Abstract
Objective:
The influence that social network members exert on the drinking behaviors of alcohol-dependent individuals may represent a behavioral change process that is sensitive to co-occurring cognitive impairment and operates outside treatment to promote or impede outcomes. This study was aimed at extending earlier research support for this hypothesis by assessing impairment in memory as well as executive functions in a more heterogeneous population with alcohol- and/or drug-use disorders.
Method:
Latent class analysis was used as a person-centered approach to characterize the nature and extent of social support for abstinence from alcohol and drug use in 122 men and women entering treatment for substance-use disorders. Substance use, executive dysfunction, and memory impairments were compared across latent classes at four points during the first year after treatment entry. The interrelationship of impairment and social support on treatment outcomes was also examined.
Results:
Three independent social support classes—(1) Frequent Positive Support, (2) Limited Positive Support, and (3) Negative Support—were identified. The Frequent Positive Support class demonstrated the most frequent substance useand greatest executive impairment at treatment entry but—by the end of treatment—showed pronounced improvements in both. In addition, less recovery of executive function by the end of treatment predicted better 12-month substance-use outcomes in the Frequent Positive Support class, whereas it predicted poorer outcomes in the Negative Support class.
Conclusions:
The results offer further evidence for the heightened importance of informal social network processes in the treatment outcomes of persons with severe and ongoing deficits in executive functioning.
There is a growing interest in identifying mechanisms that can promote and sustain behavioral changes in individuals receiving treatment for alcohol- and other drug-use disorders. The cognitive and behavioral targets of various treatment approaches, such as broadening the client's repertoire of coping skills and enhancing confi dence to resist urges to use drugs, have been conceptualized as potential mechanisms of change (e.g., Witkiewitz and Marlatt, 2004). However, individuals with co-occurring cognitive impairment and substance-use disorders often demonstrate decreased treatment compliance (Aharonovich et al., 2003; Donovan et al., 2001; Fals-Stewart and Schafer, 1992), diminished improvements in self-effi cacy during treatment, and a dissociation between change processes initiated during treatment and drinking outcomes (Bates et al., 2006; Morgenstern and Bates, 1999). Thus, one complexity in understanding the impact of treatment-focused mechanisms of change is the heterogeneity in salient personal and clinical features, such as cognitive impairment, that may variously affect the capacity for behavioral change in individual clients.
The finding that well-established treatment process factors are not strong predictors of improved ability to regulate drinking behaviors in cognitively impaired clients would seem to decrease the likelihood of positive alcoholism treatment outcomes in this population. An apparent paradox, however, is that cognitively impaired individuals nonetheless often achieve abstinence or reduced levels of drinking at a rate similar to unimpaired individuals (e.g., Donovan et al., 2001; Knight and Longmore, 1994). This suggests that there are multiple paths to behavioral regulation and that the action of potential mechanisms targeted in treatment milieus needs to be considered within defined personal and environmental contexts.
Parallels have been drawn between brain-injured patients and clients dually affected with substance-use disorders and clinically signifi cant cognitive deficits (Adams et al., 1980; Giancola and Moss, 1998; Levin et al., 1993). In the former population, environmental and contextual variables have been reported to take on increased salience in determining the behavioral, psychosocial, emotional, and vocational outcomes of individuals recovering from a traumatic brain injury (Kaplan, 1990; Prigatano et al., 1996; Tomberg et al., 2005; Webb et al., 1995; Winkler et al., 2006; Ylvisaker et al., 2003). This observation may be of particular importance for individuals with substance-use disorders and cognitive impairment. Clients in treatment for substance-use disorders are known to be positively influenced by abstinence-supporting social influences (Knight and Simpson, 1996; Manuel et al., 2007; Richter et al., 1991; Siddall and Conway, 1988; Zywiak et al., 2002) and negatively influenced by maintaining relationships with drinking-supporting individuals (e.g., see, Marlatt, 1985; McCrady, 2004); and the influence of agents in the social environment can become amplified in treatment clients with diminished cognitive capacity. This amplified influence would then represent an alternative change process operating outside the context of treatment but serving to promote or impede sustained behavioral changes needed for recovery.
This hypothesis was tested using latent class analysis (LCA) to identify the nature of unobserved, naturally occurring social support networks in two Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) samples at treatment entry (Buckman et al., 2007). This person-centered approach to characterizing the operation of helping and hindering agents in the clients' social network identified three independent latent classes. Clients with a high probability of membership in two of the classes had substantial social network support for abstinence yet differed in the amount of day-to-day contact they had with informal helping agents. Clients with a high probability of membership in the third class had substantial support for drinking by significant others in their social network and moderate contact with informal “hindering” agents. These three latent classes were invariant across the two Project MATCH samples of inpatients and aftercare clients who varied in alcohol-use problem severity and other clinical characteristics, suggesting that these unobserved social network classes may generalize to the social milieu of clients with substance-use disorders in other treatment samples. The present study examined the hypothesis that these three social support classes would be captured in a more heterogeneous sample of clients receiving treatment for an alcohol-use disorder, drug-use disorder, or dual alcohol- and drug-use disorders.
