Abstract
Objective: to assess whether incident mobility disability and neighbourhood deprivation in older people are associated independent of the effects of individual socio-economic status, health behaviours and health status.
Methods: prospective cohort study with a 2-year follow-up.
Setting: the English Longitudinal Study of Ageing (ELSA), a national probability sample of non-institutionalised older people.
Participants: 4,148 participants aged 60 years and over.
Measurements: exposure was a census-based index of neighbourhood deprivation [the Index of Multiple Deprivation (IMD)]; outcomes were measured and self-reported incident mobility difficulties.
Results: neighbourhood deprivation had a statistically significant effect on physical function following adjustment for individual socio-economic factors, health behaviours and health status. Compared to those living in the least deprived 20% of neighbourhoods, those in the most deprived neighbourhoods had a risk ratio (RR) of incident self-reported mobility difficulties of 1.75 (95% CI 1.14–2.70) and RR of incident-impaired gait speed of 1.63 (95% CI 1.01–2.62). In adjusted models, 4.0 per 100 (95% CI 3.0–5.4) older adults in neighbourhoods in the least deprived 20% had incident mobility difficulties over a 2-year period, whereas 13.6 per 100 (95% CI 10.5–17.4) older adults had incident mobility difficulties in neighbourhoods in the most deprived 20%.
Conclusions: older people living in deprived neighbourhoods are significantly more likely to experience incident mobility difficulties than those in less-deprived neighbourhoods. The mechanisms underlying this relationship are unclear and research to identify mechanisms and appropriate interventions is needed.
Keywords: Elderly, walking, local, gait speed, socio-economic status, community
Introduction
Living in a deprived neighbourhood is associated with undesirable health outcomes including poor cardiovascular health [1], higher rates of mortality [2] and depression [3], and higher levels of risky health behaviours [4]. The mechanisms by which neighbourhood qualities impact health outcomes of individuals are unclear and suggested mechanisms include built environment [5], level of access to healthcare and other resources [6], and having neighbours who are themselves disadvantaged [7].
Older people may be at a heightened risk of neighbourhood effects [8]. Mental health [9, 10], cognitive function [11, 12] and self-reported physical function [13–15] have been found to be poorer among older people in deprived urban neighbourhoods. To our knowledge the relationship between neighbourhood characteristics and objective measures of impaired mobility in older people has not been examined.
Impaired mobility is predictive of nursing home entry and mortality [16], and assessing physical performance can help identify those with pre-clinical limitations who are at higher risk for developing further disability [17]. Mobility disability, by which we mean problems with walking or climbing a single set of stairs, often occurs early in the disablement process, is a basic everyday function common to most cultures, and has a negative impact on the quality of life [18, 19]. Assessing both self-reported and measured difficulties allows us to combine an objective measure of poor performance with an indication of how everyday mobility is affected [20].
This topic is important for two reasons: the significance of good mobility to older people's health and well-being, and understanding the ways in which older people's physical and social environments impact their functioning, which enables us to improve and maintain those environments. In this study, we examined the relationship between neighbourhood deprivation and incident self-reported and measured mobility difficulties in a nationally representative cohort of community-dwelling older people in England. Our hypothesis was that neighbourhood socio-economic deprivation is associated with incident mobility disability independent of the effect of individual socio-economic circumstances and health behaviours.
Methods
We used data from the English Longitudinal Study of Ageing (ELSA), a nationally representative cohort study of older adults (aged 50 years and over) in England. The baseline wave of ELSA was drawn from households participating in the Health Survey for England (HSE), an annual government-funded cross-sectional health survey, in 1998, 1999 and 2001. Households were included in ELSA if one or more individuals living there were aged 50 years or over. There were 19,924 individuals in households that responded to HSE who would have been aged 50 years by the time the ELSA sample was taken in 2002, although not all these individuals participated in HSE. A total of 2,596 of these older individuals died or were ineligible for follow-up; of the remainder, 11,392 (65.7%) became ELSA participants. Analyses of socio-demographic characteristics against census results indicated that the ELSA sample remained population representative [21].
The gait speed test (described below) was administered to those aged 60 years and over. A total of 4,148 individuals aged 60 years and over who were alive and responded in 2004, and had complete data for our exposures and outcomes of interest, were included in our analyses. This study was conducted using fully anonymised publicly available datasets and therefore no additional ethical clearance was necessary.
Measures of neighbourhood deprivation
The Index of Multiple Deprivation (IMD) 2004 is a measure based on distinct dimensions of deprivation that can be measured at the small-area level. Seven dimensions are included: income deprivation; employment deprivation; health deprivation; education, skills and training deprivation; barriers to housing and services; living environment deprivation and crime. IMD 2004 has been used to examine the association between socio-economic deprivation and a range of health and health service outcomes [12, 22–24].
