Abstract
Objective
Recent attention has focused on moving women from having initial mammograms to maintaining adherence to regular mammography schedules. We examined behavioral intentions to maintain mammography adherence, which include the likelihood of performing a behavior, and implementation intentions, specific action plans to obtain mammograms. Potential predictors were Theory of Planned Behavior constructs, previous barriers, previous mammography maintenance, and age.
Methods
Respondents were 2062 currently adherent women due for their next mammograms in 3–4 months according to American Cancer Society recommendations for annual screening. Statistical models were used to examine predictors of behavioral and two implementation intentions, including having thought about where women would get their next mammograms and having thought about making appointments.
Results
With the exception of pros, cons, and subjective norms, all variables predicted behavioral intentions (p ≤ 0.05). Stronger perceived control, previous mammography maintenance, and one barrier (vs. none) predicted being more likely to have thought about where to get their next mammograms. Previous maintenance and no barriers (vs. two) predicted being more likely to have thought about making appointments.
Conclusions
Our findings suggest that among women currently adherent to mammography, volitional factors, such as barriers, may be better predictors of implementation intentions than motivational factors, such as attitudes. Implementation variables may be useful in understanding how women move from intentions to action. Future research should examine how such factors relate to mammography maintenance behaviors and can be integrated into behavior change interventions.
Introduction
Approximately 70% of U.S. women report having had mammograms in the previous 1–2 years.1 Although this exceeds the Healthy People 2010 objective,2 vigilance is needed to counter slightly lower mammography rates in recent years.1 A more worrisome finding is that only 46% of age-eligible women are characterized as getting regular mammograms on schedules likely to maximize the full benefit of mammography to reduce breast cancer morbidity and mortality.3 The public health challenge is both to motivate women to have their first mammograms1,4,5 and to maintain adherence to mammography on age-appropriate schedules6,7 recommended by major medical organizations.8–10 Although these organizations differ on precise recommended intervals, we focus on the American Cancer Society (ACS) guidelines that call for annual mammograms in all women aged ≥40 years.8 Based on this guideline, we define maintenance of mammography adherence as having a second mammogram no sooner than 10 months and no later than 14 months after the previous mammogram. Although specific findings are related to annual mammography, the broader constructs transcend the particular screening interval.
Important necessary conditions for performing recommended health behaviors, such as maintaining adherence to mammography, include behavioral intentions.11 When intention measures concern a specific behavior and are obtained reasonably close to the time the behavior is performed, intentions strongly predict behavior (r = 0.70).12 Despite this potential for strong correlations, many good intentions do not lead to intended behaviors.13,14 A major challenge and opportunity is to bridge the mammography intention-behavior divide.11
Fishbein and others have stressed the need to understand steps that occur between behavioral intentions and performance of health behaviors.11,12 Several conditions that facilitate strong relationships between behavioral intentions and health behaviors, such as mammography, are well documented.15–18 Intention-behavior inconsistencies may result, in part, from a lack of implementation intentions, defined as commitments to take specific actions needed to fulfill a behavioral goal or to transform intentions into behavior.19 Implementation intentions build on the idea of assessing a specific behavioral goal by breaking the behavior into specific actions toward fulfillment of the goal. In the case of mammography, implementation intentions would include knowing when and where to have a mammogram when it is due20 in addition to more precise information, such as arranging for time off work and for transportation.21 Women are more likely to complete cervical cancer screening,22 practice breast self-examinations,23and have mammograms21 if they have first formed implementation intentions to engage in these behaviors. Yet we know little about predictors of forming and holding implementation intentions in the absence of interventions.
Several studies have suggested that formation of implementation intentions can increase rates of one-time routine and diagnostic screening.21,23,24 To our knowledge, none have examined predictors of implementation intentions for mammography in a sample of women adherent for recent screening at the time of entry into the study, in other words, implementation intentions to maintain adherence to mammography. Implementation intentions seem to be most potent in prompting behaviors when behavioral intentions are strong.25 Women who have had recent mammograms report stronger behavioral intentions than those not recently screened,26 making consideration of implementation intentions particularly appealing. Examining predictors of implementation intentions to maintain adherence to mammography among currently adherent women may help to identify reasons why women intending to get mammograms are not screened on schedule.
Our examination of implementation intentions was guided by the Theory of Planned Behavior (TPB), a model that has informed prior studies of mammography intentions and behavior23,27–31 and implementation intentions.21 Constructs included in TPB—an individual's (1) attitudes toward the behavior, (2) perceived norms, (3) perceived behavioral control related to performing the behavior, and (4) behavioral intentions theorized to mediate fully the effects of attitudes and perceived norms on behavior—are included in many social-cognitive theories of health behavior change.11,32,33 Perceived behavioral control may have an especially strong influence on formation of implementation intentions. A recent intervention to encourage mammography screening that required women to form implementation intentions was more effective for women who held strong behavioral intentions but low perceived behavioral control.21 The authors concluded that women with a combination of high behavioral intentions to attend screening and low perceived control may be motivated to be screened but benefit from prompting to form implementation intentions that encourage future screening.
