Abstract
Background:
Alcohol dependence (AD) is often comorbid with other disinhibitory disorders that are characterized by poor decision making and evidenced by disadvantageous strategies on laboratory tasks such as the Iowa Gambling Task (IGT). In this study, a variant of the IGT is used to examine specific mechanisms that may account for poor decision making on the task in AD both with and without comorbid psychopathology.
Methods:
The community sample (n = 428) included 134 young adult subjects with AD and a history of childhood conduct disorder (CCD), 129 with AD and no history of CCD, 60 with a history of CCD and no AD, and 105 controls. Lifetime histories of other disinhibitory problems (adult antisocial behavior, marijuana, and other drugs) and major depression also were assessed. A modified version of the IGT was used to estimate (i) insensitivity to future consequences (IFC), and (ii) preference for large versus small immediate reward decks (PLvS).
Results:
Both AD and CCD were associated with greater IFC but not greater PLvS. Structural equation models (SEMs) indicated that IFC was associated with higher scores on a latent dimensional “disinhibitory disorders” factor representing the covariance among all lifetime measures of disinhibitory psychopathology, but was not directly related to any one disinhibitory disorder. SEMs also suggested that adult antisocial behavior was uniquely associated with a greater PLvS.
Conclusions:
Disadvantageous decision making on the IGT in those with AD and related dis-inhibitory disorders may reflect an IFC that is common to the covariance among these disorders but not unique to any one disorder.
Keywords: Alcoholism, Decision Making, Conduct Disorder, Disinhibitory Psychopathology
ALCOHOL DEPENDENCE (AD) is a heterogeneous disorder that is frequently comorbid with other types of disinhibitory psychopathology including childhood conduct disorder, adult antisocial personality, marijuana, and other drug abuse/dependence (Finn et al., 1997; Hesselbrock et al., 1986; Krueger et al., 2002; Zucker et al., 1996). These disinhibitory disorders seem to share a disadvantageous approach to decision making that favors larger immediate rewards even when there are long-term negative consequences (Bechara et al., 1994, 2001; Grant et al., 2000; Mazas et al., 2000). Although insensitivity to future negative consequences is characteristic of individuals with antisocial problems (Finn et al., 2002; Lykken, 1957; Newman, 1987; Schmauk, 1970) and alcohol abuse (Finn et al., 1994, 2002), the association between decision-making mechanisms and the broader spectrum of disinhibitory disorders is not well understood.
Various laboratory tasks have been developed and used to investigate the mechanisms underlying this kind of decision making. For example, disadvantageous decision making on the Iowa Gambling Task (IGT; Bechara et al., 1994, 1997, 2001) is thought to reflect a general predisposition to disinhibitory psychopathology (Bechara et al., 1994). Using the IGT, disadvantageous decision making has been observed in individuals with AD (Dom et al., 2006; Fein et al., 2004; Mazas et al., 2000), high levels of binge drinking (Goudriaan et al., 2007), other substance abuse (Bechara and Damasio, 2002; Bechara and Martin, 2004; Bechara et al., 2001; Grant et al., 2000; Petry et al., 1998; Rotheram-Fuller et al., 2004; Stout et al., 2005), psychopathy or antisocial personality (Mazas et al., 2000; Mitchell et al., 2002; Van Honk et al., 2002), borderline personality (Dom et al., 2006), a history of childhood conduct disorder (Kim et al., 2006), and attention deficit/hyperactivity disorder (Ernst et al., 2003). A limitation of many of these findings is that the effects of comorbidity among AD and other disinhibitory disorders (Krueger et al., 2002; Zucker et al., 1996) on decision making cannot be evaluated directly. By contrast, in those studies where it has been considered, AD comorbid with antisocial or borderline personality is associated with a greater disadvantageous decision bias than AD alone (Dom et al., 2006; Mazas et al., 2000).
There is increasing evidence that the significant covariation of AD and other disinhibitory disorders reflects a single dimension of externalizing psychopathology (Krueger and Markon, 2006; Krueger et al., 2002, 2005) that is highly heritable and genetically distinct from internalizing disorders, such as major depression (Kendler et al., 2003; Krueger et al., 2002). Thus, the initial aim of this study was to assess the influence of degree of severity of co-occurring symptoms of AD, childhood conduct disorder (CCD), adult antisocial behavior, marijuana dependence, and other drug dependence on decision making. Two theoretically distinct measures of decision-making performance on the IGT were evaluated: (i) insensitivity to future consequences (IFC), and (ii) preference for larger versus smaller rewards (PLvS). Although previous research suggests that disadvantageous decision biases observed on the IGT reflect a general IFC (e.g., Bechara and Damasio, 2002; Bechara et al., 2001; Grant et al., 2000), the original task confounds immediate reward magnitude and long-term net gain/loss. That is, decks with larger immediate rewards, in previous studies, have carried less frequent but larger magnitude losses. In this study, the decks were modified so that reward magnitude and net gain were counterbalanced and the probability of a loss was the same across all decks. This study also included a between-groups manipulation of reward “salience” that was related to a larger investigation designed to test the hypothesis that a vulnerability to substance abuse is associated with increased approach motivation manifested as an increased sensitivity to rewards (see Colder and O'Connor, 2002; Finn, 2002; Fowles, 1983).
The basic study design was a 2 × 2 [AD:CCD] independent-groups model which allows for an estimate of the relative influences of both AD and CCD on decision making. We chose to include CCD as a factor because our sample is younger (ages 18 to 30) and, while a history of CCD is a prerequisite for adult antisocial personality, it is often not assessed in studies of early-onset AD. Our primary hypothesis was that the combination of AD and a history of CCD would be associated with more disadvantageous decision making than AD without CCD, because the combination of AD and CCD represents a more severe form of externalizing psychopathology (Finn et al., 2002). Additionally, structural equation modeling was used to examine the association between a dimensional model with a single latent disinhibitory disorders factor and decision making on the task. Our recruitment strategy was designed to ensure sufficient variation and range in severity of lifetime problems with alcohol, marijuana, other drugs, CCD, and adult antisocial behavior. Because they are thought to reflect a general disinhibitory vulnerability, our hypothesis was that IFC and PLvS would be associated with the covariance among these disorders, rather than being specific to any one disinhibitory disorder.
