Abstract
We found no significant excess of fractures among Rochester, MN, residents with diabetes mellitus initially recognized in 1950–1969, but more recent studies elsewhere have documented an apparent increase in hip fracture risk. To explore potential explanations for any increase in fractures, we performed an historical cohort study among 1964 Rochester residents who first met glycemic criteria for diabetes in 1970–1994 (mean age, 61.7 ± 14.0 yr; 51% men). Fracture risk was estimated by standardized incidence ratios (SIRs), and risk factors were evaluated in Andersen-Gill time-to-fracture regression models. In 23,236 person-years of follow-up, 700 diabetic residents experienced 1369 fractures documented by medical record review. Overall fracture risk was elevated (SIR, 1.3; 95% CI, 1.2–1.4), but hip fractures were increased only in follow-up beyond 10 yr (SIR, 1.5; 95% CI, 1.1–1.9). As expected, fracture risk factors included age, prior fracture, secondary osteoporosis, and corticosteroid use, whereas higher physical activity and body mass index were protective. Additionally, fractures were increased among patients with neuropathy (hazard ratio [HR], 1.3; 95% CI, 1.1–1.6) and those on insulin (HR, 1.3; 95% CI, 1.1–1.5); risk was reduced among users of biquanides (HR, 0.7; 95% CI, 0.6–0.96), and no significant influence on fracture risk was seen with sulfonylurea or thiazolidinedione use. Thus, contrary to our earlier study, the risk of fractures overall (and hip fractures specifically) was increased among Rochester residents with diabetes, but there was no evidence that the rise was caused by greater levels of obesity or newer treatments for diabetes.
Key words: cohort study, diabetes, epidemiology, fractures, hip fracture
INTRODUCTION
We thought we had conducted a definitive study when we assessed fracture risk among all 986 Rochester, MN, residents initially diagnosed with diabetes mellitus in 1950–1969: these laboratory-confirmed cases were matched by age and sex to randomly selected community controls without diabetes, and both diabetic and control cohorts were followed for >10,000 person-years with comparable ascertainment of all clinically diagnosed fractures through review of each subject's complete community medical records.(1) Compared with controls, there was no increase in fractures other than the known association of diabetes with lower limb fractures.(2–4) Indeed, there seemed to be an overall reduction in osteoporotic fractures, with a relative risk of subsequent proximal femur (hip) fractures of only 0.8.(1) This is consistent with the fact that 82% of the study subjects had non–insulin-dependent (type 2) diabetes, and most studies have found unchanged or increased BMD in such individuals.(5) Given the quantitative relation between fracture risk and BMD of the femoral neck,(6) a 0.27 SD increase in hip BMD in patients with type 2 diabetes(7) would be expected to result in a 10% reduction in fracture risk generally and an 18% reduction in hip fractures.
However, a systematic review of more recent reports suggests that hip fracture risk is now elevated among diabetic women and men.(8) For example, in the Study of Osteoporotic Fractures, 48 of 657 elderly women with self-reported diabetes had a self-reported (but radiographically confirmed) hip fracture compared with 501 of 8997 nondiabetic women; the relative risk of hip fracture was 1.8 and was little altered by adjustments for age, body mass index (BMI), calcaneal BMD, or a host of other osteoporosis risk factors.(9) Similarly, the Iowa Women's Health Study found a 1.7-fold increase based on 38 self-reported hip fractures among 1682 postmenopausal women with self-reported diabetes.(10) Other than insulin use and longer duration of diabetes, consistent determinants of fracture risk in these patients have not been apparent.(8–14)
Presuming that these epidemiologic data are all correct, the possibility arises that fracture risk has changed substantially over time. Whereas secular trends in fracture incidence have been modest,(15,16) diabetes has increased dramatically: in Rochester, the age-adjusted incidence rose 67% in men and 42% in women between 1970 and 1994.(17) This change was accompanied by a marked increase in obesity, including a doubling of diabetic patients who were morbidly obese (BMI ≥ 40 kg/m2) when their diabetes was recognized.(18) However, fat mass protects against hip fractures by limiting impact forces during falls,(19) maintaining hip strength through skeletal loading(20) and preserving bone mass through enhanced endogenous estrogen production.(21) Therefore, one might have expected a further reduction in fracture risk over time, not an increase. Moreover, a recent meta-analysis concluded that there is no association of diabetes with distal forearm or vertebral fractures,(8) the other traditional osteoporotic fracture sites. Instead, a stronger link is usually seen with lower limb fractures, which is variously ascribed to diabetic neuropathy, peripheral vascular disease or impaired lower limb function generally rather than to osteoporosis.(1–4,9,22–24)
Regardless of the exact pathophysiology responsible for these fractures, the number of diabetic individuals in this country is rising rapidly in association with the ongoing obesity epidemic.(25) An estimated 10% of the U.S. population ⩾45 years of age will have diabetes in 2010,(26) and it is imperative to know, as a practical matter, whether their risk of fractures is really increased. Thus, we followed a new population-based cohort of patients to determine whether adult-onset diabetes is associated with an increase in fractures of all types, whether this represents a change from the past, and whether fracture risk is related to morbid obesity, diabetes treatment, or the comorbid conditions linked with diabetes.
MATERIALS AND METHODS
Rochester is well suited for disease association studies such as this because comprehensive medical records for the residents are available for review and are accessible through a centralized index to diagnoses made by essentially all medical care providers serving the local population.(27) After approval by Mayo's Institutional Review Board, this unique database (the Rochester Epidemiology Project) was used to identify 1992 Rochester residents who first met glycemic criteria for diabetes mellitus from January 1, 1970 through December 31, 1994. As described in detail elsewhere,(17) all Rochester residents who met research criteria for type 2 diabetes (i.e., onset at age ≥30 yr) were identified using a two-stage ascertainment protocol: first, residents ever assigned any diagnosis suggestive of diabetes were selected from the database, assuming that the chronic nature of the condition would ultimately lead to a clinical diagnosis for most individuals. Community medical records (including all glucose values) for each candidate case were reviewed by trained data abstractors, beginning with the date of first contact with a local health care provider until emigration, death, or December 31, 1994. Standardized criteria that approximated National Diabetes Data Group (NDDG) recommendations(28) were applied to confirm case status (i.e., two consecutive fasting plasma glucose levels ≥ 7.8 mmol/dl [140 mg/dl] or both 1- and 2-h levels ≥ 11.1 mmol/dl [200 mg/dl] during a standard oral glucose tolerance test as recorded in contemporary medical records). Individuals who failed to meet glycemic criteria, but who used oral agents or insulin for at least 2 wk or until death, were also included.
