Abstract
Rationale
Cocaine users have increased regional brain mu-opioid receptor (mOR) binding which correlates with cocaine craving. The relationship of mOR binding to relapse is unknown.
Objectives
To evaluate regional brain mOR binding as a predictor of relapse to cocaine use.
Methods
Fifteen non-treatment-seeking, adult cocaine users were housed on a closed research ward for 12 weeks of monitored abstinence, then followed for up to one year after discharge. Regional brain mOR binding was measured after one and 12 weeks using positron emission tomography (PET) with [11C]carfentanil (a selective mOR agonist). Time to first cocaine use (lapse) and to first two consecutive days of cocaine use (relapse) after discharge was based on self-report and urine toxicology.
Results
A shorter interval before relapse was associated with increased mOR binding in frontal and temporal cortical regions at one and 12 weeks of abstinence (P’s < 0.001) and with a lesser decrease in binding between one and 12 weeks (P’s < 0.0008). There were significant positive correlations between mOR binding at 12 weeks and % days of cocaine use during first month after relapse (P’s < 0.002). In multiple linear regression analysis, mOR binding contributed significantly to the prediction of time to relapse (R2 = 0.79, P < 0.001), even after accounting for clinical variables.
Conclusions
Increased brain mOR binding in frontal and temporal cortical regions is a significant independent predictor of time to relapse to cocaine use, suggesting an important role for the brain endogenous opioid system in cocaine addiction.
Keywords: cocaine, mu-opioid receptor, positron emission tomography, relapse, carfentanil, frontal cortex, temporal cortex
Introduction
There is no broadly effective treatment for cocaine addiction (Gorelick 2003; Karila, et al. 2007; Knapp, et al. 2007; Simpson, et al. 2002). Patients vary widely in their treatment response. This situation has generated a search for markers of treatment response (Ciraulo, et al. 2003). Such a marker would allow limited treatment resources to be directed towards patients who could benefit the most.
A variety of psychosocial and cocaine use variables have been found predictive of treatment response at a group level in small scale studies, including duration of cocaine use, severity of addiction, employment status, and education level (Ciraulo, et al. 2003; Hser, et al. 1999; Kampman, et al. 2002; McKay, et al. 1999; McMahon 2001; Poling, et al. 2007; Reiber, et al. 2002). The search for biological prognostic markers has also had limited success (Elkashef and Vocci 2003). EEG patterns (Prichep, et al. 1999), P300 event-related brain potentials (Bauer 1997), and peripheral measures of dopamine and serotonin function (Patkar, et al. 2003; Patkar, et al. 2004) have been predictive of relapse by cocaine addicts in treatment in small studies, but have not been replicated in larger samples or by other research groups.
We present data in support of brain mu-opioid receptor (mOR) binding as a prognostic biomarker. Animal studies show that chronic, intermittent cocaine administration (“binge” pattern) increases mOR binding (Branch, et al. 1992; Hammer 1989; Unterwald, et al. 2001; Unterwald, et al. 1994) and expression of mRNA for mOR (Azaryan, et al. 1996; Azaryan, n et al. 1996;Yuferov, et al. 1999) in specific brain regions. We have previously reported, using positron emission tomography (PET) with the radiolabeled, selective mOR agonist [11C]carfentanil, that human cocaine users show increased mOR binding in some brain regions (e.g., frontal and lateral temporal cortex, anterior cingulate) and that this increased binding is positively correlated with self-reported cocaine craving (Zubieta, et al. 1996; Gorelick, et al. 2005). mOR binding increases over the first week of monitored abstinence on a research ward, then declines toward normal values over the next 12 weeks of abstinence (Gorelick, et al. 2005). We report here that the degree of decline in mOR binding among subjects in the previous study is positively correlated with time to relapse to cocaine use after ward discharge, i.e., the greater the decline in mOR binding, the longer the time before relapse.
Methods and Materials
Subjects
Subjects were adult, non-treatment-seeking cocaine users recruited from the community. Subject eligibility criteria included current cocaine abuse or dependence by DSM-IV criteria (American Psychiatric Association 1994); current use of cocaine averaging at least 1 g per week over the prior 3 months and at least 10 days over the prior 2 weeks; urine drug tests positive for cocaine and negative for other drugs; no clinically significant current abnormalities on the screening evaluation; no history of CNS disease, head injury with loss of consciousness greater than 3 minutes, or adverse event from prior cocaine use; no current psychiatric or substance use disorder except for cocaine or tobacco; not currently taking psychoactive medication; no use of opiates more than 3 times in the prior 3 months; IQ ≥ 80. The exclusion of subjects with other current substance use disorders or more than minimal recent opiate use was designed to minimize effects on brain mOR binding from other substance use.
Applicants received a comprehensive medical and psychological evaluation, including medical history and physical examination, clinical laboratory tests, 12-lead ECG with 3-minute rhythm strip, structural magnetic resonance imaging (MRI) of the brain, Addiction Severity Index (ASI) (McLellan, et al. 1985), Diagnostic Interview Schedule (Robins, et al. 1982), and Symptom Check List-90R (SCL-90R) (Derogatis 1983).
The study was approved by the Institutional Review Boards of the National Institute on Drug Abuse (NIDA) Intramural Research Program (IRP) and the Johns Hopkins Bayview Medical Center. All subjects gave written informed consent (when not in acute drug intoxication or withdrawal) and were paid for their study participation.
Procedures
Subjects spent 3 months on the NIDA IRP closed research ward. There were usually 2–3 study subjects on the ward at any time, along with subjects from other studies. To prevent unauthorized use of drugs, no passes or visitors were allowed, personal belongings and mail were screened, and urine samples for drug testing were collected at random. No counseling, group therapy, or formal drug abuse treatment was provided. Subjects had access to cable television, video games, movies on videocassette, books, magazines, exercise equipment, arts and crafts supplies, and an enclosed court yard. While on the ward, subjects had PET scans done on three separate days: one day after ward admission (after two days for one subject, same day for one subject), about one week (6–10 days) after admission (after 18 days for one subject), and about 12 weeks (80–87 days) after admission (after 13 weeks for one subject). Subjects were not allowed to smoke for at least 30 minutes before each PET scan. Measures of self-reported mood (SCL-90R subscales for depression and anxiety) were obtained before each PET scan.
Follow-up Measures
After discharge from the ward, subjects were followed for up to one year: weekly for four weeks, monthly for the next 5 months, then at 9 and 12 months after discharge. Subjects were paid by check for each follow-up visit according to the following schedule: $40 per visit during the first 2 months, $60 per visit during the next 3 months, and $80 per visit during the last 6 months. At each visit, subjects reported the dollar amount of their cocaine use for each day since the previous visit, using a time-line follow-back method on a blank calendar (Sobell and Sobell 1992) and provided an observed urine sample for immediate on-site assay of the cocaine metabolite benzoylecgonine (Express Test #93007, Biosite Co., San Diego, CA). To maximize the validity of self-report, urine samples were obtained first, information was elicited by trained research staff in a private room when subjects were not clinically intoxicated, subjects were informed of the steps taken to ensure confidentiality (including a federal Certificate of Confidentiality for the study), and there were no adverse consequences for self-reported drug use or a positive urine drug test (Brown, et al. 1992; Hamid, et al. 1999; Harrison 1995; Nelson, et al. 1998).
