Abstract
Angiotensin II (AngII) infusions augment renal angiotensinogen mRNA and protein and urinary angiotensinogen excretion (UAGT). Further experiments were performed in 4 groups of rats: normal salt diet with sham operation, NS+Sham, n=6; NS with AngII infusion at 40 ng/min via osmotic minipump, NS+AngII(40), n=9; NS with AngII infusion at 80 ng/min, NS+AngII(80), n=9; high-salt diet with deoxycorticosterone acetate salt pellet (100 mg), HS+DOCA, n=4. These experiments sought to determine whether enhanced UAGT is specifically associated with increased kidney AngII levels or is a nonspecific consequence of the hypertension. Systolic BP (SBP) was significantly increased to 131±2 and 162±2 mm Hg at day 11 in NS+AngII(40) and NS+AngII(80), respectively, compared with NS+Sham (110±1). Regression analysis demonstrated a positive relationship (R=0.49) between SBP and UAGT for NS+Sham (1.1±0.3 nmol AngI/d), NS+AngII(40) (2.5±0.9), and NS+AngII(80) (5.5±1.5). UAGT was also highly correlated (R=0.70) with kidney AngII content for NS+Sham (49±6 fmol/g), NS+AngII(40) (215±49), and NS+AngII(80) (347±47); but not with plasma AngII (R=0.12). HS+DOCA rats also exhibited increased SBP to 134±1 mm Hg, but UAGT (1.4±0.4 nmol AngI/d) and intrarenal AngII content (13±2 fmol/g) were not increased despite the hypertension. Infused human angiotensinogen could not be detected in urine of sham-operated or AngII-infused rats (n=4 each). These data demonstrate that UAGT increases in AngII-dependent hypertension in a dose- and time-dependent manner, but not in hypertension elicited by HS+DOCA. The results support the hypothesis that AngII-dependent hypertension results in elevated intrarenal AngII and angiotensinogen levels, reflected by increased UAGT, which does not occur in an AngII-independent hypertensive model.
Keywords: angiotensin II; angiotensinogen; rats; kidney; urine; sodium, dietary; deoxycorticosterone acetate salt; Western blot
In previous studies, we demonstrated that chronic angiotensin (Ang) II infusion results in significant increases in renal expression of angiotensinogen protein,1 as well as angiotensinogen mRNA.2 Furthermore, we recently showed that urinary excretion of angiotensinogen was significantly increased and was associated with enhanced intrarenal AngII levels in AngII-infused rats fed a high-salt diet.3 These results prompted us to perform further experiments to evaluate the relationships between urinary excretion rates of angiotensinogen and intrarenal activity of the renin-angiotensin system (RAS), as well as blood pressure (BP), in AngII-induced hypertensive rats and in a volume-dependent model of hypertension induced by administration of a high-salt diet and deoxycorticosterone acetate salt (DOCA).
This study was performed to address the following hypotheses: (1) urinary excretion of angiotensinogen during AngII infusions is enhanced in a dose- and time-dependent manner, (2) enhanced urinary excretion of angiotensinogen during AngII infusions is closely associated with increased kidney AngII levels, (3) enhanced urinary excretion of angiotensinogen is not primarily a consequence of the elevated arterial pressure or of hypertension-induced proteinuria, and (4) urinary excretion of angiotensinogen originates from the kidney and not the plasma.
Methods
Preparation of Animals
The experimental protocol was approved by the Tulane Animal Care and Use Committee. Male Sprague-Dawley rats (175 to 200g, Charles River, Wilmington, Mass.) were housed in wire metabolic cages and maintained, with free access to water, in a temperature-controlled room regulated on a 12-hour light/dark cycle. Rats (n=40) were fed a commercially available rat chow containing normal salt (NS, 0.6% sodium chloride, Harlan Teklad 170950, n=36) or high salt (HS, 8% sodium chloride, Harlan Teklad TD 79119, n=4) for 2 weeks. Rats were anesthetized with sodium pentobarbital (50 mg/kg, intraperitoneally), and an osmotic minipump (Alza) or a pellet of DOCA (100 mg, Innovative Research M-121) was implanted subcutaneously at the dorsum of the neck on day 0. Rats were selected at random from the NS group to serve as sham controls (n=10) or to receive AngII (Calbiochem-Novabiochem) infusion at a rate of 40 ng/min for AngII(40), n=9, or 80 ng/min for AngII(80), n=17. Systolic BP was measured in conscious rats using tail-cuff plethysmography at days −1, 3, 7, and 11 in AngII(40) (n=9), AngII(80) (n=9), Sham (n=10), and HS+DOCA (n=4) groups.
Sample Collection
Twenty-four hour urine samples were collected on days 0, 4, 8, and 12 in 0.6 mL distilled water containing 50 μg pepstatin A, 10 mg sodium azide, 300 nmol enalaprilat, and 125 μmol EDTA as previously reported.3-5 In separate studies, we determined that an addition of 50 μg of pepstatin to the cocktail for 24-hour urine collections is essential because urine samples that do not contain pepstatin do not have arrested formation of AngI from angiotensinogen. In urine samples from 4 rats, AngI values were 59.6±5.0 pmol/mL without incubation with excess renin versus 60.1±10.5 pmol/mL following 2-hour incubation with excess renin. This indicates that the generation of AngI from urinary angiotensinogen is complete during the 24-hour collection period in the absence of pepstatin. However, we determined that 50 μg pepstatin does not inhibit the conversion of angiotensinogen to AngI following addition of excess renin in urine samples collected from AngII-infused rats (80 ng/min for 2 weeks, n=4). Urinary AngI generation is very low (0.31±0.13 nmol/d) and increases 14-fold (4.24±0.28) with the addition of excess renin (60 μU). In contrast, collection of urine samples in 500 μg pepstatin inhibits the generation of AngI in the presence (0.77±0.20) and in the absence (undetectable) of excess renin. Urine samples were centrifuged and supernatant was separated and stored at −20°C until assayed for total protein and angiotensinogen concentrations. Urinary concentration of protein was measured by a colorimetric assay using a commercially available kit (Bio-Rad).