METHOD
Participants
Recruitment
Participants were recruited from the community using advertisements in local and student newspapers and with flyers posted at various locations in the community including the university campus. These advertisements were designed using Widom's (1977) approach to elicit responses from individuals varying in terms of the level of impulsive, disinhibited traits and levels of alcohol use. The range of advertisements/flyers included those asking for “daring, rebellious, defiant individuals,” “carefree, adventurous individuals who have led exciting and impulsive lives,” “impulsive individuals,” “quiet, reflective and introspective persons,” “persons interested in psychological research,” “heavy drinkers wanted for psychological research,” and “social drinkers wanted for psychological research.”
Respondents were screened by telephone interview to determine if they met study inclusion criteria and were likely to meet the group inclusion criteria, assessed with a diagnostic interview (see Diagnostic ascertainment below) in their initial testing session. Those meeting study inclusion criteria were between ages 18 and 301, read and spoke English, had at least a grade 6 education level, did not report any severe head injuries, had no history of psychosis, and had consumed alcohol on at least one occasion in their life. Participants were given a group assignment after completing the semi-structured interview. Control group participants had no history of AD, CCD, antisocial personality (ASP), alcohol abuse or any other substance abuse or dependence. In addition, they reported (i) consuming more than 4 standard drinks on no more than one occasion in a typical month and no more than 6 drinks on any occasion in their life, (ii) using marijuananomorethantwice aweekand less than 25 timesintheir life, and (iii) not using any other mood altering drug in the last 6 months or recreationally more than 4 times in their life. The AD-alone group participants met DSM-IV criteria for a history of AD but neither CCD nor ASP. The CCD-alone group participants met DSM-IV criteria for a history of CCD but not AD. The ADCCD group participants met DSM-IV criteria for both a history of AD and CCD. To increase heterogeneity in our sample, participants in the AD-alone, CCD-alone, and ADCCD groups were allowed to have a history of alcohol abuse or other substance abuse/dependence.
Sample Characteristics
The sample consisted of 428 young adults: 105 (52 males, 53 females) control, 129 (69 males, 60 females) AD-alone, 60 (33 males, 27 females) CCD-alone, and 134 (77 males, 57 females) ADCCD. Note that the smaller sample size of the CCD-alone group is representative of a lower population base rate for CCD with no AD which makes it more difficult to recruit individuals for this group. Participants ranged in age from 18 to 30 years (M = 21.91; SD = 2.85) and in education from 6 to 22 years (M = 13.73; SD = 2.06). Approximately 77% (n = 328) were Caucasian, 13% (n = 56) were African-American, 7% (n = 31) Asian, and 3% (n = 13) were Hispanic.
Assessment
Diagnostic Ascertainment
Diagnoses of alcohol and other drug abuse/dependence, childhood conduct disorder, antisocial personality, and major depression were ascertained using the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994) applying criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV; American Psychiatric Association, 1994). Total lifetime problems in each area were determined by counting the number of positive responses to specific subsets of SSAGA questions. Table 1 displays group means and standard deviations for lifetime problems.
Table 1.
Lifetime Problems
| Controls |
CCD alone |
AD alone |
ADCCD |
|||||
|---|---|---|---|---|---|---|---|---|
| Measure | Males | Females | Males | Females | Males | Females | Males | Females |
| Alcohol lifetime problems | 3.79 (3.9) | 4.58 (5.2) | 16.64 (12.7) | 13.52 (10.9) | 36.90 (17.4) | 38.47 (15.0) | 47.44 (14.2) | 45.11 (14.7) |
| Marijuana lifetime problems | 0.42 (1.5) | 0.06 (0.3) | 10.18 (10.9) | 9.74 (9.6) | 10.87 (12.7) | 12.05 (10.7) | 19.19 (12.1) | 15.00 (10.7) |
| Other drug lifetime problems | 0.06 (0.4) | 0 (0.0) | 12.21 (19.7) | 15.52 (24.6) | 16.55 (31.0) | 14.82 (23.7) | 26.96 (31.1) | 28.79 (37.6) |
| Childhood conduct disorder lifetime problems | 5.77 (4.5) | 4.60 (3.8) | 17.21 (5.5) | 16.89 (5.1) | 12.99 (5.6) | 12.77 (5.1) | 20.27 (4.9) | 20.49 (4.5) |
| Adult antisocial lifetime problems | 4.52 (3.5) | 3.19 (3.3) | 16.18 (7.1) | 15.33 (6.1) | 12.74 (7.1) | 11.67 (5.8) | 21.97 (6.6) | 20.37 (6.5) |
| Major depression lifetime problems | 4.42 (5.3) | 4.85 (5.6) | 7.52 (6.1) | 10.63 (6.9) | 6.81 (6.6) | 11.88 (6.8) | 11.96 (6.8) | 14.35 (5.8) |
Values are given as mean (standard deviation).
Lifetime problems with alcohol, marijuana, drugs other than marijuana, conduct, adult antisocial, and depression are derived as a total count of positive responses to questions on the respective sections of the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA).
Alcohol and Other Drug Use
Alcohol use during the 6 months before participation in the study was quantified in 3 ways: average frequency (number of drinking occasions per week), average quantity (number of standard drinks per occasion), and density (maximum number of standard drinks on any occasion). Other drug use was quantified as the average frequency (days per week) of marijuana, stimulant, opiate, and sedative use during the 3 months before participation in the study. Table 2 provides the group means and standard deviations on alcohol/drug use and demographic data.
Table 2.