Several lapse/relapse variables were calculated from the self-report data (Donovan 1996): time to lapse = number of days from ward discharge until first cocaine use; time to relapse = number of days from ward discharge until two consecutive days of cocaine use; % days of cocaine use during the 30 days following relapse (= number of days with cocaine use divided by total number of days with data). While there is no generally accepted operational definition of relapse in the drug abuse field (Maisto and Connors 2006), it is usually defined in terms of more extended use after a lapse that reflects loss of control over use (Donovan 1996; Milby, et al. 2004). For this study, we defined a relapse as two consecutive days of cocaine use, on the grounds that this would be a reliable retrospective self-report measure of use reflecting some loss of control.
The validity of subjects’ self-report about cocaine use was evaluated by comparing urine drug test results with the self-reports for the 3 days preceding the sampling day (the typical duration of persistence of benzoylecgonine in urine (Cone, et al. 2003; Preston, et al. 2002)). There was 80% overall agreement between subjects’ self-report of cocaine use and results of the urine drug tests, comparable to levels of agreement reported in large published studies (Brady, et al. 2002; Brown, et al. 1992; Harrison 1995; Hersh, et al. 1999; Nelson, et al. 1998).
PET Image Acquisition
PET scans were acquired in 2D mode on a GE 4096 Plus PET scanner (GE Medical Systems, Milwaukee, WI) using [11C]carfentanil, a specific mu-opioid agonist developed for PET imaging (Frost, Wagner, Jr. et al. 1985). Images were simultaneously collected from 15 contiguous planes with an axial field-of-view of 10.5 cm. A transmission scan of 10-min duration was obtained using rotating germanium-68 rods before injection of the radiotracer. After intravenous bolus administration of 19.5 (1.2) mCi (range = 16.3–21.1 mCi) of [11C]-carfentanil (specific activity = 3213 ± 2351 mCi/μmol, range = 1475–11090 mCi/μmol), 25 sets of images with variable time period (6 × 30 sec, 5 × 60 sec, 5 × 120 sec, 9 × 480 sec) were acquired during a 90-min period for each study. After correction for attenuation using the transmission scan, images were reconstructed in a 128 × 128 × 15 matrix with pixel size of 2 × 2 × 6.5 mm with filtered back projection methods using a ramp filter and decay-corrected.
Parameterized images for [11C]-carfentanil were generated using an automated in-house program based on Logan graphical analysis (Logan, et al. 1996) with a reference-tissue model using the occipital cortex. The fitted linear slope (10–90 minutes) generates the ratio of the total distribution (DVR) in receptor-rich region and reference tissue. As previously described, the occipital cortex value of k2 was assumed to be 0.104 min−1 (Endres, et al. 2003). DVR = DVrc/DVocc = (1+k3/k4), in which k3/k4 represents the receptor binding potential (BP). Parameterized images of BP were computed from BP = DVR-1.
Data Analyses
All scan data and parametric images were processed using SPM2 (The Welcome Department of Cognitive Neurology, Institute of Neurology, University College London) implanted in Matlab 6.5 (Mathworks, Natick, MA, USA) and Analyze™ software packages (Ver 6.0, Mayo Foundation, Rochester, MN).
The 0–90 minute average image of each study was created to provide more anatomical information for spatial normalization. The average images were spatially normalized to a [11C]-carfentanil template into a standard space (MNI, Montreal Neurological Institute). The transformation matrix provided was then applied to the corresponding parametric images. Data were then smoothed using a 10-mm FWHM Gaussian smoothing kernel to reduce residual intersubject anatomical differences, increase the signal-to-noise ratio at the expense of resolution, and increase the validity of the statistical inferences by rendering the data more normally distributed.
The smoothed BP images were proportionally scaled to the global brain binding value to yield normalized binding potential of mOR. Proportional scaling allows identification of changes in regional mOR binding that exceed those in global mean mOR binding. The mean global binding was computed on subset of data > whole mean/8. This had the effect of removing regions of very low or negative mOR binding. The analysis threshold was set to > 70% of the global mean computed by SPM2 for each subject in order to retain in the analysis only the specific mOR binding.
The relationship of regional mOR binding to lapse/relapse variables was assessed at each voxel using the general linear model in SPM2. Because of the skewed distribution of these clinical variables, they were analyzed as log transforms. The relationship between changes in mOR binding during enforced abstinence (day 1 or week 1 to week 12) and lapse/relapse variables or between mOR binding at a particular time point (week 1 or week 12) and lapse/relapse variables was evaluated with simple correlation analysis using the “Multi-subjects: conditions & covariate” option for voxel-based analysis. A correlation was considered significant if a cluster consisting of at least 50 contiguous voxels exceeded an uncorrected height threshold of P < 0.005 (T = 3.01). Clusters showing a significant correlation in the SPM analysis were subjected to additional analysis in SPSS (v. 11.5, SPSS, Inc., Chicago, IL). The mean mOR binding in the cluster (calculated using Marsbar software [Matthew Brett, http://marsbar.sourceforge.net]) was used in a linear regression analysis to calculate the R2 value and p value of the correlation with lapse/relapse and to generate graphs illustrating the relationship (Figs. 1–3). As a separate secondary analysis, each cluster found to have a significant correlation with lapse/relapse in the primary SPM analysis was also evaluated for the significance of its size using a voxel-based analysis within SPM.
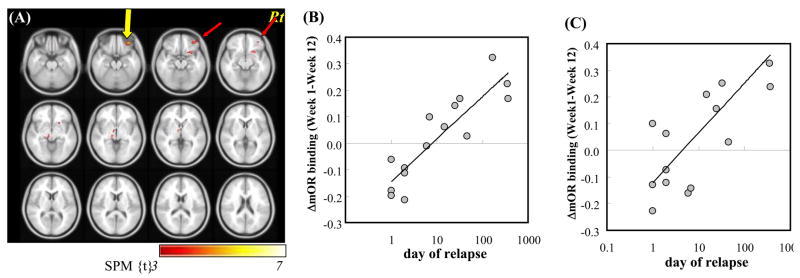
Fig. 1.
Correlation of decreases in regional brain mu-opioid receptor (mOR) binding between one week and 12 weeks of enforced abstinence with time to relapse to cocaine use in 15 cocaine-dependent subjects (see Table 1). (A) Brain regions (in red) showing a significant positive correlation between ΔmOR binding (week 1 – week 12) and time to relapse. Color bar presents the T-scores. The axial plane is cut from 40 mm below the bicommissural plane at 4-mm intervals. Panels B and C show relationship between ΔmOR binding (Y axis) and log (time to relapse) (X axis) in the right inferior frontal cortex (Brodman area 11, yellow arrow (B)) and in the right ventrolateral frontal cortex (Brodman area 47, red arrow (C)). Each data point represents an individual subject.