Using information from the 2001 UK census, the UK Office for National Statistics (ONS) calculated IMD scores at the super output area (SOA) level [25]. These areas contain a minimum of 1,000 individuals and a mean of 1,500 individuals. There are 34,378 SOAs in England [26]. Because IMD scores at the SOA level are potentially disclosive, IMD information in ELSA is only available divided by quintiles. In this study IMD divided by quintiles was used to represent the level of socio-economic deprivation of the neighbourhoods in which study participants lived.
Outcome measures
Self-reported mobility difficulties
At both Wave 1 and Wave 2, participants were asked whether they experienced difficulties, because of a health problem, with walking 100 yards or with climbing one flight of stairs without resting. Participants were asked to exclude any difficulties that they expected to last less than 3 months. We classified incident mobility difficulty as reporting difficulties with either of these activities at Wave 2 among those who reported no difficulties with them at Wave 1.
Measured gait speed
A gait speed test was performed as part of the main ELSA interview at both Wave 1 and Wave 2. Participants were excluded if they refused to attempt the test; if they or the interviewer felt that attempting the test would be unsafe; or if questions were being answered on their behalf by someone else (a proxy interview). The test involved timing how long it took to walk a distance of 8 feet. Participants began with both feet together at the beginning of the course. The interviewer started timing as soon as a participant placed either foot down on the floor across the start line. They were asked to walk (not race) to the other end of the course at their usual speed, just as if they were walking down the street to the shops, and to walk all the way past the other end of the tape before stopping. Timing was stopped when either foot was placed down on the floor across the finish line. Participants were then asked to repeat the test by lining up their feet and walking back along the course, all the way past the other end.
We used the mean of the two recorded times. Those who had a gait speed of 0.4 m/s or slower, or who were unable to walk alone, were categorised as having impaired gait speed. A 0.4-m/s threshold is conventionally used in this 8-foot test and is intended to represent the speed at which individuals may need to be able to walk, for example, to cross the street in the time allowed to cross signals [18, 27]. Participants who did not have impaired gait speed at Wave 1 but who had impaired gait speed at Wave 2 were classified as having incident-impaired gait speed.
Adjustment for potential confounders
We entered potential confounders into our model in three stages. All models were adjusted for age and gender. In Model 1 we adjusted for rurality, classed using census information as rural, small town or urban fringe (≤10,000 inhabitants), or urban, and for population density of the area divided by quintiles. We also adjusted for the length of time for which participants reported having lived in their current location, which would be significant if those in neighbourhoods in socio-economic decline live there because they lack the health or economic resources to leave [28].
In Model 2 we adjusted for individual- and household-level socio-economic factors:
Age of completion of full-time school education: having left school at age 14 or younger, age 15, age 16 or at age 17 or older.
Household wealth, including total financial, physical and housing wealth, but not pension wealth, divided by quintiles.
In Model 3, we added the following health status and health behaviours known to be associated with physical function:
Number of co-morbidities [29], that is having been told by a doctor that they have the following conditions: diabetes, cancer, psychological or emotional problems, arthritis, stroke, high blood pressure, chronic lung disease, congestive heart failure, categorised by number 0, 1, 2, 3 or more.
Smoking status [30]: never having smoked cigarettes, having quit smoking, being a current smoker.
Body mass index (BMI) [31]; height and weight were measured by a research nurse at ELSA baseline, and we calculated BMI as weight in kilograms divided by height in metres squared. BMI was categorised as: 25 or below, 25+ to 30, 30+ to 35 and 35+.
Self-reported level of physical activity [32], categorised in four levels as: none; engaging at least once a week in sports or activities that are mildly energetic; moderately energetic; and vigorous.
Statistical analysis
Logistic regression was used to estimate the effects of neighbourhood deprivation level on physical functioning. Because the primary sampling unit in ELSA is the household, cluster correction was used to take into account the anticipated similarity between individuals living in the same household. Analyses were weighted for non-response and conducted using Stata SE Version 9.2 (StataCorp PL, College Station, Texas).
Results
Baseline characteristics of participants, and percentages of participants in each category free from self-reported mobility difficulties and measured gait speed impairment, are summarised in Table 1. Participants free from baseline mobility difficulties, both self-reported and measured, were more likely to be men, better educated, wealthy, with fewer co-morbidities, with low BMI, physically active and living in less-deprived neighbourhoods.
Table 1.