Blood and kidney samples were harvested on day 13. After decapitation, trunk blood was collected into 2 chilled tubes containing EDTA (5 mmol/L) for plasma renin activity or EDTA (5 mmol/L), enalaprilat (20 μmol/L), pepstatin A (10 μmol/L), and 1,10-phenanthroline (1.25 mmol/L) for plasma AngII. Plasma was separated and stored at −20°C until assayed for plasma renin activity and AngII as previously described.1,2 Immediately after removal, kidneys were homogenized in cold methanol and processed for measurement of renal AngII as previously described.1,2
Measurements of Plasma and Kidney AngII
Plasma and kidney AngII measurements were performed as previously described6-8 using a combined method of solid phase extraction and radioimmunoassay (RIA). Plasma and kidney samples were extracted on C18 reverse-phase bond elute columns (Varian Inc, 1210−2005 for plasma, 1210−2032 for kidney). RIA was performed using 125I-AngII (NEN Life Sciences, NEX-105) and AngII antiserum (Phoenix Pharmaceuticals Inc, RAB-002−12) with commercially available standards (Phoenix Pharmaceuticals Inc, 002−12).
Measurements of Urinary Angiotensinogen
Urinary excretion of angiotensinogen was evaluated by RIA as previously reported.1,3,8 RIA was performed to measure AngI generated following incubation of samples with excess amounts of porcine renin (Sigma, 60 μU). RIA of AngI was performed with a commercially available kit (Incstar). Urine samples were incubated with renin at 37°C and removed from incubation at 0, 10, 30, 60, and 120 minutes. The amount of AngI generated at each time point was determined by comparison to the standard curve. The AngI produced was plotted versus time, and saturation kinetics due to conversion of all angiotensinogen to AngI was observed by 60 minutes. The sensitivity of the standard curve, defined as the smallest value that can be distinguished from zero, is 13.9 fmol/tube of AngI. Data on the cross-reactivity of the antiserum used in the kit are expressed as the ratio of AngI concentration to the cross-reacting substance concentration at 50% inhibition of maximum binding as follows: AngI 100%, synthetic renin substrate tetradecapeptide 0.02%, AngII <0.03%, and AngIII <0.03%.
Acute Experiment of Human Angiotensinogen Infusion
AngII-infused (80 ng/min for 2 weeks, n=4) and sham-operated (n=4) rats were anesthetized with Inactin (100 mg/kg, intraperitoneally) and prepared for acute clearance studies as previously described.9 During the surgical preparation, Ringer's solution containing 6% bovine serum albumin (pH 7.4) was infused intravenously at a rate of 20 μL/min to replace volume losses. Thereafter, Ringer's solution containing 1% bovine serum albumin (pH 7.4) was infused at a rate of 20 μL/min for the duration of the stabilization and experimental periods. Systolic and diastolic BP were monitored via a femoral artery catheter. After a 60-minute stabilization period, 2 consecutive 30-minute urine samples were collected. Then, purified human angiotensinogen (100 μg, Calbiochem-Novabiochem) was infused for 1 minute at time 0. Urine samples (≈100 μL) were collected every 30 minutes for 300 minutes from a catheter placed in the left ureter into an inhibitor cocktail as previously reported.3 Blood samples (≈100 μL) were collected via the catheterized artery at time 0 and 300 minutes with inhibitor cocktails as previously described.3 Blood and urine samples were centrifuged, and supernatant was separated and stored at −20°C until assayed for human and rat angiotensinogen by Western blot analysis.
Western Blot Analysis of Angiotensinogen
Western blot analysis of collected plasma (0.1 μL) and urine (1.5% of 30-minute collection, ≈1.5 μL) samples against rat and human angiotensinogen was done with a standard protocol as described previously.1-3 Membranes were probed with sheep anti-rat angiotensinogen primary antibody (1:5000, 2 hour), stripped with Western Re-Probe solution (Geno Technology) and reprobed with rabbit anti-human angiotensinogen primary antibody, newly developed as described below (1:5500, 2 hour). Corresponding secondary antibodies were purchased from Amersham Pharmacia Biotech (1:3000, 1 hour).
Primary Antibody against Human Angiotensinogen
Multiple alignment of amino acid sequences between rat angiotensinogen (GeneBank Accession No. AAA98779) and human angiotensinogen (NP_000020) are summarized in the Table. Multifactorial analysis as an antigen was employed (Genetyx, Software Development Co). Underlined sequences in the Table (TELNLQKLSNDRIR) were chosen as an antigen for generation of the human angiotensinogen antibody. Peptide synthesis, immunization of rabbits, and affinity purification were performed by Zymed Laboratories.
