not statistically significantly different. After re-testing within 60 days of the initial exam with children wearing best refractive correction, the prevalence of decreased Best Measured VA in both eyes was 0.5% among Whites and 1.1% among African-Americans (also not statistically significant). The most common cause of bilateral decreased Presenting VA was refractive error, accounting for half of those presenting with decreased VA. For six of the ten children with decreased Best Measured VA, we could find no explanation. Most likely this decreased VA was due to poor cooperation with testing. Only one child who met the legal definition of blindness had a clear explanation for this decreased VA, having manifest nystagmus with best measured vision of 20/800.
Unilateral decreased VA affected 3.7% of the Whites and 5.3% of the African-Americans (after all protocol-specified retesting and while wearing correction, i.e., “Best Measured VA”), which was not statistically different. African-Americans had slightly higher rates of decreased Best Measured VA in one or both eyes compared with Whites even after adjusting for age and sex, but this was not a statistically significant finding. This difference was due to a number of African-American children with no explanatory ocular findings, indicating that this finding may have related to the lower rate of “testability” among African-Americans.
We found that almost all children older than 41 months of age could be tested using the ATS VA protocol. Between 36 and 41 months about two-thirds of African-Americans and three-quarters of White children were testable on initial testing. Between 30 and 36 months, only about half of children could perform the test. These findings confirm an early report on testability of this protocol in which (as in the present study) about two-thirds of children three years of age were found to be testable.3 In addition to African-American children having lower testability (after adjustment for age and sex), boys of both races were significantly more likely to be untestable than girls after adjusting for age and race.
There are no published comparable population-based studies of VA in children 30 through 71 months of age, although the Los Angeles Multi-Ethnic Pediatric Eye Disease Study (which uses the same examination protocol as the present study) is about to publish results for African American and Latino children. The Sydney Myopia Study, a school-based vision survey of six-year-old children, reported that at presentation 0.9% of children had VA <20/40 in the better eye while 2.8% of subjects had decreased VA in the worse eye.12,. Much of the decreased VA at presentation was caused by uncorrected or undercorrected refractive error. Despite the age difference of our patients, the findings are similar to our White population.
Prevalence rates of decreased VA in children 5 − 15 years of age from developing countries (the Refractive Error Study in Children [RESC] studies) were higher than in the present study.13 - 18 Among African school aged children in South Africa the rates of presenting and best corrected visual acuity (BCVA) worse than 20/40 in the better eye were 1.4% and 1.2%, respectively, with 2.7% having presenting VA less than 20/40 in at least one eye.13 A study using the same design in Shunyi County, People's Republic of China found the prevalence of presenting bilateral decreased vision to be 10.9%, but that BCVA < 20/40 was present in 0.5% of the population.14 A separate study from southern China found rates of 10.3% and 0.62%, respectively.15 In rural south India the rates were 2.6% and 0.78% for presenting and best corrected binocular vision < 20/40.16 A separate study from south India reported only two cases (0.1%) of vision of 20/60 or worse among 1,250 children six to nine years of age, with none having severe vision loss.17 In Nepal the rate of binocular vision < 20/40 was 2.8% presenting and 1.4% best-corrected, 18 and in Chile rates were higher with 3.3% having best corrected vision < 20/40.19 With the exception of the studies from Chile and Nepal, it appears that best-corrected vision worse than 20/40 affects approximately 0.5% of children, a rate similar to what was found in the current study.
Our study has several limitations. The overall response rate for examination was 62%, raising the concern that children who participated in the examination were not representative of the target population. Data from the enrollment interview of parents/guardians indicate that those who were examined were similar in terms of race, gender, quality of eyesight, and occurrence of visual problems in the prior year compared to those who were not examined. However, the primary care giver of attendees was less likely to be working (presumably making attendance easier) and slightly more children who attended had parents/guardians with ≥ 16 years of education.
Another limitation is that 42.7% of children 30 through 41 months of age were untestable using the Amblyopia Treatment Study VA testing protocol.3 If the prevalence of decreased VA is higher among untestable children than among testable ones, then we have underestimated the prevalence of decreased VA. Among children who were unable to satisfactorily complete VA testing, 15.6% of White and 16.9% of African American children were not retested due to a subjective assessment made by the study optometrist that further testing would not succeed due to the behavior of the child. It is possible that some of these children truly had decreased VA, but due to our inability to obtain an accurate measure of VA, we were unable to categorize them and classified them as “untestable.” The requirement that all other untestable children undergo repeat testing of VA should have reduced the overall impact of misclassification of untestable children on the final prevalence estimates for decreased VA.