After additional approval by the Institutional Review Board, these confirmed cases were followed forward in time through their linked medical records in the community (retrospective, or historical, cohort study) until death or the most recent clinical contact. However, 19 subjects were excluded because they declined to authorize the use of their medical records for research(29); 2 additional subjects were deleted who only had gestational diabetes, and a further 7 were removed who proved not to be Rochester residents at the time they first met glycemic criteria. Thus, 1964 diabetic Rochester residents were included in this analysis. Their complete inpatient and outpatient community medical records were reviewed by trained nurse abstractors to collect information about lifestyle factors (e.g., tobacco and alcohol use, reproductive history), as well as a diverse array of conditions predisposing to secondary osteoporosis (e.g., rheumatoid arthritis, hyperparathyroidism, malabsorption syndrome) or to falls (e.g., stroke, epilepsy, parkinsonism).(30) BMI was recorded at the time diabetes criteria were met, and obesity was defined as BMI ≥30 kg/m2 and morbid obesity as BMI ≥40 kg/m2.(25) Physical activity was assessed on a six-point scale, with subjects in the highest two categories classified as physically active. In addition, detailed data were collected from contemporary clinical notes regarding the use of various classes of drugs associated with bone loss or osteoporosis treatment, as well as diabetes treatments and clinically diagnosed diabetic comorbidities (i.e., neuropathy, nephropathy, and retinopathy).
All inpatient and outpatient records at any local provider of medical care were searched for the occurrence of any fracture. Mayo Clinic records, for example, contain the details of every inpatient hospitalization, every outpatient office or clinic visit, all emergency room and nursing home care, as well as all laboratory results, all radiographic and pathology reports, including autopsies, and all correspondence with each patient.(27) The records contained the clinical history and the radiologist's report of each fracture, but the original radiographs were not available for review. Thus, the diagnosis of vertebral fracture was accepted on the basis of a radiologist's report of compression or collapse of one or more vertebrae.(31) Ascertainment of clinically evident fractures is believed to be complete.(16) Fractures were classified according to the circumstances of the injury: by convention, daily activities and falls from standing height or less were considered moderate trauma, whereas motor vehicle accidents and falls from a greater height were deemed severe trauma.
The influence of diabetes on fracture risk was evaluated using three basic methods of analysis, all carried out in SAS (SAS Institute, Cary, NC, USA). The primary analysis compared the number of fractures observed at each skeletal site (based on the first fracture of a given type per person) to the number expected in this cohort during their follow-up in the community (i.e., standardized incidence ratios [SIRs]). Expected numbers were derived by applying calendar year–, age-, and sex-specific incidence rates from the local population for these fractures(15,16,31–36) to the calendar year–, age-, and sex-specific person-years of follow-up in the diabetes cohort and summing over the strata. 95% CIs for the SIRs were calculated assuming the expected rates are fixed and the observed fractures follow a Poisson distribution.(37)
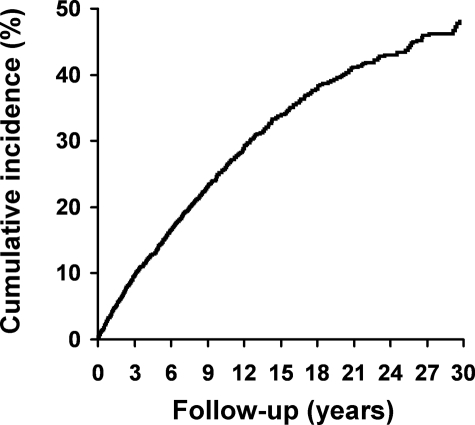
In the second method of analysis, the cumulative incidence of a new fracture (1 minus the probability of survival-free-of-fracture) was projected for up to 30 yr after the recognition of diabetes using product-limit methods.(38) In the customary approach, patients who die are censored; when the death rate is high, however, this overestimates cumulative fracture incidence as observed by attending physicians. Therefore, we treated death as a competing event in this analysis.(39) Kaplan-Meier methods were also used to assess survival, with expected death rates from the Minnesota white population. Observed and expected cumulative incidence estimates, as well as survival curves, were compared using the log-rank test.(40)
In the final approach, Andersen-Gill time-to-fracture regression models(41) were used to assess the impact of various covariates (e.g., age when glycemic criteria were met, prior fracture history, BMI, insulin use) on the subsequent risk of fracture among the diabetic patients. These models allow for the use of multiple fractures per subject while appropriately accounting for the correlation. Univariate relationships between the risk of specific fractures and each clinical characteristic under consideration were first assessed. Stepwise methods with forward selection and backward elimination were used to choose independent variables for the final models. The dependent variable was time until fracture, and the independent variables were age, sex, and the clinical characteristics at baseline; the various drug exposures were handled as time-dependent variables. For both univariate and multivariate models, the assumption of proportional hazards was examined and was not violated for the variables considered.
RESULTS
The mean ± SD age of the Rochester residents when glycemic criteria for diabetes were met was 61.7 ± 14.0 yr (median, 62 yr; range, 30–97 yr), and 992 (51%) were men. Ninety-six percent were white, reflecting the racial composition of the community (98% white in 1980). On average, these patients had been attended in the community for 32.6 yr (median, 33 yr) before recognition of their diabetes and for 11.8 yr afterward (median, 12 yr). As anticipated, survival was impaired in this cohort: By 30 yr after diabetes criteria were met, only 10% were still alive compared with an expected 24%. Ninety-five percent of the subjects were followed for fractures until the time of death or at least 2000 if they were still alive.
During 23,236 person-years of follow-up in this cohort (range, 1 day to 37 yr per subject), 700 diabetic individuals experienced 1369 different fractures. After 30 yr of follow-up, an estimated 52% of these patients had experienced at least one new fracture (Fig. 1). Almost one fifth of the fractures were caused by severe trauma (e.g., motor vehicle accidents), but the majority (71%) were attributed to moderate trauma (Table 1). Of these, 560 fractures were caused by a fall from standing height or less, whereas 414 (mostly vertebral and rib fractures) apparently occurred “spontaneously” in the course of everyday activities. The latter included 132 vertebral fractures found incidentally on radiographs taken for some other purpose. Altogether, 45 fractures (3%) resulted from a specific pathological lesion, and the etiology of the remaining 87 fractures was uncertain.
FIG. 1.
Observed cumulative incidence of any fracture among 1964 Rochester, MN, residents after first recognition of diabetes mellitus in 1970–1994, with death considered a competing risk.
Table 1.