Multiple Alignment of Amino Acid Sequences Between Rat and Human Angiotensinogen
| Rat | 1 | ---------MTPTGAGLKATIFCILTWVSLTAGDRVYIHPFHLLYYSKSTCAQLENPSVE | 51 |
| Human | 1 | MRKRAPQSEMAPAGVSLRATILCLLAWAGLAAGDRVYIHPFHLVIHNESTCEQLAKAHAG | 60 |
| * * * * *** * * * * ************ *** ** | |||
| Rat | 52 | TLPEPTFEPVPIQAKTSPVDEKTLRDKLVLATEKLEAEDRQRAAQVAMIAHFMGFRMYKM | 111 |
| Human | 61 | KPKDPTFIPAPIQAKTSPVDEKALQDQLVLVAAKLDTEDKLRAAMVGMLAHFLGFRIYGM | 120 |
| *** * ************ * * *** ** ** *** * * *** *** * * | |||
| Rat | 112 | LSEARGVASGAV-LSPPALFGTLVSFYLGSLDPTASQLQVLLGVPVKEGDCTSRLDGHKV | 170 |
| Human | 121 | HSELWGWHGATVLSPTAVFGTLASLYLGALDHTADRLQAILGVPWKDKHCTSRLDAHKV | 180 |
| ** ** ** *** * **** * *** ** ** ** **** * ****** *** | |||
| Rat | 171 | LTALQAVQGLLVTQGGSSSQTPLLQSTWGLFTAPGLRLKQPFVESLGPFTPAIFPRSLD | 230 |
| Human | 181 | LSALQAVQGLLVAQGRADSQAQLLLSTWGVFTAPGLHLKQPFVQGLALYTPWLPRSLD | 240 |
| * ********** ** ** ** ***** ****** ****** * ** ***** | |||
| Rat | 231 | LSTDPVLAAQKINRFVQAVTGWKMHLPLEGVSTDSTLFFNTYVHFQGKMRGFSQLTGLHE | 290 |
| Human | 241 | FTELDVAAE-KIDRFMQAVTGWKTGCSLMGASVDSTLAFNTYVHFQGKMKGFSLLAEPQE | 299 |
| * * ** ** ******* * * * **** *********** *** * * | |||
| Rat | 291 | FWVDNSTSVSVPMLSGTGNFQHWSDAQNNFSVTRVPLGESVTLLLIQPQCASDLDRVEVL | 350 |
| Human | 300 | FWVDNSTSVSVPMLSGMGTFQHWSDIQDNFSVTQVPFTESACLLLIQPHYASDLDKVEGL | 359 |
| **************** * ****** * ***** ** ** ****** ***** ** * | |||
| Rat | 351 | VFQHDFLTWIKNPPPRAIRLTLPQLEIRGSYNLQDLLAQAKLSTLLGAEAHLGKMGDTHP | 410 |
| Human | 360 | TFQQNSLNWMKKLSPRTIHLTMPQLVLQGSYDLQDLLAQAELPAILHTELNLQKLSNDRI | 419 |
| ** * * * ** * ** *** *** ******** * * * ** * | |||
| Rat | 411 | RVGEVLNSILLELQAGEEEQPTESAQQPGSPEVLDVTLSSPFLFAIYERDSGALHFLGRV | 470 |
| Human | 420 | RVGEVLNSIFFELEADEREPT-ESTQQLNKPEVLEVTLNRPFLFAVYDQSATALHFLGRV | 478 |
| ********* ** * * * * ** ** **** *** ***** * ******* | |||
| Rat | 471 | DNPQNW | 477 |
| Human | 479 | AHPLSTA | 485 |
| ** |
Rat angiotensinogen and human angiotensinogen have a similar structure and an equivalent molecular size, but rat renin is species-specific and cannot cleave human angiotensinogen;26 therefore, human angiotensinogen is inactive in rat. Underlined sequences were chosen as an antigen for the generation of human angiotensinogen antibody because of the least degree of homology. Bolded sequences correspond to AngI. Asterisks indicate complete match at those sites.
Statistical Analysis
Statistical analysis was performed using a 1-way factorial or a 2-way repeated ANOVA with the post hoc Scheffé F test. All data are presented as mean±SEM. P<0.05 was considered significant.
Experimental Design
To address the AngII dose- and time-dependency of urinary excretion of angiotensinogen, data were compared among the Sham, AngII(40), and AngII(80) groups of rats. Because the combined treatment of HS and DOCA induced a volume-dependent hypertension equivalent to that observed in the AngII(40) rats, comparisons were made between AngII(40) and HS+DOCA groups of rats.
Results
AngII Infusions and Urinary Angiotensinogen
AngII infusion significantly increased systolic BP in a time- and dose-dependent manner. Systolic BP was 131±2 mm Hg in the AngII(40) rats and 162±2 mm Hg in the AngII(80) rats by the 11th day of infusion (Figure 1A). AngII infusion significantly suppressed plasma renin activity (5.5±0.7 ng of AngI/mL per hour for Sham, 0.2±0.1 for AngII[40], and 0.1±0.1 for AngII[80]). Plasma AngII concentrations (Figure 1B) tended to increase with AngII infusion with values 76% greater than Sham rats (49±16 fmol/mL) in AngII(80) rats (86±8), but these changes did not achieve statistical significance in this series of experiments (P=0.10). However, kidney AngII content increased significantly at each dose of AngII infusion (49±6 fmol/g for Sham, 215±49 for AngII[40], and 347±47 for AngII[80]) as shown in Figure 1C.
Figure 1.
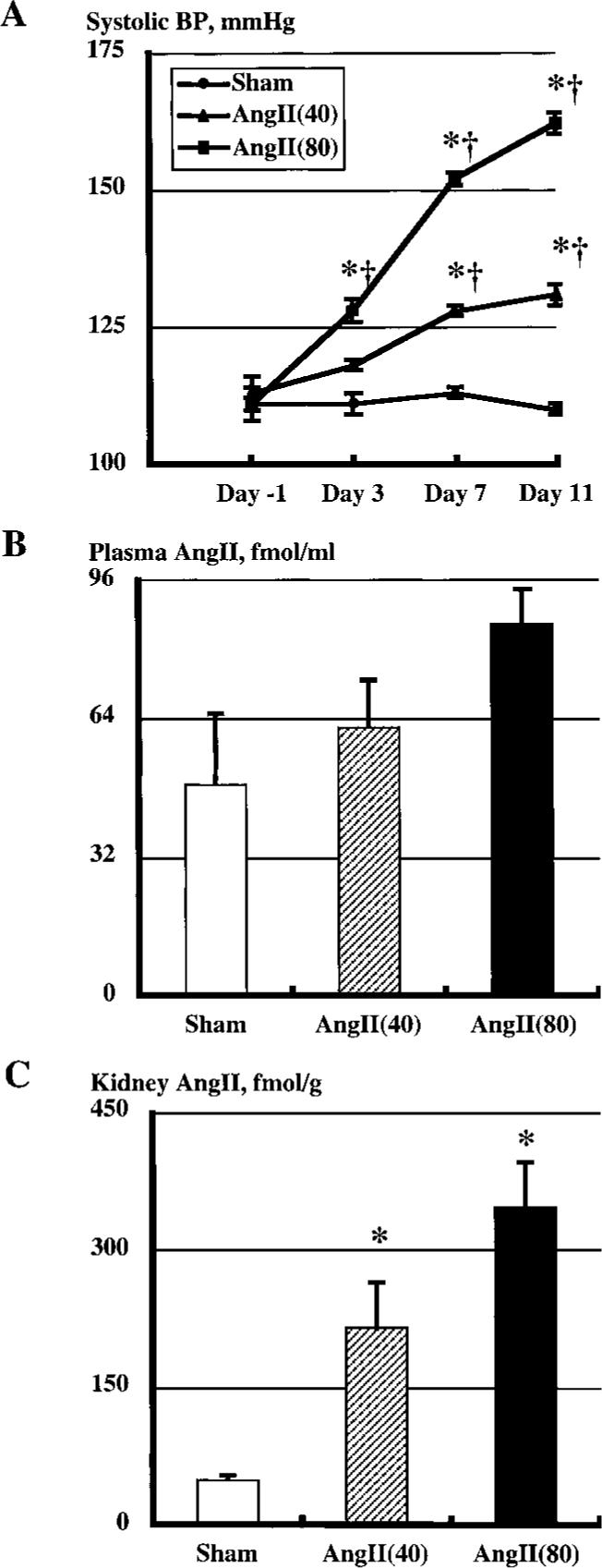
A, Systolic BP in 3 groups measured at −1, 3, 7, and 11 days. Systolic BP was unaltered during the protocol in the Sham group; however, AngII infusion significantly increased systolic BP in a time- and dose-dependent manner. *P<0.05 vs day −1; †P<0.05 vs Sham group at a given time period. B, Plasma AngII concentrations in Sham and AngII-infused rats. C, Kidney AngII contents in Sham and AngII-infused rats. *P<0.05 vs Sham group.