Sample Characteristics and Alcohol/Drug Use Variables (n = 428)
| Controls |
CCD alone |
AD alone |
ADCCD |
|||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | |
| Age | 21.06 (2.4) | 20.96 (1.8) | 22.79 (3.2) | 21.52 (2.6) | 22.01 (2.6) | 22.13 (3.1) | 22.31 (3.0) | 22.35 (3.4) |
| Education (years) | 14.31 (1.9) | 14.74 (1.6) | 13.36 (2.4) | 13.48 (1.7) | 14.12 (1.7) | 14.13 (1.9) | 13.01 (2.3) | 12.65 (2.0) |
| General intelligence | 109.24 (8.1) | 107.45 (8.6) | 106.21 (11.8) | 104.30 (8.6) | 105.46 (7.0) | 104.47 (8.2) | 101.76 (14.0) | 101.75 (9.7) |
| Alcohol | ||||||||
| Frequency | 1.69 (1.1) | 1.74 (1.5) | 2.91 (2.0) | 1.81 (1.7) | 3.87 (1.7) | 3.55 (2.5) | 4.16 (2.2) | 3.70 (2.3) |
| Quantity | 2.95 (1.9) | 2.24 (2.0) | 4.20 (4.7) | 2.23 (2.3) | 7.98 (4.6) | 5.18 (3.9) | 9.04 (5.4) | 6.69 (4.8) |
| Density | 3.11 (1.9) | 2.61 (2.6) | 5.91 (8.6) | 2.78 (3.0) | 11.30 (7.8) | 7.97 (6.0) | 12.82 (8.9) | 8.78 (6.1) |
| Drug frequencies | ||||||||
| Marijuana | 0.10 (0.4) | 0.15 (0.5) | 2.64 (3.0) | 2.00 (2.7) | 2.32 (3.0) | 3.25 (3.0) | 3.69 (3.2) | 3.40 (3.3) |
| Stimulants | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.63 (1.5) | 0.32 (1.1) | 0.33 (1.0) | 0.25 (0.8) | 0.67 (1.5) |
| Sedatives | 0.0 (0.0) | 0.0 (0.0) | 0.06 (0.3) | 0.37 (1.4) | 0.43 (1.5) | 0.55 (1.5) | 0.60 (1.5) | 1.05 (2.2) |
| Opiates | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.26 (1.3) | 0.17 (0.7) | 0.30 (1.3) | 0.36 (1.4) | 0.74 (1.8) |
Values are given as mean (standard deviation).
General intelligence was measured using the Shipley Institute of Living Scale estimate of IQ.
Alcohol frequency = number of drinking occasions in an average week during the 6 months prior to testing.
Alcohol quantity = average number of drinks consumed per occasion during the 6 months prior to testing.
Alcohol density = maximum number of drinks consumed on any one occasion during the 6 months prior to testing.
Drug frequencies = number of occasions of use in an average week during the 3 months prior to testing.
General Intelligence
The Shipley Institute of Living Scale (Zachary, 1986) estimate of IQ was used to assess general intelligence. This is a convenient self-administered measure of intelligence that correlates strongly (median correlation = 0.79) with the WAIS Full Scale IQ (Zachary, 1986). Lower Shipley IQ estimates have been associated with disadvantageous decision making on the IGT (Mazas et al., 2000) and externalizing problems (Finn et al., 2002).
Gambling Task
Our modified version of the original IGT (Bechara et al., 1994) was played under 2 payment conditions intended to model different levels of reward salience. In one condition, the participant played with real U.S. currency and received the amount won on the task that day. In the other condition, the participant played with fake currency and received payment after a 3-week delay. The same card decks were used in each payment condition. Immediate reward was varied by having the amount won on each card equal $1.00 for 2 decks and $0.50 for 2 decks. Net gain was varied by having 3 cards within each 10 card block carry losing amounts ranging from $0.75 to $5.00. Unlike previous versions of the IGT, one of the larger and one of the smaller reward decks (A and C) yielded a net gain of $2.50 over every 10 draws. The other 2 decks, one of the larger and smaller (B and D), yielded a net loss of $2.50 over every 10 draws (Table 3). Although this modified task eliminates the confound between magnitude of immediate win and long-term loss, average losses on decks A and B remain larger than those on decks C and D (Table 4). Each deck consisted of 60 cards with a loss probability of 0.33 for each deck.
Table 3.
Immediate and Net Gains/Losses
| Deck | Amount won on each draw |
Net over 10 draws |
Maximum gain/loss over 60 draws |
|---|---|---|---|
| A | $1.00 | +2.50 | +15.00 |
| B | $1.00 | −2.50 | −15.00 |
| C | $0.50 | +2.50 | +15.00 |
| D | $0.50 | −2.50 | −15.00 |
Table 4.
Loss Values
| Deck | Loss values (every 10 cards) |
Net over 10 draws |
||
|---|---|---|---|---|
| A | 2.00 | 2.50 | 3.00 | 7.50 |
| B | 3.50 | 4.00 | 5.00 | 12.50 |
| C | 0.75 | 0.75 | 1.00 | 2.50 |
| D | 2.00 | 2.50 | 3.00 | 7.50 |
The 3 loss values were randomly interspersed through every block of 10 cards.
Each participant started the task with $10.00 either in real US currency (immediate payment condition) or in fake currency (delayed payment condition) and was told that he/she would receive the winnings either at the end of the task (immediate) or 3 weeks later (delayed). Unlike many previous studies with the IGT, choices made in this study resulted in real rather than hypothetical monetary gains or losses. Each participant was instructed (i) to choose 1 card at a time from 1 of the 4 decks, (ii) that some cards win money and others have both a win and a loss (e.g., Win $1.00 AND Lose $1.50 resulting in a net loss of $0.50), and (iii) that the objective of the task was to “win as much money (real or fake) as possible.” After each choice, the amount indicated on the card was either added to or subtracted from the participant's net balance. Participants never lost any of their own money.
Procedure
Informed written consent was obtained from each participant before testing began. Participants were given a breath alcohol test using an AlcoSensor IV (Intoximeters Inc., St. Louis, MO) and asked about their alcohol and drug use over the past 24 hours. Participants were rescheduled if their breath alcohol level was greater than 0.0%, if they reported consuming any drug within the past 12 hours, if they reported feeling hung-over, or if they behaved impaired, high, overly sleepy, or unable to attend to questions. Participants were scheduled for three 2.5-hour testing sessions; these sessions included laboratory protocols that were part of a larger IRB-approved study. Participants were paid $10.00 per hour. The total hourly compensation was paid after the study was completed.
Data Analysis
Dependent Measures
Two measures of decision-making performance were derived for each participant. The first measure represents a preference to choose more cards from large versus small immediate reward decks (PLvS) and is equal to the number of cards selected from the $1.00 decks (A and B) minus the number of cards selected from the $0.50 decks (C and D). The second measure represents an IFC and is equal to the number of cards selected from the $2.50 net-loss decks (B and D) minus the number of cards selected from the $2.50 net-gain decks (A and C). Each measure can range between −120 and +120 because there are 60 cards in each deck.
Diagnostic Group-Based Analysis
Each decision-making measure (PLvS and IFC) was analyzed separately with a 2 × 2 × 2 × 2 (AD by CCD by Gender by Payment) univariate analysis of variance (ANOVA).