Distribution of Fractures Among 1964 Rochester, MN, Residents After Recognition of Diabetes Mellitus in 1970–1994 by Fracture Site and Cause
| Fracture site |
Fracture cause |
|||||
|
Severe trauma |
Fall from standing |
Spontaneous |
Pathological |
Uncertain |
All causes |
|
| n (%*) | n (%*) | n (%*) | n (%*) | n (%*) | n (%†) | |
| Skull/face | 8 (28.6) | 20 (71.4) | 0 (0) | 0 (0) | 0 (0) | 28 (2.1) |
| Hands/fingers | 38 (57.6) | 25 (37.9) | 1 (1.5) | 0 (0) | 2 (3.0) | 66 (4.8) |
| Distal forearm | 11 (13.9) | 66 (83.5) | 0 (0) | 0 (0) | 2 (2.5) | 79 (5.8) |
| Proximal humerus | 7 (9.2) | 63 (82.9) | 2 (2.6) | 2 (2.6) | 2 (2.6) | 76 (5.6) |
| Other arm | 13 (34.2) | 25 (65.8) | 0 (0) | 0 (0) | 0 (0) | 38 (2.8) |
| Clavicle/scapula/sternum | 6 (20.0) | 15 (50.0) | 3 (10.0) | 4 (13.3) | 2 (6.7) | 30 (2.2) |
| Ribs | 40 (21.7) | 63 (34.2) | 38 (20.7) | 12 (6.5) | 31 (16.8) | 184 (13.4) |
| Vertebrae | 27 (6.0) | 53 (11.8) | 339 (75.2) | 20 (4.4) | 12 (2.7) | 451 (32.9) |
| Pelvis | 5 (8.8) | 35 (61.4) | 8 (14.0) | 2 (3.5) | 7 (12.3) | 57 (4.2) |
| Proximal femur | 13 (11.1) | 95 (81.2) | 1 (0.9) | 3 (2.6) | 5 (4.3) | 117 (8.5) |
| Other leg | 37 (29.4) | 81 (64.3) | 2 (1.6) | 2 (1.6) | 4 (3.2) | 126 (9.2) |
| Feet/toes | 58 (49.6) | 19 (16.2) | 20 (17.1) | 0 (0) | 20 (17.1) | 117 (8.5) |
| All sites | 263 (19.2) | 560 (40.9) | 414 (30.2) | 45 (3.3) | 87 (6.4) | 1369 (100) |
* Percentage (%) of each type of fracture.
† Percentage (%) of total.
Compared with expected rates, there was a 1.3-fold (95% CI, 1.2–1.4) increase in overall fracture risk after the recognition of diabetes. Given the large number of fractures observed, the increase was statistically significant among men (SIR, 1.4; 95% CI, 1.3–1.6) and women (SIR, 1.3; 95% CI, 1.2–1.4). The relative risk of fractures at specific skeletal sites for men and women, separately, is delineated in Table 2. For both sexes combined, statistically significant increases were seen for a number of skeletal sites, particularly the vertebrae (SIR, 3.7; 95% CI, 3.3–4.1). Overall, the relative risk of any fracture of the axial skeleton was 1.8 (95% CI, 1.6–1.9) compared with only 1.1 (95% CI, 0.99–1.2) for all limb fractures combined.
Table 2.
Fractures Observed 1964 Rochester, MN, Resedents After Recognition of Diabetes Mellitus in 1970–1994 Compared With the Numbers expected and SIRs, With 95% CIs
| Fracture site |
Women: all fractures |
Men: all fractures |
Both sexes: all fractures |
Both sexes: nonpathologic, nonincidental moderate trauma fractures |
||||||||
| Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | |
| Skull/face | 16 | 8.0 | 2.0 (1.2–3.3)* | 12 | 14.5 | 0.8 (0.4–1.4) | 28 | 22.5 | 1.2 (0.8–1.8) | 20 | 9.8 | 2.0 (1.2–3.2)* |
| Hands/fingers | 31 | 27.8 | 1.1 (0.8–1.6) | 34 | 30.8 | 1.1 (0.8–1.5) | 65 | 58.6 | 1.1 (0.9–1.4) | 27 | 25.9 | 1.0 (0.7–1.5) |
| Distal forearm | 61 | 56.6 | 1.1 (0.8–1.4) | 13 | 13.1 | 1.0 (0.5–1.7) | 74 | 69.7 | 1.1 (0.8–1.3) | 63 | 53.5 | 1.2 (0.9–1.5) |
| Proximal humerus | 53 | 25.5 | 2.1 (1.6–2.7)* | 18 | 14.2 | 1.3 (0.8–2.0) | 71 | 39.7 | 1.8 (1.4–2.3)* | 62 | 31.8 | 2.0 (1.5–2.5)* |
| Other arm | 23 | 19.8 | 1.2 (0.7–1.8) | 14 | 10.7 | 1.3 (0.7–2.2) | 37 | 30.4 | 1.2 (0.9–1.7) | 24 | 21.9 | 1.1 (0.7–1.6) |
| Clavicle/scapula/sternum | 15 | 13.0 | 1.2 (0.6–1.9) | 15 | 14.7 | 1.0 (0.6–1.7) | 30 | 27.7 | 1.1 (0.7–1.5) | 18 | 13.8 | 1.3 (0.8–2.1) |
| Ribs | 72 | 50.2 | 1.4 (1.1–1.8)* | 78 | 54.3 | 1.4 (1.1–1.8)* | 150 | 104 | 1.4 (1.2–1.7)* | 101 | 72.5 | 1.4 (1.1–1.7)* |
| Vertebrae | 198 | 63.4 | 3.1 (2.7–3.6)* | 131 | 26.2 | 5.0 (4.2–5.9)* | 329 | 89.6 | 3.7 (3.3–4.1)* | 198 | 71.0 | 2.8 (2.4–3.2)* |
| Pelvis | 40 | 31.3 | 1.3 (0.9–1.7) | 11 | 9.1 | 1.2 (0.6–2.2) | 51 | 40.4 | 1.3 (0.9–1.7) | 44 | 31.9 | 1.4 (1.0–1.8) |
| Proximal femur | 66 | 67.0 | 1.0 (0.8–1.2) | 40 | 28.4 | 1.4 (1.01–1.9)* | 106 | 95.4 | 1.1 (0.9–1.3) | 92 | 83.8 | 1.1 (0.9–1.4) |
| Other leg | 68 | 66.1 | 1.0 (0.8–1.3) | 40 | 34.5 | 1.2 (0.8–1.6) | 108 | 101 | 1.1 (0.9–1.3) | 78 | 63.8 | 1.2 (0.97–1.5) |
| Feet/toes | 72 | 46.8 | 1.5 (1.2–1.9)* | 26 | 22.1 | 1.2 (0.8–1.7) | 98 | 68.9 | 1.4 (1.2–1.7)* | 53 | 20.8 | 2.5 (1.9–3.3)* |
| Any fracture | 402 | 317 | 1.3 (1.2–1.4)* | 298 | 205 | 1.4 (1.3–1.6)* | 700 | 523 | 1.3 (1.2–1.4)* | 497 | 386 | 1.3 (1.2–1.4)* |
Note that the number of fractures observed at specific skeletal sites may differ from those reported in Table 1 because only the first fracture of each type per patient was counted in this analysis.
* p < 0.05.
Table 3.