AngII infusion caused an increased urinary excretion of protein as depicted in Figure 2A. Similarly, AngII infusion led to progressive increases in urinary excretion rate of angiotensinogen (Figure 2B). Regression analysis showed a positive relationship between systolic BP at day 11 and urinary angiotensinogen excretion at day 12 (Figure 3A). Plasma AngII concentration was not correlated with UAGT (Figure 3B); however, regression analysis demonstrated that kidney AngII content was highly correlated with urinary angiotensinogen excretion (Figure 3C).
Figure 2.
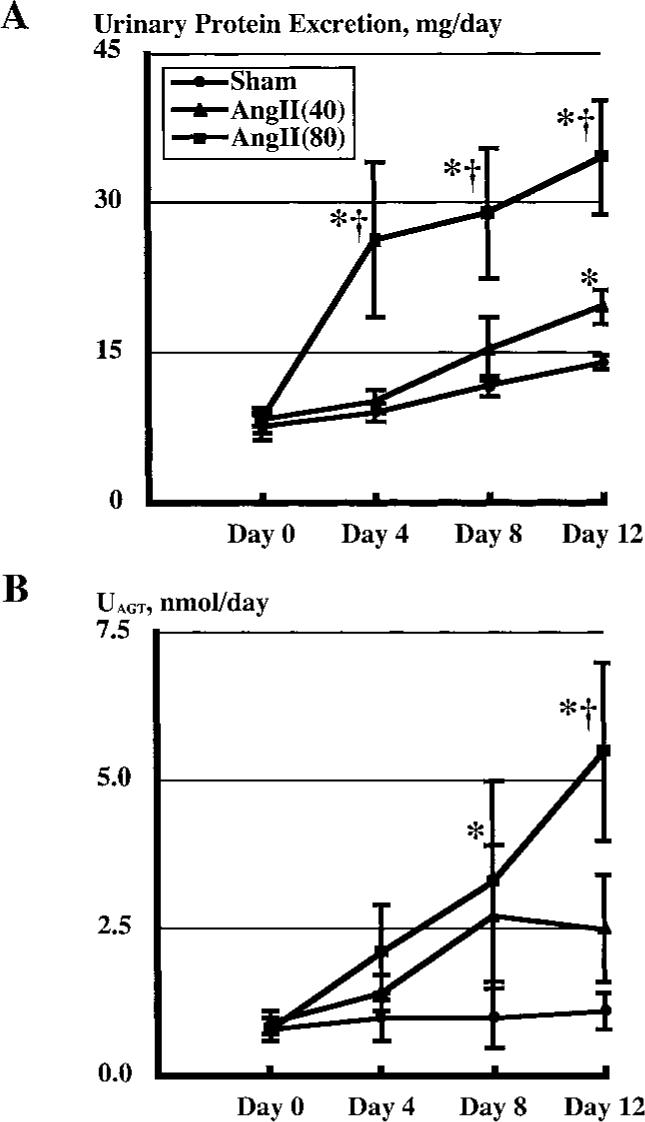
A, Urinary protein excretion rates in Sham and AngII-infused rats. B, Urinary excretion rates of angiotensinogen (UAGT) in Sham and AngII-infused rats. *P<0.05 vs day 0; †P<0.05 vs Sham group at the same time period.
Figure 3.
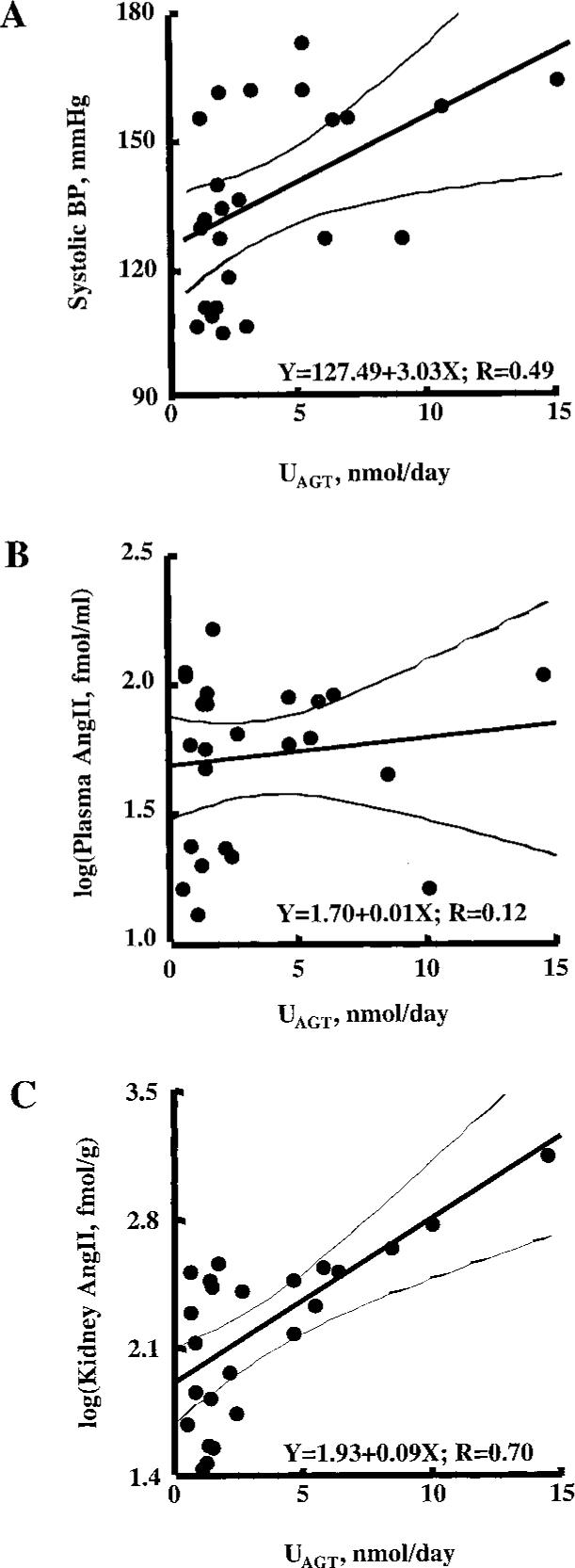
A, Regression analysis between systolic BP at day 11 and urinary angiotensinogen excretion at day 12 (R=0.49). B, Regression analysis between plasma AngII concentrations and urinary angiotensinogen excretion at day 12 (R=0.12). C, Regression analysis between kidney AngII contents and urinary angiotensinogen excretion (R=0.70).