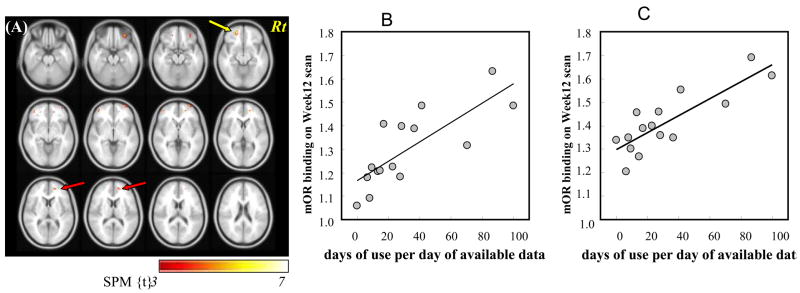
Fig. 3.
Correlation of regional brain mu-opioid receptor (mOR) binding after 12 weeks of enforced abstinence with percent days of cocaine use during the month following relapse in 15 cocaine-dependent subjects (see Table 3). (A) Brain regions (in red) showing a significant positive correlation. Color bar presents the T-scores. The axial plane is cut from 24 mm below the bicommissural plane at 4 mm intervals. Panels B and C show the relationship between mOR binding (Y axis) in the left inferior frontal cortex (yellow arrow in A) (B) and right anterior cingulate cortex (red arrow in A) (C) after 12 weeks of abstinence and percent days of cocaine use (X axis) during the month after relapse. Each data point represents an individual subject.
The relative value of mOR binding and subjects’ baseline clinical characteristics in predicting time to lapse and relapse was evaluated with the linear regression function of SPSS v. 11.5 (SPSS, Inc., Chicago, IL). First, univariate regression analyses were performed between subjects’ clinical characteristics (obtained from the ASI interview done at screening) and time to lapse and relapse. Clinical variables that were significant in the regression analyses were then included with regional brain mOR binding in a second round of stepwise multiple regression analyses to evaluate their relative predictive contribution (entry criterion was significance of F value < 0.001). These analyses used mean mOR binding in the most significant cluster in the voxel-based SPM analysis (Table 1), calculated with MarsBar software (Matthew Brett, http://marsbar.sourceforge.net).
Table 1.
Correlation of decreases in regional brain mu-opioid receptor binding between one day or one week and 12 weeks of enforced abstinence with time to relapse to cocaine use in 15 cocaine-dependent subjects
| Correlation with time to relapse
| |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change from day 1 to week 12 of abstinence
|
Change from week 1 to week 12 of abstinence
|
||||||||||||
| Brain region | Side of Brain | Voxel-based analysis in SPM | Cluster-based linear regression analysis in SPSS | Voxel-based analysis in SPM | Cluster-based linear regression analysis in SPSS | ||||||||
| MNIa | max-z | Kb (p-valuec) | r2 | F 1,13 | p-valued | MNIa | max-z | Kb (p-valuec) | r2 | F 1,13 | p-valued | ||
| Temporal | L | −56, −6,34 | 4.48 | 92 (0.049) | 0.77 | 44.06 | <0.0001 | ||||||
| Temporal | L | −32,14, −46 | 3.67 | 143 (0.018) | 0.57 | 17.2 | 0.001 | −48,18, −28 | 3.89 | 85 (0.043) | 0.64 | 23.56 | 0.0003 |
| Temporal | L | −30, −8, −26 | 3.07 | 93 (0.048) | 0.58 | 18.16 | 0.0009 | ||||||
| Temporal | R | 52, −2, −30 | 3.25 | 85 (0.043) | 0.59 | 18.58 | 0.0008 | ||||||
| Frontal | R | 36,42, −20 | 4.10 | 157 (0.009) | 0.79 | 49.73 | 0.0001 | ||||||
| Frontal, inferior | R | 24,14, −14 | 3.45 | 91 (0.037) | 0.59 | 18.71 | 0.0008 | ||||||
| Thalamus | L | −12, −8, −2 | 3.88 | 87 (0.041) | 0.77 | 42.78 | 0.0001 | ||||||
location of peak expressed as x,y,z coordinates in Montreal Neurological Institute (MNI) space
Cluster size k represents number of continguous voxels (2 × 2 × 2 mm3) at a height threshold of P = 0.005, uncorrected
p-value for significance at cluster-level in voxel-based analysis in SPM.
p-value for significance in cluster-based multiple regression analysis in SPSS
Results
Sample Description
Twenty subjects enrolled in the study: one withdrew before admission because of inability to tolerate the MRI scan, one could not be studied because of technical problems in radiolabeling carfentanil, and one was discharged from the ward after one day because of behavioral issues. The remaining 17 subjects had at least one PET scan; their findings have been presented previously (Gorelick, Kim et al. 2005). Of these 17 subjects, one withdrew from the study prior to ward discharge and so was lost to follow-up, and one had a technically inadequate second PET scan. The remaining 15 subjects (6 with cocaine dependence, 9 with abuse) included in the present relapse analysis were 10 African-American men, 3 African-American women, and 2 white men with mean (SD) age 33.8 (4.1) years. All subjects smoked cocaine; two also occasionally used intranasally. They had used cocaine regularly for 7.6 (4.5) years. Twelve subjects tended to use cocaine daily (subject to availability); three used cocaine intermittently (i.e., several days a week, with abstinence the other days). They smoked cocaine on 10.9 (2.7) of the 14 days prior to ward admission (3 subjects reported less than 10 days of use). They reported spending $499 ($432) on cocaine during those two weeks. Their last cocaine use was 14.9 (10.1) hours prior to admission. Use of other illegal drugs was negligible. No subject reported opiate use during the month prior to admission; all urine drug tests were negative for opiates.
As expected from the study eligibility criteria, no subject was clinically depressed at the time of admission. SCL-90R depression and anxiety subscale scores remained low throughout the study, e.g., mean (SD) of 0.8 (0.15) and 0.04 (0.10), respectively, before the first PET scan and 0.03 (0.08) and 0.006 (0.02) before the second PET scan. There were no significant correlations between subscale scores and mOR binding (Gorelick et al. 2005).
Cocaine Use During Follow-Up
Subjects were followed after ward discharge for a mean (SD) of 28.2 (22.2) weeks (median = 28 weeks, range 1 to 52 weeks). The first cocaine use (lapse) occurred 6.1 (9.0) days (range = 0–32 days, median = 1 day) after discharge; the first relapse 67.8 (126.2) days (range = 0–363 days, median = 6 days) after discharge. The mean interval between lapse and relapse was 61.7 (125.1) days (range = 0–357 days, median = 0 days). Subjects reported using cocaine on 50.9% (38.0%) of the first 30 days after lapse, and on 55.9% (34.2%) of the first 30 days after relapse.
