Abstract
Introduction
The cost of genetic testing and the limited knowledge about the BRCA1 and BRCA2 genes in different ethnic groups has limited its availability in medium- and low-resource countries, including Malaysia. In addition, the applicability of many risk-assessment tools, such as the Manchester Scoring System and BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) which were developed based on mutation rates observed primarily in Caucasian populations using data from multiplex families, and in populations where the rate of breast cancer is higher, has not been widely tested in Asia or in Asians living elsewhere. Here, we report the results of genetic testing for mutations in the BRCA1 or BRCA2 genes in a series of families with breast cancer in the multi-ethnic population (Malay, Chinese and Indian) of Malaysia.
Method
A total of 187 breast cancer patients with either early-onset breast cancer (at age ≤ 40 years) or a personal and/or family history of breast or ovarian cancer were comprehensively tested by full sequencing of both BRCA1 and BRCA2. Two algorithms to predict the presence of mutations, the Manchester Scoring System and BOADICEA, were evaluated.
Results
Twenty-seven deleterious mutations were detected (14 in BRCA1 and 13 in BRCA2), only one of which was found in two unrelated individuals (BRCA2 490 delCT). In addition, 47 variants of uncertain clinical significance were identified (16 in BRCA1 and 31 in BRCA2). Notably, many mutations are novel (13 of the 30 BRCA1 mutations and 24 of the 44 BRCA2). We report that while there were an equal proportion of BRCA1 and BRCA2 mutations in the Chinese population in our study, there were significantly more BRCA2 mutations among the Malays. In addition, we show that the predictive power of the BOADICEA risk-prediction model and the Manchester Scoring System was significantly better for BRCA1 than BRCA2, but that the overall sensitivity, specificity and positive-predictive value was lower in this population than has been previously reported in Caucasian populations.
Conclusion
Our study underscores the need for larger collaborative studies among non-Caucasian populations to validate the role of genetic testing and the use of risk-prediction models in ensuring that the other populations in the world may also benefit from the genomics and genetics era.
Introduction
The discovery of the BRCA1 and BRCA2 genes has transformed the management of women who are at high risk of developing breast and ovarian cancer. Diagnostically, it has facilitated the accurate identification of women at risk of cancer; through screening and preventive measures, it has reduced the incidence of cancer in such women [1], and perhaps most importantly, exploitation of the knowledge that these genes function in DNA repair has opened up avenues for the development of new treatments for women with hereditary tumours [2].
Although predictive genetic testing is increasingly becoming a part of clinical practice in many developed countries, the cost of testing and the limited knowledge about the prevalence of these genes in different ethnic groups has limited its availability in medium- and low-resource countries [3,4]. There is relatively little information about the BRCA1 and BRCA2 mutations in Asia and among Asians living elsewhere and, to date, no significant founder-effect mutation has been reported [5,6]. Notably, although 60% of the world's population reside in the Asian continent, and the Malays, Chinese and Indians are three major Asian ethnic groups, relatively little is known about the genetic predisposition to hereditary diseases and the applicability of genetic testing in these diverse ethnic groups [7-16].
Malaysia is a multi-ethnic country with a population of approximately 23 million, comprising approximately 65% Malays and other indigenous groups, approximately 26% Chinese and approximately 8% Indian (Malaysia Housing and Population Census 2000, Department of Statistics Malaysia). The Chinese and Indians are largely first- or second-generation migrants from southern China and southern India, while the Malays and other minority indigenous groups are native to South-East Asian countries including Malaysia and Indonesia. In Malaysia, which may be described as a typical Asian country, breast cancer is characterised by: a lower age-standardised rate (30 per 100,000 [17]); a proportionately higher incidence of early-onset breast cancer (47% of new cases occurred in women <50 years [17]); and an incomplete family history or structure because of a lack of information about second degree and further relatives, premature mortality and significant dispersal of families. Taken together, studies in this typical Asian multi-ethnic population provide an excellent opportunity to understand genetic predisposition among the different ethnic groups and among the different risk categories.
Furthermore, in order to ensure that medicine based in genetics can also be equitably implemented in low- and medium-resource countries, it is critically important that there are cost-effective mutation screening programmes. Currently, there is little information about the effectiveness of these risk-assessment tools in other ethnic populations, particularly in countries with low age-standardised rate of breast cancer, which also reflects the setting in many low- and medium-resource countries.
Using a unique, ethnically diverse cohort of high-risk families, we sought to: examine the significance of founder/recurrent and novel rare BRCA1 and BRCA2 mutations to familial breast and ovarian cancer in the Malays, Chinese and Indian populations of Malaysia; and compare the accuracy of the Manchester Scoring System and the BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) risk-prediction models to predict pathogenic mutations and particularly to discriminate at the 10% likelihood level. Taken together, we wished to devise the most relevant definition of individuals or families who would benefit from mutation testing in this typical Asian country with a lower incidence of breast cancer.
Materials and methods
Breast cancer cohort
The recruitment of Malaysian families with a high risk of breast or ovarian cancer started in 2003 at the University Malaya Medical Centre in Kuala Lumpur. Patients with breast cancer were first approached by clinicians responsible for their care to see if they would participate in a research study to determine the genetic factors which increase the risk of breast cancer in Malaysia. Thereafter, individuals interested in the project were approached by a member of the research team who explained to them the nature and objectives of the research project. A total of 678 index cases were referred to our study between January 2003 and December 2007. Index cases signed a consent form and a blood sample was taken. A family history was recorded and the pedigree analysed. Where possible, pathology reports were requested to confirm all diagnoses of breast and ovarian cancers in the index case.
The study was approved by the ethics committee of University Malaya Medical Centre.
Inclusion criteria for analysis of BRCA1 and BRCA2
All breast cancer patients in the cohort had: early-onset breast cancer (≤ 40 years) and 1 or more additional cases of breast cancer in first- or second-degree relatives; breast cancer (≥ 40 years) and two or more additional cases of breast cancer in first- or second-degree relatives; bilateral breast cancer; or a personal or family history of ovarian cancer. They were analysed for mutations in the BRCA1 and BRCA2 genes. In addition, approximately 50% of patients with only early-onset breast cancer (≥ 40 years) with no significant family history or breast cancer (≤ 40 years) and one additional case of breast cancer in a first- or second-degree relative were also analysed. Individuals were categorised based on self-reported race or ethnicity. Of the 678 index cases, 187 were analysed for mutations in the BRCA1 and BRCA2 genes (Table 1).
Table 1.