In addition to studies that have applied TPB to the study of implementation intentions, parallels have been drawn between implementation intentions and planning required in the latter stages of the Precaution Adoption Process Model (PAPM).34,35 In these latter stages, individuals move from motivation to volition and must confront obstacles that impede the behavioral goal.36,37 Thus, intentions to maintain adherence to mammography among currently adherent women may be governed more by volitional constructs, such as barriers. The degree to which women have experienced barriers in the past and the related ease associated with getting prior mammograms may influence women's plans for their next mammograms. Finally, we considered whether forming implementation intentions was predicted by previous mammography maintenance. Women who have maintained adherence to mammography should report stronger implementation intentions to do so in the future compared with those who have not been adherent.26
The current study
We examined TPB constructs, previous barriers, and previous mammography maintenance as predictors of behavioral and implementation intentions to maintain mammography adherence among women adherent to mammography at baseline. We predicted that all model variables would significantly predict behavioral intentions. We also explored their utility as predictors of implementation intentions. We considered two global components necessary for implementation intentions, including whether they had thought about where they would have their next mammograms and whether they had thought about making their appointments.
Materials and Methods
Study respondents
Eligible women were North Carolina residents enrolled with the North Carolina Teachers' and State Employees' Comprehensive Major Medical Plan (State Health Plan) for ≥2 years prior to sampling, had their last screening mammograms between September 2003 and September 2004 (to ensure all were adherent to recent mammograms on study entry), had only one mammogram within the designated timeframe (to exclude those who had diagnostic mammograms), had no personal history of breast cancer, and were between the ages of 40 and 75. All women had their last screening mammograms approximately 8–9 months before baseline telephone interviews.
Personally Relevant Information about Screening Mammography (PRISM) study recruitment occurred from October 2004 to April 2005. Researchers mailed invitation letters to a random sample of 9087 women who met eligibility criteria. Letters included required Health Insurance Portability and Accountability Act of 1996 (HIPAA) information and provided instructions for opting out of the study. Trained telephone interviewers from Battelle Centers for Public Health Research and Evaluation contacted potential participants to obtain their consent. The consent process and survey took an average of 31 minutes to complete. Interviewers made up to 12 attempts to contact women.
Of those invited, 3547 women completed baseline telephone interviews, 2051 refused to participate, and 747 were determined to be ineligible. The remaining 2742 women were classified as unknown eligibility once calls were initiated because their call attempts were exhausted (n = 2570) or their enrollment was no longer needed (n = 172) to reach the target sample size before we could verify eligibility. The range in response rates based on the American Association for Public Opinion Research Standard Definitions was 47.1%–63.7%.38 The lower response rate excludes a portion of women with unknown eligibility from response rate computation; the higher response rate excludes all women with unknown eligibility. These rates are consistent with trends toward declining national participation in surveys.39 We requested a level of engagement greater than would be required for most surveys, as we asked women to agree to be part of a 5-year intervention study.
The current report focuses on women for whom we could calculate previous mammography maintenance. We included only women aged ≥43 to allow us to include 2 full years of medical records. If they began having mammograms at age 40, women aged ≥43 could have received two annual mammograms needed to compute the measure of previous mammography maintenance. In addition, we included only women who had not yet made appointments for their next mammograms. Thus, all women in the sample would have to take several behavioral steps if they were to obtain their next mammograms on time.
Measures
Demographics
We assessed several sociodemographic variables, including age, race, marital status, education, and financial status (defined as overall financial situation), variables previously related to mammography use. Based on the literature, marital status was trichotomized as married/living as married, separated/divorced/widowed, and single/never married. Race was dichotomized as white and African American. Because too few women were in other racial groups to permit meaningful analysis, their data were excluded from analyses (n = 32; 7 Asian, 18 American Indian or Alaskan Native, 7 not defined or refused). Education was coded to indicate having completed twelve or fewer years of education (coded as 1), some college (2), college degree (3), and graduate degree (4). To minimize typically high levels of nonresponse to questions about income, we assessed financial status using an item previously shown to have high levels of completion: “Without giving exact dollars, how would you describe your household's financial situation right now?”40 A dichotomous variable indicated sufficient/limited financial status.
Previous mammography maintenance
All women were adherent for mammography at entry into the study. We calculated previous maintenance by determining if these women also had a second mammogram within our defined window, determined by self-report and confirmed via claims data. We created a dichotomous variable with 0 = not repeatedly adherent and 1 = repeatedly adherent.41
TPB constructs
This study was not designed to test TPB but rather to inform intervention development and evaluate interventions. Some TPB measures were adapted for study purposes.42
Attitudes
Research on TPB has demonstrated that attitudes toward a behavior are a combination of beliefs and an evaluation of the behavioral outcome.29 In practice, however, many studies use much simpler approaches. To reduce participant burden, we assessed the pros and cons related to mammography.43 We did not include an evaluation of the behavioral outcome, as previous experience indicates that most respondents would rate the outcome (not receiving mammograms or being diagnosed with breast cancer at a later stage) as very bad. When people routinely assess a behavioral outcome negatively, it may not be necessary to include such measures in the model.29 Therefore, beliefs about mammography are likely to be the key aspect of overall attitude toward mammography in this context. Measures of pros and cons, our measure of beliefs, are compatible with the way many typical TPB items are framed. Examples of our items included: “Mammograms are needed even when a woman has no family history of breast cancer,” and “Once you have a couple of mammograms that are normal, you don't need any more for a few years.” Pros and cons scales were computed by summing the six pros items and nine cons items. Similar to other recent studies,41 we do not report reliability statistics for pros and cons of mammography. These items capture different aspects of mammography that may not be related to each other.