DOCA plus high-salt diet rats significantly increased systolic BP (112±2 mm Hg at day −1, 120±3 at day 3, 135±3 at day 7, and 134±1 at day 11) to levels achieved with 40 ng/min AngII infusion by day 11 (Figure 4A). Plasma renin activity was suppressed by high-salt diet and DOCA (0.1±0.1 ng of AngI/mL per hour) to similar values found in the AngII(40) rats (0.2±0.1). Plasma AngII concentrations tended to decrease in HS+DOCA rats (27±5 fmol/mL), but these changes were not statistically significant compared with those measured in the AngII(40) rats (62±11, P=0.07). However, kidney AngII content was significantly lower in HS+DOCA (13±2 fmol/g) compared with the AngII(40) group (215±49).
Figure 4.
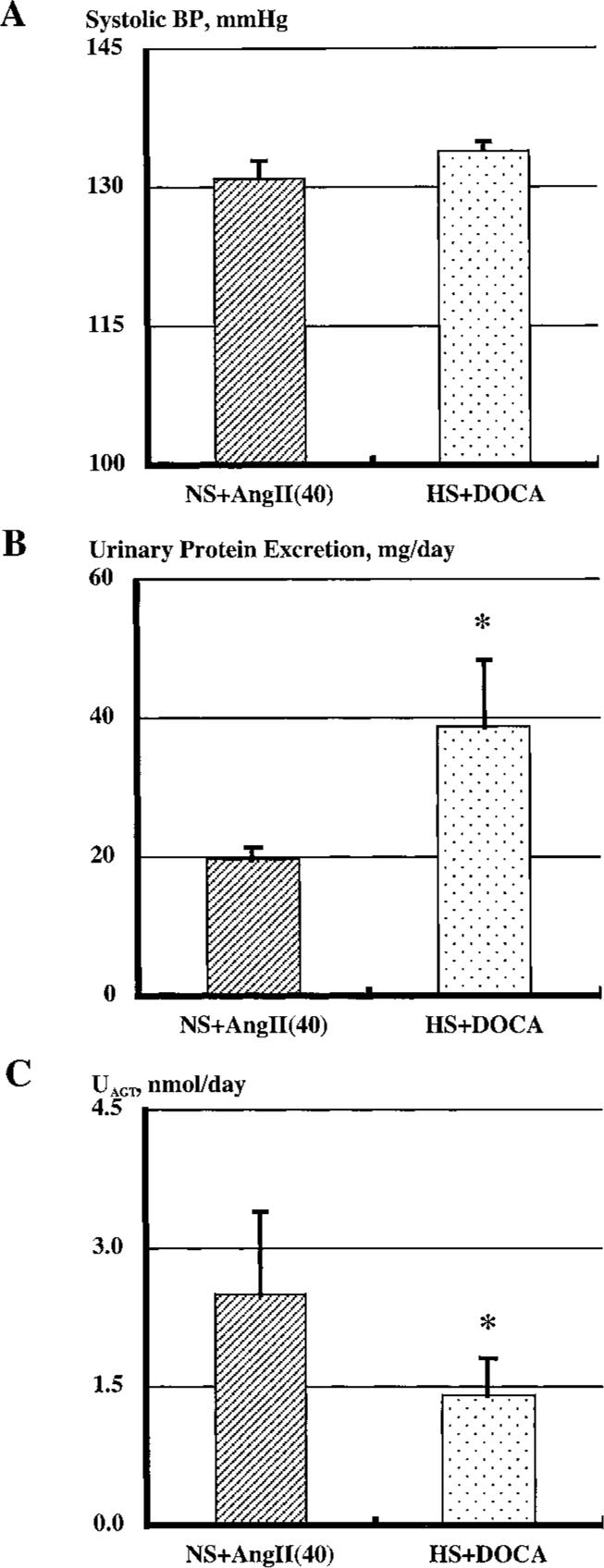
A, Systolic BP at day 11 in NS+AngII(40) and HS+DOCA groups. B, Urinary excretion of protein at day 12 in NS+AngII(40) and HS+DOCA. C, Urinary excretion rates of angiotensinogen in AngII-infused rats and in HS+DOCA rats. *P<0.05 vs NS+AngII(40) group.
Urinary excretion of protein at day 12 is depicted in Figure 4B. Urinary excretion of protein (8.0±2.0 mg/d at day 0 and 38.9±9.7 at day 12) was significantly higher in the HS+DOCA rats compared with AngII(40) animals at day 11 despite similar levels of systolic BP. In contrast, urinary excretion of angiotensinogen at day 12 (Figure 4C) was significantly lower in HS+DOCA rats than in AngII-infused rats. Urinary excretion of angiotensinogen was unchanged in HS+DOCA rats over time (0.9±0.3 nmol/d at day 0 and 1.4±0.4 at day 12).
Primary Antibody Against Human Angiotensinogen
Purified human angiotensinogen (25 to 50 ng) and human plasma (0.025 to 0.05 μL) were probed with the newly developed human angiotensinogen antibody (Figure 5A). Purified human angiotensinogen and human plasma showed bands at 60 kDa, which is consistent with a previous report.10 When the antiserum was preadsorbed with purified human angiotensinogen, the 60-kDa bands of the purified human angiotensinogen and human plasma were abolished (Figure 5B). These results indicate that the antiserum recognizes human angiotensinogen. A 50-kDa band was observed in the human plasma sample, which may be nonspecific binding because it was still evident after preadsorption of the antiserum. The 50-kDa band is also recognized in rat plasma samples in Figure 6.
Figure 5.