Family characteristics
| Total (n = 187) | Malay (n = 44) | Chinese (n = 118) | Indian (n = 22) | Others (n = 3) | |
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| Age of onset of breast cancer in index case (years) | |||||
| 20 to 29 | 14 (7) | 3 (7) | 10 (8) | 1 (5) | 0 (0) |
| 30 to 39 | 64 (34) | 21 (48) | 36 (31) | 6 (27) | 1 (33) |
| 40 to 49 | 49 (26) | 8 (18) | 35 (30) | 5 (23) | 1 (33) |
| ≥ 50 | 60 (32) | 12 (27) | 37 (31) | 10 (45) | 1 (33) |
| Personal cancer history of breast, or breast and ovarian cancer | |||||
| Breast only | 182 (97) | 43 (98) | 117 (99) | 19 (86) | 3 (100) |
| Both breast and/or ovarian | 5 (3) | 1 (2) | 1 (1) | 3 (14) | 0 (0) |
| Bilateral breast cancer | 25 (13) | 6 (14) | 15 (13) | 4 (18) | 0 (0) |
| Family history of breast and ovarian cancer in pedigree | |||||
| 1 case (no family history) | a73 (39) | 24 (54) | 40 (34) | 8 (36) | 1 (33) |
| 2 cases | 76 (41) | 13 (30) | 54 (46) | 9 (41) | 1 (33) |
| 3 cases | 24 (13) | 4 (9) | 17 (14) | 2 (9) | 0 (0) |
| ≥ 4 cases | 14 (7) | 3 (7) | 7 (6) | 3 (14) | 1 (33) |
A total of 187 breast cancer patients were analysed for mutations in BRCA1 and BRCA2 by DNA sequencing and multiple ligation dependent probe amplification (MLPA) analysis. Table 1 shows the distribution of patients according to their self-declared ethnicity, personal history of breast and ovarian cancer, and family history of breast and ovarian cancer in first- and second-degree relatives. aNotably, the 73 individuals with no family history of breast and ovarian cancer were included in the study because they had either early age of onset of breast cancer (≤ 40 years of age: 45 individuals; 41 to 55 years of age: nine individuals), bilateral breast cancer (16 individuals), both breast and ovarian cancer (one individual) or family history of prostate cancer in the third degree (three individuals).
Mutation detection
Blood from index cases was separated into two 10 ml EDTA-tubes and DNA was extracted using standard methods. Samples were analysed either at Genetic Technologies Laboratory (Australia) or at Cancer Research Initiatives Foundation (Malaysia) using direct DNA sequencing and multiple ligation dependent probe amplification (MLPA), as previously described [18]. Confirmation tests were performed on a second blood sample. Naming and interpretation of sequence analysis were performed as previously described and all patients were classified as having a deleterious mutation if the BRCA1 or BRCA2 protein terminated prematurely at least 10 or 110 amino acids, respectively, from the C terminus. Genetic variants of undetermined clinical significance (unclassified variants) included missense mutations and mutations that occurred in analysed intronic regions whose clinical significance had not yet been determined. If more than one variant was observed in a single analysis, the overall interpretation was that of the most clinically significant mutation observed.
BOADICEA
The BOADICEA model allows for a polygenic modifier locus effect in which several low-penetrance genes have joint effects [19]. Family history information (including incidence of breast, ovarian and other cancers, age at diagnosis and relationship to the proband) was collected and recorded by a genetic counsellor or researcher. Breast cancer patients were included in the BOADICEA analysis if they had more than one primary cancer or if they had a family history of breast, ovarian, pancreatic and/or prostate cancer in first-, second- or third-degree relatives. Of the 187 individuals who were analysed for mutations in BRCA1 and BRCA2, we excluded 42 individuals (including three individuals with deleterious BRCA2 mutations), all of whom had a single case of breast cancer and no family history of breast, ovarian, pancreatic or prostate cancer in first-, second- or third-degree relatives. The predicted likelihood of carrying either a BRCA1 or BRCA2 mutation was generated for each individual using BOADICEA risk estimation on the internet (BOADICEA WEB APPLICATION v1.0).
Manchester Scoring System
We used the Manchester Scoring System to estimate the probability of identifying mutations in BRCA1 and BRCA2 genes [20,21]. In brief, the scoring system was developed using a combination of results from screening and family history of those with and without mutations, where a combined score of 15 or more was proposed to correlate with a 10% mutation probability. The exclusion criteria for BOADICEA analysis was also applied to the Manchester Scoring System.
Results
Mutation testing outcome
A total of 1226 patients with breast cancer were treated at the University Malaya Medical Centre between January 2003 and December 2007, of which 678 individuals with breast cancer from 674 families were recruited to the present study. Despite rigorous efforts to identify women with a family history of breast cancer, only 159 women were found to exhibit a family history in a first- or second-degree relative (129 with one additional affected member, 19 with two additional affected members and 11 with three or more additional affected members).
We conducted full sequence analysis of the BRCA1 and BRCA2 genes in 187 women (Table 1). Of these: 73 had no significant family history of breast or ovarian cancer in first- or second-degree relatives (45 of whom developed breast cancer ≤ 40 years old, nine of whom developed breast cancer between 41 and 55 years old; one had both breast and ovarian cancer, 16 had bilateral breast cancer and two had a family history of prostate cancer); and 114 had two or more cases of breast or ovarian cancer in first- or second-degree relatives.
Mutation detection led to the discovery of 27 deleterious mutations in 28 breast cancer patients (14 in BRCA1 and 13 in BRCA2; Table 2). Notably, 14 of these mutations were novel (five in BRCA1 and eight in BRCA2) and one mutation in BRCA2 was found in two unrelated families. In addition, we identified 47 sequence variants of unknown clinical significance (16 in BRCA1 and 31 in BRCA2), of which eight were found to occur in more than one unrelated family (Table 3). Of these, 26 sequence variants were novel (nine in BRCA1 and 17 in BRCA2). Eleven sequence variants (two in BRCA1 and nine in BRCA2) may be potentially damaging based on sequence conservation and Grantham score, and five sequence variants are unlikely to be clinically relevant.
Table 2.
Deleterious mutations including frame-shift, nonsense and splice site deleterious mutations identified in Malaysian breast cancer patients
| No. | Exon | Nucleotide change | AA change | Reported | Family (No.) | Ethnicity | |
| 1 | BRCA1 | 2 | 180 delA | STOP 22 | Novel | 1 | Indian |
| 2 | 2 | 185 delAG | STOP 39 | Ashkenazi Jews, others | 1 | Indian | |
| 3 | 2 | 185 insA | STOP 40 | Caucasian, European | 1 | Chinese | |
| 4 | 8 | 589 delCT | STOP 157 | Caucasian, Caribbean | 1 | Chinese | |
| 5 | 11 | 1100 delAT | STOP 328 | Caucasian, Chinese [10,16] | 1 | Chinese | |
| 6 | 11 | 1173 G>T | E352X | Caucasian | 1 | Indian | |
| 7 | 11 | 1323 G>T | E402X | Novel | 1 | Malay | |
| 8 | 11 | 3889 delAG | STOP1265 | Various | 1 | Chinese | |
| 9 | 13 | 4377 C>T | Q1420X | Caucasian, African-American | 1 | Chinese | |
| 10 | 20 | 5370 C>T | R1751X | Various | 1 | Indian | |
| 11 | IVS 3+1 G>T | Novel | 1 | Chinese | |||
| 12 | IVS 3+2 delT | Novel | 1 | Chinese | |||
| 13 | IVS 4-1G>C | Novel | 1 | Indian | |||
| 14 | IVS 5-12 A>G | Various | 1 | Chinese | |||
| 1 | BRCA2 | 3 | 490 delCT | STOP 99 | Novel | 2 | Malay |
| 2 | 10 | 1184 insA | STOP 326 | Caucasian | 1 | Chinese | |
| 3 | 10 | 2001 del4 | STOP 612 | Caucasian | 1 | Chinese | |
| 4 | 11 | 2699 del6 | STOP 824 | Novel | 1 | Malay | |
| 5 | 11 | 2864 delCT | STOP 879 | Novel | 1 | Chinese | |
| 6 | 11 | 4265 delCT | STOP 1350 | Filipino | 1 | Malay | |
| 7 | 11 | 6195 insA | STOP 2002 | Novel | 1 | Malay | |
| 8 | 11 | 6553 delGT | STOP 2109 | Novel | 1 | Chinese | |
| 9 | 11 | 6901 delA | STOP 2228 | Novel | 1 | Chinese | |
| 10 | 11 | 6943 G>T | E2239X | Novel | 1 | Chinese | |
| 11 | 22 | 9097 C>T | Q2957X | Novel | 1 | Indian | |
| 12 | 23 | 9326 insA | STOP 3042 | Various | 1 | Chinese | |
| 13 | IVS 17+1 G>A | Caucasian | 1 | Chinese | |||
Table 3.