Subjective norms
We assessed norms by asking, “Most people who are important to you think you should get a mammogram when you are due,” measured on a 4-point scale: 1 = strongly disagree, 2 = somewhat disagree, 3 = somewhat agree, 4 = strongly agree, and dichotomized as strongly agree/other.
Perceived behavioral control
We assessed perceived behavioral control using the item: “How much control do you have over whether you get a mammogram when you are due?” using a three-point scale (1 = no control, 2 = some control, 3 = complete control) that was dichotomized as complete control/other.
Previous barriers
We assessed barriers to mammography through open-ended and closed-ended questions developed in previous studies.44,45 First, we asked: “In the past, has anything ever delayed your getting a mammogram?” If yes, this was followed by: “What was the main reason that delayed your getting a mammogram?” and “In the past, did anything else delay your getting a mammogram?” This was asked until no other barriers were reported.
Participants then were asked 10 closed-ended questions about what might delay their next mammograms. Responses used 4-point scales, including strongly agree/disagree and somewhat agree/disagree. Barriers were considered present if respondents endorsed somewhat or strongly agree. Responses to open-ended and closed-ended questions were summed to determine the total number of barriers. Analyses included total number of barriers endorsed by respondents, categorized as 0, 1, and ≥2 barriers.
Intentions
Mammography behavioral intentions
On a 4-point scale (1 = very unlikely–4 = very likely), we assessed behavioral intentions using the item: “How likely or unlikely is it that you will have a mammogram when you are due?” Women who said they were very likely to have mammograms when due were categorized as having the strongest behavioral intentions.
Mammography implementation intentions
Two questions measured key global components for the formation of implementation intentions based on questions from published studies.46 “Have you thought about where you will have your next mammogram?” and “Have you thought about making the appointment?” These items assessed two key steps needed to move from more general intentions to action.
Statistical analyses
Analyses were conducted using SAS statistical software 9.1 (SAS Institute, Inc., Cary, NC). We calculated frequency distributions for variables of interest. To identify potential covariates, we examined relationships between outcome measures and participant demographics, such as age, income, education, race, marital, and financial status, using point biserial correlations and tested for confounding among study variables. Demographic variables significantly related to outcome variables were included in models. Skewness in the data was corrected using transformation. It was not possible to correct adequately for the skewness of subjective norms or perceived control through transformations, resulting in dichotomization of those variables.
Proportional odds models were used to predict behavioral intentions (four categories) and implementation intention components (two categories). These models yield odds ratios (ORs) and 95% confidence intervals (CIs) interpreted in ways similar to those obtained from binary logistic regression.
Results
Descriptive analyses
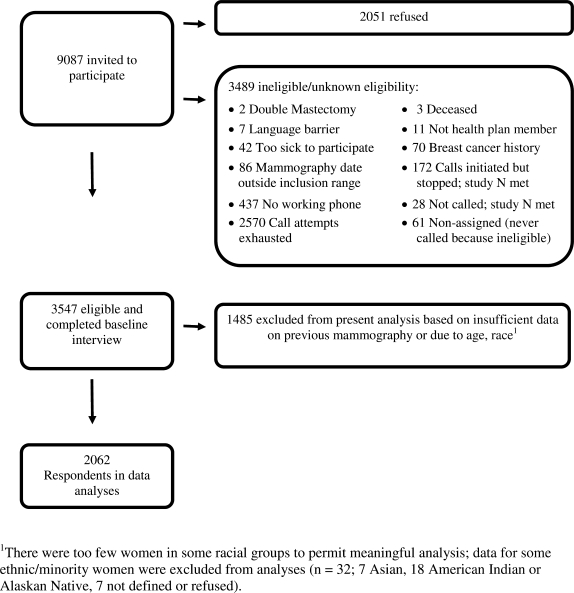
As seen in Figure 1, of 9087 women invited to participate, 3547 completed baseline interviews. We report data for 2062 women who met inclusion criteria, confirmed dates regarding their two most recent mammograms, and had not made appointments for their next mammograms. Most participants were white (90%), married or living as married (82%), and employed full-time (76%) (Table 1). Mean age was 55.52 years (SD = 5.64). Most women in the study held the strongest behavioral intentions; 93% (1911 of 2062) said they were very likely to get their next mammograms when due. Whereas 93% (1920 of 2062) of women had thought about where they would make their appointments, only 34% (698 of 2062) had thought about making appointments, even though they would be due for their next mammograms in 3–4 months.
FIG. 1.
Accrual process for study.
Table 1.