SIRs, With 95% CIs, for Moderate Trauma Fractures (Excluding Pathologic Fractures and Those Found Incidentally) Among 1964 Rochester, MN, Residents After Recognition of Diabetes Mellitus in 1970–1994, by Follow-up Interval
| Fracture site |
Women |
Men |
||
| <10 yr[SIR (95% CI)] | ≥10 yr[SIR (95% CI)] | <10 yr[SIR (95% CI)] | ≥10 yr[SIR (95% CI)] | |
| Skull/face | 3.5 (1.7–6.4)* | 3.4 (1.2–7.3)* | 0.0 (0.0–1.2) | 2.0 (0.5–5.1) |
| Hands/fingers | 1.0 (0.5–1.8) | 1.0 (0.4–2.1) | 1.2 (0.5–2.4) | 1.1 (0.3–2.9) |
| Distal forearm | 1.1 (0.7–1.5) | 1.2 (0.7–1.9) | 1.5 (0.6–3.0) | 1.6 (0.4–4.0) |
| Proximal humerus | 1.9 (1.2–2.8)* | 3.0 (1.9–4.4)* | 1.0 (0.4–2.2) | 1.7 (0.7–3.4) |
| Other arm | 1.1 (0.5–2.0) | 0.8 (0.3–1.9) | 1.4 (0.5–3.3) | 1.5 (0.3–4.4) |
| Clavicle/scapula/sternum | 1.1 (0.4–2.6) | 1.8 (0.6–4.1) | 1.0 (0.3–2.5) | 1.7 (0.5–4.3) |
| Ribs | 1.2 (0.8–1.8) | 1.4 (0.9–2.1) | 1.6 (1.1–2.2)* | 1.4 (0.8–2.2) |
| Vertebra | 2.2 (1.7–2.7) | 2.3 (1.7–3.1)* | 5.6 (4.1–7.3)* | 3.8 (2.4–5.7)* |
| Pelvis | 1.0 (0.6–1.6) | 1.8 (1.1–2.8)* | 0.9 (0.2–2.7) | 2.6 (0.96–5.7) |
| Proximal femur | 0.7 (0.5–1.03) | 1.5 (1.04–2.1)* | 1.2 (0.7–1.9) | 1.5 (0.8–2.5) |
| Other leg | 1.0 (0.6–1.4) | 1.6 (1.0–2.3) | 1.4 (0.8–2.2) | 1.2 (0.5–2.4) |
| Feet/toes | 2.1 (1.3–3.1)* | 3.8 (2.4–5.7)* | 2.2 (0.7–5.2) | 1.4 (0.2–5.1) |
| Any fracture | 1.1 (0.97–1.3) | 1.3 (1.05–1.5)* | 1.5 (1.2–1.8)* | 1.5 (1.2–1.9)* |
* p < 0.05.
Table 4.
Univariate and Multivariate HRs* for the Development of Any New Fracture (N = 1369) Among 1964 Rochester, MN, Residents After Recognition of Diabetes Mellitus in 1970–1994
| Risk factor† | Univariate [HR (95% CI)] | Age-adjusted [HR (95% CI)] | Multivariate [HR (95% CI)] |
| Age at recognition (per 10 yr) | 1.5 (1.4–1.6) | — | 1.3 (1.2–1.4) |
| Female sex | 1.7 (1.5–2.0) | 1.6 (1.3–1.9) | 1.6 (1.3–1.9) |
| Prior osteoporotic fracture | 2.5 (1.6–3.8) | 1.8 (1.2–2.7) | 1.6 (1.03–2.4) |
| Physically active | 0.4 (0.3–0.5) | 0.5 (0.4–0.7) | 0.6 (0.5–0.8) |
| BMI (per unit increase) | 0.97 (0.95–0.98) | 0.98 (0.97–0.99) | |
| Secondary osteoporosis | 1.5 (1.3–1.8) | 1.4 (1.2–1.6) | 1.2 (1.1–1.5) |
| Renal failure | 1.8 (1.4–2.5) | 1.6 (1.2–2.2) | |
| Falling factors | 1.5 (1.2–1.7) | ||
| Neuropathy | 1.4 (1.2–1.7) | 1.4 (1.2–1.7) | 1.3 (1.1–1.6) |
| Neuropathy | 1.3 (1.1–1.5) | 1.5 (1.3–1.7) | 1.3 (1.1–1.5) |
| Use of biquanides | 0.6 (0.5–0.8) | 0.7 (0.6–0.95) | 0.7 (0.6–0.96) |
| Use of thiazolidinediones | 0.6 (0.4–0.9) | ||
| Use of corticosteroids | 2.0 (1.6–2.4) | 1.9 (1.6–2.3) | 1.6 (1.3–2.0) |
| Use of osteoporosis drugs | 3.1 (2.1–4.6) | 2.5 (1.7–3.7) | 2.0 (1.4–2.9) |
| Use of estrogens | 1.4 (1.1–1.7) | 1.5 (1.2–1.8) | |
| Use of progestins | 2.2 (1.4–3.5) | ||
| Use of SERMS | 3.1 (1.6–6.2) | 2.6 (1.3–5.3) | |
| Use of diuretics | 1.3 (1.1–1.6) | ||
| Use of anticoagulants | 1.5 (1.3–1.8) | 1.3 (1.1–1.5) | |
| Use of thyroid replacement | 1.4 (1.2–1.7) | 1.4 (1.2–1.7) |
* Proportional hazards models where the event is a fracture and the dependent variable is survival time (days) free of fracture.
† Only risk factors that were significant in the univariate and/or multivariate analysis are included in the table.
Among the diabetes-specific factors, fracture risk was increased among persons with neuropathy (HR, 1.3; 95% CI, 1.1–1.6) but not those with clinically diagnosed nephropathy (HR, 1.1; 95% CI, 0.8–1.3) or retinopathy (HR, 1.0; 95% CI, 0.8–1.2) after adjustment for age. The risk was also enhanced among the 1075 who required insulin therapy to manage their diabetes (HR, 1.3; 95% CI, 1.1–1.5), although greater duration of insulin therapy had no additional effect. No increase in fractures was seen among the 1243 users of various sulfonylureas (HR, 0.9; 95% CI, 0.8–1.1) or the 159 treated with thiazolidinediones (TZD; HR, 0.7; 95% CI, 0.5–1.1) in age-adjusted analyses. Of the latter group, 46 patients took troglitazone, 21 of whom were later switched to rosiglitazone or pioglitazone, and 113 used only the latter agents. Use of biquanides was protective even after adjusting for other risk factors (HR, 0.7; 95% CI, 0.6–0.96). There was no association of fracture risk with baseline fasting plasma glucose level (per 10 mg/dl increase: HR, 1.0; 95% CI, 0.99–1.02). The same risk and protective factors were generally seen when the outcomes were restricted to the 1061 fractures attributed to moderate trauma, the 562 osteoporotic fractures that were observed, or the 101 hip fractures alone (Table 5).