Multivariate Modeling
Because of their skewed distribution, all measures of lifetime problems were Blom transformed for the structural equation model (SEM) analyses. Blom transformation is considered to be the optimal approach to handling psychiatric symptom counts in multivariate modeling analyses (Krueger et al., 2002; Van den Oord et al., 2000) The multivariate analyses were conducted in 3 stages. First, a SEM was used to assess the relationship between the 2 exogenous lifetime problem variables (i.e., a latent disinhibitory disorders factor and an observed variable representing lifetime problems with major depression) and the 2 endogenous variables of decision-making (i.e., PLvS and IFC). The disinhibitory disorders (DD) latent factor was measured by 5 Blom-transformed indicators of lifetime problems with alcohol (ALC), marijuana (MAR), other drugs (DRG), childhood conduct disorder (CCD), and adult antisocial behavior (AAB). Modification indices were used to assess if any of the individual indicators of the DD variable were uniquely associated with either PLvS or IFC. The second stage of SEM assessed the influence of general intelligence on IFC and PLvS and whether general intelligence accounted for any significant associations between the exogenous and endogenous variables. The third stage of SEM analyses assessed the direct influence of alcohol and drug use on IFC and PLvS and whether alcohol or drug use accounted for any observed association between the exogenous factors and either IFC or PLvS. All exogenous variables were allowed to freely covary in these models. The Bentler and Bonett (1980) normed-fit index (NFI) and the root mean square error of approximation (RMSEA; Browne and Cudek, 1993) were used to assess goodness-of-fit. An acceptable model approximation to the data should yield an NFI >0.94 and an RMSEA ≤0.05.
RESULTS
Group Characteristics
A 2 × 2 × 2 (AD by CCD by Gender) ANOVA model was used to examine group differences in age, education, IQ, alcohol and drug use. None of the interactions on these measures were statistically significant. However, there were significant main effects of both AD and CCD on age, Fs (1,420) = 4.65 and 5.91, ps < 0.05, years of education, Fs (1,420) = 6.07 and 35.81, ps < 0.05 and 0.001, and Shipley IQ scores, Fs (1,420) = 12.00 and 10.10, ps < 0.005, respectively (cf. Table 2). AD and CCD were associated with being older, having fewer years of education, and lower Shipley IQ scores2.
Alcohol and Substance Use
There were significant main effects of AD on all measures of alcohol use (quantity, frequency, and density), Fs (1,420) = 106.18, 79.99, and 100.71, respectively, ps < 0.001. AD participants also used all other drugs more frequently than non-AD participants, Fs (1,420) = 50.27, 15.27, 8.48, and 5.80, ps < 0.05, for marijuana, sedatives, opiates, and stimulants, respectively. There were significant main effects of CCD on all measures of alcohol use, Fs (1,420) = 5.19, 4.74, and 4.04, ps < 0.05, and on frequency of marijuana, opiate, and stimulant use, F (1,420) = 29.05, 3.85, 5.25, ps < 0.05. Approximately half of the participants (n = 216) were tested in the delayed payment condition and half (n = 212) were tested in the immediate payment condition. There were no differences between the payment conditions either in symptoms of AD, numbers of participants with AD, symptoms of CCD, or in number of participants with CCD.
Decision Making: Effects of AD, CCD, Gender, and Payment Condition
PLvS
The univariate ANOVA with PLvS as the dependent variable revealed no significant interactions and no significant main effects of AD, CCD, gender, or payment, Fs = 3.32, 2.06, 0.0, 0.16, ns.
IFC
The univariate ANOVA with IFC as the dependent variable showed a significant three-way AD × gender × payment interaction, F (1, 412) = 5.98, p < 0.05, a significant two-way AD × gender interaction, F (1, 412) = 5.28, p < 0.05, and main effects of both AD, F (1, 412) = 7.45, p < 0.01, standardized effect size (Cohen's d) = 0.29, and CCD, F (1, 412) = 10.18, p < 0.005, Cohen's d = 0.28. On average, AD participants had higher IFC scores (M = −14.83, SD = 28.23) than non-AD participants (M = −23.21, SD = 30.01), and CCD participants had higher IFC scores (M = −13.34, SD = 29.99) than non-CCD participants (M = −21.97, SD = 27.96). Figure 1 shows the overall AD and CCD main effects of individual group means for IFC collapsed across gender and payment for each group.
Fig. 1.
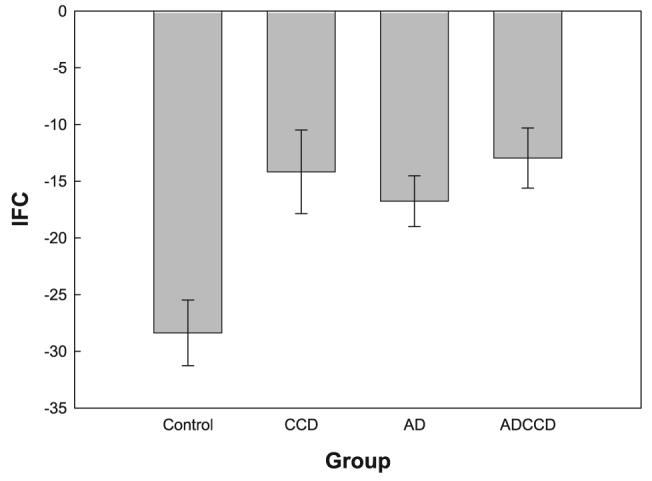
Mean insensitivity to future consequences (IFC) scores for each group. Lower scores reflect better performance on the task. Error bars represent the standard error of the mean.
To clarify the nature of the AD × gender × payment interaction, separate significance tests of the two-way AD × gender interaction within both levels of payment were performed. These tests revealed a significant AD × gender interaction within the immediate payment condition, F (1, 412) = 8.56, p < 0.01, but not within the delayed payment condition, F (1, 412) = 0.00, ns. Simple main effects analyses revealed a significant main effect of payment for non-AD women, F (1,412) = 6.52, p < 0.001, Cohen's d = 0.65. There were no significant main effects of payment for AD women, AD men, or non-AD men, Fs (1,412) = 0.81, 0.59, 0.03, ns. AD women had higher IFC scores than non-AD women in the immediate payment condition, F (1,412) = 35.62, p < 0.0001, Cohen's d = 0.97. AD women did not differ from non-AD women in the delayed payment condition, F (1,412) = 0.83, ns. These effects are illustrated in Fig. 2.
Fig. 2.