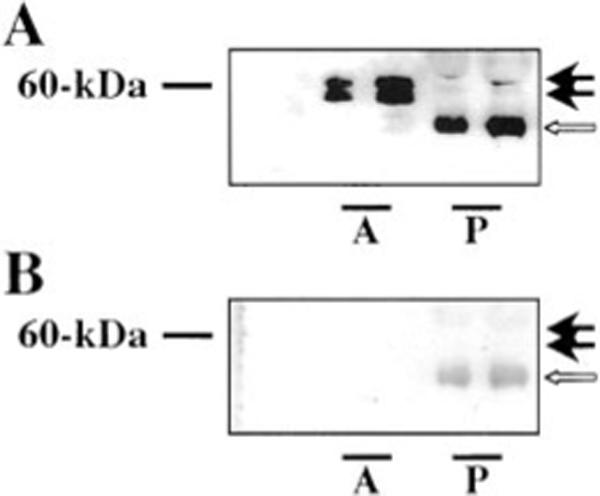
A, Purified human angiotensinogen (A, 25 to 50 ng) and human plasma (P, 0.025 to 0.05 μL), were probed with a newly raised antiserum against human angiotensinogen. Purified human angiotensinogen and human plasma showed bands at 60 kDa (black arrows). B, When the antiserum was preadsorbed with purified human angiotensinogen, these bands were abolished (black arrows). The lower band at 50 kDa of human plasma sample (white arrows) may be nonspecific binding.
Figure 6.
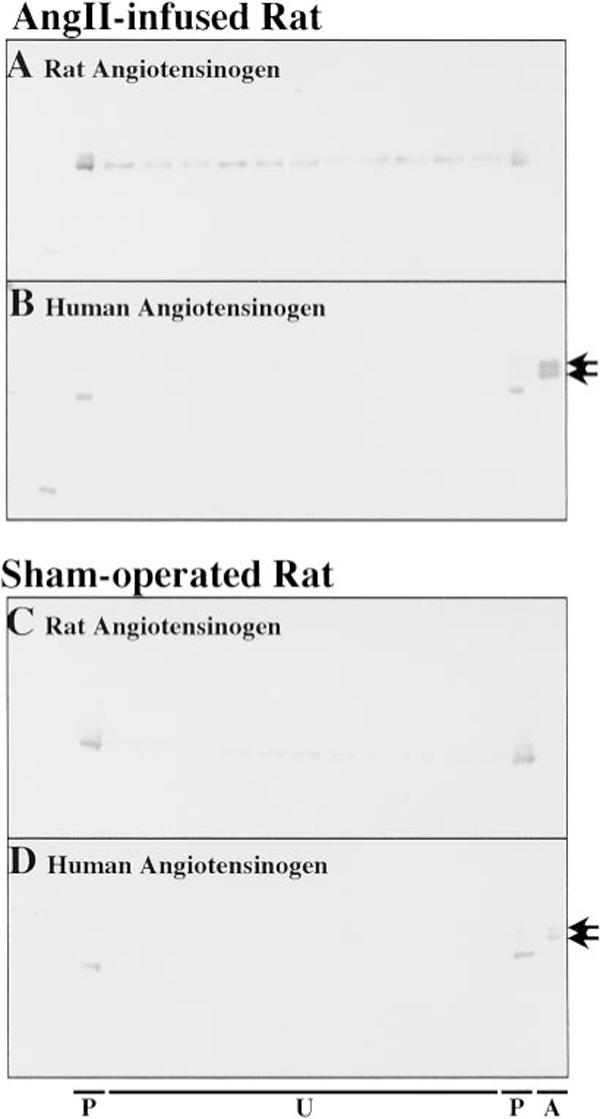
Representative films of Western blot analysis of AngII-infused (A and B) or sham-operated (C and D) rats against rat angiotensinogen (A and C) and human angiotensinogen (B and D). A and C, The antibody against rat angiotensinogen does not recognize human angiotensinogen (the right blank lanes on panels A and C). Rat angiotensinogen was detected in plasma and urine before and after the administration of human angiotensinogen. B and D, Human angiotensinogen was detected only in the plasma collected from rats infused with human angiotensinogen. Human angiotensinogen was not detected in the urine in either AngII-infused or sham-operated rats. The lower bands at 50 kDa of rat plasma samples may be nonspecific binding. P, on the left, indicates 0.1 μL of plasma sample before the administration; U, 1.5% of urine sample collected every 30 minutes from 30 minutes before the purified human angiotensinogen infusion to 300 minutes after; P, on the right, 0.1 μL of plasma sample after the administration of human angiotensinogen; A, purified human angiotensinogen, 75 ng on Panel B, 25 ng on Panel D.
Hemodynamic Effects of Human Angiotensinogen Infusion
Systolic (Figure 7A) and diastolic (Figure 7B) BP and urinary volumes (Figure 7C) are shown before and after administration of purified human angiotensinogen. BP of AngII-infused rats was significantly higher than that of sham-operated rats. However, administration of human angiotensinogen did not alter BP in either group. Urinary volume was not different between groups and was not altered by administration of human angiotensinogen. These results indicate that administration of 100 μg human angiotensinogen does not affect the hemodynamics of rats.
Figure 7.