Missense and intervening sequence variants identified
| No. | Exon | Nucleotide change | AA change | Reported | Family (No.) | Mutation classification | Ethnicity | |
| BRCA1 | 1 | 7 | 491 C>A | I124I | Novel | 1 | Benign? | Malay |
| 2 | 9 | 690 G>A | V191I | Various | 2 | Benign? | Chinese | |
| 3 | 11 | 873 C>T | R252C | Novel | 1 | Deleterious? | Malay | |
| 4 | 11 | 914 T>C | S265S | Novel | 1 | Benign? | Chinese | |
| 5 | 11 | 1155 C>T | P346S | Asian | 2 | Benign? | Chinese | |
| 6 | 11 | 2405 A>T | R762S | Chinese [8] | 1 | Benign? | Malay | |
| 7 | 11 | 2685 T>C | Y856H | Chinese | 6 | Benign? | Chinese | |
| 8 | 11 | 2845 A>T | N909I | Chinese | 1 | Benign? | Chinese | |
| 9 | 11 | 2858 T>A | N913K | Novel | 1 | Benign? | Chinese | |
| 10 | 11 | 3050 A>G | P977P | Novel | 1 | Benign? | Chinese | |
| 11 | 11 | 3781 A>C | E1221A | Novel | 1 | Benign? | Chinese | |
| 12 | 11 | 3922 A>G | N1268S | Novel | 1 | Benign? | Malay | |
| 13 | 16 | 5011 G>A | S1631N | Novel | 1 | Benign? | Chinese | |
| 14 | 24 | 5623 G>A | R1835Q | Novel | 1 | Benign? | Malay | |
| 15 | IVS 1-10 T>C | Various | 1 | Not clinically relevant [43] | Malay | |||
| 16 | IVS 12-10 G>A | Various | 1 | Deleterious? | Indian | |||
| BRCA2 | 1 | 3 | 443 A>G | N72S | Novel | 1 | Benign? | Chinese |
| 2 | 5 | 668 A>G | Q147R | Asian, various | 2 | Benign? | 1 Malay, 1 Chinese | |
| 3 | 10 | 1171 T>A | C315S | Asian | 2 | Benign? | Chinese | |
| 4 | 10 | 1503 A>G | E425E | Novel | 1 | Benign? | Chinese | |
| 5 | 10 | 1590 A>G | K454K | Novel | 3 | Benign? | Chinese | |
| 6 | 10 | 1828 G>A | E534K | Novel | 1 | Deleterious? | Malay | |
| 7 | 10 | 1872 G>A | Q548Q | Various | 1 | Benign? | Chinese | |
| 8 | 10 | 1875 G>A | K549K | Novel | 1 | Benign? | Chinese | |
| 9 | 10 | 2053 C>G | Q609E | Novel | 1 | Benign? | Malay | |
| 10 | 11 | 2906 A>G | Q893R | Novel | 1 | Benign? | Malay | |
| 11 | 11 | 3648 T>C | S1140S | Chinese [8] | 1 | Benign? | Chinese | |
| 12 | 11 | 3673 A>G | M1149V | Asian, various | 3 | Benign? | 2 Malay, 1 Chinese | |
| 13 | 11 | 3903 A>G | T1225T | Novel | 1 | Benign? | Malay | |
| 14 | 11 | 4010 C>G | S1261C | Novel | 1 | Deleterious? | Malay | |
| 15 | 11 | 4806 A>G | T1526T | Novel | 1 | Benign? | Other | |
| 16 | 11 | 5395 A>C | T1723P | Novel | 1 | Benign? | Malay | |
| 17 | 11 | 5540 G>A | G1771D | Various | 1 | Not clinically relevant [BIC] | Malay | |
| 18 | 11 | 5863 G>A | E1879K | Caucasian | 1 | Benign? | Indian | |
| 19 | 11 | 6013 A>G | I1929V | Asian, various | 1 | Not clinically relevant [BIC] | Chinese | |
| 20 | 11 | 6550 C>T | R2108C | Various | 3 | Benign? | 2 Malay, 1 Chinese | |
| 21 | 12 | 7157 C>A | T2310N | Novel | 1 | Deleterious? | Indian | |
| 22 | 17 | 8169 A>C | L2647L | Novel | 1 | Benign? | Malay | |
| 23 | 18 | 8415 G>T | K2729N | Asian, various | 1 | Not clinically relevant [44] | Chinese | |
| 24 | 19 | 8584 G>A | A2786T | Novel | 1 | Deleterious? | Chinese | |
| 25 | 21 | 8930 G>A | G2901D | Asian | 1 | Deleterious? | Chinese | |
| 26 | 23 | 9332 A>G | Y3035C | Caucasian | 1 | Deleterious? | Chinese | |
| 27 | 23 | 9334 C>G | Q3036E | Novel | 1 | Benign? | Chinese | |
| 28 | 27 | 10135 A>T | S3303C | Novel | 1 | Deleterious? | Other | |
| 29 | 27 | 10462 A>G | I3412V | Various | 1 | Not clinically relevant [45] | Chinese | |
| 30 | IVS 2-7T>A | Caucasian | 1 | Deleterious? | Malay | |||
| 31 | IVS 7-10 insT | Novel | 1 | Deleterious? | Other | |||
Mutation classification was made based on published studies and analysis using PolyPhen. BIC, Breast Cancer Information Core.
Table 4 shows that the majority of mutations in the Indian subgroup were BRCA1 mutations, whereas the majority of the mutations in the Malay subgroup were BRCA2 mutations, and there were an equal number of mutations in both genes among the Chinese subgroup. One possible explanation for the higher incidence of BRCA1 mutations in the Indian subgroup is that there was a high proportion of women with both breast and ovarian cancer in this subgroup compared with the Chinese or Malay subgroups (14% of total, compared with 1 to 2% among the Chinese and Malay; Table 1) and it is clear from other studies that BRCA1 mutations confer a higher penetrance to ovarian cancer [22]. By contrast, the reason for the higher prevalence of BRCA2 mutations among the Malays is unclear.
Table 4.