Buckman et al. (2007) further found that the stability of drinking over the first year after treatment, as well as the average level of cognitive impairment at treatment entry, differed across the social support classes. Clients with a high probability of social networks that supported drinking were drinking more heavily, stably, and/or problematically over the year following treatment, and they were unable to maintain a moderate or unproblematic drinking status, compared with clients with a high probability of frequent contact with an abstinence-supporting network. In addition, although clients were classified based on the characteristics of their social network, having a high probability of frequent contact with an abstinence-supporting social network was related to more clinically significant cognitive impairment at treatment entry. These findings suggested that the availability and use of abstinence-supporting social networks outside the treatment domain may be one way in which cognitively impaired individuals with an alcohol-use disorder can reinforce (or substitute for) more cognitively demanding change processes being promoted during treatment, thereby enhancing the likelihood of a positive treatment outcome. Indeed, moderation analyses revealed that cognitive impairment strengthened the relationship between social support and drinking outcomes. That is, impaired outpatients with social networks that supported abstinence demonstrated better drinking outcomes, whereas high severity aftercare clients with cognitive impairments and support for drinking demonstrated poorer drinking outcomes.
The present study used data from an independent sample with the goal of replicating the observation of heterogeneous classes of social support that differ in their drinking behaviors and cognitive abilities (Buckman et al., 2007) in individuals seeking treatment for alcohol- and/or drug-use disorders. Accordingly, it was predicted that individuals who entered treatment with social networks that support abstinence would exhibit positive substance-use outcomes (i.e., fewer days of drinking/drug using), compared with those having social networks that support substance use. Cognitive impairment at treatment entry was expected to be more evident in individuals with a high probability of having a social network that supported treatment goals when they entered treatment. In addition, this study extended the approach used in Buckman et al. (2007) by examining not only impairment at treatment entry but also changes in cognitive impairment across the first year after treatment entry. Furthermore, a more comprehensive neuropsychological battery was used to distinguish between cognitive impairment in the executive functioning and memory domains. The previous study did not include memory assessments, leaving unanswered questions about the relationship of this important domain of alcohol- and drug-related cognitive impairment to social support and outcome. Individuals in frequent contact with an abstinence-supporting network were expected to demonstrate greater improvements in cognitive function over the first year following treatment entry, compared withthose individuals with more limited support for abstinence. This is based on the expectation that they would engage in less substance use during the year following treatment and that abstinence would be associated with neurocognitive recovery (e.g., Bartsch et al., 2007; Pfefferbaum et al., 1995). Finally, moderation analyses were performed to examine the prediction of an enhanced relationship between social support and substance-use outcomes in the context of cognitive impairment.
Method
Participants
Demographic and substance-use characteristics of this study sample have been previously described in detail (Morgenstern and Bates, 1999). Social support data were collected from male (n = 72) and female (n = 50) volunteers who were recruited from two private, hospital-based chemical dependency treatment programs offering residential or intensive day treatment. Both program approaches were based on the traditional “Minnesota Model.” Program features of each of these treatment facilities have been previously described (Morgenstern et al., 1996, 1997). On average (SD), participants were 33.6 (9.4) years of age with 13.0 (2.6) years of education. All participants met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994) criteria for a current psychoactive substance-use disorder (45% alcohol, 27% drug, and 28% dual alcohol and drug diagnoses). Exclusion criteria included a history of organic brain dysfunction, Korsakoff's syndrome, severe dementia, psychotic disorder, serious medical problems that precluded testing, methadone maintenance treatment, inability to read test materials, and age less than 18 years. At the 6-month follow-up, 82.8% (n = 101) of the clients participated; at the 1-year assessment, 75% (n = 92) of the clients participated.
Measures
Neuropsychological tests.
Cognitive functioning of participants was assessed at intake as well as at 6-week, 6-month, and 12-month follow-ups using a battery of psychometrically sound neuropsychological tests. These tests were selected based on their sensitivity to the types and range of executive functioning and memory deficits often noted in individuals with substance-use disorders (Bates and Convit, 1999; Bates et al., 2005; Knight and Longmore, 1994; Nixon, 1995) and their standardization and time efficiency that facilitates use in applied and clinical settings (Lezak, 1995; Spreen and Strauss, 1998).
Executive functioning was measured with the Shipley Institute of Living Scale, Verbal Abstraction test (number correct; Zachary, 1986), word fluency (FAS) test (number correct; Benton and Hamsher, 1976), a brief version of the Booklet Category (CAT) test (number of errors; Russell and Levy, 1987), Stroop color and word test (number correct; Golden, 1978), Wisconsin Card Sorting Test (number of perseveration errors; Nelson, 1976), Trail Making Test Part B (time in seconds; Reitan and Wolfson, 1985), Tower of Hanoi-4 block (time in seconds; Simon, 1975), and the Digit Symbol Substitution Test (number correct in 90 seconds; Kaplan et al., 1991). Memory was measured with the California Verbal Learning Test, short delay test (number correctly recalled; Delis et al., 1987); Product Recall Test (number correctly recalled; Sussman, 1996); and the Digit Symbol Substitution Test (number correctly recalled and the incidental learning task). Classifi cations of these tests as executive or memory tests are in line with data from the field; however, there is some overlap in the cognitive domains they measure (Bates et al., 2002, 2005).
Serious cognitive impairment was defined using the method described in Morgenstern and Bates (1999) based on available age-stratified normative data or clinical impairment cut-off scores (Spreen and Strauss, 1998; Zachary, 1986). Overall executive functioning and memory impairment scores were calculated by summing the number of tests (0-8, 0-4, respectively) on which performance was impaired.
Social support variables.