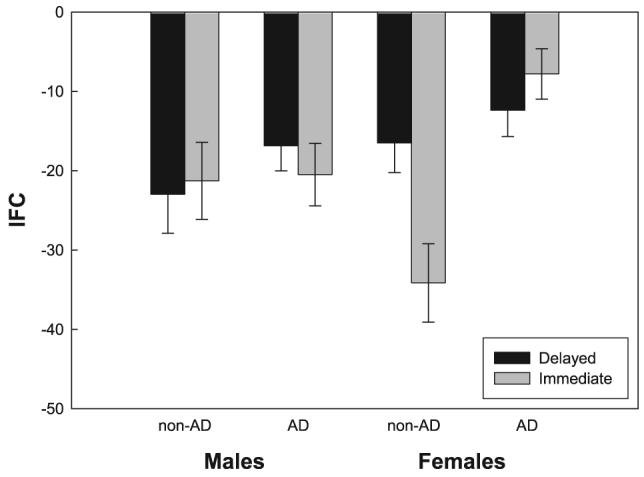
Mean insensitivity to future consequences (IFC) scores by payment condition for AD and non-AD males and females. Error bars represent the standard error of the mean.
Multivariate Analyses
Sample correlation coefficients (Pearson product-moment) among all variables included in the SEM are shown in Table 5.
Table 5.
Correlations Among Lifetime Problems, IQ, and Decision-Making Measures
| ALC | MAR | DRG | CCD | AAB | MD | IQ | PLvS | IFC | |
|---|---|---|---|---|---|---|---|---|---|
| ALC | 1 | 0.654** | 0.584** | 0.633** | 0.684** | 0.470** | −0.260** | 0.059 | 0.171** |
| MAR | 1 | 0.678** | 0.573** | 0.589** | 0.413** | −0.190** | 0.006 | 0.193** | |
| DRG | 1 | 0.535** | 0.576** | 0.376** | −0.290** | 0.027 | 0.208** | ||
| CCD | 1 | 0.842** | 0.449** | −0.329** | 0.051 | 0.197** | |||
| AAB | 1 | 0.473** | −0.290** | 0.108* | 0.200** | ||||
| MD | 1 | −0.189** | 0.009 | 0.168** | |||||
| IQ | 1 | −0.024 | −0.238** | ||||||
| PLvS | 1 | 0.194** | |||||||
| IFC | 1 |
All measures of lifetime problems are Blom-transformed.
ALC, alcohol lifetime problems; MAR, marijuana lifetime problems; DRG, other drug lifetime problems; CCD, childhood conduct disorder lifetime problems; AAB, adult antisocial behavior lifetime problems; MD, major depression lifetime problems; IQ, Shipley IQ score; PLvS, preference for large versus small decks; IFC, insensitivity to future consequences.
p < 0.01
p < 0.05
The first SEM fit the data well, χ2(13, n = 428) = 13.51, p = 0.41, NFI = 0.991, RMSEA = 0.01. The path from the DD factor and IFC was significant, β = 0.22, p < 0.001. Although this model fit the data very well, inspection of the modification indices suggested that adding a direct path from adult antisocial behavior (AAB) to PLvS would significantly improve the model fit (modification index = 7.1). Re-specifying the model to include a path from AAB to PLvS improved the overall fit, χ2(12, n = 428) = 9.12, p = 0.69, NFI = 0.994, RMSEA = 0.001. Figure 3 displays this SEM and includes only the significant regression paths. In this model, the standardized regression coefficient from AAB to PLvS was significant, β = 0.24, p < 0.05, as was the coefficient from the DD factor to IFC, β = 0.22, p < 0.001. Despite the fit of this model to the data, it explained only 6% of the total variance in IFC scores and 2% of the variance in PLvS.
Fig. 3.
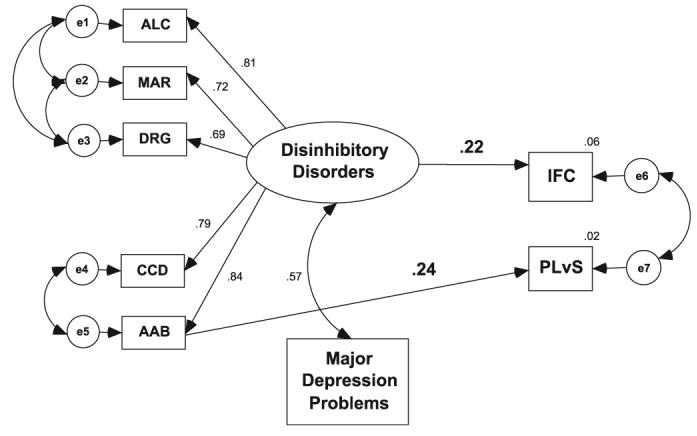
First stage Structural Equation Model (SEM) including the latent disinhibitory disorders factor and lifetime major depression problems as exogenous variables and insensitivity to future consequences (IFC) and preference for larger versus small immediate reward (PLvS) decision-making dependent variables. Indicators for the disinhibitory disorders factor are Blom transformed lifetime problems with alcohol (ALC), marijuana (MAR), other drugs (DRG), childhood conduct disorder (CCD), and adult antisocial behavior (AAB). Coefficients are displayed only for those paths that are statistically significant.
Because there was no evidence for a main effect of gender or payment condition on decision-making performance, neither was included as a grouping factor in the initial structural model. However, because of the presence of significant three-and two-way interactions involving gender and payment on IFC, multiple-group analyses were used to specifically evaluate the effects of gender and payment condition on the associations between the DD factor and IFC and AAB and PLvS. These multiple-group analyses revealed no significant differences between genders or payment conditions.
In the next stage of SEM, the Shipley IQ estimate was added to the model as an exogenous variable to assess the association between IQ and IFC and PLvS and to assess whether intelligence accounted for either the association between DD and IFC or AAB and PLvS. This model, shown in Fig. 4, fit the data well, χ2(18, n = 428) = 25.17, p = 0.12, NFI = 0.985, RMSEA = 0.031. The standardized regression coefficient for the path from the DD factor to IFC was significant, β = 0.19, p < 0.001, as was the path from AAB to PLvS, β = 0.27, p < 0.05. The additional path from IQ to IFC was significant, β = −0.17, p < 0.001 and the total variance explained in IFC increased from 6 to 9%.
Fig. 4.

Second stage SEM including the Shipley IQ estimate as an exogenous covariate. Coefficients are displayed only for those paths that are statistically significant.