Incidence of BRCA1 and BRCA2 deleterious mutations, by race/ethnicity
| Ethnicity | Total families | Families with deleterious mutation | Families with unclassified variant | ||
| BRCA1 | BRCA2 | BRCA1 | BRCA2 | ||
| Malay | 44 | 1 | 5 | 6 | 14 |
| Chinese | 118 | 8 | 8 | 15 | 18 |
| Indian | 22 | 5 | 1 | 1 | 2 |
| Others | 3 | 0 | 0 | 0 | 3 |
| Total | 187 | 14 | 14 | 22 | 37 |
Clinical presentation of breast cancer
The mean age of diagnosis of all women analysed was 43.8 years (range 22 to 78 years), and the mean age of diagnosis was 40.3 years for BRCA1-positive (range 28 to 57 years), 43.6 years for BRCA2-positive (range 34 to 59 years) and 44.2 years for BRCA-negative women (range 22 to 78 years) (Table 5 and 6). This is comparable to data from a large study of 10,000 individuals in the USA [6], where individuals with BRCA1 mutations had a significantly younger age at diagnosis (40 years) than those with BRCA2 (41 years).
Table 5.
Family characteristics and pathological characteristics of breast cancers of individuals with deleterious BRCA1 and BRCA2 mutations
| Nucleotide change | AA change | Age of diagnosis of breast cancer | No. of breast/ovarian cancers in family | Mean age diagnosis (Breast cancer) | No. of cases (Breast cancer ≤ 50) | ER | PR | HER2 | Grade | ||
| BRCA1 | 180 delA | STOP 22 | 55 | 2 | 43 | 1 | - | - | - | 2 | IDC |
| 185 delAG | STOP 39 | 33 | 1 | 33 | 1 | - | - | - | 3 | IDC | |
| 185 insA | STOP 40 | 57 | 7 | 44 | 4 | NA | NA | NA | NA | IDC | |
| 589 delCT | STOP 157 | 45 | 3 | 41 | 3 | - | - | - | NA | IDC | |
| 1100 delAT | STOP 328 | 28 | 2 | 28 | 1 | - | - | - | 3 | IDC | |
| 1173 G>T | E352X | 45 | 3 | 45 | 1 | - | - | - | 2 | IDC | |
| 1323 G>T | E402X | 34 | 3 | 31 | 2 | NA | NA | NA | NA | Sarcoma | |
| 3889 delAG | STOP1265 | 47 | 3 | 47 | 2 | - | NA | + | NA | DCIS/IDC | |
| 4377 C>T | Q1420X | 39 | 2 | 45 | 2 | - | - | +/- | 3 | IDC | |
| 5370 C>T | R1751X | 31 | 5 | 38 | 3 | NA | NA | NA | NA | NA | |
| IVS 3+1 G>T | 46 | 2 | 47 | 2 | - | NA | + | NA | IDC | ||
| IVS 3+2 delT | 32 | 2 | 56 | 1 | - | NA | - | 2 | IDC | ||
| IVS 4-1G>C | 39 | 2 | 48 | 1 | NA | NA | NA | NA | IDC | ||
| IVS5-12 A>G | 33 | 1 | 33 | 1 | - | - | - | 3 | IDC | ||
| BRCA2 | 490 delCT | STOP 99 | 39 | 2 | 56 | 1 | - | - | - | 2 | IDC |
| 490 delCT | STOP 99 | 51 | 4 | 45 | 3 | + | + | - | NA | ILC | |
| 1184 insA | STOP 326 | 34 | 1 | 34 | 1 | + | + | - | 2 | IDC | |
| 2001 del4 | STOP 612 | 37 | 1 | 37 | 1 | + | - | + | 3 | IDC | |
| 2699 del6 | STOP 824 | 41 | 2 | 57 | 1 | + | NA | NA | 2 | IDC | |
| 2864 delCT | STOP 879 | 40 | 1 | 40 | 1 | - | NA | NA | 3 | IDC | |
| 4265 delCT | STOP 1350 | 55 | 4 | 44 | 3 | + | + | - | 2 | IDC | |
| 6195 insA | STOP 2002 | 42 | 3 | 46 | 2 | NA | NA | NA | NA | NA | |
| 6553 delGT | STOP 2109 | 59 | 3 | 49 | 1 | + | NA | - | 2 | IDC | |
| 6901 delA | STOP 2228 | 35 | 1 | 35 | 1 | NA | NA | NA | NA | IDC/DCIS | |
| 6943 G>T | E2239X | 47 | 2 | 44 | 2 | NA | NA | NA | NA | NA | |
| 9097 C>T | Q2957X | 38 | 7 | 44 | 2 | NA | NA | NA | NA | NA | |
| 9326 insA | STOP 3042 | 56 | 4 | 49 | 2 | - | - | NA | NA | NA | |
| IVS 17+1 G>A | 36 | 2 | 46 | 1 | - | - | - | 3 | IDC | ||
ER, oestrogen receptor; PR, progesterone receptor; AA, amino acid; DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma.
Table 6.
Summary of family characteristics and pathological characteristics of breast cancers of individuals with deleterious BRCA1 and BRCA2 mutations
| Overall | BRCA1 | BRCA2 | Non-BRCA | |
| Age of onset | 22 to 78 | 28 to 57 | 34 to 59 | 22 to 78 |
| Average age of onset (years) | 41.9 | 40.3 | 43.6 | 44.2 |
| Total no. of breast and ovarian cancers in family | 1 to 7 | 1 to 7 | 1 to 7 | 1 to 6 |
| Average no. of breast and ovarian cancers in family | 1.9 | 2.7 | 2.6 | 1.8 |
| No. of cases of breast cancer <50 | 0 to 4 | 1 to 3 | 1 to 3 | 0 to 4 |
| Average no. of cases of breast cancer <50 | 1.1 | 1.6 | 1.5 | 1.0 |
| % with ER-negative tumours | 48% | 100% | 40% | 45% |
Table 5 shows the pathological characteristics of breast cancer arising in BRCA1 and BRCA2 deleterious mutation carriers. Consistent with other studies [23], the majority of BRCA1 tumours are high grade and negative for the oestrogen, progesterone and HER2 receptors. By contrast, the BRCA2 tumours arise with various status for the oestrogen, progesterone and HER2 receptor.
Prediction of BRCA1/BRCA2 carrier status based on risk factors
Table 7 shows the likelihood of having a BRCA1 or BRCA2 deleterious mutation, based on the personal and family history of the individual. We found that the best predictive factors for the presence of a BRCA1 or BRCA2 mutation are families with at least two cases of breast cancer, at least one of which occuring before the age of 50 (p = 0.0335), and families with a history of both breast and ovarian cancer (p < 0.0001). Notably, of the 15 breast cancer patients with personal or family history of ovarian cancer, six had mutations in BRCA1 and two in BRCA2. In addition, of the 14 BRCA1 carriers and 14 BRCA2 carriers identified in this study, five had bilateral breast cancer (one synchronous and four metachronous). The mean time interval between surgery for the first primary cancer and the second occurrence in the contralateral breast was 9.8 years (range four to 24 years). However, the association between bilaterality and BRCA mutation status was not statistically significant (p = 0.45). Taken together, the data suggests that the presence of two or more breast cancers with at least one case under the age of 50, and ovarian cancer at any age are significant predictors for the presence of a BRCA1 or BRCA2 mutation.
Table 7.