Sociodemographic Characteristics of Respondents and Model Variables (n = 2062)
| % | M | SD | |
|---|---|---|---|
| Age, years | 55.52 | 5.64 | |
| 43–49 | 15.9 | ||
| 50–59 | 57.2 | ||
| 60–74 | 26.9 | ||
| Race | |||
| White | 89.8 | ||
| Black | 10.2 | ||
| Hispanic | |||
| Yes | 0.4 | ||
| Marital status | |||
| Married/living as married | 82.1 | ||
| Widowed/divorced | 14.1 | ||
| Single/never married | 3.8 | ||
| Education | |||
| <12 years | 16.5 | ||
| Some college | 20.1 | ||
| College degree | 27.5 | ||
| Graduate degree | 35.9 | ||
| Employment status | |||
| Working for pay | 76.4 | ||
| Not working for pay | 23.6 | ||
| Perceived income | |||
| Sufficient | 93.7 | ||
| Limited | 6.3 | ||
| Previously adherent to mammography | 53.2 | ||
| Prosa | 23.02 | 0.22 | |
| Consb | 10.93 | 2.12 | |
| Perceived controlc | 2.80 | 0.43 | |
| Complete control | 81.0 | ||
| Some/no control | 19.0 | ||
| Subjective normd | 3.81 | 0.52 | |
| Strongly agree | 85.0 | ||
| Somewhat agree | |||
| Somewhat or strongly disagree | 15.0 | ||
| Total barriers | |||
| None | 27.4 | ||
| 1 | 27.0 | ||
| 2+ | 45.6 | ||
| Behavior intention | |||
| Likelihood of having next mammogram when due | |||
| Very likely | 92.7 | ||
| Somewhat likely | 6.1 | ||
| Somewhat unlikely | 0.6 | ||
| Very unlikely | 0.6 | ||
| Implementation intentions | |||
| Thought about where to have next mammogram | |||
| Yes | 93.1 | ||
| No | 6.9 | ||
| Thought about making an appointment for next mammogram | |||
| Yes | 33.9 | ||
| No | 66.1 | ||
Range = 6–24.
Range = 9–36.
Range = 1–3.
Range = 1–4.
Bivariate correlational analyses
As shown in Table 2, behavioral intentions and the two components of implementation intention were significantly but weakly correlated. Behavioral intentions were most strongly related to having thought about making an appointment (r = 0.10, p < 0.001) but also related to having thought about where (r = 0.06, p < 0.01). Age was significantly and positively related to behavioral intentions, such that the strength of intentions increased with age (r = 0.14, p < 0.001). No other demographic variables were related to behavioral or implementation intentions. For this reason, race, employment, education, marital status, and financial status were not included in subsequent analyses.
Table 2.
Correlations among Predictors, Behavioral Intentions, and Implementation Intentionsa
| Behavioral intentions | Thought about where | Thought about appointment | Pros | Cons | Subjective norms | Perceived control | Age | Previous mammograpy maintenance | Barriers | |
|---|---|---|---|---|---|---|---|---|---|---|
| Behavioral intentions | — | 0.06** | 0.10*** | −0.03 | −0.01 | 0.05* | 0.12*** | 0.14*** | 0.20*** | −0.15*** |
| Thought about where | 0.08*** | 0.00 | −0.02 | −0.02 | 0.05* | −0.02 | 0.06** | 0.00 | ||
| Thought about appointment | 0.01 | 0.02 | 0.02 | −0.03 | 0.01 | 0.14*** | −0.08*** | |||
| Pros | 0.34*** | −0.30*** | 0.00 | 0.00 | 0.00 | 0.03 | ||||
| Cons | −0.19*** | −0.04 | −0.02 | −0.01 | 0.03 | |||||
| Subjective norms | 0.02 | 0.02 | 0.04 | −0.04 | ||||||
| Perceived control | 0.09*** | 0.05* | −0.12*** | |||||||
| Age | 0.23*** | −0.13*** | ||||||||
| Previous mammography maintenance | −0.28*** | |||||||||
| Barriers | — |
Correlations reported are bivariate, point biserial correlations.
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001.
Multivariate analyses
Table 3 shows associations between model predictors and behavioral intentions. With the exception of pros, cons, and subjective norms, all variables in the model predicted behavioral intentions, with stronger rather than weaker behavioral intentions associated with older age, such that the odds of having stronger behavioral intentions go up by 5% with every year increase in age (OR = 1.05, p < 0.01), previous mammography maintenance (OR = 5.21, p < 0.001), stronger perceived behavioral control (OR = 2.07, p < 0.001), and barriers. Specifically, no barriers (vs. two barriers) predicted stronger behavioral intentions (OR = 0.26, p < 0.001). Those reporting no barriers vs. one barrier did not differ significantly in their behavioral intentions.
Table 3.