Baseline characteristics of participants
| All | No baseline self-reported mobility difficulties | No baseline gait speed impairment | ||||
|---|---|---|---|---|---|---|
| n = 4148 (% of total) | (% with no difficulty) | n = 3525 P-value | (% with no impairment) | n = 3974 P-value | ||
| Age | 60–64 | 1073 (25.9) | 959 (89.4) | 0.000 | 1051 (98.0) | 0.000 |
| 65–69 | 1086 (26.2) | 963 (88.7) | 1063 (97.9) | |||
| 70–74 | 902 (21.8) | 744 (82.5) | 861 (95.5) | |||
| 75–79 | 582 (14.0) | 479 (82.3) | 551 (94.7) | |||
| 80 + | 505 (12.2) | 380 (75.3) | 448 (88.7) | |||
| Mean length of residence (years) | 24.1 | 24.2 | 24.1 | |||
| Gender | Men | 1847 (44.5) | 1619 (87.7) | 0.000 | 1797 (97.3) | 0.000 |
| Women | 2301 (55.5) | 1906 (82.8) | 2177 (94.6) | |||
| Area type | Rural | 571 (13.8) | 495 (86.7) | 0.409 | 561 (98.3) | 0.005 |
| Small town | 96 (2.3) | 424 (85.5) | 470 (94.8) | |||
| Urban | 3081 (74.3) | 2606 (84.6) | 2943 (95.5) | |||
| Education (age of | 14 or younger | 1310 (31.6) | 1021 (77.9) | 0.000 | 1210 (92.4) | 0.000 |
| completion of schooling) | 15 | 1312 (31.6) | 1107 (84.4) | 1268 (96.7) | ||
| 16 | 666 (16.1) | 601 (90.2) | 651 (97.8) | |||
| 17 or older | 860 (20.7) | 796 (92.6) | 845 (98.3) | |||
| Wealth | Highest 20% | 871 (21.0) | 809 (92.9) | 0.000 | 856 (98.3) | 0.000 |
| 2 | 889 (21.4) | 798 (89.8) | 869 (97.8) | |||
| 3 | 889 (21.4) | 768 (86.4) | 859 (96.6) | |||
| 4 | 791 (19.1) | 648 (81.9) | 745 (94.2) | |||
| Lowest 20% | 708 (17.1) | 502 (70.9) | 645 (91.1) | |||
| Health conditions | None | 1254 (30.2) | 1199 (95.6) | 0.000 | 1238 (98.7) | 0.000 |
| One | 1606 (38.7) | 1401 (87.2) | 1545 (96.2) | |||
| Two | 942 (22.7) | 725 (77.0) | 883 (93.7) | |||
| Three | 346 (8.3) | 200 (57.8) | 308 (89.0) | |||
| Smoking | Never smoked | 1503 (36.2) | 1319 (87.8) | 0.000 | 1443 (96.0) | 0.769 |
| Ex-smoker | 2071 (49.9) | 1737 (83.9) | 1984 (95.8) | |||
| Current smoker | 574 (13.8) | 469 (81.7) | 547 (95.3) | |||
| Body Mass Index (BMI) | ≤25 | 1167 (28.1) | 1048 (89.8) | 0.000 | 1133 (97.1) | 0.000 |
| 25 to < 30 | 1956 (47.2) | 1693 (86.6) | 1885 (96.4) | |||
| 30 to < 35 | 789 (19.0) | 639 (81.0) | 749 (94.9) | |||
| 35+ | 236 (5.7) | 145 (61.4) | 207 (87.7) | |||
| Level of physical activity | None | 324 (7.8) | 180 (55.6) | 0.000 | 269 (83.0) | 0.000 |
| Mild | 605 (14.6) | 405 (67.0) | 547 (90.4) | |||
| Moderate | 2139 (51.6) | 1914 (89.5) | 2091 (97.8) | |||
| Vigorous | 1080 (26.0) | 1026 (95.0) | 1067 (98.8) | |||
| Neighbourhood deprivation | Least deprived | 979 (23.6) | 882 (90.1) | 0.000 | 954 (97.5) | 0.000 |
| 2 | 1004 (24.2) | 882 (87.9) | 982 (97.8) | |||
| 3 | 868 (20.9) | 743 (85.6) | 828 (95.4) | |||
| 4 | 731 (17.6) | 587 (80.3) | 696 (95.2) | |||
| Most deprived | 566 (13.6) | 431 (76.2) | 514 (90.8) | |||
Note: Self-reported mobility difficulties = difficulties with one or both of walking 100 yards or climbing one flight of stairs without resting.
Gait speed impairment = measured gait speed of 0.4 m/s or less.