The Important People and Activities (IPA) inventory (Clifford and Longabaugh, 1991) was used to characterize social support at intake. Clients listed up to 12 individuals in their social network during the past 6 months and reported the type (e.g., family, friend) and length of relationship; frequency of interaction; members' drinking and drug-using habits; how well liked and important the client considered each; and the 4 most important people's attitudes toward the patient's substance use, abstinence, and treatment. Eight binary variables from Buckman et al. (2007) were derived from the raw Important People and Activities data for the LCA. For each of the eight respective variables, a code of “1” was given if (1) at least one network member was abstinent or a light substance user, supported the client's abstinence, and interacted three or more times per week with the client; (2) at least one network member was a heavy substance user, supported the client's substance use, and interacted three or more times per week with the client; (3) all members of the network supported abstinence; (4) all members of the network encouraged drinking/drug use; (5) two or more nonusers were within the social network; (6) three or more heavy substance users were within the network; (7) daily contact was maintained with at least four network members; or (8) daily contact was maintained with at least half of the members in the social network. The two contact measures differed in that one measure (7) assessed whether a client had multiple alternative sources of support, whereas the other measure (8) took into account network size and assessed a client's likelihood of using available support. One variable—“three or more frequent drinkers were within the network”—that was included in the Buckman et al. (2007) LCA was not available in the present data.
Substance-use variable.
The percentage of days during which a client used either alcohol or other drugs for the 6 months before treatment entry, as well as during the days between follow-ups, was calculated using a modified version of the Timeline Followback interview (Sobell and Sobell, 1992). The number of “use” days was divided by the overall number of “valid” days (excluding days they were hospitalized or incarcerated). On average, clients reported on 176 valid days before treatment, 29 days during treatment, 176 days between the 6-week and 6-month follow-ups, and 169 days between the 6-month and 12-month follow-ups.
Procedure
Participants provided informed consent and were individually tested at treatment entry (1-week window following detoxification, when necessary) and retested at 6 weeks, 6 months, and 12 months after treatment entry with the neuropsychological battery and Timeline Followback interview. Neuropsychological evaluations were performed using highly standardized procedures by the same cadre of extensively trained testers, whose test administration skills were reevaluated every 6 months to prevent drift. Zero blood alcoholconcentration was confirmed by breath analysis before testing. All testing was conducted in compliance with National Institutes of Health guidelines for the ethical treatment of human subjects and approved by the Rutgers Institutional Review Board for the Protection of Human Subjects in Research.
Data analysis
LCA was used to capture the integrated behaviors of an individual's social network by classifying unobserved heterogeneity in constellations of support variables at the level of the person. Unlike variable-centered approaches (e.g., regression or factor analysis) that independently model social support variables across all members of the client's social network, LCA characterizes the interdependent action of multiple social support features from a single network member.
LCA identifies the fewest number of mutually exclusive, homogeneous classes of persons based on the pattern of individual characteristics (McCutcheon, 1987). Characteristic profiles of each unobserved class, statistically independent patterns of endorsement probabilities that are stable among all members, and the probabilities of a given individual endorsing a given variable and of belonging to a specific latent class (based on the similarity of an individual's support profile to the class profile) were generated using MPlus (Muthén and Muthén, 1998-2004). Latent class models were fi tted to eight binary indices of social support using a maximum likelihood approach with missing data assumed to be missing at random (Little and Rubin, 1987). An initial model with one social support class was specified, classes were added in a stepwise fashion, and the goodness of fit of model solutions was compared. Changes in the Bayesian Information Criteria(BIC)—in addition to entropy, class sizes, and interpretability of classes—were used to establish the best-fitting and most stable model (Muthén and Muthén, 1998-2004). Gender was added to the model to improve classification accuracy. The substance-use outcomes and cognitive impairment levels of each latent class were compared in a pairwise fashion. The modest size of the present sample precluded the use of chi-square tests of model invariance, which are commonly used to test for statistical differences between classes but are highly sensitive to sample size. Effect size measurements (calculated as Cohen's d, the mean differences between two latent classes, divided by the standard deviation) were used to gauge differences between classes. Differences of 0.2-0.5 were considered small, 0.5-0.8 were considered medium, and 0.8 or greater were considered large; effect sizes below 0.2 were considered nonsignificant (Cohen, 1988).
Regression analyses were performed within the MPlus mixture model framework to replicate previous moderation analyses assessing whether neuropsychological impairment altered the relationship between social support class membership probability and drinking outcome (Buckman et al., 2007). The percentage of days in which the participants used drugs or alcohol between the 6-week and 12-month follow-ups was regressed on treatment entry and 6-week follow-up executive and memory impairment scores within each class. Baseline use was included in all models, and the variances of all variables were aligned on the same scale to minimize parameter estimate bias. A statistically signifi cant regression coefficient within one or more, but not all, social support classes provided evidence for moderation.
Results
The mean network size was 8.1 (3.0), with an average level of contact of several times per week (5.5 [0.9], range: 1-7). As observed in the Project MATCH samples (Buckman et al., 2007), the majority of clients (79.5%) reported having one or more abstinent/light substance-using network member who supported the client's abstinence and had frequent contact with the client, whereas relatively fewer (21.3%) endorsed having one or more heavy substance-using network member who supported the client's substance use and had frequent contact with the client. Mean executive impairment scores for the overall sample were 1.8 (1.7) at treatment entry and 1.2 (1.4), 1.1 (1.4), and 1.0 (1.3) at the 6-, 26-, and 52-week follow-ups, respectively (range: 0-7 impaired tests). Mean memory impairment scores for the overall sample were 1.5 (1.3) at treatment entry and 1.0 (1.1), 0.8 (1.1), and 0.9 (1.0) at the 6-, 26-, and 52-week follow-ups, respectively (range: 0-4 impaired tests).