Our analysis of presenting VA included the 26 children (1.7%) who presented wearing glasses and were tested with that correction. The prevalence of decreased presenting VA may be higher or lower in other communities where spectacles may be more or less available to children in this age range. Finally, we did not obtain best-corrected VA on all subjects. Patients who had 20/40 or better VA among those 48 months and older, and 20/50 or better among those under 48 months were not retested with any indicated refractive correction. Thus, the reported VA distributions slightly underestimate best VA.
Bilateral decreased VA of White and African-American children in an urban United States population was infrequent. Uncorrected ametropia was the most common cause. Decreased VA was not consistently associated with age, race or sex in this population, although the very low rates precluded detection of potentially small but meaningful differences in prevalence.
Acknowledgments
Support: Supported by the National Eye Institute, National Institutes of Health, Bethesda, MD (EY14483)
Footnotes
Conflicts of Interest: The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
References
- 1.Simons K. Visual acuity norms in young children. Surv Ophthalmol. 1983;28:84–92. doi: 10.1016/0039-6257(83)90076-0. [DOI] [PubMed] [Google Scholar]
- 2.Sprague JB, Stock LA, Connett JE, Bromberg J. Study of chart designs and optotypes for preschool vision screening. Am Orthopt J. 1988;38:18–23. doi: 10.3928/0191-3913-19890701-09. [DOI] [PubMed] [Google Scholar]
- 3.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 4.McGraw PV, Winn B, Gray LS, Elliott DB. Improving the reliability of visual acuity measures in young children. Ophthalmic Physiol Opt. 2000;20:173–84. [PubMed] [Google Scholar]
- 5.Vision in Preschoolers (VIP) Study Group Visual acuity results in school-aged children and adults: Lea Symbols chart versus Bailey-Lovie chart. Optom Vis Sci. 2003;80:650–4. doi: 10.1097/00006324-200309000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Vision in Preschoolers (VIP) Study Group Threshold visual acuity testing of preschool children using the crowded HOTV and Lea Symbols acuity tests. J AAPOS. 2003;7:396–9. doi: 10.1016/s1091-8531(03)00211-8. [DOI] [PubMed] [Google Scholar]
- 7.Ganz ML, Xuan Z, Hunter DG. Prevalence and correlates of children's diagnosed eye and vision conditions. Ophthalmology. 2006;113:2298–306. doi: 10.1016/j.ophtha.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Roberts J, Rowland M. Refraction status and motility defects of persons 4−74 years, United States, 1971−1972. Vital Health Stat. 1978;11(206):1–124. [PubMed] [Google Scholar]
- 9.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthamol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 11.Friedman DS, Katz J, Repka MX, et al. Lack of concordance between fixation preference and HOTV optotype visual acuity in preschool children. Ophthalmology. doi: 10.1016/j.ophtha.2008.04.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robaei D, Rose K, Ojaimi E, et al. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005;112:1275–82. doi: 10.1016/j.ophtha.2005.01.052. [DOI] [PubMed] [Google Scholar]
- 13.Naidoo KS, Raghunandan A, Mashige KP, et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci. 2003;44:3764. doi: 10.1167/iovs.03-0283. [DOI] [PubMed] [Google Scholar]
- 14.Chew E, Remaley NA, Tamboli A, et al. Risk factors for esotropia and exotropia. Arch Ophthalmol. 1994;112:1349–55. doi: 10.1001/archopht.1994.01090220099030. [DOI] [PubMed] [Google Scholar]
- 15.Buch H, Vinding T, La Cour M, et al. Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology. 2004;111:53–61. doi: 10.1016/j.ophtha.2003.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Dandona R, Dandona L, Srinivas M, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–22. [PubMed] [Google Scholar]
- 17.Thulasiraj RD, Nirmalan PK, Ramakrishnan R, et al. Blindness and vision impairment in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology. 2003;110:1491–8. doi: 10.1016/S0161-6420(03)00565-7. [DOI] [PubMed] [Google Scholar]
- 18.Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive Error Study in Children: results from Mechi Zone, Nepal. Am J Ophthalmol. 2000;129:436. doi: 10.1016/s0002-9394(99)00453-5. [DOI] [PubMed] [Google Scholar]
- 19.Maul E, Barroso S, Munoz SR, et al. Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]