Brain Mu-Opioid Receptor Binding & Relapse
The decrease in mOR binding in the right inferior frontal cortex (including adjacent ventral striatum) between one week and 12 weeks of abstinence showed a significant positive correlation with time to relapse to cocaine use after discharge (Table 1; Fig. 1), i.e., the greater the decrease in binding during abstinence, the longer the time before relapse. The right and left temporal cortex and left thalamus also had decreases in mOR binding between one and 12 weeks of abstinence that correlated significantly with time to relapse (Table 1; Fig. 1). There was a similar pattern of correlations between mOR binding and time to lapse (data not shown).
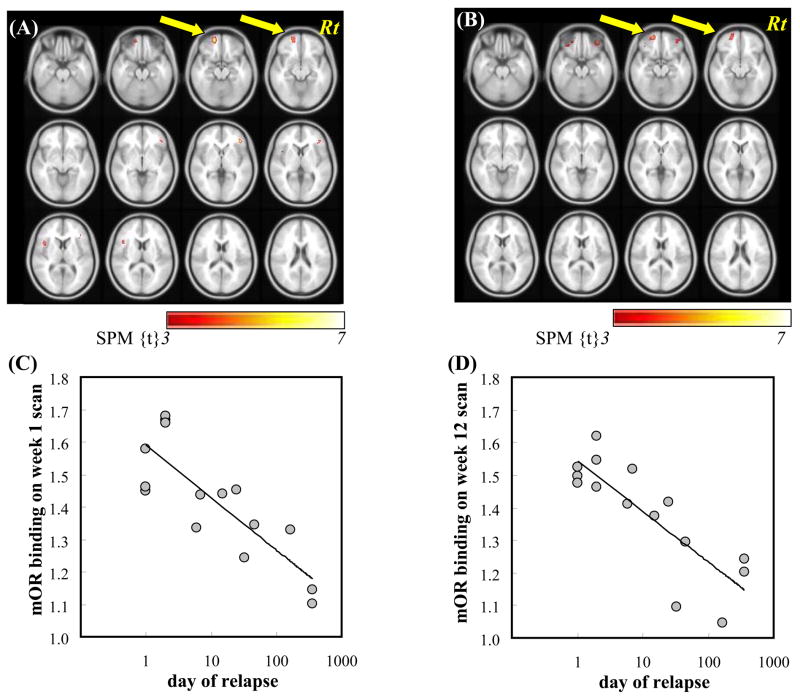
There were significant negative correlations between mOR binding in bilateral frontal cortex after one week or 12 weeks of abstinence and time to relapse to cocaine use (Table 2; Fig. 2), i.e., the higher the binding, the shorter the time before relapse.
Table 2.
Correlation of regional brain mu-opioid receptor (mOR) binding after one week or 12 weeks of enforced abstinence with time to relapse to cocaine use in 15 cocaine-dependent subjects.
| One week of abstinence
|
12 Weeks of abstinence
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Voxel-based Analysis in SPM | Cluster-based linear regression analysis in SPSS | Voxel-based Analysis in SPM | Cluster-based linear regression analysis in SPSS | |||||||||
| Brain region | MNI x,y,z coordinatea | max-z | cluster kb (p-value)c | r2 | F 1,13 | p-valued | MNI x,y,z coordinatea | max- z | cluster kb (p-value) c | r2 | F 1,13 | p-valued |
| Frontal | (−20,56, −16) | 4.41 | 168 (0.024) | 0.69 | 28.54 | 0.0001 | (−22,54, −14) | 3.58 | 180 (0.018) | 0.69 | 29.19 | 0.0001 |
| Frontal | (−44,14,8) | 3.42 | 65 (0.138) | 0.62 | 21.27 | 0.0004 | ||||||
| Frontal | (42,36, −2) | 4.26 | 74 (0.115) | 0.70 | 30.92 | <0.0001 | (34,44, −20) | 3.55 | 87 (0.085) | 0.57 | 17.09 | 0.001 |
| Temporal | (−46,18, −34) | 3.55 | 171 (0.021) | 0.66 | 25.44 | 0.0002 | ||||||
location of peak expressed as x,y,z coordinates in Montreal Neurological Institute (MNI) space.
cluster size k represents number of voxels (2 × 2 × 2 mm3) at a height threshold of p = 0.005, uncorrected.
p-value for significance of cluster size in voxel-based analysis in SPM.
p-value for significance of relationship between mOR binding and time to relapse in linear regression analysis outside SPM.
Fig. 2.
Correlation of regional brain mu-opioid receptor (mOR) binding after one week or 12 weeks of enforced abstinence with time to relapse to cocaine use in 15 cocaine-dependent subjects (see Table 2). Brain regions (in red) showing a significant negative correlation after one week 1 (A) or 12 weeks (B) of abstinence. Color bar presents the T-scores. The axial plane is cut from 24 mm below the bicommissural plane at 4 mm intervals. Panels C and D show the relationship between mOR binding (Y axis) in the left orbitofrontal cortex (yellow arrow in A and B) after one week (C) or 12 weeks (D) of abstinence and log (time to relapse) (X axis). Each data point represents an individual subject.
There was also a significant correlation between regional brain mOR binding after 12 weeks of enforced cocaine abstinence and severity of relapse. There was a significant positive correlation between mOR binding in the right anterior cingulate cortex and bilateral inferior frontal cortex and percent days of cocaine use during the 30 days following relapse (Table 3; Fig. 3), i.e., the higher the mOR binding, the greater the percentage of days on which cocaine was reported used.
Table 3.
Correlation of regional brain mu-opioid receptor (mOR) binding after 12 weeks of enforced abstinence with proportion of days with cocaine use during 30 days after relapse in 15 cocaine-dependent subjects
| Voxel-Based Analysis in SPM | Cluster-based multiple regression analysis in SPSS | ||||||
|---|---|---|---|---|---|---|---|
| Side of brain | Brain region | max-z | MNI coordinatea | Cluster kb (p-valuec) | r2 | F 1,13 | p-valued |
| R | Anterior cingulate | 3.44 | (18,50,2) | 85 (0.081) | 0.70 | 30.16 | 0.0001 |
| R | Frontal | 3.22 | (28,42, −22) | 67 (0.117) | 0.52 | 13.85 | 0.002 |
| R | Frontal | 3.57 | (26, 68, −2) | 63 (0.127) | 0.58 | 18.17 | 0.0009 |
| L | Frontal | 3.48 | (−20,52, −12) | 82 (0.086) | 0.61 | 20.08 | 0.0006 |
| L | Frontal | 3.63 | (−44,54,0) | 51 (0.167) | 0.62 | 21.30 | 0.0004 |
location of peak expressed as x,y,z coordinates in Montreal Neurological Institute (MNI) space.