Likelihood of having a BRCA1 or BRCA2 deleterious mutations
| Personal history | Family history | Total | BRCA1 positive | BRCA2 positive | BRCA positive | BRCA positive |
| Number | Number | Number | % | |||
| Breast cancer <50 years | Nil | 61 | 2 | 3 | 5 | 8.2 |
| Breast cancer <50 years | 1 breast cancer <50 years | 29 | 1 | 3 | 4 | 13.8 |
| Breast cancer ≥ 50 years | 1 breast cancer <50 years | 13 | 1 | 0 | 1 | 7.7 |
| Breast cancer at any age | ≥ 2 breast cancer <50 years | 7 | 1 | 0 | 1 | 14.3 |
| Breast cancer at any age | ≥ 3 breast cancer at any age | 9 | 0 | 3 | 3 | 33.3 |
| Breast cancer at any age | ≥ 1 ovarian cancer at any age | 10 | 4 | 1 | 5 | 50.0 |
| Breast and ovarian cancer | Any | 5 | 2 | 1 | 3 | 60.0 |
| Bilateral breast cancer | Any | 25 | 4 | 1 | 5 | 20.0 |
Risk prediction models (BOADICEA) and scoring methods (Manchester Scoring System)
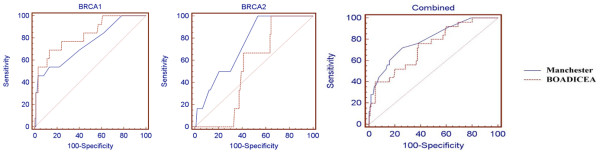
Using receiver operating curves (Figure 1), we evaluated the accuracy of using the Manchester Scoring System empirical method compared with the BOADICEA risk-prediction models to discriminate between those families that have a BRCA mutation and those that do not (Table 8). The classifications based on Manchester Score System and BOADICEA are similar for BRCA1, but significantly different for BRCA2, which BOADICEA did not predict accurately. In terms of discriminating between those with and without a mutation, the areas under the receiver operating curves, a common measure of the adequacy of a quantitative predictive algorithm, are 0.74 (95% confidence interval [CI] = 0.67 to 0.81) and 0.82 (95% CI = 0.75 to 0.88) for BRCA1, and 0.82 (95% CI = 0.75 to 0.88) and 0.56 (95% CI = 0.48 to 0.64) for BRCA2, for Manchester Score System and BOADICEA, respectively (Table 8).
Figure 1.
Receiver Operating Characteristic curves for Manchester Scoring and BOADICEA predictions of the probability of carrying a BRCA1 or BRCA2 mutation.
Table 8.
The sensitivities, specificities, and positive and negative predictive values calculated with a Manchester Scoring System cut-off score of ≥ 10 for each gene and ≥ 15 combined, and for BOADICEA score of ≥ 0.10 for each gene and ≥ 0.10 combined (ie, 10% probability of carrying a deleterious mutation)
| Manchester Scoring System | BOADICEA | |||||
| BRCA1 | BRCA2 | Combined | BRCA1 | BRCA2 | Combined | |
| Area under the receiver operating curves | 0.74 | 0.82 | 0.80 | 0.82 | 0.56 | 0.73 |
| Standard error | 0.078 | 0.079 | 0.06 | 0.070 | 0.093 | 0.061 |
| 95% CI | 0.67 – 0.81 | 0.75 – 0.88 | 0.72 – 0.86 | 0.75 – 0.88 | 0.48 – 0.64 | 0.65 – 0.80 |
| P valuea | 0.0018 | 0.0001 | 0.0001 | 0.0001 | 0.507 | 0.0001 |
| Sensitivity | 57% | 55% | 72% | 57% | 9% | 40% |
| Specificity | 76% | 87% | 74% | 93% | 93% | 85% |
| Positive-predictive value | 20% | 25% | 37% | 47% | 10% | 36% |
| Negative-predictive value | 94% | 96% | 93% | 95% | 93% | 87% |
aP value is the probability that the sample area under the ROC curve is found when in fact, the true area under the ROC curve is 0.5 (i.e. null hypothesis: Area = 0.5).
The probability of identifying a mutation was 66% (96 of 145), 10% (15 of 145), 9.7% (14 of 145), 6.2% (nine of 145) and 7.6% (11 of 145), at ranges of scores 4 to 14, 15 to 16, 17 to 20, 21 to 24 and 25 and above by the Manchester Scoring System. Our analysis also indicated that a cut-off at a combined Manchester score of 15 seems optimal as a threshold (sensitivity of 72%, specificity of 74%, positive-predictive value of 37% and negative-predictive value of 93%). At a combined score of 18, the sensitivity was 56%, specificity was 84%, positive-predictive value was 42% and negative-predictive value was 90%.
For a combined score of 0.10 or above using BOADICEA, we observed sensitivity of 40%, specificity of 85%, positive-predictive value of 36% and negative-predictive value of 87%.
The total number of cases predicted by the Manchester Scoring System was eight BRCA1 mutation carriers, nine BRCA2 mutation carriers and 17 mutation carriers in total (using the probabilities listed [20,21]), and by BOADICEA was nine BRCA1 mutation carriers, five BRCA2 mutation carriers and 14 mutation carriers in total. This was compared with the observed numbers of 14 BRCA1, 11 BRCA2 and 25 total carriers (three BRCA2 carriers were among the 42 individuals excluded in the analysis because they had a single case of breast cancer and did not have any family history of cancer in the family). This suggests that both the Manchester Scoring System and BOADICEA methods underpredicted the probability of having a mutation in BRCA1 or BRCA2 in our cohort.
Discussion
This study provides important data on the prevalence and spectrum of mutations in BRCA1 and BRCA2 in the multi-ethnic population of Malaysia. This key information was then coupled with the family history of cancer and selection criteria to determine the optimal strategy for clinical genetic testing in this population, keeping in mind that this service is not yet available in the national health care system and that it is necessary to target interventions at high-risk individuals who have the most health benefits to gain from available preventive and risk-reduction strategies.
BRCA1 and BRCA2 mutation spectrum and prevalence
Of the 27 deleterious mutations identified, 13 mutations have never been previously reported in any other population. Two groups studying BRCA mutations in Singapore, where the population is also multi-ethnic but in different proportions (Chinese 77%, Malays 14% and Indians 8%), reported seven mutations in BRCA1 that were not observed in our cohort [24-27]. One mutation, c.2845insA in BRCA1, was recently reported to have a founder effect among the Malay population in Singapore [25,28,29], but this was not found in 44 Malays in our study.
We did not identify any mutations that occur with high frequency in Asians. Four mutations that have previously been reported in Asians: BRCA1 589delCT in at least four families from Southern China [30], BRCA1 1100delAT in families from Shanghai [16], BRCA2 4265delCT in at least three families from the Philippines [31] and BRCA2 2699del6 in two families from Indonesia [32], were also found in our cohort but these are unlikely to be common enough to warrant specific testing. Given the genetic diversity of the Asian populations, it is unlikely that screening for a panel of founder mutations will be as effective in this population as is the case for the Ashkenazi Jewish [33] or Icelandic [34] populations.
We found that BRCA2 may play an important role in genetic susceptibility among the small numbers of Malays in this cohort. Similar associations have been reported among the Filipinos and Japanese [31,35]. However, the reason for a higher proportion of BRCA2 mutations over BRCA1 mutations is not known, but may reflect cohort selection, genetic drift, or a possible prevalence of a modifying genetic or environmental factor that modifies the penetrance of BRCA1 or BRCA2 among Malays. Further studies using larger cohorts of Malay individuals are needed to address these possibilities.