Latent classes of social support at treatment entry
Fit statistics were compared between models that contained 1-5 classes (Table 1), and a three-class solution was determined to be optimal based on changes in BIC, improvements in model fit, and the ability of the three-class solution to identify well-differentiated classes and capture theoretically meaningful structures of social support. The three classes generally paralleled those previously observed in two Project MATCH samples (Buckman et al., 2007). In agreement with the earlier study, the classes were identified as the (1) Frequent Positive Support class (including clients with a high likelihood of support for abstinence and frequent contact with network members), (2) Limited Positive Support class (including clients with a high likelihood of support for abstinence but limited contact with network members), and (3) Negative Support class (including clients with a high likelihood of support for substance use and some contact with network members). Classification accuracies were at least 0.93 before adding demographic variables and greater than 0.96 after adding gender as a covariate. Significantly more individuals with a high likelihood of Negative Support class membership were male (69%), compared with those with Limited Positive Support class membership (32%); 56% of those with a high probability of Frequent Positive Support class membership were male.
Table 1.
Latent class analysis fit statistics
| Models | Free parameters | BIC | Difference in BIC between models | Entropy | Estimated group sizesa |
| 1 class | 8 | 1,074.48 | – | 1.00 | 100 |
| 2 class | 17 | 1,048.52 | -25.96 | 0.94 | 11, 89 |
| 3 class | 26 | 1,054.03 | 5.51 | 0.97 | 11, 21, 68 |
| 4 class | 35 | 1,075.12 | 21.09 | 0.96 | 9, 11, 14, 66 |
| 5 class | 44 | 1,105.94 | 30.82 | 0.97 | 6, 9, 9, 18, 58 |
Notes: Bold = optimal model. BIC = Bayesian Information Criteria.
Group sizes are presented as percentage of total sample.
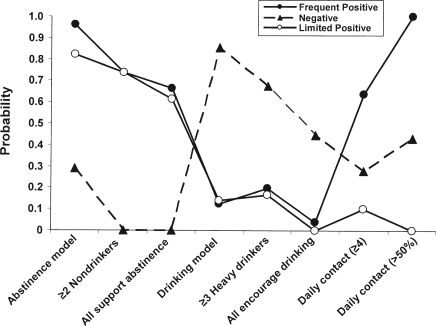
Figure 1 shows the probabilities of network support variable endorsement for each class (i.e., the probability that an individual in a given class will exhibit a given network support feature). The Frequent and Limited Positive Support classes differed only in their endorsement of the two contact variables. Conversely, the Negative Support class was considerably different, endorsing substantially lower probabilities of having an abstinence model (29%), a network completely supportive of their abstinence (0%), and two or more nonusers in their network (0%), as well as higher probabilities of having a substance-using model (85%), a network completely supportive of their substance use (45%), and three or more heavy users (67%) in their social network.
Figure 1.
The latent class analysis probability of a given individual endorsing each of eight binary variables derived from the Important Persons and Activities inventory. Three unique (statistically independent) classes of social support endorsement probabilities were identified: two with support for abstinence that differed in the amount of contact the client had with network members (Frequent Positive and Limited Positive) and one with support for drinking (Negative).
Cognitive impairment and substance-use outcomes in the latent social support classes
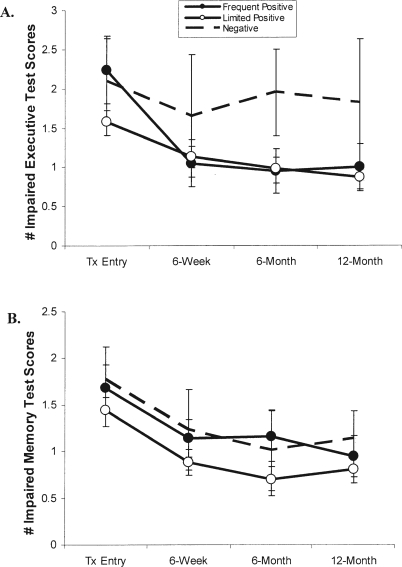
Differences in cognitive impairment across classes were assessed using effect size calculations (Cohen's d). At treatment entry, a high probability of membership in the Limited Positive Support class was related to less impairment on tests of executive functioning compared with Frequent Positive Support or Negative Support class membership (d = 0.39 and 0.30, respectively; Figure 2, panel A). By the 6-week follow-up, a high likelihood of both Frequent Positive Support and Limited Positive Support class memberships was associated with fewer impaired executive test scores as compared with the Negative Support class (d = 0.44 and 0.39, respectively). This pattern of improved executive functioning performance in the two Positive Support class members, compared with the Negative Support class, was even more dramatic at the 6-month and 12-month follow-ups. At these points, medium effect size differences were noted between the Frequent Positive Support and Negative Support classes (d = 0.76 and 0.65, respectively) and between the Limited Positive Support and Negative Support classes (d = 0.73 and 0.75, respectively).
Figure 2.
Mean impairment index scores (±SEs) for (A) executive functioning and (B) memory at all four times. Tx = treatment.
In terms of performance on tests of memory, a high probability of Negative Support class membership was associated with greater impairment, compared with the Limited Positive Support class at all four points (d = 0.26, 0.32, 0.28, and 0.33, respectively; Figure 2, panel B). In addition, clients with a high probability of Frequent Positive Support class membership demonstrated poorer memory performance compared with those with Limited Positive Support class membership. But small effect size differences were noted only at the 6-week and 6-month follow-ups and were otherwise nonsignifi cant (d = 0.19, 0.24, 0.42, and 0.14, respectively).
Substance-use outcomes were calculated as the percentage of days during which a client used drugs or alcohol. At treatment entry, those with a high likelihood of Frequent Positive Support (d = 0.29) and Negative Support (d = 0.38) class membership reported a greater percentage of days on which they used alcohol or other drugs, compared with those with Limited Positive Support class membership (Table 2). At all three posttreatment follow-ups, however, a high probability of Negative Support class membership was related to more frequent substance use, compared with the Frequent Positive Support (d = 0.27, 0.30, and 0.25) and Limited Positive Support (d = 0.33, 0.37, and 0.19) classes, whereas the Positive Support classes did not differ from each other.