Cluster size k represents number of voxels (2 × 2 × 2 mm3) at a height threshold of p = 0.005, uncorrected.
p-value for significance of cluster size in voxel-based analysis in SPM.
p-value for significance of relationship between mOR binding and proportion of days with cocaine use in multiple-regression analysis outside SPM.
To complement these correlational analyses, we compared regional mOR binding between the 8 subjects who relapsed within 10 days of ward discharge (early relapsers) and the 7 subjects who relapsed later (late relapsers). The early relapsers had significantly smaller decreases in mOR binding between week 1 and week 2 in the right ventral striatum (max-z = 3.99 at coordinates 20,16,−12, cluster size k = 110), right orbitofrontal cortex (max-z = 3.92 at 36,42, −20, k = 111), right frontal cortex (max-z = 3.61 at 56,14,4, k = 60), and left anterior temporal cortex (max-z = 3.38 at −48,18, −28, k = 55). The early relapsers also had greater mOR binding at week 1 in the left temporal cortex (max-z = 3.92 at −50, −24, −34, k = 93), left orbitofrontal cortex (max-z = 3.92 at −18,56, −16, k = 62), right ventral striatum (max-z = 3.32 at 18, −4, −10, k = 69), and right temporal cortex (max-z = 3.15 at −48,18, −28, k = 56). These findings of greater initial (week 1) mOR binding and less decrease in mOR binding between week 1 and week 12 in the early relapsers are consistent with the correlational analyses. The latter also showed greater initial mOR binding and lesser week 1 to week 12 decrease in mOR binding associated with shorter time to relapse.
Three subject baseline characteristics from the ASI correlated significantly with time to lapse in univariate analyses; only one ASI variable correlated significantly with time to relapse (Table 4). Other clinical variables previously reported to be significantly associated with relapse in treatment samples, e.g., days or years of cocaine use or employment status (McKay, et al. 1999), did not show significant correlations with lapse or relapse in this non-treatment-seeking sample. Stepwise multiple regression analysis including the one clinical variable (years of lifetime alcohol use) with a significant univariate correlation found that a mOR binding variable (decrease in binding in the right inferior frontal cortex between one and 12 weeks of abstinence) was a more significant predictor of time to relapse than was years of lifetime alcohol use (Table 4). These two variables combined accounted for 86% of the variance in time to relapse. This mOR binding variable was second only to legal problems composite score in predicting time to lapse in a stepwise analysis including the three clinical variables (drug, legal, and family/social problems ASI composite scores) with significant univariate correlations (Table 4). These two variables combined accounted for 91% of the variance in time to lapse.
Table 4.
Significant univariate clinical predictors, and comparison with PET regional brain mu-opioid receptor (mOR) binding predictor, of time to lapse and to relapse to cocaine use in 15 cocaine-dependent subjects
| Predictor Variable | Time to Lapse* | Time to Relapse* | ||||
|---|---|---|---|---|---|---|
| Beta [SE] | R2 | P | Beta [SE] | R2 | P | |
| Univariate Predictors | ||||||
| ASI Drug Composite Score | 134.9 [23.0] | 0.71 | <0.0001 | |||
| ASI Legal Composite Score | 73.3 [10.7] | 0.78 | <0.0001 | |||
| ASI Family/Social Composite Score | 138.6 [29.4] | 0.63 | <0.0001 | |||
| Lifetime Alcohol Use (yrs) | 0.18 [0.06] | 0.44 | 0.007 | |||
| Multivariate Predictors# | ||||||
| ASI Legal Composite Score | 56.2 [8.4] | 0.78 | 0.0001 | |||
| mOR binding variable@ | 31.9 [7.9] | 0.13 | 0.002 | |||
| Lifetime Alcohol Use (yrs) | 0.82 [0.34] | 0.07 | 0.03 | |||
| mOR binding variable@ | 9.61 [1.61] | 0.79 | < 0.001 | |||
analyzed as log (days) because of skewed distributions
based on stepwise multiple regression analysis with entry criterion of F value significance < 0.001
decrease in mOR binding in right inferior frontal cortex between one and 12 weeks of abstinence
PET = positron emission tomography, ASI = Addiction Severity Index
The four subject baseline characteristics from the ASI that showed significant univariate correlations with time to lapse or relapse did not show a consistent pattern of univariate correlations with regional brain mOR binding at week 1 and week 12 (data not shown). For example, at week one, lifetime alcohol use (years) had a significant positive correlation with mOR binding in the right inferior frontal cortex and a significant negative correlation with mOR binding in the right inferior and superior frontal cortex and left superior temporal cortex. At week 12, there were no significant positive correlations and significant negative correlations only in the left precentral frontal cortex and right inferior frontal cortex.
Discussion
We found that increased mOR binding in frontal and temporal cortex, and changes in binding over 12 weeks of enforced abstinence, are associated with time to relapse (and the related variable time to lapse) after release from enforced abstinence on a closed research ward. Regional mOR binding contributed significant predictive power beyond that provided by standard clinical variables such as drug and alcohol use and employment status.
These findings suggest that brain mOR binding could serve as a predictive marker for patient response to cocaine addiction treatment. Confirmation of this finding offers the potential to use mOR binding as a tool to identify patients at greater risk of relapse and to better allocate limited drug addiction treatment resources to patients most in need. The observation of a significant correlation between time to relapse and mOR binding 11 weeks before discharge suggests that mOR binding may have predictive value prior to or early in treatment. All significant R2 values (square of correlation coefficient) were within the range of 0.57–0.79 (Tables 1 and 2). Our sample size was too small to provide sufficient statistical power to evaluate whether any of these were significantly higher (i.e., more predictive) than the others.
Subjects’ mood is unlikely to have confounded the observed relationship between brain mOR binding and relapse. Subjects had no current DSM-IV mood disorder and low self-rated depression or anxiety (SCL-90R subscales) throughout the study. Furthermore, there were no significant correlations between depression or anxiety scores and mOR binding (Gorelick, et al. 2005).
We are aware of only two other studies, both involving subjects with alcoholism, in which a human brain imaging parameter was significantly correlated with relapse to substance use (Grusser, et al. 2004; Guardia, et al. 2000). In one study, detoxified alcoholic patients who relapsed during 3 months of outpatient treatment had significantly greater dopamine D2 receptor availability in the striatum (assessed by single photon emission computed tomography (SPECT) with radiolabeled iodobenzamide) during their initial inpatient detoxification than did patients who did not relapse (based on self-reported drinking status) (Guardia, et al. 2000). In the other study, the intensity of activation in the anterior cingulate, medial prefrontal cortex, and striatum (measured by fMRI) in response to alcohol-related cues was significantly correlated with amount of alcohol intake over the subsequent 3 months in 10 alcoholic patients scanned while abstinent (Grusser, et al. 2004).