P-values are from Pearson's chi-squared test for independence
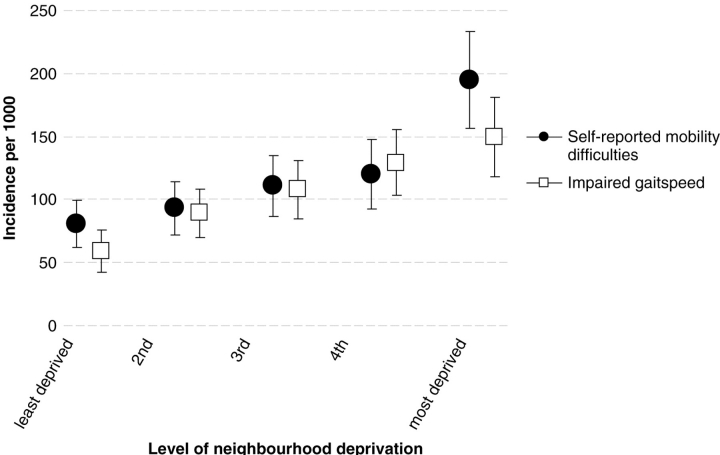
Figure 1 shows the relationship between incident mobility difficulties and level of neighbourhood deprivation. For both self-reported mobility difficulties and impaired gait speed there is a monotonic increase in the incidence rate associated with increasing neighbourhood deprivation (P for trend < 0.001). For impaired gait speed, the incidence rate in the least deprived neighbourhoods is 59.2 per 1,000 (95% CI 42.7–75.8), and in the most deprived neighbourhoods it is 149.4 per 1,000 (95% CI 117.7–181.1). For self-reported mobility difficulties, the mean incidence in the least deprived neighbourhoods is 80.3 per 1,000 (95% CI 61.6–98.9), and in the most deprived neighbourhoods it is 195.0 per 1,000 (95% CI 156.7–233.3).
Figure 1.
Rate of incident mobility difficulties after 2-year follow-up in relation to baseline level of neighbourhood deprivation (bars show 95% confidence intervals). Note: Self-reported mobility difficulties = difficulties with one or both of walking 100 yards or climbing one flight of stairs without resting. Impaired gait speed = measured gait speed of 0.4 m/s or less
Table 2 shows the outcomes of analyses in which the relationship between level of neighbourhood deprivation and incident self-reported mobility difficulties is adjusted for three different sets of potential confounders. Table 3 shows the same thing for incident-impaired gait speed. In each table there is a marked relationship between level of deprivation and our outcome of interest in Model 1, which is attenuated but remains significant when socio-economic variables are added (Model 2), and attenuated further, but still significant, when health and health behaviours are added (Model 3). For self-reported difficulties the relative risk ratio (RR) of a poor outcome in the most deprived areas compared to the least deprived is 1.75 (95% CI 1.14–2.70), and for impaired gait speed the RR is 1.63 (95% CI 1.01–2.62). A test for trend in these fully adjusted models was significant for both outcomes (RR 1.13, 95% CI 1.02–1.26 for self-reported difficulties, RR 1.12, 95% CI 1.02–1.25 for impaired gait speed).
Table 2.
Relative risk ratios of incident self-reported mobility difficulties after a 2-year follow-up (n = 3525)
| RR | Model 1 95% CI | RR | Model 2 95% CI | RR | Model 3 95% CI | ||
|---|---|---|---|---|---|---|---|
| Age | 1.07 | 1.06, 1.09 | 1.07 | 1.05, 1.09 | 1.07 | 1.05, 1.09 | |
| Gender | Female | 1.44 | 1.15, 1.79 | 1.45 | 1.16, 1.81 | 1.39 | 1.09, 1.78 |
| Area type | Rural | — | — | — | |||
| Small town | 1.55 | 0.94, 2.56 | 1.35 | 0.81, 2.23 | 1.18 | 0.71, 1.97 | |
| Urban | 1.23 | 0.77, 1.97 | 1.12 | 0.70, 1.79 | 1.00 | 0.61, 1.61 | |
| Duration of residence (years) | 1.00 | 0.99, 1.01 | 1.00 | 0.99, 1.01 | 1.00 | 0.99, 1.01 | |
| Population density | 1.00 | 0.89, 1.12 | 1.00 | 0.89, 1.12 | 1.01 | 0.89, 1.14 | |
| Education (age of completion of schooling) | 14 or younger | — | — | ||||
| 15 | 0.98 | 0.72, 1.33 | 0.93 | 0.68, 1.29 | |||
| 16 | 0.79 | 0.55, 1.14 | 0.84 | 0.57, 1.23 | |||
| 17 or older | 0.82 | 0.57, 1.18 | 0.89 | 0.61, 1.30 | |||
| Wealth | Highest 20% | — | — | — | |||
| 2 | 1.65 | 1.10, 2.44 | 1.62 | 1.07, 2.47 | |||
| 3 | 2.09 | 1.38, 3.16 | 1.92 | 1.25, 2.93 | |||
| 4 | 1.73 | 1.12, 2.68 | 1.55 | 0.99, 2.43 | |||
| Lowest 20% | 2.20 | 1.41, 3.42 | 1.74 | 1.09, 2.77 | |||
| Health conditions | None | — | |||||
| One | 1.87 | 1.36, 2.59 | |||||
| Two | 2.66 | 1.89, 3.75 | |||||
| Three or more | 3.42 | 2.16, 5.41 | |||||
| Smoking | Never smoked | — | |||||
| Ex-smoker | 1.35 | 1.06, 1.84 | |||||
| Current smoker | 2.08 | 1.44, 2.99 | |||||
| Body mass index (BMI) | ≤25 | — | |||||
| 25 to < 30 | 1.06 | 0.79, 1.41 | |||||
| 30 to < 35 | 1.54 | 1.11, 2.14 | |||||
| 35 + | 2.57 | 1.59, 4.17 | |||||
| Level of physical activity | None | — | |||||
| Mild | 0.68 | 1.59, 1.07 | |||||
| Moderate | 0.34 | 0.43, 0.50 | |||||
| Vigorous | 0.32 | 0.22, 0.51 | |||||
| Neighbourhood deprivation | Least deprived | — | — | — | — | ||
| 2 | 1.16 | 0.81, 1.66 | 1.04 | 0.72, 1.49 | 1.01 | 0.69, 1.48 | |
| 3 | 1.45 | 1.01, 2.09 | 1.21 | 0.83, 1.76 | 1.15 | 0.78, 1.70 | |
| 4 | 1.59 | 1.09, 2.32 | 1.27 | 0.85, 1.91 | 1.19 | 0.78, 1.81 | |
| Most deprived | 2.80 | 1.91, 4.10 | 2.04 | 1.35, 3.09 | 1.75 | 1.14, 2.70 |
Note: Self-reported mobility difficulties = self-reported difficulties with one or both of walking 100 yards or climbing one flight of stairs without resting
Table 3.