Table 2.
Percentage of days using alcohol or drugs in each latent class across the first-year after treatment
| Assessment point | Frequent Positive (n = 27) | Limited Positive (n = 82) | Negative (n = 13) |
| Treatment entry | 69.73a | 61.21 | 72.59a |
| 6-week follow-up | 5.41 | 4.24 | 10.57a,b |
| 26-week follow-up | 11.17 | 9.62 | 18.33a,b |
| 52-week follow-up | 12.56 | 14.09 | 19.76b |
Small effect size vs Limited Positive;
small effect size vs Frequent Positive.
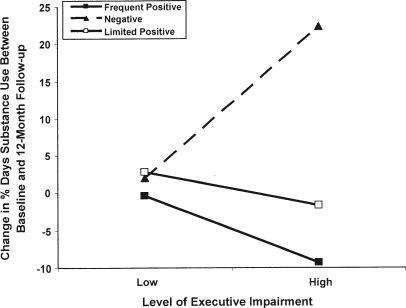
Moderation analyses were performed to replicate and extend the observation that cognitive impairment can influence the relationship between social support available at treatment entry and later substance use (Buckman et al., 2007). In the current study, the influence of impairment in executive functioning and memory on the relationship between social support and the percentage of days of substance use between the end of treatment and the end of the first year was tested. Neither executive nor memory impairment scores at treatment entry predicted frequency of substance use during the first year following treatment in any of the latent classes. However, executive impairment at the end of treatment predicted frequency of substance use in the Frequent Positive Support and Negative Support classes but not in the Limited Positive Support class (impairment at baseline was included in the model as a covariate). The unstandardized regression coefficients were -1.12 (p < .01) for the Frequent Positive Support class, 2.54 (p < .01) for the Negative Support class, and -0.57 (p = NS) for the Limited Positive Support class (Figure 3). These results suggest that, controlling for level of impairment at treatment entry, more severe executive function impairment at the end of treatment (i.e., less recovery of function) predicted (1) better substance-use outcomes across 12 months in clients with a high probability of frequent contact with an abstinence-supporting network and (2) poorer substance-use outcomes across 12 months in clients with a high probability of a substance use-supporting network.
Figure 3.
Moderation of the relationship of social support and changes in substance use by level of executive impairment. In the Negative Support class, more severe executive dysfunction at the end of treatment (controlling for baseline impairment) predicted poorer substance-use outcomes (increase in percentage of days of use) across the first 12 months after treatment entry. Conversely, in the Frequent Positive Support class, more severe executive function impairment at the end of treatment (controlling for baseline impairment) predicted better substance-use outcomes (decrease in percentage of days of use) across 12 months.
Discussion
Cognitively impaired clients seem to benefit less from mechanisms of change that are targeted by treatment approaches compared with unimpaired clients (Aharonovich et al., 2003; Bates et al., 2006; Donovan et al., 2001; Fals-Stewart and Schafer, 1992; Morgenstern and Bates, 1999), thus pointing to the need to identify factors that operate outside the context of treatment that may also support an impaired client's goal of abstinence. This study was designed to replicate and extend a prior study of clients with an alcohol-use disorder that suggested that support received from an individual's social network influences drinking outcomes and that the presence of cognitive impairment can heighten that influence (Buckman et al., 2007). In large part, the present results replicated these observations in a sample of individuals with an alcohol- and/or drug-use disorder and offer further evidence for the importance of an abstinence-supporting social network to reduce substance use, particularly in those persons with executive function impairment.
As previously found, three independent social support classes were identified at treatment entry, two that supported abstinence (with frequent and limited contact) and one that supported substance use. In the present sample, however, unlike both samples of Project MATCH, the Negative Support class lacked the presence of at least one strong abstinence role model with whom the client had consistent contact. In fact, in this mixed substance-use disorders sample, only 29% of the Negative Support class reported having an abstinence role model. The illicit nature of drug use may result in a social network being more deeply entrenched in similar substance-using behaviors. This may present an additional hurdle for treatment providers and warrants further examination.
In agreement with Buckman et al. (2007), individuals with a high probability of having a social network that supported substance use reported the most frequent use of alcohol and/or drugs. This is also in general agreement with Beattie and Longabaugh (1999), Longabaugh et al. (1993, 2001), and Mohr et al. (2001). Although at treatment entry, individuals with strong, frequent support for abstinence reported a substance-use frequency similar to individuals with support for substance use, at each follow-up, those with a high likelihood of Negative Support reported nearly twice the frequency of substance-using days as the two Positive Support classes. In other words, by the end of treatment, the Frequent Positive Support class members demonstrated a pronounced decrease in the frequency of substance use that was not observed in the Negative Support class. This findingis of particular interest in light of the relatively higher levels of cognitive impairment observed in both of these latent classes.
Previously, individuals with a high probability of Frequent Positive Support class membership were reported to demonstrate the most profound impairment at treatment entry (Buckman et al., 2007). Impairment in this earlier study was determined using data from four tests of executive functioning and one test of verbal ability. The present study extended this finding by identifying that impairment in the executive functioning domain versus the memory domain was most relevant to social network influence on substance use and thatexecutive impairment at treatment entry was greatest in the Frequent Positive Support class. In addition to distinguishing between executive and memory dysfunction, the present study also examined cognitive recovery at four points in time across the first year after treatment entry. Mean impairment levels in the executive functioning domain decreased in both Positive Support classes across the first year after treatment entry, particularly between treatment entry and the 6-week follow-up in the Frequent Positive Support class. This may suggest that frequent contact with an abstinence-supporting network serves to promote cognitive recovery early in treatment and that even moderate contact with a substance use-supporting network can delay or stunt recovery of cognitive performance across time. Although the mechanism underlying this relationship is not addressed by the present data, the abstinence versus substance-using behaviors reinforced by the different social network classes may well have provided more or fewer opportunities for neural recovery.