Relationship Between Predictors and Intentions: OR (95% CI)a
| Predictors | Behavioral intentions | Thought about where | Thought about appointment |
|---|---|---|---|
| Pros | 0.94 (0.47–1.91) | 1.11 (0.55–2.27) | 1.14 (0.79–1.65) |
| Cons | 1.13 (0.10–12.36) | 0.29 (0.03–2.96) | 1.90 (0.55–6.52) |
| Subjective norms | 1.51 (0.96–2.39) | 0.70 (0.41–1.22) | 1.14 (0.87–1.50) |
| Perceived control | 2.07 (1.42–3.01)*** | 1.57 (1.05–2.35)* | 0.81 (0.64–1.02) |
| Age | 1.05 (1.02–1.09)** | 0.98 (0.95–1.01) | 0.99 (0.98–1.01) |
| Previous mammography maintenance | 5.21 (3.23–8.40)*** | 1.78 (1.23–2.59)** | 1.73 (1.42–2.10)*** |
| Barriers | |||
| 0 vs. 1 | 0.59 (0.28–1.24) | 1.88 (1.14–3.12)* | 0.91 (0.71–1.16) |
| 0 vs. 2 | 0.26 (0.14–0.50)*** | 1.29 (0.85–1.96) | 0.79 (0.63–0.99)* |
All models satisfied the proportional odds assumption (p > 0.05) and were significant overall (p < 0.001).
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001.
The pattern of findings differed somewhat depending on which implementation intentions were used. Stronger rather than weaker implementation intentions about where to get their next mammograms when due were predicted by previous mammography maintenance (OR = 1.78, p < 0.01), stronger perceived control (OR = 1.57, p < 0.05), and barriers. Specifically, having one barrier (vs. no barriers) predicted greater likelihood of women having thought about where to get their next mammograms (OR = 1.88, p < 0.05). There was not a significant difference among those reporting no barriers vs. two barriers. Stronger rather than weaker implementation intentions for having thought about making an appointment were predicted only by previous mammography maintenance (OR = 1.73, p < 0.001) and barriers. Those with no barriers (vs. two barriers) were more likely to have thought about making an appointment (OR = 0.79, p < 0.05), but there was no difference between those reporting no barriers vs. one barrier.
Discussion
Among women who had mammograms in the past 8–9 months and were due for their next mammograms soon, most variables in the TPB-informed model significantly predicted behavioral intentions for having their next mammograms when due.47 Only a subset of these variables significantly predicted implementation intentions. Expressing complete behavioral control and reporting one barrier, as opposed to no barriers, were related to women having thought about where to get their next mammograms. Reporting no barriers, as opposed to two barriers, was related to having thought about making an appointment. Previous adherence to mammography maintenance, not surprisingly, was significant in all models.
Our findings complement previous intervention findings of Rutter et al.21 Their intervention, designed to encourage women to form implementation intentions as a strategy to enhance mammography use, was more effective when women held strong behavioral intentions but low perceived behavioral control. This makes sense because women who do not intend to get mammograms would not have had reasons to think about where or when they would make their appointments, an indicator of implementation intentions.
Our data suggest that those with higher perceived behavioral control were more likely to have thought about where they would get their next mammograms in the absence of intervention. Women who perceive less control about having their next mammograms on schedule may need additional encouragement to form implementation intentions to ensure that they are screened. Our results suggest that perceived behavioral control should be considered when examining mechanisms through which implementation intentions may act. It may be useful for physicians and other healthcare practitioners to assess the extent to which women believe they have some control over whether they get their next mammograms on time. This could be done with a direct question and appropriate feedback provided. Of course, more research would be needed to assess this assumption.
The degree to which perceptions of control match reality may vary over time and should be examined more fully. Although not significant, we found a trend toward women expressing complete control being less likely to have thought about making their mammography appointments. One of the many explanations for the overall decline in mammography rates may be the decline in the number of radiology facilities that perform mammograms.48,49 This may lengthen the time required between making appointments and actual appointments, requiring that appointments be scheduled months in advance and requiring greater planning, even among motivated women.50,51 Breen et al.48 stated that “it is not too early to consider what types of interventions would be needed should these downward trends continue.” Why reporting one barrier rather than no barriers is more predictive of women's mammograms is not entirely clear. Perhaps these women are more aware of what it takes to get mammograms because they have the self-awareness to realize that something stands in their way. Alternatively, having experienced a barrier in the past may prompt these women to think about where they would get their next mammograms.
Our findings also highlight differences between motivational and volitional constructs.52 Previous studies that have used TPB as a framework to examine implementation intentions for screening behaviors applied these to encourage one-time screening for those who had not been screened recently21 and found TPB to be useful in these settings. In contrast to previous studies, our sample included women who had recent mammograms and would be due again in the coming months.
The developers of PAPM highlighted differences between motivational and volitional phases and noted that variables that serve as powerful predictors for one stage may be irrelevant for another. For example, the detailed plans formed by currently adherent women would be irrelevant to women who remained in more motivational phases. Predictors of maintaining adherence to mammography (among currently adherent women) may not apply to intentions among other women This may explain, in part, why the majority of variables included in TPB were not significant predictors of intention in the present study. Previous studies using the PAPM have found that as individuals move toward maintenance, motivational factors, such as those included in TPB, become less important, and volitional factors, such as barriers related to performing the behavior, become more important.37 These differences and our overall findings underscore the need for increased attention to theories of implementation and implementation intentions. In addition to barriers and perceived control, other factors related to social-cognitive theory and behavioral self-regulation also may be relevant in this context.53,54
Likewise, age did not predict implementation intentions. This may have been due to our examination of implementation intentions for mammography in a sample of adherent women who had insurance coverage. A woman's age, along with other demographic variables that were not significantly related to our intention outcomes, may be less important to maintaining mammography than when considering initial uptake.