In addition to the clearly deleterious protein-truncating mutations, a number of unclassified sequence variants were detected by sequencing. Of these, nine of 16 in BRCA1 (56%) and 17 of 31 in BRCA2 are novel (55%), and several of the remainder have only been described in Asian women. It is likely that the majority of these sequence variants have no clinical relevance, and the few that are likely to be deleterious are unlikely to change the basic conclusions of this study. We are conducting further analyses using established methods [36-38] to better understand the clinical significance of these sequence variants in our cohort.
Predicting BRCA1- and BRCA2-positive family status in Asia
As BRCA1 and BRCA2 mutation testing is expensive, any ability to determine the probability that a specific family may benefit is an important issue. Several tools have been developed to help clinicians in predicting the probability of carrying a BRCA1 or BRCA2 mutation based on the familial history of breast and/or ovarian cancer and all tools have been based on populations where the age-standardised rate for breast cancer has been significantly higher than that reported in Malaysia (80 to 100 per 100,000 compared with 30 to 50 per 100,000 in Malaysia).
The Manchester Scoring System is perhaps the easiest of these prediction tools to use, and to determine whether the likelihood of identifying a mutation in a family reaches the 10% threshold for either BRCA1 or BRCA2. This model is does not require computer implementation. However, given that the Manchester Scoring System was devised using data from the Manchester region in northwest England, it is unclear whether it would be as effective in populations with different demographics, such as that in many Asian countries. Our analysis indicated that a cut-off at a combined Manchester score of 15 seems optimal as a threshold (sensitivity of 72%, specificity of 74%, negative-predictive value of 93%) but with a low positive-predictive value (37%). Notably, for the same cut-off of 15 among the Danish [39], the sensitivity was 84%, but the specificity was lower at 44%. The optimal cut-off appears to be lower for our population compared with studies in Australians [40] and French-Canadians in Canada [41], where comparable sensitivity and specificity (86% and 82% respectively in the Australians, and 72% and 64% respectively in the Canadians) were obtained with a higher score of 18. Taken together, our data suggests that in populations such as ours, where the overall incidence of breast and ovarian cancers is lower than that in Caucasian populations, family history is more significant therefore giving a higher specificity at a lower score.
In contrast, BOADICEA requires computation and is more difficult to implement in a clinical setting that is not familiar with risk prediction and genetic testing. Nevertheless, the strength of the model relies in its ability to compute extensive family history, and mutations in other genes relevant to breast cancer, such as CHEK2, to calculate the probability of carrying a mutation in the BRCA genes. In our analysis, a cut-off probability of 10% or higher yielded comparable specificity albeit with compromised sensitivity (85% and 40% respectively) to that reported in an analysis of 300 non-Ashkenazi Jewish, predominantly Caucasian families [42] (specificity 68% and sensitivity 73% respectively).
We found that both the Manchester Scoring System and BOADICEA underestimated the number of mutation carriers in our cohort. The most likely explanation, which is consistent with other studies, may be that both methods underestimate the number of carriers in families with insignificant family history [42], that is both methods underestimate the exceptional nature of the families, within the context of a lower population rate of breast cancer. In addition, the underestimate may be more significant for BRCA2 in BOADICEA because the allelic frequency of BRCA2 may be different in the ethnic population we have studied compared with Caucasian populations, and may be because BRCA2 may have a different penetrance in this population.
Overall, in this typically Asian cohort where 80% (149 of 187) of the breast cancer patients had no or only a single first- or second-degree relative with breast cancer or ovarian cancer, 15% of women carried deleterious mutations in BRCA1 or BRCA2. This suggests that a family history as reported by an individual who carries a mutation in BRCA1 or BRCA2 may be neither dramatic nor obvious. Indeed, in a study of 10,000 individuals in the USA, up to 13% of individuals with a single first- or second-degree relative with early-onset breast cancer or ovarian cancer, carried deleterious mutations [6]. This suggests that careful evaluation of paternal as well as maternal family history is required, especially in women diagnosed with breast cancer before age 50 years or ovarian cancer at any age, to enable the appropriate identification and counselling of individuals at risk of carrying mutations in BRCA1 and BRCA2. We believe that identification of individuals at risk is particularly significant in Asia because the problem of limited family structure is not uncommon, in part because of loss of family information from migration, and there remains significant stigma in talking about cancer [9].
Conclusion
Taking into consideration the recommendations described above and our findings, it seems reasonable in a clinical setting to offer individuals with a personal or family history of cancer testing if they have a combined Manchester score of 15 or above. Lower thresholds could be used when resources become available and where the judgement of health care professionals involved in familial cancer clinics indicates. Our study underscores the need for larger collaborative studies among non-Caucasian populations to validate the role of genetic testing, the use of risk-prediction models and the role of risk-reducing strategies in ensuring that the other populations in the world may also benefit from the genomics and genetics era.
Abbreviations
BIC = Breast Cancer Information Core; BOADICEA = Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm; CI = confidence interval; MLPA = multiple ligation dependent probe amplification
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ET, LSY, PK, DL, TGT and SS carried out the genetic studies, data collection and data analysis. ET, YSY, TMK, NAMT, YCH and TSH participated in the selection and recruitment of patients to the study. YCH and TSH conceived the study and ET and TSH drafted the manuscript. All authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
We thank the participants and their families for taking part in this study and Nancy Tan for technical assistance in the project. This study was funded by research grants from the Malaysian Ministry of Science, Technology and Innovation, University Malaya Research Grants and Cancer Research Initiatives Foundation.
Contributor Information
E Thirthagiri, Email: eswary.thirthagiri@carif.com.my.
SY Lee, Email: sheauyee.lee@carif.com.my.
P Kang, Email: peter.kang@carif.com.my.
DS Lee, Email: daphne.lee@carif.com.my.
GT Toh, Email: gttoh@hotmail.com.
S Selamat, Email: suhaidaadura@yahoo.com.
S-Y Yoon, Email: sookyee.yoon@carif.com.my.
NA Mohd Taib, Email: naisha@um.edu.my.
MK Thong, Email: thongmk@ummc.edu.my.
CH Yip, Email: yipch@ummc.edu.my.
SH Teo, Email: soohwang.teo@carif.com.my.