Results of the moderation analyses also were in general agreement with those from the Project MATCH samples (Buckman et al., 2007) in suggesting that different social support environments affect substance-using behaviors differently, depending on the presence or absence of serious neuropsychological impairment. The specifics of how this relationship plays out in samples of varying severity and substance-use disorders, however, remain to be clarifi ed. For example, in the Project MATCH study, more severe cognitive impairment at treatment entry (in the verbal and executive domains) predicted better substance-use outcomes in out-patients in the Frequent Positive Support class and poorer substance-use outcomes in aftercare clients (more severe alcohol-use histories) in the Negative Support class. In the current sample of clients with mixed alcohol- and drug-use disorders, both of these patterns of results were obtained but only in relation to the level of executive impairment at the end of treatment (controlling for initial degree of impairment), rather than the level of impairment observed at treatment entry. This may suggest that the degree of cognitive recovery that occurs during the earliest stages of recovery (i.e., during treatment) importantly modifi es the relationship between social support and substance-use outcomes. Because cognitive impairment at the end of treatment was not assessed in Project MATCH, further study of cognitive impairment and its recovery over time in treatment populations that vary in the nature and severity of substance-use disorders is needed.
Clients in the Frequent Positive Support class who demonstrated more impairment in executive functioning at the end of treatment reported a lower percentage of days of alcohol/drug use across the first year after treatment than less impaired clients with similar social network characteristics. For these clients with a social network that supported abstinence and provided consistent and stable contact, the lack of executive functioning recovery seemed to act in a protective fashion, thus resulting in the apparently counterintuitive finding that more impairment in this latent social support class led to better substance-use outcomes. For unimpaired or more mildly impaired persons (or those who tended to recover the most during treatment) in this latent class, the availability of an abstinence-supporting social network exerted a much less sustained positive influence on substance-using behaviors. Conversely, clients in the Negative Support class who demonstrated more impairments in executive functioning at the end of treatment reported a greater percentage of alcohol-/drug-using days across the first year after treatment, compared with less impaired clients with substance use-supporting social networks. Thus, maintained impairment (or failure to recover) led to worse substance-use outcomes.
These observations support the idea that cognitively impaired individuals tend to draw more heavily on external resources, such as social network members, who may implicitly guide their substance-use behaviors or possibly their decision-making processes. When surrounded by an abstinence-supporting social network, the impaired client seems to engage in behaviors consistent with the maintenance of an abstinent lifestyle; when surrounded by a substance-using social network, the impaired client tends to engage in behaviors related to continued substance use. In general, therefore, the present results suggest that, as with the Project MATCH samples (Buckman et al., 2007), cognitive dysfunction seems to magnify the influence of individuals' social network on their drinking outcomes following treatment. In addition, executive impairment may be of specific importance because memory impairments appeared to be independent of substance-use outcomes in the different support classes.
The present findings must be considered in relation to limitations of moderate sample size and attrition at follow-up. Although the use of effect-size measurements supports the validity of the findings and suggests that a larger sample would not have yielded substantively different main effect results, the moderation analyses can only be considered exploratory because of their limited power. The modest sample size did not allow exploration of gender as a potential moderator. In the present sample, diagnoses related to cocaine, opiate, marijuana, sedative, hallucinogen, and stimulant use were combined into a single “drug-use disorder” category. It is possible, however, that different drugs have differential impacts on cognitive ability and recovery (Carlin and O'Malley, 1996), particularly considering their specific and often unique neurobiological targets (Rogers and Robbins, 2001). Finally, abstinence from drugs was assessed through self-report and collateral reports only; validation of these reports with urinalysis and drug screening would be advantageous in future research. Nonetheless, the present study offers further support for the importance of social support in recovery from a substance-use disorder, particularly in individuals who demonstrate severe and ongoing executive dysfunction. It suggests that, although the ability to acquire and use potentially cognitively demanding treatment strategies may be diminished, cognitively impaired individuals with substance-use disorders may be more influenced by their informal social environment outside of treatment. This implies that impaired individuals may supplement treatment-related processes with a social network comprised of helping agents who encourage and support the goal of abstinence. Unfortunately, this also implies that social networks comprising substance users who encourage use can further diminish the impaired individuals' chances at sustained recovery.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants P50 AA08747, R01 AA11594, and K02 AA00325. Preliminary results of this study were presented at the 115th Annual Meeting of the American Psychological Association, San Francisco, CA, August 2007.