Relative risk ratios of incident gait speed impairment after a 2-year follow-up (n = 3974)
| RR | Model 1 95% CI | RR | Model 2 95% CI | RR | Model 3 95% CI | ||
|---|---|---|---|---|---|---|---|
| Age | 1.10 | 1.08, 1.12 | 1.10 | 1.08, 1.12 | 1.10 | 1.08, 1.12 | |
| Gender | Female | 1.29 | 1.03, 1.60 | 1.28 | 1.02, 1.60 | 1.16 | 0.90, 1.48 |
| Area type | Rural | — | — | — | |||
| Small town | 1.46 | 0.88, 2.42 | 1.33 | 0.81, 2.20 | 1.18 | 0.70, 1.99 | |
| Urban | 1.58 | 1.01, 2.49 | 1.52 | 0.97, 2.38 | 1.35 | 0.85, 2.16 | |
| Duration of residence (years) | 1.00 | 0.99, 1.00 | 1.00 | 0.99, 1.00 | 1.00 | 0.99, 1.01 | |
| Population density | 0.90 | 0.80, 1.02 | 0.91 | 0.80, 1.02 | 0.92 | 0.81, 1.04 | |
| Education (age of completion of schooling) | 14 or younger | — | — | ||||
| 15 | 1.10 | 0.81, 1.49 | 1.11 | 0.81, 1.53 | |||
| 16 | 0.81 | 0.55, 1.18 | 0.85 | 0.57, 1.26 | |||
| 17 or older | 0.81 | 0.56, 1.18 | 0.93 | 0.63, 1.36 | |||
| Wealth | Highest 20% | — | — | ||||
| 2 | 1.38 | 0.91, 2.10 | 1.38 | 0.90, 2.12 | |||
| 3 | 1.30 | 0.84, 2.03 | 1.19 | 0.76, 1.86 | |||
| 4 | 2.05 | 1.33, 3.16 | 1.85 | 1.19, 2.88 | |||
| Lowest 20% | 2.38 | 1.52, 3.72 | 1.84 | 1.15, 2.94 | |||
| Health conditions | None | — | |||||
| One | 1.57 | 1.10, 2.24 | |||||
| Two | 2.21 | 1.52, 3.20 | |||||
| Three or more | 4.30 | 2.85, 6.48 | |||||
| Smoking | Never smoked | — | |||||
| Ex-smoker | 1.03 | 0.78, 1.35 | |||||
| Current smoker | 1.39 | 0.96, 2.00 | |||||
| Body mass index (BMI) | ≤25 | — | |||||
| 25 to < 30 | 1.41 | 1.03, 1.94 | |||||
| 30 to < 35 | 1.59 | 1.10, 2.30 | |||||
| 35+ | 2.91 | 1.77, 4.77 | |||||
| Level of physical activity | None | — | |||||
| Mild | 0.78 | 0.52, 1.15 | |||||
| Moderate | 0.34 | 0.24, 0.50 | |||||
| Vigorous | 0.28 | 0.17, 0.44 | |||||
| Neighbourhood deprivation | Least deprived | — | — | — | |||
| 2 | 1.56 | 1.07, 2.27 | 1.42 | 0.98, 2.07 | 1.43 | 0.97, 2.11 | |
| 3 | 2.11 | 1.43, 3.09 | 1.71 | 1.15, 2.56 | 1.73 | 1.14, 2.62 | |
| 4 | 2.62 | 1.78, 3.86 | 1.90 | 1.25, 2.90 | 1.79 | 1.15, 2.78 | |
| Most deprived | 3.02 | 1.99, 4.58 | 1.87 | 1.18, 2.97 | 1.63 | 1.01, 2.62 |
Note: Gait speed impairment = measured gait speed of 0.4 m/s or less
Based on Model 3, for self-reported outcomes, 4.0 per 100 (95% CI 3.0–5.4) older adults in neighbourhoods in the least deprived 20% had incident mobility difficulties over a 2-year period, whereas 13.6 per 100 (95% CI 10.5–17.4) older adults had incident mobility difficulties in neighbourhoods in the most deprived 20%. For measured outcomes, 2.0 per 100 (95% CI 1.4–2.9) older adults in neighbourhoods in the least deprived 20% had incident mobility difficulties over a 2-year period, whereas 7.3 per 100 (95% CI 5.4–9.8) older adults had incident mobility difficulties in neighbourhoods in the most deprived 20%.