Table 5.
Multivariate HRs* for the Development of a New Moderate Trauma Fracture (N = 1061). Osteoporotic Fracture (N = 562), or Hip Fracture (N = 101) Among 1964 Rochester, MN, Residents After Recognition of Diabetes Mellitus in 1970–1994
| Risk factor† | [Moderate trauma HR (95% CI)] | Osteoporotic fracture [HR (95% CI)] | Hip fracture [HR (95% CI)] |
| Age at recognition (per 10 yr) | 1.5 (1.4–1.7) | 1.6 (1.5–1.8) | 2.0 (1.7–2.5) |
| Female sex | 1.8 (1.5–2.1) | 1.6 (1.3–2.0) | |
| Prior osteoporotic fracture | 1.7 (1.1–2.6) | ||
| Physically active | 0.6 (0.5–0.9) | 0.7 (0.5–0.98) | 0.5 (0.3–0.96) |
| BMI (per unit increase) | 0.8 (0.7–0.99) | 0.8 (0.6–0.98) | 0.95 (0.91-0.99) |
| BMI (≥30) | |||
| Secondary osteoporosis | 1.4 (1.1–1.7) | 1.4 (1.1–1.8) | |
| Falling factors | 1.2 (1.01–1.5) | 1.3 (1.1–1.7) | 5.2 (2.7–10) |
| Neuropathy | 1.4 (1.1–1.7) | ||
| Use of insulin | 1.3 (1.1–1.6) | 1.3 (1.04–1.7) | |
| Use of biquanides | 0.7 (0.5–0.97) | ||
| Use of corticosteroids | 1.5 (1.2–1.8) | 1.6 (1.3–2.0) | |
| Use of osteoporosis drugs | 2.0 (1.4–3.0) | 2.2 (1.3–3.8) | 3.9 (1.5–9.9) |
| Use of anticoagulants | 1.4 (1.1–1.7) |
* Proportional hazards models where the event is a fracture and the dependent variable is survival time (days) free of fracture.
† Only risk factors that were significant in the multivariate analysis are included in the table.
DISCUSSION
In contrast to our earlier report that Rochester residents whose diabetes was initially diagnosed in 1945–1969 had no increase in fractures generally or hip fractures specifically,(1) this update among the residents who first met glycemic criteria for diabetes in 1970–1994 found significant increases in both of these categories. This could relate partly to use in the earlier study of criteria(42) analogous to recent American Diabetes Association criteria for diabetes,(43) whereas we used the more stringent NDDG glycemic criteria(28) applicable at the time our study cohort was identified; this defined a more severe clinical spectrum of disease.(42) In addition, the update may reflect greater use of imaging modalities. Thus, the greatest disparity in results was evident for vertebral fractures. Although the previous study directly compared diabetic subjects with equally followed age- and sex-matched controls, attention to vertebral fractures likely increased over time. Indeed, the crude incidence of vertebral fractures among those with diabetes was 3 per 1000 person-years in the earlier study compared with 15 per 1000 in this analysis. Because we estimated relative risk with standardized incidence ratios, there is a potential for bias: expected numbers were determined from clinically diagnosed fracture rates in this community, but such rates do not include fractures found incidentally on radiographs and never formally diagnosed (e.g., healed rib fractures and some vertebral body deformities), which may have been overascertained among the diabetic subjects. When the analysis was limited to moderate trauma fractures, but excluding pathologic fractures and those found incidentally, the relative risk of vertebral fracture fell from 3.7 to 2.8.
The overall increase was confined to the fractures caused by moderate trauma; fractures attributed to other causes were not increased compared with expected. Moderate trauma (or fragility) fractures are the ones linked most closely with osteoporosis. Although osteoporosis is increasingly identified clinically,(44) the increased fracture risk associated with diabetes did not seem to reflect a secular trend: each calendar year increase in the date that diabetes criteria were met (index year) was associated with an HR of 1.0. As expected, greater BMI was protective of fractures,(45) and fracture risk was lower even among the diabetic patients whose BMI at diagnosis was ≥30 or ≥40 kg/m2. Fracture risk was slightly increased among the insulin users, as seen in a number of other studies,(10–13,46) but not among the users of sulfonylureas.(47) The earlier cohort of diabetic Rochester residents could have been exposed to these same agents, although insulin use was less frequent at that time.(48) Regarding the newer diabetic drugs, the biquanides were associated with a reduced risk of fractures, whereas TZDs were not associated with fracture risk after adjustment for age. The latter result conflicts with recent reports of greater bone loss among diabetic women treated with these agents(49) and an increase in appendicular fractures.(50,51) Among the 75 women in our study so treated (85% with exposure to rosiglitazone or pioglitazone) for durations up to 9 yr, the 6 appendicular fractures observed were slightly more than the 4.5 fractures expected.
There was, however, an important effect of diabetes duration. Compared with the first decade of follow-up after the recognition of diabetes, relative risk estimates for most specific fracture types, as well as overall fracture risk, were greater in follow-up beyond 10 yr. Our result is consistent with a recent Canadian study that documented an increase in osteoporotic fractures (including hip fractures) >5 yr after the diagnosis of diabetes but not before; indeed, newly diagnosed patients had reduced fracture risk.(14) This could help explain conflicting reports regarding hip fractures. Thus, elevated hip fracture risk is typically seen in studies of diabetic prevalence cohorts and patients with long follow-up(8) compared with diabetes inception cohorts with shorter follow-up where no excess hip fracture risk has been observed in some studies.(1,14,52) Greater duration of insulin therapy did not account for the influence of diabetes duration on fracture risk.