References
- Adams JH, Graham DI, Scott G, Parker LS, Doyle D. Brain damage in fatal non-missile head injury. J. Clin. Pathol. 1980;33:1132–1145. doi: 10.1136/jcp.33.12.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aharonovich E, Nunes E, Hasin D. Cognitive impairment, retention and abstinence among cocaine abusers in cognitive-behavioral treatment. Drug Alcohol Depend. 2003;71:207–211. doi: 10.1016/s0376-8716(03)00092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Bartsch AJ, Homola G, Biller A, Smith SM, Weijers HG, Wiesbeck GA, Jenkinson M, De Stefano N, Solymosi L, Bendszus M. Manifestations of early brain recovery associated with abstinence from alcoholism. Brain. 2007;130(Pt 1):36–47. doi: 10.1093/brain/awl303. [DOI] [PubMed] [Google Scholar]
- Bates ME, Convit A. Neuropsychology and neuroimaging of alcohol and illicit drug abuse. In: Calev A, editor. Assessment of Neuropsycho-logical Functions in Psychiatric Disorders. Washington, DC: American Psychiatric Press; 1999. pp. 373–445. [Google Scholar]
- Bates ME, Labouvie EW, Voelbel GT. Individual differences in latent neuropsychological abilities at addictions treatment entry. Psychol. Addict. Behav. 2002;16:35–46. doi: 10.1037//0893-164x.16.1.35. [DOI] [PubMed] [Google Scholar]
- Bates ME, Pawlak AP, Tonigan JS, Buckman JF. Cognitive impairment influences drinking outcome by altering therapeutic mechanisms of change. Psychol. Addict. Behav. 2006;20:241–253. doi: 10.1037/0893-164X.20.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates ME, Voelbel GT, Buckman JF, Labouvie EW, Barry D. Short-term neuropsychological recovery in clients with substance use disorders. Alcsm Clin. Exp. Res. 2005;29:367–377. doi: 10.1097/01.alc.0000156131.88125.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie MC, Longabaugh R. General and alcohol-specific social support following treatment. Addict. Behav. 1999;24:593–606. doi: 10.1016/s0306-4603(98)00120-8. [DOI] [PubMed] [Google Scholar]
- Benton A, Hamsher KDes. Multilingual Aphasia Examination. Iowa City, IA: University of Iowa; 1976. [Google Scholar]
- Buckman JF, Bates ME, Cisler RA. Social networks and their influence on drinking behaviors: Differences related to cognitive impairment in clients receiving alcohol treatment. J. Stud. Alcohol Drugs. 2007;68:738–747. doi: 10.15288/jsad.2007.68.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlin AS, O'Malley S. Neuropsychological consequences of drug abuse. In: Grant I, Adams KM, editors. Neuropsychological Assessment of Neuropsychiatric Disorders. 2nd Edition. New York: Oxford Univ. Press; 1996. pp. 486–503. [Google Scholar]
- Clifford PR, Longabaugh R. Adapted for use by Project MATCH, Providence, RI: Center for Alcohol and Addiction Studies. Brown University; 1991. Manual for the Administration of the Important People and Activities Instrument. [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. Mahwah, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Delis D, Kramer JH, Kaplan E, Ober B. California Verbal Learning Test: Adult Version Manual. San Antonio, TX: The Psychological Corporation; 1987. [Google Scholar]
- Donovan DM, Kivlahan DR, Kadden RM, Hill D. Longabaugh R, Wirtz PW, editors. Cognitive impairment as a client-treatment matching hypothesis. Washington: Government Printing Office; Project MATCH Hypotheses: Results and Causal Chain Analyses. NIAAA Project MATCH Monograph Series, Vol. 8, NIH Publication No. 01-4238. 2001:62–81.
- Fals-Stewart W, Schafer J. The relationship between length of stay in drug-free therapeutic communities and neurocognitive functioning. J. Clin. Psychol. 1992;48:539–543. doi: 10.1002/1097-4679(199207)48:4<539::aid-jclp2270480416>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Moss HB. Executive cognitive functioning in alcohol use disorders. In: Galanter M, editor. Recent Developments in Alcoholism. Vol. 14. The Consequences of Alcoholism; 1998. pp. 227–251. [DOI] [PubMed] [Google Scholar]
- Golden, C.J. Stroop Color and Word Test. A Manual for Clinical and Experimental Uses. Wood Dale, IL: Stoelting Co; 1978. [Google Scholar]
- Kaplan SP. Social support, emotional distress, and vocational outcomes among persons with brain injuries. Rehab. Counsel. Bull. 1990;34:16–23. [Google Scholar]
- Kaplan E, Fein D, Morris R, Delis DC. The WAIS-R as a Neuropsychological Instrument. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- Knight DK, Simpson DD. Influences of family and friends on client progress during drug abuse treatment. J. Subst. Abuse. 1996;8:417–429. doi: 10.1016/s0899-3289(96)90003-6. [DOI] [PubMed] [Google Scholar]
- Knight RG, Longmore BE. Clinical Neuropsychology of Alcoholism. Mahwah, NJ: Lawrence Erlbaum; 1994. [Google Scholar]
- Levin HS, Culhane KA, Mendelsohn D, Lilly MA, Bruce D, Fletcher JM, Chapman SB, Harward H, Eisenberg HM. Cognition in relation to magnetic resonance imaging in head-injured children and adolescents. Arch. Neurol. 1993;50:897–905. doi: 10.1001/archneur.1993.00540090008004. [DOI] [PubMed] [Google Scholar]
- Lezak MD. Neuropsychological Assessment. 3rd Edition. New York: Oxford Univ. Press; 1995. [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: John Wiley & Sons; 1987. [Google Scholar]
- Longabaugh R, Beattie M, Noel N, Stout R, Malloy P. The effect of social investment on treatment outcome. J. Stud. Alcohol. 1993;54:465–478. doi: 10.15288/jsa.1993.54.465. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A. Stout R. Longabaugh R, Wirtz PW, editors. Network support for drinking. Washington: Government Printing Office; Project MATCH hypotheses: Results and Causal Chain Analyses. Project MATCH Monograph Series, Vol. 8, NIH Publication No. 01-4238. 2001:260–275.