The mechanism mediating the relationship between brain mOR binding and relapse cannot be directly determined from this study. Based on animal studies and our previous human studies (Zubieta, et al. 1996; Gorelick, et al. 2005), we suggest that increased mOR activation (due to increased binding potential) mediates increased cocaine craving, which increases the risk of relapse in many (Palij, et al. 1996; Rohsenow, et al. 2007; Weiss, et al. 2003), but not all (Kosten, et al. 2006), studies of cocaine addiction treatment. The mechanism by which mORs are upregulated is incompletely understood, but may be related to tonically reduced release of endogenous opioid receptor ligands associated with long-term cocaine exposure (Daunais, et al. 1997; Laforge, et al. 2003; Przewlocka and Lason 1995). In this study, two of the brain regions showing significant correlations between increased mOR binding and time to or severity of relapse were the inferior frontal cortex and anterior cingulate cortex. Activation of these brain regions has been associated with cocaine craving, salience of reinforcers, and risk of relapse in animal models of relapse to drug self-administration (Daglish and Nutt 2003; Goldstein and Volkow 2002; Kalivas and McFarland 2003). Thus, increased activation of mORs in these brain regions may have mediated the increased tendency to relapse to cocaine use among our subjects (Gianoulakis 2004). The inferior frontal cortex is an important region in brain circuits involved with memory for reinforcement and risk-reward decision-making (Robbins and Everitt 2002; Volkow, et al. 2002), i.e., the ability to make decisions that appropriately balance the probability and magnitude of positive and negative consequences. The anterior cingulate cortex also has a role in risk-reward decision-making (Bush, et al. 2002; Williams, et al. 2004).
This study has some limitations. Subjects were not representative of all cocaine-dependent individuals because we excluded those with other current substance use disorders (except tobacco dependence) and with more than minimal recent opiate use. This was done to minimize possible effects on brain mOR binding from other substance use and give greater ability to detect a relationship between mOR binding and relapse. However, there is no reason to believe that the underlying relationship observed in our somewhat selected sample would not also hold for subjects with current substance use other than cocaine.
Subjects were not treatment-seeking and did not receive drug abuse treatment during their 3-month residential stay or one-year follow-up. Previous studies showing an association between sociodemographic and drug use variables and relapse to cocaine use have been conducted in treatment settings with treatment-seeking patients (Ciraulo, et al. 2003; Kampman, et al. 2002; McKay, et al. 1999; McMahon 2001; Poling, et al. 2007; Reiber, et al. 2002). In our sample of non-treatment-seeking subjects, few of these clinical variables showed a significant correlation with time to lapse or relapse. This lack of correlation may be due, in part, to our relatively small sample size (15 subjects), but also could reflect a difference in valid predictors of relapse between treatment and non-treatment samples. Thus, the generalizability of our findings to treatment-seeking cocaine users in a treatment setting remains to be confirmed.
Cocaine use during follow-up was measured by subject self-report, with periodic confirmation by urine drug testing. The study procedures should have maximized valid self-report (Brown, et al. 1992; Hamid, et al. 1999; Harrison 1995; Nelson, et al. 1998). There was 80% overall agreement between self-report and the urine drug tests, comparable to the agreement reported in large published studies (Brown, et al. 1992; Harrison 1995; Hersh, et al. 1999; Nelson, et al. 1998; Simpson, et al. 2002). In any case, distortions of self-report would have decreased the ability to detect a significant correlation with mOR binding (unless one assumes a significant association between mOR binding and tendency to under-report drug use).
The PET scanning procedure used does not distinguish between increased numbers of mOR and increased receptor affinity. This limits the ability to deduce the mechanism of the observed effect. Animal studies suggest that cocaine exposure in a binge pattern increases mOR number rather than affinity (Unterwald, et al. 1992).
In summary, our findings show that increased regional brain mOR binding is associated with shorter time to relapse and more severe relapse to cocaine use after monitored abstinence. These findings improve our understanding of the neuropharmacological mechanisms involved in cocaine addiction and could lead to improved treatment and prediction of treatment outcome.
Acknowledgments
Supported by the Intramural Research Program, National Institutes of Health, National Institute on Drug Abuse and NIH grant RO1 DA-09479 to JJF.
This work was supported by the Intramural Research program of the National Institutes of Health, National Institute on Drug Abuse and NIH grant RO1 DA-09479 to JJF.
Footnotes
Financial Disclosures
The authors have no competing financial interests to declare.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, D.C.: 1994. [Google Scholar]
- Azaryan AV, Clock BJ, Cox BM. Mu opioid receptor mRNA in nucleus accumbens is elevated following dopamine receptor activation. Neurochem Res. 1996;21:1411–1415. doi: 10.1007/BF02532382. [DOI] [PubMed] [Google Scholar]
- Azaryan AV, Coughlin LJ, Buzas B, Clock BJ, Cox BM. Effect of chronic cocaine treatment on mu- and delta-opioid receptor mRNA levels in dopaminergically innervated brain regions. J Neurochem. 1996;66:443–448. doi: 10.1046/j.1471-4159.1996.66020443.x. [DOI] [PubMed] [Google Scholar]
- Bauer LO. Frontal P300 decrements, childhood conduct disorder, family history, and the prediction of relapse among abstinent cocaine abusers. Drug Alcohol Depend. 1997;44:1–10. doi: 10.1016/s0376-8716(96)01311-7. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sonne SC, Malcolm RJ, Randall CL, Dansky BS, Simpson K, Roberts JS, Brondino M. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276–285. doi: 10.1037//1064-1297.10.3.276. [DOI] [PubMed] [Google Scholar]
- Branch AD, Unterwald EM, Lee SE, Kreek MJ. Quantitation of preproenkephalin mRNA levels in brain regions from male Fischer rats following chronic cocaine treatment using a recently developed solution hybridization assay. Brain Res Mol Brain Res. 1992;14:231–238. doi: 10.1016/0169-328x(92)90178-e. [DOI] [PubMed] [Google Scholar]