The final stage of SEM involved adding the substance use latent factors to the model outlined in the second stage to assess the association between substance use and the decision-making measures and the extent to which substance use accounted for either the association between DD and IFC or AAB and PLvS. Figure 5A illustrates the model that included the alcohol use latent factor. This model fit the data poorly, χ2(44, n = 428) = 142.99, p < 0.001, NFI = 0.954, RMSEA = 0.073. Figure 5B illustrates the model that included the drug use latent factor. This model also fit the data poorly, χ2(55, n = 428) = 186.00, p < 0.001, NFI = 0.913, RMSEA = 0.075.
Fig 5.

(A) Third stage SEM including the latent variable for alcohol use as an exogeneous variable. Alcohol use indicators were Blom transformed measures of average quantity (QTY) per occasion, frequency (FRQ) per week, and density (DEN) of alcohol use in the past 6 months. Coefficients are displayed only for those paths that are statistically significant. (B) Third stage SEM including the latent variable for drug use as an exogeneous variable. Drug use indicators were Blom transformed measures of average frequency (per week) of marijuana (MAR), stimulant (STM), opiate (OP), and sedative (SED) use in the past 3 months. Coefficients are displayed only for those paths that are statistically significant.
DISCUSSION
There were 2 main goals of this study: (i) to assess the influence of co-occurring symptoms of AD, CCD, adult antisocial behavior, marijuana and other drug dependence on measures of decision making by using a dimensional model of AD and these related disorders, and (ii) to test the hypothesis that decision-making biases in those with AD with a history of CCD are associated with a greater IFC, rather than a preference to choose cards from large versus small immediate reward decks (PLvS). Diagnostic, univariate analyses showed that both AD and CCD were significantly associated with greater IFC, but the ADCCD group did not differ from the AD-alone or the CCD-alone groups in IFC bias as hypothesized. These analyses also suggested that the immediate payment condition significantly improved the decision making of the non-AD women compared to AD women, but had no effect on non-AD or AD men. The dimensional models indicated that the covariance among problems with alcohol, marijuana, other drugs, childhood conduct and adult antisocial behavior was associated with a greater IFC, but none was associated with IFC beyond their shared covariance. However, the SEMs suggested that adult antisocial behavior was uniquely associated with an increased PLvS and this association was not shared with the other disinhibitory disorders. General intelligence was associated with the disinhibitory disorders factor and greater IFC, but not with PLvS. The SEMs also suggested that general intelligence did not account for the association between the disinhibitory disorders factor and IFC. Finally, the SEMs suggested that recent alcohol and other drug use was not associated with either IFC or PLvS and did not account for the associations between the disinhibitory disorders factor and greater IFC or adult antisocial behavior and increased PLvS.
The SEM results showed that this dimensional model of disinhibitory disorders fit the data well. The measurement model of the disinhibitory disorders is identical to the externalizing dimension studied by Krueger and colleagues (Krueger and Markon, 2006; Krueger et al., 2002). This disinhibitory disorders factor reflects Gorenstein and Newman's (1980) construct of disinhibitory psychopathology, whichishypothesizedtoindicate a general lack of behavioral inhibition, especially in order to avoid negative consequences. Our results are consistent with the general interpretation that disadvantageous decision making on laboratory tasks like the IGT in disinhibited samples reflects a general neglect of future consequences (Bechara et al., 2002; Bechara et al., 2001; Grant et al., 2000), rather than a specific sensitivity to larger immediate rewards or lower general intelligence. The results also are consistent with Gorenstein and Newman's (1980) theory about the critical processes that contribute to disinhibitory disorders. However, the SEMs showed that adult antisocial behavior was uniquely associated with a tendency to choose more cards from the larger versus smaller immediate reward decks. This suggests that a unique aspect of adulthood antisociality, unrelated to CCD, substance use problems, and general intelligence, is modestly associated with a greater preference for larger versus smaller immediate rewards.
In the original version of the IGT, it is difficult to determine exactly what processes underlie the decision-making problems characteristic of substance abusers and antisocial individuals because of the confound between the magnitude of immediate reward and long-term negative consequences. By counterbalancing net gain within large and small reward decks, we observed that both AD and a history of CCD were significantly associated with greater IFC, but not with PLvS. Our results indicated that all 3 clinical groups had similar IFC scores and are not consistent with our hypothesis that the combination of AD and CCD would be associated with greater disadvantageous decision making compared with AD-alone subjects. These results, like the results of the structural models, suggest that the decision-making biases in disinhibited populations on IGT—like measures reflect a relative insensitivity to future negative consequences.
It is possible that disadvantageous decision making on the IGT reflects an underlying vulnerability toward impaired global decision making that is present only in a subset of those with disinhibitory psychopathology. Some research suggests that antisocial psychopathology or disinhibited personality predicts more disadvantageous decision making on the IGT in substance abusers (Mazas et al., 2000; Stout et al., 2005), however not all studies observe these associations (Fein et al., 2004). Research also suggests that neuropsychological tests of cognitive function do not predict more disadvantageous decision making on the IGT in those with disinhibitory disorders (Bazanis et al., 2002; Bechara et al., 2001). Fein et al. (2006a) observed disadvantageous decision making on the IGT in long-term abstinent alcoholics but not in younger, treatment naïve alcoholics (Fein et al., 2006a), prompting them to suggest that AD associated with disadvantageous decision making on the IGT may represent a more virulent form of alcoholism (Fein et al., 2006b). Studies have not yet identified any phenotypes (neuropsychological, behavioral, or personality) that reliably distinguish subpopulations with dis-inhibitory disorders who show poorer performance on the IGT from those who do not (Bazanis et al., 2002; Bechara et al., 2001; Fein et al., 2004).
The results of studies using the IGT and other studies of decision making in substance abusers and antisocial individuals highlight the complex nature of the processes that contribute to self-regulation and decision making in these populations. A problem with relying solely on laboratory tasks of decision making to understand the processes that affect decisions about substance use is that these tasks do not reflect typical decision-making contexts and thus, may not adequately capture the contextual, emotional, or motivational factors that affect decision making in those with AD or other disinhibitory disorders. In those with substance use disorders, decisions to use alcohol/drugs are directly tied to physical drug cues, internal motivational states, such as craving, current blood alcohol/drug levels, past experience with the substance, and current environmental contexts for alcohol or drug consumption (Finn, 2002; Tiffany and Conklin, 2000). Future studies should attempt to examine the influence of different environmental cues, internal motivational states, and relevant environmental contexts on decisions to drink or use drugs by using either new tasks or creative adaptations of the IGT, such as scenario-based decision tasks using specific motivational/emotional priming (e.g., Conklin and Tiffany, 2001), decision tasks conducted in virtual reality environments or laboratory environments that simulate relevant contexts, such as bars, or social gatherings.