References
- Domchek SM, Weber BL. Clinical management of BRCA1 and BRCA2 mutation carriers. Oncogene. 2006;25:5825–5831. doi: 10.1038/sj.onc.1209881. [DOI] [PubMed] [Google Scholar]
- Gudmundsdottir K, Ashworth A. The roles of BRCA1 and BRCA2 and associated proteins in the maintenance of genomic stability. Oncogene. 2006;25:5864–5874. doi: 10.1038/sj.onc.1209874. [DOI] [PubMed] [Google Scholar]
- Hall MJ, Olopade OI. Disparities in genetic testing: thinking outside the BRCA box. J Clin Oncol. 2006;24:2197–2203. doi: 10.1200/JCO.2006.05.5889. [DOI] [PubMed] [Google Scholar]
- Huo D, Olopade OI. Genetic testing in diverse populations: are researchers doing enough to get out the correct message? JAMA. 2007;298:2910–2911. doi: 10.1001/jama.298.24.2910. [DOI] [PubMed] [Google Scholar]
- Liede A, Narod SA. Hereditary breast and ovarian cancer in Asia: genetic epidemiology of BRCA1 and BRCA2. Hum Mutat. 2002;20:413–424. doi: 10.1002/humu.10154. [DOI] [PubMed] [Google Scholar]
- Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, Gumpper KL, Scholl T, Tavtigian SV, Pruss DR, Critchfield GC. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol. 2002;20:1480–1490. doi: 10.1200/JCO.20.6.1480. [DOI] [PubMed] [Google Scholar]
- Balraj P, Khoo AS, Volpi L, Tan JA, Nair S, Abdullah H. Mutation analysis of the BRCA1 gene in Malaysian breast cancer patients. Singapore Med J. 2002;43:194–197. [PubMed] [Google Scholar]
- Suter NM, Ray RM, Hu YW, Lin MG, Porter P, Gao DL, Zaucha RE, Iwasaki LM, Sabacan LP, Langlois MC, Thomas DB, Ostrander EA. BRCA1 and BRCA2 mutations in women from Shanghai China. Cancer Epidemiol Biomarkers Prev. 2004;13:181–189. doi: 10.1158/1055-9965.EPI-03-0196. [DOI] [PubMed] [Google Scholar]
- Chieng WSLS. Establishing a Cancer Genetics Programme in Asia – the Singapore Experience. Hereditary Cancer in Clinical Practice. 2006;4:126–135. doi: 10.1186/1897-4287-4-3-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song CG, Hu Z, Wu J, Luo JM, Shen ZZ, Huang W, Shao ZM. The prevalence of BRCA1 and BRCA2 mutations in eastern Chinese women with breast cancer. J Cancer Res Clin Oncol. 2006;132:617–626. doi: 10.1007/s00432-006-0105-9. [DOI] [PubMed] [Google Scholar]
- Chen ST, Chen RA, Kuo SJ, Chien YC. Mutational screening of breast cancer susceptibility gene 1 from early onset, bi-lateral, and familial breast cancer patients in Taiwan. Breast Cancer Res Treat. 2003;77:133–143. doi: 10.1023/A:1021386026051. [DOI] [PubMed] [Google Scholar]
- Saxena S, Chakraborty A, Kaushal M, Kotwal S, Bhatanager D, Mohil RS, Chintamani C, Aggarwal AK, Sharma VK, Sharma PC, Lenoir G, Goldgar DE, Szabo CI. Contribution of germline BRCA1 and BRCA2 sequence alterations to breast cancer in Northern India. BMC Med Genet. 2006;7:75. doi: 10.1186/1471-2350-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syamala V, Sreeja L, Syamala VS, Vinodkumar B, Raveendran PB, Sreedharan H, Kuttappan R, Balakrishnan L, Ankathil R. Novel germline mutations in BRCA2 gene among 96 hereditary breast and breast-ovarian cancer families from Kerala, South India. J Cancer Res Clin Oncol. 2007;133:867–874. doi: 10.1007/s00432-007-0229-6. [DOI] [PubMed] [Google Scholar]
- Hu Z, Wu J, Liu CH, Lu JS, Luo JM, Han QX, Shen ZZ, Shao ZM. The analysis of BRCA1 mutations in eastern Chinese patients with early onset breast cancer and affected relatives. Hum Mutat. 2003;22:104. doi: 10.1002/humu.9156. [DOI] [PubMed] [Google Scholar]
- Vinodkumar B, Syamala V, Abraham EK, Balakrishnan R, Ankathil R. Germline BRCA1 mutation and survival analysis in familial breast cancer patients in Kerala; South India. J Exp Clin Cancer Res. 2007;26:329–336. [PubMed] [Google Scholar]
- Li WF, Hu Z, Rao NY, Song CG, Zhang B, Cao MZ, Su FX, Wang YS, He PQ, Di GH, Shen KW, Wu J, Lu JS, Luo JM, Liu XY, Zhou J, Wang L, Zhao L, Liu YB, Yuan WT, Yang L, Shen ZZ, Huang W, Shao ZM. The prevalence of BRCA1 and BRCA2 germline mutations in high-risk breast cancer patients of Chinese Han nationality: two recurrent mutations were identified. Breast Cancer Res Treat. 2007;110:99–109. doi: 10.1007/s10549-007-9708-3. [DOI] [PubMed] [Google Scholar]
- National Cancer Register, Malaysia; 2003. [Google Scholar]
- Toh GTKP, Lee SS, Lee DS, Lee SY, Selamat S, Mohd Taib NA, Yoon SY, Yip CH, Teo SH. BRCA1 and BRCA2 germline mutations in Malaysian women with early-onset breast cancer without a family history. PLoS ONE. 2008;3:e2024. doi: 10.1371/journal.pone.0002024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoniou AC, Pharoah PP, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer. 2004;91:1580–1590. doi: 10.1038/sj.bjc.6602175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DG, Eccles DM, Rahman N, Young K, Bulman M, Amir E, Shenton A, Howell A, Lalloo F. A new scoring system for the chances of identifying a BRCA1/2 mutation outperforms existing models including BRCAPRO. J Med Genet. 2004;41:474–480. doi: 10.1136/jmg.2003.017996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DG, Lalloo F, Wallace A, Rahman N. Update on the Manchester Scoring System for BRCA1 and BRCA2 testing. J Med Genet. 2005;42:e39. doi: 10.1136/jmg.2005.031989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramus SJ, Harrington PA, Pye C, DiCioccio RA, Cox MJ, Garlinghouse-Jones K, Oakley-Girvan I, Jacobs IJ, Hardy RM, Whittemore AS, Ponder BA, Piver MS, Pharoah PD, Gayther S. Contribution of BRCA1 and BRCA2 mutations to inherited ovarian cancer. Hum Mutat. 2007;28:1207–1215. doi: 10.1002/humu.20599. [DOI] [PubMed] [Google Scholar]
- Lakhani SR, Jacquemier J, Sloane JP, Gusterson BA, Anderson TJ, Vijver MJ van de, Farid LM, Venter D, Antoniou A, Storfer-Isser A, Smyth E, Steel CM, Haites N, Scott RJ, Goldgar D, Neuhausen S, Daly PA, Ormiston W, McManus R, Scherneck S, Ponder BA, Ford D, Peto J, Stoppa-Lyonnet D, Bignon YJ, Struewing JP, Spurr NK, Bishop DT, Klijn JG, Devilee P, et al. Multifactorial analysis of differences between sporadic breast cancers and cancers involving BRCA1 and BRCA2 mutations. J Natl Cancer Inst. 1998;90:1138–1145. doi: 10.1093/jnci/90.15.1138. [DOI] [PubMed] [Google Scholar]