- Brown J, Kranzler HR, Del Boca FK. Self-reports by alcohol and drug abuse inpatients: factors affecting reliability and validity. Br J Addict. 1992;87:1013–1024. doi: 10.1111/j.1360-0443.1992.tb03118.x. [DOI] [PubMed] [Google Scholar]
- Bush G, Vogt BA, Holmes J, Dale AM, Greve D, Jenike MA, Rosen BR. Dorsal anterior cingulate cortex: a role in reward-based decision making. Proc Natl Acad Sci USA. 2002;99:523–528. doi: 10.1073/pnas.012470999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciraulo DA, Piechniczek-Buczek J, Iscan EN. Outcome predictors in substance use disorders. Psychiatr Clin North Am. 2003;26:381–409. doi: 10.1016/s0193-953x(02)00106-5. [DOI] [PubMed] [Google Scholar]
- Cone EJ, Sampson-Cone AH, Darwin WD, Huestis MA, Oyler JM. Urine testing for cocaine abuse: metabolic and excretion patterns following different routes of administration and methods for detection of false-negative results. J Anal Toxicol. 2003;27:386–401. doi: 10.1093/jat/27.7.386. [DOI] [PubMed] [Google Scholar]
- Daglish MR, Nutt DJ. Brain imaging studies in human addicts. Eur Neuropsychopharmacol. 2003;13:453–458. doi: 10.1016/j.euroneuro.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Daunais JB, Nader MA, Porrino LJ. Long-term cocaine self-administration decreases striatal preproenkephalin mRNA in rhesus monkeys. Pharmacol Biochem Behav. 1997;57:471–475. doi: 10.1016/s0091-3057(96)00432-7. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90R Administration, Scoring and Procedures. Manual II. Clinical Psychometric Research; Towson, MD: 1983. [Google Scholar]
- Donovan DM. Assessment issues and domains in the prediction of relapse. Addiction. 1996;91(Suppl):S29–S36. [PubMed] [Google Scholar]
- Elkashef A, Vocci F. Biological markers of cocaine addiction: implications for medications development. Addict Biol. 2003;8:123–139. doi: 10.1080/1355621031000117356. [DOI] [PubMed] [Google Scholar]
- Endres CJ, Bencherif B, Hilton J, Madar I, Frost JJ. Quantification of brain mu-opioid receptors with [11C]carfentanil: reference-tissue methods. Nucl Med Biol. 2003;30:177–186. doi: 10.1016/s0969-8051(02)00411-0. [DOI] [PubMed] [Google Scholar]
- Frost JJ, Wagner HN, Jr, Dannals RF, Ravert HT, Links JM, Wilson AA, Burns HD, Wong DF, McPherson RW, Rosenbaum AE. Imaging opiate receptors in the human brain by positron tomography. J Comput Assist Tomogr. 1985;9:231–236. doi: 10.1097/00004728-198503000-00001. [DOI] [PubMed] [Google Scholar]
- Gianoulakis C. Endogenous opioids and addiction to alcohol and other drugs of abuse. Curr Top Med Chem. 2004;4:39–50. doi: 10.2174/1568026043451573. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. American Journal of Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelick DA. Pharmacologic interventions for cocaine, crack, and other stimulant addiction. In: Graham AW, Schultz TK, Mayo-Smith MF, Ries RK, Wilford BB, editors. Principles of Addiction Medicine. American Society of Addiction Medicine; Chevy Chase, MD: 2003. pp. 785–800. [Google Scholar]
- Gorelick DA, Kim YK, Bencherif B, Boyd SJ, Nelson R, Copersino M, Endres CJ, Dannals RF, Frost JJ. Imaging brain mu-opioid receptors in abstinent cocaine users: time course and relation to cocaine craving. Biol Psychiatry. 2005;57:1573–1582. doi: 10.1016/j.biopsych.2005.02.026. [DOI] [PubMed] [Google Scholar]
- Grusser SM, Wrase J, Klein S, Hermann D, Smolka MN, Ruf M, Weber-Fahr W, Flor H, Mann K, Braus DF, Heinz A. Cue-induced activation of the striatum and medial prefrontal cortex is associated with subsequent relapse in abstinent alcoholics. Psychopharmacology (Berl) 2004;175:296–302. doi: 10.1007/s00213-004-1828-4. [DOI] [PubMed] [Google Scholar]
- Guardia J, Catafau AM, Batlle F, Martin JC, Segura L, Gonzalvo B, Prat G, Carrio I, Casas M. Striatal dopaminergic D(2) receptor density measured by [(123)I]iodobenzamide SPECT in the prediction of treatment outcome of alcohol-dependent patients. American Journal of Psychiatry. 2000;157:127–129. doi: 10.1176/ajp.157.1.127. [DOI] [PubMed] [Google Scholar]
- Hamid R, Deren S, Beardsley M, Tortu S. Agreement between urinalysis and self-reported drug use. Subst Use Misuse. 1999;34:1585–1592. doi: 10.3109/10826089909039416. [DOI] [PubMed] [Google Scholar]
- Hammer RP. Cocaine alters opiate receptor binding in critical brain reward regions. Synapse. 1989;3:55–60. doi: 10.1002/syn.890030108. [DOI] [PubMed] [Google Scholar]
- Harrison LD. The validity of self-reported data on drug use. Journal of Drug Issues. 1995;25(1):91–111. [Google Scholar]
- Hersh D, Mulgrew CL, Van Kirk J, Kranzler HR. The validity of self-reported cocaine use in two groups of cocaine abusers. J Consult Clin Psychol. 1999;67:37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- Hser YI, Maglione M, Boyle K. Validity of self-report of drug use among STD patients, ER patients, and arrestees. Am J Drug Alcohol Abuse. 1999;25:81–91. doi: 10.1081/ada-100101847. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, McFarland K. Brain circuitry and the reinstatement of cocaine-seeking behavior. Psychopharmacology (Berl) 2003;168:44–56. doi: 10.1007/s00213-003-1393-2. [DOI] [PubMed] [Google Scholar]
- Kampman KM, Volpicelli JR, Mulvaney F, Rukstalis M, Alterman AI, Pettinati H, Weinrieb RM, O’Brien CP. Cocaine withdrawal severity and urine toxicology results from treatment entry predict outcome in medication trials for cocaine dependence. Addict Behav. 2002;27:251–260. doi: 10.1016/s0306-4603(01)00171-x. [DOI] [PubMed] [Google Scholar]
- Karila L, Gorelick D, Weinstein A, Noble F, Benyamina A, Coscas S, Blecha L, Lowenstein W, Martinot JL, Reynaud M, Lepine JP. New treatments for cocaine dependence: a focused review. Int J Neuropsychopharmacol. 2007:1–14. doi: 10.1017/S1461145707008097. [DOI] [PubMed] [Google Scholar]
- Knapp WP, Soares BG, Farrel M, Lima MS. Psychosocial interventions for cocaine and psychostimulant amphetamines related disorders. Cochrane Database Syst Rev. 2007:CD003023. doi: 10.1002/14651858.CD003023.pub2. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Scanley BE, Tucker KA, Oliveto A, Prince C, Sinha R, Potenza MN, Skudlarski P, Wexler BE. Cue-induced brain activity changes and relapse in cocaine-dependent patients. Neuropsychopharmacology. 2006;31:644–650. doi: 10.1038/sj.npp.1300851. [DOI] [PubMed] [Google Scholar]
- Laforge KS, Yuferov V, Zhou Y, Ho A, Nyberg F, Jeanne KM. “Binge” cocaine differentially alters preproenkephalin mRNA levels in guinea pig brain. Brain Res Bull. 2003;59:353–357. doi: 10.1016/s0361-9230(02)00927-9. [DOI] [PubMed] [Google Scholar]