Previous mammography maintenance was the strongest predictor of intention in all statistical models. This is not surprising and is a consistent finding in behavioral research. Of issue, women who have been on schedule are more likely to remain so. Formation of implementation intentions attenuates the relationship between delay in previous cervical cancer screening and receipt of future screening.22 As our study progresses, we will examine the relationship to mammography use.
Our findings highlight relationships between behavioral and implementation intentions themselves. These constructs were weakly but significantly correlated (r ≤ 0.10). Whereas the vast majority of women said they were very likely to get their next mammograms when due and had thought about where they would make their appointments, only 34% had thought about making appointments. Without thinking about making appointments, it is unlikely that many of these women will have their mammograms when due. This is especially true given the previously mentioned contraction in the number of mammography providers locally and nationally. Queues in appointments may force even previously adherent women to get off schedule if they do not book appointments months in advance.
This study has several limitations. Our analyses are based on cross-sectional data. Establishing a causal chain requires longitudinal or experimental data, as would determining reverse causality.55 Our data did not permit us to examine the association of implementation intentions with actual mammography use. These analyses will be conducted in the future when data are available. Also, because of time constraints for telephone interviews, we assessed only two key elements of implementation intentions. We did not include several other implementation intentions identified by Rutter et al.21 (e.g., arranging for time off from work or for transportation), nor did we ask when women planned to have their next mammograms. These additional implementation intentions could be important as women approach their mammography appointments. Further examination of specific implementation intentions is warranted. The tradeoff between our focus of gaining a deeper perspective on a very specific group of women is our inability to generalize beyond this group. The degree to which our results would have been similar had we studied a different screening interval, such as biennial mammography, or different screening behavior with a different interval, such as colonoscopy or cervical cancer screening, is unclear. We also found ceiling effects for most of our predictors. There may be greater variability in these variables if measured for other screening behaviors, such as colon cancer screening, or in other samples.
Our sample overwhelmingly comprised women who were white and had insurance, limiting generalizability of findings to uninsured women56 or to minority women. These factors also may have contributed to the lack of variability and ceiling effects in predictors, which may have, in turn, affected our ability to detect differences. As we described elsewhere,57 we obtained slightly different nonresponse by race. Our findings may not be generalizable to some populations. Finally, we excluded women who already had made appointments for their next mammograms.
Conclusions
These data contribute to the literature in several ways. The TPB-informed model enabled us to examine traditional correlates of behavioral intentions as predictors of two key implementation intentions for maintaining adherence to mammography. Stronger perceived control predicted having thought about where women would get their next mammograms. Previous mammography maintenance and previous barriers predicted this variable, as well as having thought about making an appointment. Future research should examine these constructs in the context of maintaining mammography use over time. As recent U.S. data suggest, just because women have been getting mammograms does not mean they will continue to do so. Understanding how to initiate and maintain optimal health behaviors is a critical challenge in improving women's health.
Footnotes
This study and manuscript preparation were supported by grants 5R01 CA105786 and 2R25 CA57726 from the National Cancer Institute.
Acknowledgments
We thank Jessica DeFrank, Sonali Garg, Jeanine Matuszewski, Jennifer Gierisch, and Deborah Usinger for their assistance with this manuscript. Most importantly, we thank the women who participated in this study.
Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control Prevention. Use of mammograms among women aged >40 years—United States, 2000–2005. MMWR. 2007;56:49. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 3.Clark MA. Rakowski W. Bonacore LB. Repeat mammography: Prevalence estimates and considerations for assessment. Ann Behav Med. 2003;26:201. doi: 10.1207/S15324796ABM2603_05. [DOI] [PubMed] [Google Scholar]
- 4.Henderson L. Schenck A. Identifying and characterizing one-time and never users of mammography screening services among Medicare eligible women. Prev Med. 2001;32:529. doi: 10.1006/pmed.2001.0846. [DOI] [PubMed] [Google Scholar]
- 5.Meissner H. Breen N. Taubman M, et al. Which women aren't getting mammograms and why? (United States) Cancer Causes Control. 2007;18:61. doi: 10.1007/s10552-006-0078-7. [DOI] [PubMed] [Google Scholar]