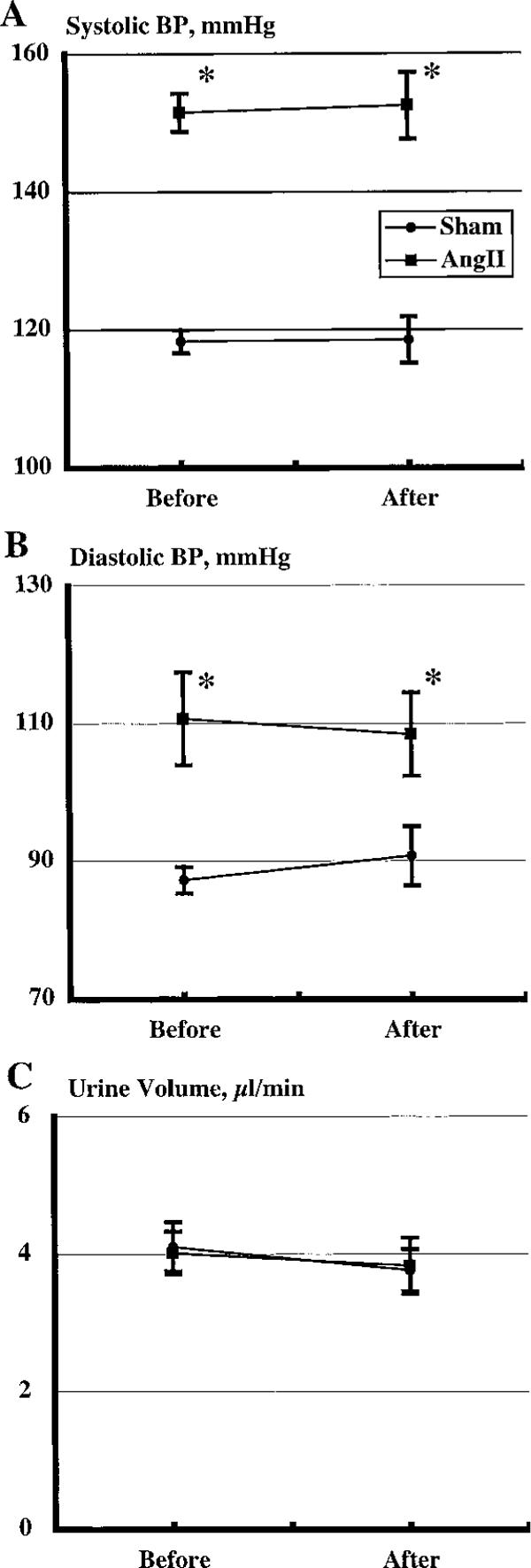
Systolic (A) and diastolic (B) BP and urinary volume (C) before and after administration of purified human angiotensinogen. Administration of human angiotensinogen did not alter BP in either group. Urinary volume was unchanged between groups or by administration of human angiotensinogen. *P<0.05 between AngII-infused and sham-operated rats.
Western Blot Analysis of Angiotensinogen
Representative films of Western blot analysis of an AngII-infused (Figures 6A and 6B) or sham-operated (Figures 6C and 6D) rat against rat angiotensinogen (Figures 6A and 6C) and human angiotensinogen (Figures 6B and 6D) show that the antibody against rat angiotensinogen does not recognize human angiotensinogen (the right blank lanes on Figures 6A and 6C). Rat angiotensinogen was detected in plasma and urine before and after the administration of human angiotensinogen. Human angiotensinogen, however, was detected only in the plasma collected after the administration of human angiotensinogen, but was not detected in the urine in AngII-infused or sham-operated rats. As described in the methods section, the low molecular weight bands in rat plasma samples before and after the administration may be nonspecific binding. We repeated the same procedures with 4 independent rats from both groups, and the results were similar. The failure to detect human angiotensinogen in the urine suggests limited glomerular permeability and/or tubular degradation. These results indicate that urinary angiotensinogen originates from the kidney and not the plasma.
Discussion
The present study demonstrates that chronic AngII infusion leads to increases in urinary excretion of angiotensinogen in a time- and dose-dependent manner. These results are consistent with previous data showing that chronic AngII infusion significantly increases renal expression of angiotensinogen mRNA levels2,11 and protein levels.1 As previously shown, AngII infusion enhances kidney AngII content even when the increases in plasma AngII concentration were not statistically significant.1,3 Because intrarenal angiotensinogen protein is predominantly localized to proximal tubular cells2,12-18 and there is extensive expression of AngII type I receptor on proximal tubular cells,19 it seems likely that, in AngII-infused rats, the modest increases in AngII, either in the filtrate or interstitial fluid, activate the AngII type I receptor complex and enhance angiotensinogen expression in proximal tubular cells, leading to increased angiotensinogen secretion. Presumably, increased angiotensinogen secretion from proximal tubular cells into the lumen is responsible for the increased urinary excretion rate of angiotensinogen. These increased levels of angiotensinogen in the urine indicate that greater amounts of angiotensinogen traverse the distal nephron segments and may result in increased formation of AngII in distal as well as proximal tubular fluid. The increased tubular AngII formation may be partially responsible for the elevated intrarenal AngII content found in this model.
Chronic AngII-induced hypertension was also associated with increased urinary protein excretion. Thus, it is possible that the enhanced urinary excretion rate of angiotensinogen during AngII infusions is a nonspecific consequence of the hypertension or of the increases in urinary excretion of protein. To address these issues, the urinary excretion rate of angiotensinogen was investigated in the DOCA plus high-salt hypertensive model, which displays markedly depressed plasma renin activity.20 Although some studies have used the combination of DOCA, uninephrectomy, and high-salt diet, this combination induces severe hypertension with systolic BP of approximately 190 mm Hg.21 For the present study, however, we employed DOCA and high-salt diet without uninephrectomy to induce a mild hypertension that was equivalent to the NS+AngII(40) group. The lower dose of AngII infusion or the combination of high-salt diet and DOCA increased systolic BP to similar levels. Interestingly, urinary protein excretion in HS+DOCA was significantly higher than in the AngII-infused rats. In contrast, urinary excretion of angiotensinogen was significantly lower in HS+DOCA rats than in the AngII-infused rats. These results demonstrate a dissociation between urinary protein excretion and the urinary angiotensinogen excretion rate. Thus, the enhanced urinary excretion rate of angiotensinogen is not simply the consequence of hypertension or proteinuria. Collectively, the results indicate that the enhanced urinary excretion rate of angiotensinogen is specifically a consequence of AngII-induced hypertension and the associated stimulation of intrarenal angiotensinogen mRNA and protein levels.