Similar trends were apparent when we analysed men and women separately (results not shown). The effect on impaired gait speed was more marked in men and the effect on self-reported mobility difficulties was more marked in women, but interaction terms were not statistically significant. In order to provide more precise estimates we present only the combined results here.
Sensitivity analysis
We conducted sensitivity analyses to test the robustness of our models. In particular, we wanted to assess the effects of additional individual- and household-level socio-economic variables. We added the following variables to our model:
Income (including income from employment, self-employment, private or state pension, benefits, assets and other sources), divided by quintiles.
Childhood socio-economic status has been shown to be predictive of physical functioning in mid-life [33], and we adjusted for participant's self-reports of his/her father's or main carer's occupation when the participant was aged 14.
Individual occupational social class, based on the UK National Statistics Socio-economic Classification Analytic Classes (NS- SEC 8).
Occupational social class of spouse or partner in the same household, also using the NS- SEC 8.
Level of education of spouse or partner, categorised as for the participant.
When we re-ran our models including these additional variables there was little change in the overall shape of the response.
A contributing factor to poor health in deprived neighbourhoods may be that the better-off tend to leave declining neighbourhoods [28]. We repeated our analyses excluding individuals who reported having lived in their current location for longer or shorter periods of time. Again, this produced little change in the shape of the responses observed.
We repeated our analyses to examine transitions in the opposite direction, i.e. looking at those who reported mobility problems at baseline but did not have them at follow-up, or had impaired gait speed at baseline but not at follow-up. Six hundred and twenty-three individuals reported mobility problems at baseline but not at follow-up, and 174 had impaired gait speed at baseline but not at follow-up. For both outcomes those who lived in deprived neighbourhoods were less likely to show improvement at follow-up, although the differences were not statistically significant. (Results of all analyses available from authors on request.)
Discussion
Community-dwelling older adults had a higher risk of incident self-reported mobility difficulties and incident-impaired gait speed if they lived in a neighbourhood with higher levels of deprivation. This relationship was attenuated but remained statistically significant when adjustment was made for individual demographic and socio-economic factors, health status and health behaviours.
To our knowledge, no previous studies have assessed the effects of neighbourhood deprivation on objectively measured mobility difficulties. Our findings are in line with studies that found higher levels of self-reported difficulties with physical function in older people in more deprived areas [12, 13]. This is the first study to use data from a nationally representative survey to assess these outcomes.
We used an objective measure of neighbourhood deprivation, the IMD (IMD 2004), calculated using national census data. Intended to capture multiple aspects of neighbourhood deprivation, IMD scores are calculated in relation to neighbourhoods with a mean population of 1,500 individuals, areas smaller and more locally specific than the 1990 US Census Tracts used in a previous study [13]. One shortcoming with IMD scores is that, because they summarise deprivation, we cannot assess how specific aspects of deprivation are associated with poor outcomes. Examining specific features of areas can help to assess the relationship between neighbourhood deprivation and individual outcomes [34]. The strongest association with poor outcomes in our analyses was with number of co-morbidities, and it may be that some residual effect of the severity of co-morbidities in people in deprived neighbourhoods partially explains the differences we observed.
These findings answer existing questions and raise new ones. The mechanisms by which neighbourhood deprivation affects health outcomes have been the subject of much recent discussion [35–38]. The exposures used here do not capture all possible variation in situation to which people are exposed. The ‘lifespace’ of individuals is broader than the areas they inhabit: people travel, work and live in areas that go far beyond the neighbourhoods where they have their homes, and simple measures of socio-economic status may leave out important aspects of this. Ignoring this poses the risk of falling into the ‘local trap’ [36] and potentially failing to account for the full range of contexts to which individuals are exposed. The IMD measure may also miss other factors more likely to affect deprived neighbourhoods, such as air quality and pollution levels [39]. Future research must look more broadly, including into the realm of culture [40], if we are to understand how living in deprived neighbourhoods impacts individual health.
An important aspect of these findings is that they indicate the importance of assessing relationships between health in later life and the socio-economic factors associated with neighbourhoods, as well as those associated with individuals and households. Previous analyses of socio-economic influences on incident mobility problems have focussed on individual or household differences, but we found that the effects of neighbourhood deprivation were of similar size to the effects of household wealth. One implication of our findings may be that even if redistribution of socio-economic resources across individuals was attempted, it might be insufficient to level out differences in health. To achieve that, direct intervention at the neighbourhood level—whether through GP practices, local government or by engaging communities in some other way—may be necessary.