Our results are also consistent with other work showing no association of diabetes with distal forearm fractures.(8) In contrast to many previous reports,(1–4,9,22–24) however, we found no overall increase in lower limb fractures, exclusive of the hip, although there was a 1.2-fold increase in ankle fractures that was not significant. The apparent increase in vertebral fractures is also at odds with most reports,(8) but this result was inflated by ascertainment bias. We observed 329 subjects with at least one vertebral fracture compared with only 90 expected on the basis of clinically evident vertebral fracture rates in the community.(31) Because the majority of vertebral fractures do not come to clinical attention,(53) it might be preferable to base the expected number on incidence rates derived from vertebral fracture prevalence data that take into account asymptomatic vertebral deformities.(54) Using the latter data, the expected number of subjects with a vertebral fracture rises to 304 and the resulting SIR falls to 1.0 (95% CI, 0.9–1.1). This agrees with detailed morphometric studies, which have found no association of diabetes with vertebral deformities.(9,55–58)
The other risk factors for fracture among the diabetic subjects are not unexpected because they resemble those for the population generally as derived from an extensive analysis of the world's epidemiology data(59,60) and used by the World Health Organization (WHO) to create a new fracture risk prediction algorithm.(61) As expected from those analyses, fracture incidence was greater among the women and rose with age in both sexes. After adjusting for age, there was a 1.8-fold increase in fractures among the subjects who had already experienced an osteoporotic fracture. Indeed, such fractures are one of the strongest predictors of future fracture risk.(62) The new WHO fracture prediction algorithm also includes cigarette smoking and excessive alcohol intake as risk factors and higher BMI as a protective factor.(59) In this analysis, cigarette and alcohol use did not have a significant influence on future fracture risk, although the protective effect of higher BMI accords with previous work.(45)
The adverse effect of systemic corticosteroid use on fracture risk is well known,(63,64) but the WHO algorithm also considers secondary osteoporosis independently of corticosteroid use,(59) and we found an adverse effect of such conditions in aggregate. The term “secondary osteoporosis” includes many diverse disorders,(30) and we observed a particular association with renal failure in the univariate analysis (HR, 1.8; 95% CI, 1.4–2.5), although not with nephropathy generally. Renal failure has been linked to fracture risk in other studies,(65,66) in part on the basis of an increased likelihood of falling.(67) Falling contributes to fractures in diabetic patients generally,(5) and we saw a 1.5-fold increase in overall fracture risk among the subjects with one or more risk factors for falling, but this variable was not an independent predictor of fractures in the multivariate analysis after adjusting for peripheral neuropathy. The positive association of fractures with various osteoporosis drugs is because of the fact that elevated fracture risk is an indication for treatment: whereas these therapies can reduce fractures compared with untreated patients,(68) they do not eliminate the increased risk entirely.
This study has a number of strengths. The study subjects represented a large, population-based inception cohort registered at the time their diabetes was first confirmed. Because of the unique records linkage system in Rochester, which provides access to the medical records of the entire community,(27) there should be nearly complete ascertainment of diabetes by NDDG criteria to the extent that the condition came to clinical attention: one third of the population has at least one plasma glucose test annually,(17) and patients who were ever diagnosed with diabetes or a related condition were screened for the study.(69) The clinical characteristics were recorded before any knowledge of resulting fractures, which were documented in the detailed inpatient and outpatient medical records that spanned each subject's entire period of residency in the community. Fracture ascertainment should also be nearly complete because the vast majority come to medical attention.(16)
There are also corresponding limitations of a study based on medical records. One may be the generalizability of these data from a small Midwestern community that is predominantly white and better educated than the white population of the United States as a whole,(27) although the incidence of hip fractures in this community is quite comparable to national figures for U.S. whites generally.(15) More importantly, measurements of BMD or biochemical markers of bone turnover were not routinely performed, so the role of bone loss in fracture risk could not be assessed directly. However, fracture etiologies beyond osteoporosis are implied by the modest increases in overall fracture risk, especially among women, plus the failure of most other studies to find a strong association with vertebral fractures(8) along with the observation that bone density is generally increased in type 2 diabetes.(7) Unfortunately, observational studies do not represent a strong design for evaluating causality. Nonetheless, the data indicate that overall fracture risk may be modestly elevated, which is consistent with the 1.2-fold increase documented in a recent meta-analysis.(8) The increase relative to our earlier study in the community did not seem to be related to morbid obesity or use of new diabetic treatments. Instead, the risk factors for fracture were generally those proposed to identify high-risk individuals for osteoporosis treatment in the nondiabetic population.(61) This suggests that standard osteoporosis assessment strategies can be used for most patients with type 2 diabetes.
ACKNOWLEDGMENTS
The authors thank Leona Bellrichard, RN, Marcia Erickson, RN, Wendy Gay, RN, Joan LaPlante, RN, and Barbara Nolte, RN, for assistance with data collection and Mary Roberts for help in preparing the manuscript. This project was supported in part by Grants AG-04875 and AR-30582 from the National Institutes of Health, U.S. Public Health Service.
Footnotes
The authors state that they have no conflicts of interest.
REFERENCES
- 1.Heath H, III, Melton LJ, III, Chu CP. Diabetes mellitus and risk of skeletal fracture. N Engl J Med. 1980;303:567–570. doi: 10.1056/NEJM198009043031008. [DOI] [PubMed] [Google Scholar]
- 2.Daly PJ, Fitzgerald RH, Jr, Melton LJ, Ilstrup DM. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand. 1987;58:539–544. doi: 10.3109/17453678709146395. [DOI] [PubMed] [Google Scholar]
- 3.Seeley DG, Kelsey J, Jergas M, Nevitt MC. Predictors of ankle and foot fractures in older women. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1996;11:1347–1355. doi: 10.1002/jbmr.5650110920. [DOI] [PubMed] [Google Scholar]
- 4.Keegan TH, Kelsey JL, Sidney S, Quesenberry CP., Jr Foot problems as risk factors of fractures. Am J Epidemiol. 2002;155:926–931. doi: 10.1093/aje/155.10.926. [DOI] [PubMed] [Google Scholar]
- 5.Hofbauer LC, Brueck CC, Singh SK, Dobnig H. Osteoporosis in patients with diabetes mellitus. J Bone Miner Res. 2007;22:1317–1328. doi: 10.1359/jbmr.070510. [DOI] [PubMed] [Google Scholar]
- 6.Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ, III, O'Neill T, Pols H, Reeve J, Silman A, Tenenhouse A. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185–1194. doi: 10.1359/JBMR.050304. [DOI] [PubMed] [Google Scholar]
- 7.Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int. 2007;18:427–444. doi: 10.1007/s00198-006-0253-4. [DOI] [PubMed] [Google Scholar]
- 8.Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166:495–505. doi: 10.1093/aje/kwm106. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR Study of Osteoporotic Features Research Group. Older women with diabetes have an increased risk of fracture: A prospective study. J Clin Endocrinol Metab. 2001;86:32–38. doi: 10.1210/jcem.86.1.7139. [DOI] [PubMed] [Google Scholar]
- 10.Nicodemus KK, Folsom AR Iowa Women's Health Study Group. Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care. 2001;24:1192–1197. doi: 10.2337/diacare.24.7.1192. [DOI] [PubMed] [Google Scholar]