Our results indicated that the immediate payment condition significantly improved the decision making of the non-AD women compared to AD women. This specific effect is difficult to interpret. Although not specifically associated with AD or CCD, this effect is fairly strong and worth further investigation. Additionally, research targeting the possibility that disadvantageous decision making on the IGT marks a subpopulation of disinhibited populations is necessary. Our results also suggested that adult antisociality is uniquely associated with a greater preference for larger versus smaller immediate rewards. Future research needs to replicate this finding before a strong conclusion can be made.
Although the association between the disinhibitory disorders factor and IFC was statistically significant, the latent dis-inhibitory disorders factor accounts for only 6% of the variance in IFC. Similarly, adult antisocial behavior accounts for only 2% of the variance in PLvS. These results are consistent with previous studies in which substance use and antisocial disorders accounted for only a small proportion of the variance in decision-making performance (Bechara et al., 2001; Fein et al., 2004; Dom et al., 2006; Grant et al., 2000; Mazas et al., 2000; Petry et al., 1998; Stout et al., 2005; Van Honk et al., 2002). Therefore, the decision-making processes elicited and modeled by the IGT may not be the same as those underlying substance-use and behavioral problems in more realistic contexts.
It is also important to note that our IGT differed from Bechara et al. (1994) in terms of the relative probability of incurring a net loss across decks. Specifically, in the original IGT, the probability of encountering a net loss varied across decks (0.10 or 0.50). In our version, the loss probability was the same for all decks (0.33). Equating the probability allows us to interpret effects of magnitude of immediate reward and long-term negative consequences directly since across-deck variation in the relative frequency of loss cannot be contributing to performance. Although research using the IGT with disinhibited populations do not report significant effects linked to the probability of loss, the extent to which variation in the relative frequencies of losses contributes to the overall pattern of results cannot be determined. Unfortunately, differences in the deck gain/losses, probabilities of loss, and payment conditions limit comparison with previous IGT studies. Additionally, our sample was recruited from the community, which means that the results of this study are not directly comparable to those using treatment samples (e.g.,Bechara and Damasio, 2002; Bechara et al. 2002; Grant et al., 2000; Petry et al., 1998).
In summary, IFC may contribute significantly to poor decision making exhibited by individuals with disinhibitory disorders. More importantly, this insensitivity appears directly associated with shared variability among disorders defining a broader spectrum of externalizing psychopathology. Conversely, choosing large over small immediate rewards regardless of long-term outcome may uniquely reflect specific component disorders of this spectrum, such as adult antisocial behavior. Finally, the disinhibitory factor accounted for less than 10% of the total variance in our decision-making measures, suggesting that the IGT is not the optimal task for investigating the factors that contribute to the poor decision making of these populations. This underscores the need for more ecologically valid studies of decision making.
ACKNOWLEDGMENTS
This work was conducted at the Department of Psychological and Brain Sciences, Indiana University, Bloomington, IN 47405. This research was supported by National Institutes of Alcohol Abuse and Alcoholism grant R01 AA13650 to Peter R. Finn. Hope Cantrell was supported on grant T32 AA07642 during this research. H. Cantrell, P. R. Finn, M. E. Rickert, and J. Lucas are at the Department of Psychological and Brain Sciences, Indiana University in Bloomington. The authors thank Dr. Tim Bogg for his contributions to this research.
Footnotes
The larger, IRB-approved study focused on early-onset alcohol dependence, which limited the age of participants.
These ANOVA results should be interpreted with caution because the variance within groups differed significantly (based on Levene's test for equality of variance) on these demographic variables.
REFERENCES
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bazanis E, Rogers RD, Dowson JH, Taylor P, Meux C, Staley C, Nevinson-Andrews D, Taylor C, Robbins TW, Sahakian BJ. Neurocognitive deficits in decision-making and planning in patients with DSM-III-R borderline personality disorder. Psychol Med. 2002;32:1395–1405. doi: 10.1017/s0033291702006657. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H. Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before knowing the advantageous strategy. Science. 1997;275:1293–1295. doi: 10.1126/science.275.5304.1293. [DOI] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39:376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Hindes A. Decision-making and addiction (part II):myopia for the future or hypersensitivity to reward. Neuropsychologia. 2002;40:1690–1705. doi: 10.1016/s0028-3932(02)00016-7. [DOI] [PubMed] [Google Scholar]
- Bechara A, Martin EM. Impaired decision making related to working memory deficits in individuals with substance addictions. Neuropsychology. 2004;18:152–162. doi: 10.1037/0894-4105.18.1.152. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- Browne MW, Cudek R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Bucholz K, Cadoret R, Cloninger CR, Dinwiddie S, Hesselbrock V, Nurberger J, Reich T, Schmit I, Schuckit M. A new, semistructured psychiatric interview for use in genetic linkage studies: a report of the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Colder CR, O'Connor R. Attention bias and disinhibited behavior as predictors of alcohol use and enhancement reasons for drinking. Psychol Addict Behav. 2002;16:325–332. [PubMed] [Google Scholar]
- Conklin CA, Tiffany ST. The impact of imagining personalized versus standardized urge scenarios on cigarette craving and autonomic reactivity. Exp Clin Psychopharmacol. 2001;9:399–408. doi: 10.1037//1064-1297.9.4.399. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van den Brink W, Sabbe B. Decision-making deficits in alcohol-dependent patients with and without comorbid personality disorder. Alcohol Clin Exp Res. 2006;30:1670–1677. doi: 10.1111/j.1530-0277.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- Ernst M, Kimes AS, London ED, Matochik JA, Eldreth D, Tata S, Contoreggi C, Leff M, Bolla K. Neural substrates of decision making in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160:1061–1070. doi: 10.1176/appi.ajp.160.6.1061. [DOI] [PubMed] [Google Scholar]