Holding confounders constant, in neighbourhoods in the least deprived 20%, approximately 4 in 100 older adults had new self-reported mobility difficulties over a 2-year period, whereas 14 of 100 older adults in neighbourhoods in the most deprived 20% had new mobility difficulties. These higher levels of incident disability undoubtedly bring with them an increased burden of costs. These costs may be borne by health services [41] or informal carers [42], but are liable to affect those least able to cope with them: the inhabitants of, and health services in, the most deprived areas.
Key points
Living in a deprived neighbourhood is known to have adverse effects on individual health and is associated with self-reported mobility difficulties in older people.
We found that in community-dwelling older people, both measured and self-reported incident mobility disabilities are associated with living in a deprived neighbourhood.
These effects are independent of the effects of individual socio-economic circumstances and health behaviours.
The policy implications of these findings relate to the need for community-level interventions to address the effects of both neighbourhood and individual socio-economic inequalities upon health among older people.
Acknowledgements
Iain A. Lang is an NHS Academic Specialist Registrar in Public Health funded by the Southwest of England Public Health Training Scheme. Kenneth M. Langa is funded from US NIA Grants, K08 AG019180 and R01 AG027010.
The ELSA is co-funded by the US National Institute of Ageing, and a number of UK Government departments involved in areas related to the ageing process.
Conflicts of interest
None.
References
- 1.Winkleby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prev Med. 2007;32:97–106. doi: 10.1016/j.amepre.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davey Smith G, Hart C, Watt G, et al. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley study. J Epidemiol Community Health. 1998;52:399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galea S, Ahern J, Nandi A, et al. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol. 2007;17:171–9. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stimpson JP, Ju H, Raji MA, et al. Neighborhood deprivation and health risk behaviours in NHANES III. Am J Health Behav. 2007;31:215–22. doi: 10.5555/ajhb.2007.31.2.215. [DOI] [PubMed] [Google Scholar]
- 5.Jackson RJ. The impact of the built environment on health: an emerging field. Am J Public Health. 2003;93:1382–4. doi: 10.2105/ajph.93.9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jencks C, Mayer SE. The social consequences of growing up in a poor neighborhood. In: Lynn JLE, McGeary MHH, editors. Inner City Poverty in the United States. Washington, DC: National Academy Press; 1990. pp. 111–86. [Google Scholar]
- 8.Cagney KA, Browning CR, Wen M. Racial disparities in self-rated health at older ages: what difference does the neighborhood make? J Gerontol B Psychol Sci Soc Sci. 2005;60(4):S181–90. doi: 10.1093/geronb/60.4.s181. [DOI] [PubMed] [Google Scholar]
- 9.Aneshensel CS, Wight RG, Miller-Martinez D, et al. Urban neighborhoods and depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2007;62:S52–69. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- 10.Walters K, Breeze E, Wilkinson P, et al. Local area deprivation and urban-rural differences in anxiety and depression among people older than 75 years in Britain. Am J Public Health. 2004;94:1768–74. doi: 10.2105/ajph.94.10.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wight RG, Aneshensel CS, Miller-Martinez D, et al. Urban neighborhood context, educational attainment, and cognitive function among older adults. Am J Epidemiol. 2006;163:1071–8. doi: 10.1093/aje/kwj176. [DOI] [PubMed] [Google Scholar]
- 12.Lang IA, Llewellyn DJ, Langa KM, et al. Neighborhood deprivation, individual socioeconomic status, and cognitive function in older people: analyses from the English Longitudinal Study of Ageing. J Am Geriatr Soc. 2008;56:191–8. doi: 10.1111/j.1532-5415.2007.01557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schootman M, Andresen EM, Wolinsky FD, et al. Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans. Am J Epidemiol. 2006;163:450–8. doi: 10.1093/aje/kwj054. [DOI] [PubMed] [Google Scholar]
- 14.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. Am J Epidemiol. 2002;155:507–15. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 15.Bowling A, Barber J, Morris R, et al. Do perceptions of neighbourhood environment influence health? Baseline findings from a British survey of aging. J Epidemiol Community Health. 2006;60:476–83. doi: 10.1136/jech.2005.039032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 17.Cavazzini C, Bandinelli S, Gangemi S, et al. Screening for poor performance of lower extremity in primary care: The Camucia project. Aging Clin Exp Res. 2004;16:331–6. doi: 10.1007/BF03324560. [DOI] [PubMed] [Google Scholar]