- 11.Forsen L, Meyer HE, Midthjell K, Edna TH. Diabetes mellitus and the incidence of hip fracture: Results from the Nord-Trondelag Health Survey. Diabetologia. 1999;42:920–925. doi: 10.1007/s001250051248. [DOI] [PubMed] [Google Scholar]
- 12.Ivers RQ, Cumming RG, Mitchell P, Peduto AJ Blue Mountains Eye Study. Diabetes and risk of fracture: The Blue Mountains Eye Study. Diabetes Care. 2001;24:1198–1203. doi: 10.2337/diacare.24.7.1198. [DOI] [PubMed] [Google Scholar]
- 13.Janghorbani M, Feskanich D, Willett WC, Hu F. Prospective study of diabetes and risk of hip fracture: The Nurses' Health Study. Diabetes Care. 2006;29:1573–1578. doi: 10.2337/dc06-0440. [DOI] [PubMed] [Google Scholar]
- 14.Leslie WD, Lix LM, Prior HJ, Derksen S, Metge C, O'Neil J. Biphasic fracture risk in diabetes: A population-based study. Bone. 2007;40:1595–1601. doi: 10.1016/j.bone.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 15.Melton LJ, III, Atkinson EJ, Madhok R. Downturn in hip fracture incidence. Public Health Rep. 1996;111:146–150. [PMC free article] [PubMed] [Google Scholar]
- 16.Melton LJ, III, Crowson CS, O'Fallon WM. Fracture incidence in Olmsted County, Minnesota: Comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int. 1999;9:29–37. doi: 10.1007/s001980050113. [DOI] [PubMed] [Google Scholar]
- 17.Burke JP, O'Brien P, Ransom J, Palumbo PJ, Lydick E, Yawn BP, Melton LJ, III, Leibson CL. Impact of case ascertainment on recent trends in diabetes incidence in Rochester, Minnesota. Am J Epidemiol. 2002;155:859–865. doi: 10.1093/aje/155.9.859. [DOI] [PubMed] [Google Scholar]
- 18.Leibson CL, Williamson DF, Melton LJ, III, Palumbo PJ, Smith SA, Ransom JE, Schilling PL, Narayan KM. Temporal trends in BMI among adults with diabetes. Diabetes Care. 2001;24:1584–1589. doi: 10.2337/diacare.24.9.1584. [DOI] [PubMed] [Google Scholar]
- 19.Greenspan SL, Myers ER, Maitland LA, Resnick NM, Hayes WC. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. JAMA. 1994;271:128–133. [PubMed] [Google Scholar]
- 20.Beck TJ, Oreskovic TL, Stone KL, Ruff CB, Ensrud K, Nevitt MC, Genant HK, Cummings SR. Structural adaptation to changing skeletal load in the progression toward hip fragility: The Study of Osteoporotic Fractures. J Bone Miner Res. 2001;16:1108–1119. doi: 10.1359/jbmr.2001.16.6.1108. [DOI] [PubMed] [Google Scholar]
- 21.Riggs BL, Khosla S, Melton LJ., III Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23:279–302. doi: 10.1210/edrv.23.3.0465. [DOI] [PubMed] [Google Scholar]
- 22.Cundy TF, Edmonds ME, Watkins PJ. Osteopenia and metatarsal fractures in diabetic neuropathy. Diabet Med. 1985;2:461–464. doi: 10.1111/j.1464-5491.1985.tb00683.x. [DOI] [PubMed] [Google Scholar]
- 23.Kalker AJ, Pirsch JD, Heisey D, Sollinger HW, Belzer FO, Knechtle SJ, D'Alessandro AM. Foot problems in the diabetic transplant recipient. Clin Transplant. 1996;10:503–510. [PubMed] [Google Scholar]
- 24.Bonds DE, Larson JC, Schwartz AV, Strotmeyer ES, Robbins J, Rodriguez BL, Johnson KC, Margolis KL. Risk of fracture in women with type 2 diabetes: The Women's Health Initiative Observational Study. J Clin Endocrinol Metab. 2006;91:3404–3410. doi: 10.1210/jc.2006-0614. [DOI] [PubMed] [Google Scholar]
- 25.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–1728. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 26.Boyle JP, Honeycutt AA, Narayan KM, Hoerger TJ, Geiss LS, Chen H, Thompson TJ. Projection of diabetes burden through 2050: Impact of changing demography and disease prevalence in the U.S. Diabetes Care. 2001;24:1936–1940. doi: 10.2337/diacare.24.11.1936. [DOI] [PubMed] [Google Scholar]
- 27.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 28.Anonymous. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. National Diabetes Data Group. Diabetes. 1979;28:1039–1057. doi: 10.2337/diab.28.12.1039. [DOI] [PubMed] [Google Scholar]
- 29.Melton LJ., III The threat to medical-records research. N Engl J Med. 1997;337:1466–1470. doi: 10.1056/NEJM199711133372012. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Department of Health and Human Services. Rockville, MD, USA: U.S. Department of Health and Human Services; 2004. Bone Health and Osteoporosis: A Report of the Surgeon General. [Google Scholar]
- 31.Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ., III Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992;7:221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 32.Garraway WM, Stauffer RN, Kurland LT, O'Fallon WM. Limb fractures in a defined population. I. Frequency and distribution. Mayo Clin Proc. 1979;54:701–707. [PubMed] [Google Scholar]
- 33.Melton LJ, III, Sampson JM, Morrey BF, Ilstrup DM. Epidemiologic features of pelvic fractures. Clin Orthop. 1981;155:43–47. [PubMed] [Google Scholar]
- 34.Rose SH, Melton LJ, III, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop. 1982;168:24–30. [PubMed] [Google Scholar]
- 35.Arneson TJ, Melton LJ, III, Lewallen DG, O'Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop. 1988;234:188–194. [PubMed] [Google Scholar]
- 36.Melton LJ, III, Amadio PC, Crowson CS, O'Fallon WM. Long-term trends in the incidence of distal forearm fractures. Osteoporos Int. 1998;8:341–348. doi: 10.1007/s001980050073. [DOI] [PubMed] [Google Scholar]
- 37.Cox DR. Some simple approximate tests for Poisson variates. Biometrika. 1953;40:354–360. [Google Scholar]
- 38.Kaplan EL, Meier P. Non-parametic estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 39.Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: New representations of old estimators. Stat Med. 1999;18:695–706. doi: 10.1002/(sici)1097-0258(19990330)18:6<695::aid-sim60>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 40.Kalbfleisch JD, Prentice RL. New York, NY, USA: John Wiley and Sons; 1980. The Statistical Analysis of Failure Time Data. [Google Scholar]
- 41.Therneau TM, Grambsch PM. New York, NY, USA: Springer-Verlag; 2000. Modeling Survival Data: Extending the Cox Model. [Google Scholar]
- 42.Melton LJ, III, Palumbo PJ, Dwyer MS, Chu CP. Impact of recent changes in diagnostic criteria on the apparent natural history of diabetes mellitus. Am J Epidemiol. 1983;117:559–565. doi: 10.1093/oxfordjournals.aje.a113578. [DOI] [PubMed] [Google Scholar]
- 43.Expert Committee on the Diagnosis Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 44.Stafford RS, Drieling RL, Hersh AL. National trends in osteoporosis visits and osteoporosis treatment, 1988-2003. Arch Intern Med. 2004;164:1525–1530. doi: 10.1001/archinte.164.14.1525. [DOI] [PubMed] [Google Scholar]
- 45.De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ, III, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A. Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos Int. 2005;16:1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 46.Ottenbacher KJ, Ostir GV, Peek MK, Goodwin JS, Markides KS. Diabetes mellitus as a risk factor for hip fracture in Mexican American older adults. J Gerontol A Biol Sci Med Sci. 2002;57:M648–M653. doi: 10.1093/gerona/57.10.m648. [DOI] [PubMed] [Google Scholar]
- 47.Vestergaard P, Rejnmark L, Mosekilde L. Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia. 2005;48:1292–1299. doi: 10.1007/s00125-005-1786-3. [DOI] [PubMed] [Google Scholar]
- 48.Melton LJ, III, Ochi JW, Palumbo PJ, Chu CP. Sources of disparity in the spectrum of diabetes mellitus at incidence and prevalence. Diabetes Care. 1983;6:427–431. doi: 10.2337/diacare.6.5.427. [DOI] [PubMed] [Google Scholar]
- 49.Schwartz AV, Sellmeyer DE, Vittinghoff E, Palermo L, Lecka-Czernik B, Feingold KR, Strotmeyer ES, Resnick HE, Carbone L, Beamer BA, Park SW, Lane NE, Harris TB, Cummings SR. Thiazolidinedione use and bone loss in older diabetic adults. J Clin Endocrinol Metab. 2006;91:3349–3354. doi: 10.1210/jc.2005-2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, Kravitz BG, Lachin JM, O'Neill MC, Zinman B, Viberti G, Group AS. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355:2427–2443. doi: 10.1056/NEJMoa066224. [DOI] [PubMed] [Google Scholar]
- 51.Takeda Pharmaceuticals North America Inc. Observation of an increased incidence of fractures in female patients who received long-term treatment with ACTOS (pioglitazone HCl) tablets for type 2 diabetes mellitus (Letter to Health Care Providers) 2007 http://www.fda.gov/medwatch/safety/2007/Actosmar0807.pdf.