- 6.Rakowski W. Meissner H. Vernon SW, et al. Correlates of repeat and recent mammography for women ages 45 to 75 in the 2002 to 2003 Health Information National Trends Survey (HINTS 2003) Cancer Epidemiol Biomarkers Prev. 2006;15:2093. doi: 10.1158/1055-9965.EPI-06-0301. [DOI] [PubMed] [Google Scholar]
- 7.Russell KM. Champion V. Skinner CL. Psychosocial factors related to repeat mammography screening over 5 years in African American women. Cancer Nurs. 2006;29:236. doi: 10.1097/00002820-200605000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Smith R. Saslow D. Sawyer K, et al. American Cancer Society guidelines for breast cancer screening: Update 2003. CA Cancer J Clin. 2003;53:141. doi: 10.3322/canjclin.53.3.141. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Preventive Services Task Force. Screening for breast cancer: Recommendations and rationale. Rockville, MD: Agency for Healthcare Research and Quality; 2002. [Jul 17;2007 ]. [Google Scholar]
- 10.American College of Obstetricians Gynecologists (ACOG) ACOG practice bulletin. Clincial management guidelines for obstetrician-gynecologists. Breast cancer screening. Obstet Gynecol. 2003;101:821. doi: 10.1016/s0029-7844(03)00253-9. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Speaking of health: Assessing health communication strategies for diverse populations. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 12.Fishbein M. Hennessy M. Kamb M, et al. Using intervention theory to model factors influencing behavior change: Project Respect. Eval Health Prof. 2001;24:363. doi: 10.1177/01632780122034966. [DOI] [PubMed] [Google Scholar]
- 13.Brewer NT. Hallman WK. Subjective and objective risk as predictors of influenza vaccination during the vaccine shortage of 2004–2005. Clin Infect Dis. 2006;43:1379. doi: 10.1086/508466. [DOI] [PubMed] [Google Scholar]
- 14.DiBonaventura MD. Chapman GB. Moderators of the intention-behaviour relationship in influenza vaccinations: Intention stability and unforeseen barriers. Psychol Health. 2005;20:761. [Google Scholar]
- 15.Ajzen I. Brown TC. Carvajal F. Explaining the discrepancy between intentions and actions: The case of hypothetical bias in contingent valuation. Pers Soc Psychol Bull. 2004;30:1108. doi: 10.1177/0146167204264079. [DOI] [PubMed] [Google Scholar]
- 16.Sheeran P. Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. Br J Soc Psychol. 1998;37:231. doi: 10.1111/j.2044-8309.1998.tb01167.x. [DOI] [PubMed] [Google Scholar]
- 17.Sheeran P. Intention-behaviour relations: A conceptual and empirical review. Eur Rev Soc Psychol. 2002;12:1. [Google Scholar]
- 18.Rakowski W. Dube CE. Marcus BH, et al. Assessing elements of women's decisions about mammography. Health Psychol. 1992;11:111. doi: 10.1037//0278-6133.11.2.111. [DOI] [PubMed] [Google Scholar]
- 19.Gollwitzer PM. Sheeran P. Implementation intentions and goal achievement: A meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:249. [Google Scholar]
- 20.Gollwitzer PM. Goal achievement: The role of intentions. Eur Rev Soc Psychol. 1993;4:141. [Google Scholar]
- 21.Rutter DR. Steadman L. Quine L. An implementation intentions intervention to increase uptake of mammography. Ann Behav Med. 2006;32:127. doi: 10.1207/s15324796abm3202_10. [DOI] [PubMed] [Google Scholar]
- 22.Sheeran P. Orbell S. Using implementation intentions to increase attendance for cervical cancer screening. Health Psychol. 2000;19:283. doi: 10.1037//0278-6133.19.3.283. [DOI] [PubMed] [Google Scholar]
- 23.Orbell S. Hodgkins S. Sheeran P. Implementation intentions and the Theory of Planned Behavior. Pers Soc Psychol Bull. 1997;23:945. doi: 10.1177/0146167297239004. [DOI] [PubMed] [Google Scholar]
- 24.Bish A. Ramirez A. Burgess C, et al. Understanding why women delay in seeking help for breast cancer symptoms. J Psychosom Res. 2005;58:321. doi: 10.1016/j.jpsychores.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Sheeran P. Webb TL. Gollwitzer PM. The interplay between goal intentions and implementation intentions. Pers Soc Psychol Bull. 2005;31:87. doi: 10.1177/0146167204271308. [DOI] [PubMed] [Google Scholar]
- 26.Mayne L. Earp J. Initial and repeat mammography screening: Different behaviors/different predictors. J Rural Health. 2003;19:63. doi: 10.1111/j.1748-0361.2003.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 27.Drossaert CH. Boer H. Seydel ER. Monitoring women's experiences during three rounds of breast cancer screening: Results from a longitudinal study. J Med Screen. 2002;9:168. doi: 10.1136/jms.9.4.168. [DOI] [PubMed] [Google Scholar]
- 28.Tolma EL. Reininger BM. Evans A, et al. Examining the Theory of Planned Behavior and the construct of self-efficacy to predict mammography intention. Health Educ Behav. 2006;33:233. doi: 10.1177/1090198105277393. [DOI] [PubMed] [Google Scholar]
- 29.Montaño DE. Kasprzyk D. The Theory of Reasoned Action and Theory of Planned Behavior. In: Glanz K, editor; Rimer BK, editor; Lewis FM, editor. Health behavior and health education: Theory, research and practice. San Francisco: Jossey-Bass; 2002. p. 67. [Google Scholar]
- 30.Rutter DR. Attendance and reattendance of breast cancer screening: A prospective three-year test of the Theory of Planned Behaviour. Br J Health Psychol. 2000;5:1–13. [Google Scholar]