- Fein G, Klein L, Finn P. Impairment on a simulated gambling task in long-term abstinent alcoholics. Alcohol Clin Exp Res. 2004;28:1487–1492. doi: 10.1097/01.alc.0000141642.39065.9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Landman B, Tran H, McGillivray S, Finn P, Barakos J, Moon K. Brain atrophy in long-term abstinent alcoholics who demonstrate impairment on a simulated gambling task. Neuroimage. 2006a;32:1465–1471. doi: 10.1016/j.neuroimage.2006.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, McGillivary S, Finn P. Normal performance on a simulated gambling task in treatment-naïve alcohol dependent individuals. Alcohol Clin Exp Res. 2006b;30:959–966. doi: 10.1111/j.1530-0277.2006.00109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR. Motivation, working memory and decision making: a cognitive-motivational theory of personality vulnerability to alcoholism. Behav Cogn Neurosci Rev. 2002;1:183–205. doi: 10.1177/1534582302001003001. [DOI] [PubMed] [Google Scholar]
- Finn PR, Kessler DN, Hussong AM. Risk for alcoholism and classical conditioning to signals for punishment: evidence for a weak behavioral inhibition system. J Abnorm Psychol. 1994;103:293–301. doi: 10.1037//0021-843x.103.2.293. [DOI] [PubMed] [Google Scholar]
- Finn PR, Mazas CA, Justus AN, Steinmetz J. Early-onset alcoholism with conduct disorder: go/no go learning deficits, working memory capacity, and personality. Alcohol Clin Exp Res. 2002;26:186–206. [PubMed] [Google Scholar]
- Finn PR, Sharkansky EJ, Viken R, West TL, Sandy J, Bufferd G. Heterogeneity in the families of sons of alcoholics: the impact of familial vulnerability type on offspring characteristics. J Abnorm Psychol. 1997;106:26–36. doi: 10.1037//0021-843x.106.1.26. [DOI] [PubMed] [Google Scholar]
- Fowles DC. Motivational effects on heart rate and electrodermal activity: implications for research on personality and psychopathology. J Res Pers. 1983;17:48–71. [Google Scholar]
- Gorenstein EE, Newman JP. Disinhibitory psychopathology: a new perspective and a model for research. Psychol Rev. 1980;87:301–315. [PubMed] [Google Scholar]
- Goudriaan AE, Grekin ER, Sher KJ. Decision making and binge drinking: a longitudinal study. Alcohol Clin Exp Res. 2007;31:928–938. doi: 10.1111/j.1530-0277.2007.00378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant S, Contoreggi C, London ED. Drug abusers show impaired performance in a laboratory test of decision making. Neuropsychologia. 2000;38:1180–1187. doi: 10.1016/s0028-3932(99)00158-x. [DOI] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN, Workman-Daniels KL. Effect of major depression and antisocial personality on alcoholism: course and motivational patterns. J Stud Alcohol. 1986;47:207–212. doi: 10.15288/jsa.1986.47.207. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kim YT, Lee SJ, Kim SH. Effects of the history of conduct disorder on the Iowa Gambling Tasks. Alcohol Clin Exp Res. 2006;30:466–472. doi: 10.1111/j.1530-0277.2006.00051.x. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick PJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick PJ, Iacono WG. Externalizing psychopathology in adulthood: a developmental-spectrum conceptualization and its implications for DSM-V. J Abnorm Psychol. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lykken DT. A study of anxiety in the sociopathic personality. J Abnorm Soc Psychol. 1957;55:6–10. doi: 10.1037/h0047232. [DOI] [PubMed] [Google Scholar]
- Mazas CA, Finn PR, Steinmetz JE. Decision-making biases, antisocial personality, and early-onset alcoholism. Alcohol Clin Exp Res. 2000;24:1036–1040. [PubMed] [Google Scholar]
- Mitchell DGV, Colledge E, Leonard A, Blair RJR. Risky decisions and response reversal: is there evidence of orbitofrontal cortex dysfunction in psychopathic individuals? Neuropsychologia. 2002;40:2013–2022. doi: 10.1016/s0028-3932(02)00056-8. [DOI] [PubMed] [Google Scholar]
- Newman JP. Reaction to punishment in extraverts and psychopaths: implications for the impulsive behavior of disinhibited individuals. J Res Pers. 1987;21:464–480. [Google Scholar]
- Petry NM, Bickel WK, Arnett M. Shortened time horizons and insensitivity to future consequences in heroin addicts. Addiction. 1998;93:729–738. doi: 10.1046/j.1360-0443.1998.9357298.x. [DOI] [PubMed] [Google Scholar]
- Rotheram-Fuller E, Shoptaw S, Berman SM, London ED. Impaired performance in a test of decision-making by opiate-dependent tobacco smokers. Drug Alcohol Depend. 2004;73:79–86. doi: 10.1016/j.drugalcdep.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Schmauk FJ. Punishment, arousal, and avoidance learning in socio-paths. J Abnorm Psychol. 1970;76:325–335. doi: 10.1037/h0030398. [DOI] [PubMed] [Google Scholar]
- Stout JC, Rock SL, Campbell MC, Busemeyer JR, Finn PR. Psychological processes underlying risky decisions in drug abusers. Psychol Addict Behav. 2005;19:148–157. doi: 10.1037/0893-164X.19.2.148. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Conklin CA. A cognitive processing model of alcohol craving and compulsive alcohol use. Addiction. 2000;95:S145–S153. doi: 10.1080/09652140050111717. [DOI] [PubMed] [Google Scholar]
- Van den Oord EJCG, Simonoff E, Eaves LJ, Pickles A, Silberg J, Maes H. An evaluation of different approaches for behavior genetic analyses with psychiatric symptom scores. Behav Genet. 2000;30:1–18. doi: 10.1023/a:1002095608946. [DOI] [PubMed] [Google Scholar]
- Van Honk J, Hermans EJ, Putman P, Montagne B, Schutter DJLG. Defective somatic markers in sub-clinical psychopathy. Cogn Neurosci Neuropsychol. 2002;13:1025–1027. doi: 10.1097/00001756-200206120-00009. [DOI] [PubMed] [Google Scholar]
- Widom CS. A method for studying noninstitutionalized psychopaths. J Consult Clin Psychol. 1977;44:614–623. [PubMed] [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale: Revised Manual. Western Psychological Services; Los Angeles, CA: 1986. [Google Scholar]
- Zucker RA, Ellis DA, Fitzgerald HE, Bingham C. Other evidence for at least two alcoholism II. Life course variation in antisociality and heterogeneity of alcoholic outcome. Dev Psychopathol. 1996;8:831–848. [Google Scholar]