- 52.de Liefde I, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA. Bone mineral density and fracture risk in type-2 diabetes mellitus: The Rotterdam Study. Osteoporos Int. 2005;16:1713–1720. doi: 10.1007/s00198-005-1909-1. [DOI] [PubMed] [Google Scholar]
- 53.Melton LJ, III, Wenger DE, Atkinson EJ, Achenbach SJ, Berquist TH, Riggs BL, Jiang G, Eastell R. Influence of baseline deformity definition on subsequent vertebral fracture risk in postmenopausal women. Osteoporos Int. 2006;17:978–985. doi: 10.1007/s00198-006-0106-1. [DOI] [PubMed] [Google Scholar]
- 54.Melton LJ, III, Lane AW, Cooper C, Eastell R, O'Fallon WM, Riggs BL. Prevalence and incidence of vertebral deformities. Osteoporos Int. 1993;3:113–119. doi: 10.1007/BF01623271. [DOI] [PubMed] [Google Scholar]
- 55.Melton LJ, III, Atkinson EJ, Khosla S, O'Fallon WM, Riggs BL. Secondary osteoporosis and the risk of vertebral deformities in women. Bone. 1999;24:49–55. doi: 10.1016/s8756-3282(98)00150-1. [DOI] [PubMed] [Google Scholar]
- 56.Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC, II, Black DM. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48:241–249. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 57.Lunt M, Masaryk P, Scheidt-Nave C, Nijs J, Poor G, Pols H, Falch JA, Hammermeister G, Reid DM, Benevolenskaya L, Weber K, Cannata J, O'Neill TW, Felsenberg D, Silman AJ, Reeve J. The effects of lifestyle, dietary dairy intake and diabetes on bone density and vertebral deformity prevalence: The EVOS study. Osteoporos Int. 2001;12:688–698. doi: 10.1007/s001980170069. [DOI] [PubMed] [Google Scholar]
- 58.Hanley DA, Brown JP, Tenenhouse A, Olszynski WP, Ioannidis G, Berger C, Prior JC, Pickard L, Murray TM, Anastassiades T, Kirkland S, Joyce C, Joseph L, Papaioannou A, Jackson SA, Poliquin S, Adachi JD Canadian Multicentre Osteoporosis Study Research Group. Associations among disease conditions, bone mineral density, and prevalent vertebral deformities in men and women 50 years of age and older: Cross-sectional results from the Canadian Multicentre Osteoporosis Study. J Bone Miner Res. 2003;18:784–790. doi: 10.1359/jbmr.2003.18.4.784. [DOI] [PubMed] [Google Scholar]
- 59.Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N. Assessment of fracture risk. Osteoporos Int. 2005;16:581–589. doi: 10.1007/s00198-004-1780-5. [DOI] [PubMed] [Google Scholar]
- 60.Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Glüer C, Goltzman D, Hans D, Krieg M-A, La Croix A, McCloskey E, Mellstrom D, Melton LJ, III, Pols H, Reeve J, Sanders K, Schott A-M, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–1046. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 61.Bonjour P, Clark P, Cooper C, De Laet C, Johansson H, Johnell O, Kanis J, Lau E, Melton LJ, III, Oden A, Toroptsova N. Switzerland: WHO, Geneva; 2007. Assessment of Osteoporosis at the Primary Care Level. WHO Technical Report Series. [Google Scholar]
- 62.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 63.van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: A meta-analysis. Osteoporos Int. 2002;13:777–787. doi: 10.1007/s001980200108. [DOI] [PubMed] [Google Scholar]
- 64.Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton LJ, III, Tenenhouse A, Reeve J, Silman AJ, Pols HAP, Eisman JA, McCloskey EV, Mellstrom D. A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res. 2004;19:893–899. doi: 10.1359/JBMR.040134. [DOI] [PubMed] [Google Scholar]
- 65.Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396–399. doi: 10.1046/j.1523-1755.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 66.Nickolas TL, McMahon DJ, Shane E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol. 2006;17:3223–3232. doi: 10.1681/ASN.2005111194. [DOI] [PubMed] [Google Scholar]
- 67.Dukas L, Schacht E, Stahelin HB. In elderly men and women treated for osteoporosis a low creatinine clearance of <65 ml/min is a risk factor for falls and fractures. Osteoporos Int. 2005;16:1683–1690. doi: 10.1007/s00198-005-1903-7. [DOI] [PubMed] [Google Scholar]
- 68.Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2005;353:595–603. doi: 10.1056/NEJMcp043801. [DOI] [PubMed] [Google Scholar]
- 69.Leibson CL, O'Brien PC, Atkinson E, Palumbo PJ, Melton LJ., III Relative contributions of incidence and survival to increasing prevalence of adult-onset diabetes mellitus: A population-based study. Am J Epidemiol. 1997;146:12–22. doi: 10.1093/oxfordjournals.aje.a009187. [DOI] [PubMed] [Google Scholar]