- 31.Armitage CJ. Conner M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. Br J Soc Psychol. 2007;40:471. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 32.Sheppard BH. Hartwick J. Warshaw PR. The Theory of Reasoned Action: A meta-analysis of past research with recommendations for modifications and future research. J Consum Res. 1988;15:325. [Google Scholar]
- 33.Sheeran P. Orbell S. Implementation intentions and repeated behaviour: Augmenting the predictive validity of the Theory of Planned Behaviour. Eur J Soc Psychol. 1999;29:349. [Google Scholar]
- 34.Weinstein ND. The precaution adoption process. Health Psychol. 1988;7:355. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein ND. Sandman PM. The precaution adoption process model and its application. In: DiClemente RJ, editor; Crosby RA, editor; Kegler MC, editor. Emerging theories in health promotion practice and research. San Francisco: Jossey-Bass; 2002. p. 16. [Google Scholar]
- 36.Blalock SJ. DeVellis RF. Giorgino KB, et al. Osteoporosis prevention in premenopausal women: Using a stage model approach to examine the predictors of behavior. Health Psychol. 1996;15:84. doi: 10.1037//0278-6133.15.2.84. [DOI] [PubMed] [Google Scholar]
- 37.Blalock SJ. Predictors of calcium intake patterns: A longitudinal analysis. Health Psychol. 1996;26:251. doi: 10.1037/0278-6133.26.3.251. [DOI] [PubMed] [Google Scholar]
- 38.The American Association for Public Opinion Research. Standard definitions: Final dispositions of case codes and outcome rates for surveys. 4th. Lenexa, KS: AAPOR; 2006. [Google Scholar]
- 39.Curtin R. Presser S. Singer E. Changes in telephone survey nonresponse over the past quarter century. Public Opin Q. 2005;69:87. [Google Scholar]
- 40.Rimer BK. Halabi S. Skinner CS, et al. Effects of a mammography decision-making intervention at 12 and 24 months. Am J Prev Med. 2002;22:247. doi: 10.1016/s0749-3797(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 41.Otero-Sabogal R. Stewart S. Shema SJ, et al. Ethnic differences in decisional balance and stages of mammography adoption. Health Educ Behav. 2007;34:278. doi: 10.1177/1090198105277854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ajzen I. The Theory of Planned Behavior. Org Behav Human Decis. 1991;50:179. [Google Scholar]
- 43.Rakowski W. Andersen MR. Stoddard AM, et al. Confirmatory analysis of opinions regarding the pros and cons of mammography. Health Psychol. 1997;16:433. doi: 10.1037//0278-6133.16.5.433. [DOI] [PubMed] [Google Scholar]
- 44.Champion VL. Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. J Womens Health. 2003;12:277. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- 45.Rimer BK. Keintz MK. Kessler HB, et al. Why women resist screening mammography: Patient-related barriers. Radiology. 1989;172:243. doi: 10.1148/radiology.172.1.2740510. [DOI] [PubMed] [Google Scholar]
- 46.Dholakia UM. Bagozzi RP. Mustering motivation to enact decisions: How decision process characteristics influence goal realization. J Behav Dec Making. 2002;15:167. [Google Scholar]
- 47.Steadman L. Rutter DR. Field S. Individually elicited versus modal normative beliefs in predicting attendance at breast screening: Examining the role of belief salience in the Theory of Planned Behavior. Br J Health Psychol. 2002;7:317. doi: 10.1348/135910702760213706. [DOI] [PubMed] [Google Scholar]
- 48.Breen N. Cronin KA. Meissnes HI, et al. Reported drop in mammography: Is this cause for concern? Cancer. 2007;109:2405. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 49.Committee on New Approaches to Early Detection and Diagnosis of Breast Cancer, Institute of Medicine, and National Research Council. Saving women's lives. In: Joy JE, editor; Penhoet EE, editor; Petitti DB, editor. Strategies for improving breast cancer detection and diagnosis. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 50.D'Orsi CJ. Mammography: Will adequate manpower exist? Radiol Clin North Am. 2004;42:975. doi: 10.1016/j.rcl.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 51.D'Orsi CJ. Tu SP. Nakano C, et al. Current realities of delivering mammography services in the community: Do challenges with staffing and scheduling exist? Radiology. 2005;235:391. doi: 10.1148/radiol.2352040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gollwitzer PM. Implementation intentions: Strong effects of simple plans. American Psychologist. 1999;54:493. [Google Scholar]
- 53.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 54.Cameron LD, editor; Leventhal H, editor. The self-regulation of health and illness behavior. New York: Routledge; 2003. [Google Scholar]
- 55.Weinstein ND. Misleading tests of health behavior theories. Ann Behav Med. 2007;33:1. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]
- 56.Carrasquillo O. Pati S. The role of health insurance on Pap smear and mammography utilization by immigrants living in the United States. Prev Med. 2004;39:943. doi: 10.1016/j.ypmed.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 57.DeFrank JT. Bowling JM. Rimer BK. Gierisch JM. Skinner CS. Triangulating differential nonresponse by race in a telephone survey. Prev Chronic Dis [serial online] 2007 July. www.cdc.gov/pcd/issues/2007/jul/06_0102.htm. [Jul 20;2007 ]. www.cdc.gov/pcd/issues/2007/jul/06_0102.htm [PMC free article] [PubMed]