- 18.Lan TY, Melzer D, Tom BD, et al. Performance tests and disability: developing an objective index of mobility-related limitation in older populations. J Gerontol A Biol Sci Med Sci. 2002;57:M294–301. doi: 10.1093/gerona/57.5.m294. [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–31. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 20.Reuben DB, Seeman TE, Hirsch SH, et al. Refining the categorization of physical functional status: the added value of combining self-reported and performance-based measures. J Gerontol A Biol Sci Med Sci. 2004;59:1056–61. doi: 10.1093/gerona/59.10.m1056. [DOI] [PubMed] [Google Scholar]
- 21.Taylor R, Conway L, Calderwood L. Methodology. Health, Wealth and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study Of Ageing. In: Marmot M, Banks J, Blundell R, et al., editors. London: Institute for Fiscal Studies; 2003. pp. 357–74. [Google Scholar]
- 22.Maunder P, Landes DP, Steen N. The equity of access to primary dental care for children in the North East of England. Community Dent Health. 2006;23:116–9. [PubMed] [Google Scholar]
- 23.Woods LM, Rachet B, Riga M, et al. Geographical variation in life expectancy at birth in England and Wales is largely explained by deprivation. J Epidemiol Community Health. 2005;59:115–20. doi: 10.1136/jech.2003.013003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith LK, Draper ES, Manktelow BN, et al. Socioeconomic inequalities in very preterm birth rates. Arch Dis Child Fetal Neonatal Ed. 2007;92:F11–4. doi: 10.1136/adc.2005.090308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office of the Deputy Prime Minister. The English Indices of Deprivation 2004 (revised). 1–180. London: ODPM Publications; 2004. [Google Scholar]
- 26.Bates C. Methodology used for producing ONS's Small Area Population Estimates. Popul Trends. 2006;125:30–6. (Autumn 2006) [PubMed] [Google Scholar]
- 27.Rantanen T, Guralnik JM, Ferrucci L, et al. Coimpairments as predictors of severe walking disability in older women. J Am Geriatr Soc. 2001;49:21–7. doi: 10.1046/j.1532-5415.2001.49005.x. [DOI] [PubMed] [Google Scholar]
- 28.Kawachi I, Subramanian SV. Neighbourhood influences on health. J Epidemiol Community Health. 2007;61:3–4. doi: 10.1136/jech.2005.045203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guralnik JM, LaCroix AZ, Abbott RD, et al. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137:845–57. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 30.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–69. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 31.Coakley EH, Kawachi I, Manson JE, et al. Lower levels of physical functioning are associated with higher body weight among middle-aged and older women. Int J Obes Relat Metab Disord. 1998;22:958–65. doi: 10.1038/sj.ijo.0800698. [DOI] [PubMed] [Google Scholar]
- 32.Lang IA, Guralnik JM, Melzer D. Physical activity in middle-aged adults reduces risks of functional impairment independent of its effect on weight. J Am Geriatr Soc. 2007;55:1836–41. doi: 10.1111/j.1532-5415.2007.01426.x. [DOI] [PubMed] [Google Scholar]
- 33.Guralnik JM, Butterworth S, Wadsworth MEJ, et al. Childhood socioeconomic status predicts physical functioning a half century later. J Gerontol A Biol Sci Med Sci. 2006;61:694–701. doi: 10.1093/gerona/61.7.694. [DOI] [PubMed] [Google Scholar]
- 34.Diez Roux AV, Mujahid MS, Morenoff JD, et al. Respond to “Beyond the Metrics for Measuring Neighborhood Effects”. Am J Epidemiol. 2007;165:872–3. [Google Scholar]
- 35.Mujahid MS, Diez Roux AV, Morenoff JD, et al. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 36.Pearce J, Witten K, Hiscock R, et al. Are socially disadvantaged neighbourhoods deprived of health-related community resources? Int J Epidemiol. 2007;36:348–55. doi: 10.1093/ije/dyl267. [DOI] [PubMed] [Google Scholar]
- 37.Cummins S. Commentary: investigating neighbourhood effects on health—avoiding the ‘Local Trap’. Int J Epidemiol. 2007;36:355–7. doi: 10.1093/ije/dym033. [DOI] [PubMed] [Google Scholar]
- 38.Galea S, Ahern J. Invited commentary: considerations about specificity of associations, causal pathways, and heterogeneity in multilevel thinking. Am J Epidemiol. 2006;163:1079–82. doi: 10.1093/aje/kwj177. [DOI] [PubMed] [Google Scholar]
- 39.Brown P. Race, class, and environmental health: a review and systematization of the literature. Environ Res. 1995;69:15–30. doi: 10.1006/enrs.1995.1021. [DOI] [PubMed] [Google Scholar]
- 40.Eckersley R. Is modern Western culture a health hazard? Int J Epidemiol. 2006;35:252–8. doi: 10.1093/ije/dyi235. [DOI] [PubMed] [Google Scholar]
- 41.Chan L, Beaver S, MacLehose RF, et al. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil. 2002;83:1196–201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 42.Andersson A, Levin LA, Emtinger BG. The economic burden of informal care. Int J Technol Assess Health Care. 2002;18:46–54. [PubMed] [Google Scholar]