- Logan J, Fowler JS, Volkow ND, Wang GJ, Ding YS, Alexoff DL. Distribution volume ratios without blood sampling from graphical analysis of PET data. J Cereb Blood Flow Metab. 1996;16:834–840. doi: 10.1097/00004647-199609000-00008. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ. Relapse in the addictive behaviors: integration and future directions. Clin Psychol Rev. 2006;26:229–231. doi: 10.1016/j.cpr.2005.11.009. [DOI] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Mulvaney FD, Koppenhaver JM. Predicting proximal factors in cocaine relapse and near miss episodes: clinical and theoretical implications. Drug Alcohol Depend. 1999;56:67–78. doi: 10.1016/s0376-8716(99)00013-7. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, O’Brien CP. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McMahon RC. Personality, stress, and social support in cocaine relapse prediction. J Subst Abuse Treat. 2001;21:77–87. doi: 10.1016/s0740-5472(01)00187-8. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Vuchinich RE, Wallace D, Plant MA, Freedman MJ, McNamara C, Ward CL. Transitions during effective treatment for cocaine-abusing homeless persons: establishing abstinence, lapse, and relapse, and reestablishing abstinence. Psychol Addict Behav. 2004;18:250–256. doi: 10.1037/0893-164X.18.3.250. [DOI] [PubMed] [Google Scholar]
- Nelson DB, Kotranski L, Semaan S, Collier K, Lauby J, Feighan K, Halbert J. The validity of self-reported opiate and cocaine use by out-of-treatment drug users. Journal of Drug Issues. 1998;28(2):483–494. [Google Scholar]
- Palij M, Rosenblum A, Magura S, Handelsman L, Stimmel B. Daily cocaine use patterns: effects of contextual and psychological variables. J Addict Dis. 1996;15:13–37. doi: 10.1300/J069v15n04_02. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Gottheil E, Berrettini WH, Thornton CC, Hill KP, Weinstein SP. Relationship between platelet serotonin uptake sites and treatment outcome among African-American cocaine dependent individuals. J Addict Dis. 2003;22:79–92. doi: 10.1300/J069v22n01_06. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Mannelli P, Certa KM, Peindl K, Murray H, Vergare MJ, Berrettini WH. Relationship of serum prolactin with severity of drug use and treatment outcome in cocaine dependence. Psychopharmacology (Berl) 2004;176:74–81. doi: 10.1007/s00213-004-1856-0. [DOI] [PubMed] [Google Scholar]
- Poling J, Kosten TR, Sofuoglu M. Treatment outcome predictors for cocaine dependence. Am J Drug Alcohol Abuse. 2007;33:191–206. doi: 10.1080/00952990701199416. [DOI] [PubMed] [Google Scholar]
- Preston KL, Epstein DH, Cone EJ, Wtsadik AT, Huestis MA, Moolchan ET. Urinary elimination of cocaine metabolites in chronic cocaine users during cessation. J Anal Toxicol. 2002;26:393–400. doi: 10.1093/jat/26.7.393. [DOI] [PubMed] [Google Scholar]
- Prichep LS, Alper KR, Kowalik SC, Vaysblat LS, Merkin HA, Tom M, John ER, Rosenthal MS. Prediction of treatment outcome in cocaine dependent males using quantitative EEG. Drug Alcohol Depend. 1999;54:35–43. doi: 10.1016/s0376-8716(98)00147-1. [DOI] [PubMed] [Google Scholar]
- Przewlocka B, Lason W. Adaptive changes in the proenkephalin and D2 dopamine receptor mRNA expression after chronic cocaine in the nucleus accumbens and striatum of the rat. Eur Neuropsychopharmacol. 1995;5:465–469. doi: 10.1016/0924-977x(95)80005-m. [DOI] [PubMed] [Google Scholar]
- Reiber C, Ramirez A, Parent D, Rawson RA. Predicting treatment success at multiple timepoints in diverse patient populations of cocaine-dependent individuals. Drug Alcohol Depend. 2002;68:35–48. doi: 10.1016/s0376-8716(02)00103-5. [DOI] [PubMed] [Google Scholar]
- Robbins TW, Everitt BJ. Limbic-striatal memory systems and drug addiction. Neurobiol Learn Mem. 2002;78:625–636. doi: 10.1006/nlme.2002.4103. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Ratcliff KS, Seyfried W. Validity of the diagnostic interview schedule, version II: DSM-III diagnoses. Psychol Med. 1982;12:855–870. doi: 10.1017/s0033291700049151. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Eaton CA, Monti PM. Cocaine craving as a predictor of treatment attrition and outcomes after residential treatment for cocaine dependence. J Stud Alcohol Drugs. 2007;68:641–648. doi: 10.15288/jsad.2007.68.641. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Arch Gen Psychiatry. 2002;59:538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring Alcohol Consumption: Psychosocial and Biological Methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Unterwald EM, Horne-King J, Kreek MJ. Chronic cocaine alters brain mu opioid receptors. Brain Research. 1992;584:314–318. doi: 10.1016/0006-8993(92)90912-s. [DOI] [PubMed] [Google Scholar]
- Unterwald EM, Kreek MJ, Cuntapay M. The frequency of cocaine administration impacts cocaine-induced receptor alterations. Brain Res. 2001;900:103–109. doi: 10.1016/s0006-8993(01)02269-7. [DOI] [PubMed] [Google Scholar]
- Unterwald EM, Rubenfeld JM, Kreek MJ. Repeated cocaine administration upregulates kappa and mu, but not delta, opioid receptors. Neuroreport. 1994;5:1613–1616. doi: 10.1097/00001756-199408150-00018. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Goldstein RZ. Role of dopamine, the frontal cortex and memory circuits in drug addiction: insight from imaging studies. Neurobiol Learn Mem. 2002;78:610–624. doi: 10.1006/nlme.2002.4099. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Mazurick C, Berkman B, Gastfriend DR, Frank A, Barber JP, Blaine J, Salloum I, Moras K. The relationship between cocaine craving, psychosocial treatment, and subsequent cocaine use. Am J Psychiatry. 2003;160:1320–1325. doi: 10.1176/appi.ajp.160.7.1320. [DOI] [PubMed] [Google Scholar]
- Williams ZM, Bush G, Rauch SL, Cosgrove GR, Eskandar EN. Human anterior cingulate neurons and the integration of monetary reward with motor responses. Nat Neurosci. 2004;7:1370–1375. doi: 10.1038/nn1354. [DOI] [PubMed] [Google Scholar]
- Yuferov V, Zhou Y, Spangler R, Maggos CE, Ho A, Kreek MJ. Acute “binge” cocaine increases mu-opioid receptor mRNA levels in areas of the rat mesolimbic mesocortical dopamine system. Brain Res Bull. 1999;48:109–112. doi: 10.1016/s0361-9230(98)00155-5. [DOI] [PubMed] [Google Scholar]
- Zubieta J-K, Gorelick DA, Stauffer R, Ravert HT, Dannals RF, Frost JJ. Increased mu opioid receptor binding detected by PET in cocaine-dependent men is associated with cocaine craving. Nature Medicine. 1996;2:1225–1229. doi: 10.1038/nm1196-1225. [DOI] [PubMed] [Google Scholar]