- McCrady BS. To have but one true friend: Implications for practice of research on alcohol use disorders and social network. Psychol. Addict. Behav. 2004;18:113–121. doi: 10.1037/0893-164X.18.2.113. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent Class Analysis. Thousand Oaks, CA: SAGE; 1987. [Google Scholar]
- Manuel JK, McCrady BS, Epstein EE, Cook S, Tonigan JS. The pretreatment social networks of women with alcohol dependence. J. Stud. Alcohol Drugs. 2007;68:871–878. doi: 10.15288/jsad.2007.68.871. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. Cognitive factors in the relapse process. In: Marlatt GA, Gordon JR, editors. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford Press; 1985. pp. 128–200. [Google Scholar]
- Mohr CD, Averna S, Kenny DA, Del Boca FK. “Getting by (or getting high) with a little help from my friends”: An examination of adult alcoholics' friendships. J. Stud. Alcohol. 2001;62:637–645. doi: 10.15288/jsa.2001.62.637. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Bates ME. Effects of executive function impairment on change processes and substance use outcomes in 12-step treatment. J. Stud. Alcohol. 1999;60:846–855. doi: 10.15288/jsa.1999.60.846. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Frey RM, McCrady BS, Labouvie E, Neighbors CJ. Examining mediators of change in traditional chemical dependency treatment. J. Stud. Alcohol. 1996;57:53–64. doi: 10.15288/jsa.1996.57.53. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: A study of its therapeutic effects and mechanisms of action. J. Cons. Clin. Psychol. 1997;65:768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus: The Comprehensive Modeling Program for Applied Researchers: User's Guide, Version 3. Los Angeles, CA: Muthén & Muthén; 1998-2004. [Google Scholar]
- Nelson HE. A modified card sorting test sensitive to frontal lobe defects. Cortex. 1976;12:313–324. doi: 10.1016/s0010-9452(76)80035-4. [DOI] [PubMed] [Google Scholar]
- Nixon SJ. Assessing cognitive impairment. Alcohol Hlth Res. World. 1995;19:97–103. [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Mathalon DH, Shear PK, Rosenbloom MJ, Lim KO. Longitudinal changes in magnetic resonance imaging brain volumes in abstinent and relapsed alcoholics. Alcsm Clin. Exp. Res. 1995;19:1177–1191. doi: 10.1111/j.1530-0277.1995.tb01598.x. [DOI] [PubMed] [Google Scholar]
- Prigatano GP, Glisky EL, Konoff PS. Corrigan PW, Yudofsky SC, editors. Cognitive rehabilitation after traumatic brain injury. Washington, DC: American Psychiatric Press; Cognitive Rehabilitation for Neuropsychiatric Disorders. 1996:223–242.
- Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Battery: Theory and Clinical Implications. Tucson, AZ: Neuropsychology Press; 1985. [Google Scholar]
- Richter SS, Brown SA, Mott MA. The impact of social support and self-esteem on adolescent substance abuse treatment outcome. J. Subst. Abuse. 1991;3:371–385. doi: 10.1016/s0899-3289(10)80019-7. [DOI] [PubMed] [Google Scholar]
- Rogers RD, Robbins TW. Investigating the neurocognitive deficits associated with chronic drug misuse. Curr. Opin. Neurobiol. 2001;11:250–257. doi: 10.1016/s0959-4388(00)00204-x. [DOI] [PubMed] [Google Scholar]
- Russell EW, Levy M. Revision of the Halstead Category Test. J. Cons. Clin. Psychol. 1987;55:898–901. doi: 10.1037//0022-006x.55.6.898. [DOI] [PubMed] [Google Scholar]
- Siddall JW, Conway GL. Interactional variables associated with retention and success in residential drug treatment. Int. J. Addict. 1988;23:1241–1254. doi: 10.3109/10826088809058855. [DOI] [PubMed] [Google Scholar]
- Simon HA. The functional equivalence of problem solving skills. Cog. Psychol. 1975;7:268–288. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Spreen O, Strauss E. A Compendium of Neuropsychological Tests: Administration, Norms and Commentary. 2nd Edition. New York: Oxford Univ. Press; 1998. [Google Scholar]
- Sussman S. Development of a school-based drug abuse prevention curriculum for high-risk youths. J. Psychoact. Drugs. 1996;28:169–182. doi: 10.1080/02791072.1996.10524389. [DOI] [PubMed] [Google Scholar]
- Tomberg T, Toomela A, Pulver A, Tikk A. Coping strategies, social support, life orientation and health-related quality of life following traumatic brain injury. Brain Injury. 2005;19:1181–1190. doi: 10.1080/02699050500150153. [DOI] [PubMed] [Google Scholar]
- Webb CR, Wrigley M, Yoels W, Fine PR. Explaining quality of life for persons with traumatic brain injuries 2 years after injury. Arch. Phys. Med. Rehab. 1995;76:1113–1119. doi: 10.1016/s0003-9993(95)80118-9. [DOI] [PubMed] [Google Scholar]
- Winkler D, Unsworth C, Sloan S. Factors that lead to successful community integration following severe traumatic brain injury. J. Head Trauma Rehab. 2006;21:8–21. doi: 10.1097/00001199-200601000-00002. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. Amer. Psychol. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Ylvisaker M, Jacobs HE, Feeney T. Positive supports for people who experience behavioral and cognitive disability after brain injury: Areview. J. Head Trauma Rehab. 2003;18:7–32. doi: 10.1097/00001199-200301000-00005. [DOI] [PubMed] [Google Scholar]
- Zachary RA. Los Angeles, CA: Western Psychological Services; Shipley Institute of Living Scale: Revised Manual. 1986
- Zywiak WH, Longabaugh R, Wirtz PW. Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. J. Stud. Alcohol. 2002;63:114–121. [PubMed] [Google Scholar]