- Sng JH, Ali AB, Lee SC, Zahar D, Wong JE, Blake V, Sharif A, Cross G, Iau PT. BRCA1 c.2845insA is a recurring mutation with a founder effect in Singapore Malay women with early onset breast/ovarian cancer. J Med Genet. 2003;40:e117. doi: 10.1136/jmg.40.10.e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sng JH, Ali AB, Lee SC, Zahar D, Wong JE, Cross G, Iau PT. BRCA1 c.2845insA is a founder mutation in Singaporean Malay women with early onset breast/ovarian cancer. Ann Acad Med Singapore. 2003;32(Suppl 5):S53–55. [PubMed] [Google Scholar]
- Sng JH, Chang J, Feroze F, Rahman N, Tan W, Lim S, Lehnert M, Pool S van der, Wong J. The prevalence of BRCA1 mutations in Chinese patients with early onset breast cancer and affected relatives. Br J Cancer. 2000;82:538–542. doi: 10.1054/bjoc.1999.0960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho GH, Phang BH, Ng IS, Law HY, Soo KC, Ng EH. Novel germline BRCA1 mutations detected in women in singapore who developed breast carcinoma before the age of 36 years. Cancer. 2000;89:811–816. doi: 10.1002/1097-0142(20000815)89:4<811::AID-CNCR13>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Ali AB, Iau PT, Putti TC, Sng JH. BRCA1 disease-associated haplotypes in Singapore Malay women with early-onset breast/ovarian cancer. Breast Cancer Res Treat. 2007;104:351–353. doi: 10.1007/s10549-006-9467-6. [DOI] [PubMed] [Google Scholar]
- Lee AS, Ho GH, Oh PC, Balram C, Ooi LL, Lim DT, Wong CY, Hong GS. Founder mutation in the BRCA1 gene in Malay breast cancer patients from Singapore. Hum Mutat. 2003;22:178. doi: 10.1002/humu.9162. [DOI] [PubMed] [Google Scholar]
- Tang NL, Pang CP, Yeo W, Choy KW, Lam PK, Suen M, Law LK, King WW, Johnson P, Hjelm M. Prevalence of mutations in the BRCA1 gene among Chinese patients with breast cancer. J Natl Cancer Inst. 1999;91:882–885. doi: 10.1093/jnci/91.10.882. [DOI] [PubMed] [Google Scholar]
- De Leon Matsuda ML, Liede A, Kwan E, Mapua CA, Cutiongco EM, Tan A, Borg A, Narod SA. BRCA1 and BRCA2 mutations among breast cancer patients from the Philippines. Int J Cancer. 2002;98:596–603. doi: 10.1002/ijc.10194. [DOI] [PubMed] [Google Scholar]
- Purnomosari D, Pals G, Wahyono A, Aryandono T, Manuaba TW, Haryono SJ, van Diest PJ. BRCA1 and BRCA2 germline mutation analysis in the Indonesian population. Breast Cancer Res Treat. 2007;106:297–304. doi: 10.1007/s10549-006-9493-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayther SA, Harrington P, Russell P, Kharkevich G, Garkavtseva RF, Ponder BA. Frequently occurring germ-line mutations of the BRCA1 gene in ovarian cancer families from Russia. Am J Hum Genet. 1997;60:1239–1242. [PMC free article] [PubMed] [Google Scholar]
- Thorlacius S, Olafsdottir G, Tryggvadottir L, Neuhausen S, Jonasson JG, Tavtigian SV, Tulinius H, Ogmundsdottir HM, Eyfjord JE. A single BRCA2 mutation in male and female breast cancer families from Iceland with varied cancer phenotypes. Nat Genet. 1996;13:117–119. doi: 10.1038/ng0596-117. [DOI] [PubMed] [Google Scholar]
- Ikeda N, Miyoshi Y, Yoneda K, Shiba E, Sekihara Y, Kinoshita M, Noguchi S. Frequency of BRCA1 and BRCA2 germline mutations in Japanese breast cancer families. Int J Cancer. 2001;91:83–88. doi: 10.1002/1097-0215(20010101)91:1<83::AID-IJC1013>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Abkevich V, Zharkikh A, Deffenbaugh AM, Frank D, Chen Y, Shattuck D, Skolnick MH, Gutin A, Tavtigian SV. Analysis of missense variation in human BRCA1 in the context of interspecific sequence variation. J Med Genet. 2004;41:492–507. doi: 10.1136/jmg.2003.015867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavtigian SV, Samollow PB, de Silva D, Thomas A. An analysis of unclassified missense substitutions in human BRCA1. Fam Cancer. 2006;5:77–88. doi: 10.1007/s10689-005-2578-0. [DOI] [PubMed] [Google Scholar]
- Tavtigian SV, Deffenbaugh AM, Yin L, Judkins T, Scholl T, Samollow PB, de Silva D, Zharkikh A, Thomas A. Comprehensive statistical study of 452 BRCA1 missense substitutions with classification of eight recurrent substitutions as neutral. J Med Genet. 2006;43:295–305. doi: 10.1136/jmg.2005.033878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdes AM, Cruger DG, Thomassen M, Kruse TA. Evaluation of two different models to predict BRCA1 and BRCA2 mutations in a cohort of Danish hereditary breast and/or ovarian cancer families. Clin Genet. 2006;69:171–178. doi: 10.1111/j.1399-0004.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- James PA, Doherty R, Harris M, Mukesh BN, Milner A, Young MA, Scott C. Optimal selection of individuals for BRCA mutation testing: a comparison of available methods. J Clin Oncol. 2006;24:707–715. doi: 10.1200/JCO.2005.01.9737. [DOI] [PubMed] [Google Scholar]
- Simard J, Dumont M, Moisan AM, Gaborieau V, Malouin H, Durocher F, Chiquette J, Plante M, Avard D, Bessette P, Brousseau C, Dorval M, Godard B, Houde L, INHERIT BRCAs, Joly Y, Lajoie MA, Leblanc G, Lépine J, Lespérance B, Vézina H, Parboosingh J, Pichette R, Provencher L, Rhéaume J, Sinnett D, Samson C, Simard JC, Tranchant M, Voyer P, et al. Evaluation of BRCA1 and BRCA2 mutation prevalence, risk prediction models and a multistep testing approach in French-Canadian families with high risk of breast and ovarian cancer. J Med Genet. 2007;44:107–121. doi: 10.1136/jmg.2006.044388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barcenas CH, Hosain GM, Arun B, Zong J, Zhou X, Chen J, Cortada JM, Mills GB, Tomlinson GE, Miller AR, Strong LC, Amos CI. Assessing BRCA carrier probabilities in extended families. J Clin Oncol. 2006;24:354–360. doi: 10.1200/JCO.2005.02.2368. [DOI] [PubMed] [Google Scholar]
- Fetzer S, Tworek HA, Piver MS, DiCioccio RA. Classification of IVS1-10T-->C as a polymorphism of BRCA1. Cancer Genet Cytogenet. 1999;113:58–64. doi: 10.1016/S0165-4608(99)00005-9. [DOI] [PubMed] [Google Scholar]
- Easton DF, Deffenbaugh AM, Pruss D, Frye C, Wenstrup RJ, Allen-Brady K, Tavtigian SV, Monteiro AN, Iversen ES, Couch FJ, Goldgar DE. A systematic genetic assessment of 1,433 sequence variants of unknown clinical significance in the BRCA1 and BRCA2 breast cancer-predisposition genes. Am J Hum Genet. 2007;81:873–883. doi: 10.1086/521032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang P, Lim IH, Lee TC, Luo JT, Ong DC, Tan PH, Lee AS. BRCA1 and BRCA2 Mutations in an Asian Clinic-based Population Detected Using a Comprehensive Strategy. Cancer Epidemiol Biomarkers Prev. 2007;16:2276–2284. doi: 10.1158/1055-9965.EPI-07-0403. [DOI] [PubMed] [Google Scholar]