The amounts of urinary angiotensinogen measured in this study are low (1 to 6 nmol/d) compared with the circulating concentrations of angiotensinogen (800 to 1000 pmol/mL), suggesting the possibility that urinary angiotensinogen is derived from circulatory angiotensinogen. However, previous studies have suggested that angiotensinogen excreted into urine reflects the intrarenal production of this protein rather than filtered angiotensinogen.22 There is evidence that angiotensinogen is not filtered across the glomerular membrane because of the size of circulating angiotensinogen (60 to 65 kDa) and that urinary angiotensinogen is of proximal tubular cell origin.23-25 Some of degraded angiotensinogen in plasma may be filtered in the glomerulus, and, therefore, urine samples may include degradated fragments of angiotensinogen. However, our AngI RIA method for the measurement of urinary angiotensinogen detects only intact angiotensinogen containing the AngI peptide. To address this issue more directly, we performed experiments in which human angiotensinogen was infused intravenously into both sham-operated normotensive and AngII-infused hypertensive rats. As described in the Table, rat angiotensinogen and human angiotensinogen have a similar structure and an equivalent molecular size, but rat renin is species-specific and cannot cleave human angiotensinogen;26 therefore, human angiotensinogen is inactive in the rat. Indeed, administration of human angiotensinogen did not alter arterial BP or urine flow in either sham-operated or AngII-infused hypertensive rats. Although we could clearly detect human angiotensinogen in the plasma, we were not able to detect any trace of human angiotensinogen in the urine of either control or AngII-infused rats, indicating that circulating angiotensinogen is not excreted in the urine of either control or AngII-infused rats. The failure to detect human angiotensinogen in the urine supports limited glomerular permeability and/or tubular degradation of filtered angiotensinogen. Therefore, the results support the hypothesis that urinary angiotensinogen originates from the kidney and not the plasma.
In the previous paper by Von Thun et al,27 it was reported that 40 ng/min of AngII infusions for 2 weeks in uninephrectomized rats failed to show significant increases in renal or hepatic expression of angiotensinogen mRNA assessed by Northern blot analysis in a limited number (n=4) of rats. Thus, in that study performed in a small number of animals, the lower dose of AngII infusion was not sufficient to induce statistically significant augmentation of renal and/or hepatic expression of angiotensinogen. In a more recent study, however, we reported that 80 ng/min of AngII infusions for 2 weeks evoked significant increases in renal and hepatic expression of angiotensinogen mRNA2 assessed using reverse transcription-polymerase chain reaction. The present study is an extension of this more recent report and shows that 80 ng/min of AngII infusions significantly increases urinary excretion of angiotensinogen. Thus, the current study differs from that of Von Thun27 in that the rats were not nephrectomized and a higher dose of AngII was used to obtain statistically significant elevations in renal and urinary angiotensinogen levels.
We and other investigators have previously shown that AngII, both in vivo and in vitro, elicits enhanced kidney angiotensinogen mRNA expression and protein levels.1,2,11,28 Studies have demonstrated that AngII type I receptor blockade markedly reduces the increased intrarenal AngII that develops with chronic AngII infusions8 and the increased angiotensinogen mRNA by AngII exposure in immortalized rat proximal tubular cells.28 The current study was not designed to address the role of the AngII type I receptor in the regulation of renal and urinary angiotensinogen levels. Future studies will examine the effect of AngII type 1 receptor antagonists on kidney angiotensinogen mRNA expression and protein levels, as well as urinary angiotensinogen excretion rates in AngII-infused rats.
Although we did not directly examine intrarenal angiotensinogen formation in this study, we and others have previous shown that (1) angiotensinogen is not filtered across the glomerular membrane,23-25 (2) renal angiotensinogen mRNA and protein are predominantly expressed and localized in proximal tubule cells,2,12-18 (3) chronic AngII infusion results in significant increases in renal expression of angiotensinogen protein,1 as well as angiotensinogen mRNA,1,2,11 which is associated with an augmented urinary excretion of angiotensinogen in AngII-infused rats.3 Collectively, the data support the hypothesis that intrarenal angiotensinogen formation is responsible for the augmented urinary angiotensinogen excretion rates.
Perspectives
This study demonstrates that chronic AngII infusions to normal rats significantly increased urinary excretion of angiotensinogen in a time- and dose-dependent manner that was associated with elevation in kidney AngII levels. Urine excretion of angiotensinogen was closely correlated with systolic BP and kidney AngII content, but not with plasma AngII concentration. In contrast, hypertension elicited with a combination of high-salt diet and deoxycorticosterone acetate salt pellet was not associated with increased urinary angiotensinogen excretion rates, even though there was an increase in urinary excretion of total protein. These data indicate that urinary excretion of angiotensinogen reflects intrarenal angiotensinogen levels and may provide a useful method for detecting enhanced intrarenal AngII activity in the absence of elevated systemic renin or AngII concentrations. Together with our previous findings showing that AngII infusions increased renal angiotensinogen mRNA and protein levels, the data support the hypothesis that urinary excretion of angiotensinogen provides a specific index of intrarenal AngII production in AngII-dependent hypertension. To the extent that this hypothesis is shown to be applicable to human subjects, a diagnostic test that would identify those hypertensive patients most likely to respond to drugs that block the actions of the renin-angiotensin system could provide information to allow a mechanistic rationale for selecting an optimized approach to treatment.
Acknowledgments
This work was supported by a National Heart, Lung, and Blood Institute grant (HL26371) and by a Health Excellence Fund from the Louisiana Board of Regents. H.K. is a recipient of fellowships from the National Kidney Foundation and the Uehara Memorial Foundation. A.N. is a recipient of a grant-in-aid for scientific research from the Ministry of Education, Science and Culture of Japan. L.M.H.-B. is a recipient of a Scientific Development Grant from the American Heart Association. The polyclonal antibody against rat angiotensinogen was generously provided by Conrad Sernia, PhD (University of Queensland, Australia).
References
- 1.Kobori H, Harrison-Bernard LM, Navar LG. Enhancement of angiotensinogen expression in angiotensin II-dependent hypertension. Hypertension. 2001;37:1329–1335. doi: 10.1161/01.hyp.37.5.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobori H, Harrison-Bernard LM, Navar LG. Expression of angiotensinogen mRNA and protein in angiotensin II-dependent hypertension. J Am Soc Nephrol. 2001;12:431–439. doi: 10.1681/asn.v123431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kobori H, Harrison-Bernard LM, Navar LG. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney Int. 2002;61:579–585. doi: 10.1046/j.1523-1755.2002.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ding Y, Davisson RL, Hardy DO, Zhu LJ, Merrill DC, Catterall JF, Sigmund CD. The kidney androgen-regulated protein promoter confers renal proximal tubule cell-specific and highly androgen-responsive expression on the human angiotensinogen gene in transgenic mice. J Biol Chem. 1997;272:28142–28148. doi: 10.1074/jbc.272.44.28142. [DOI] [PubMed] [Google Scholar]
- 5.Yoshiya M, Tsutsui Y, Itoh N, Okamoto H. Angiotensinogen excretion in rat urine: effects of lipopolysaccharide treatment and sodium balance. Jpn J Pharmacol. 1991;57:37–44. doi: 10.1254/jjp.57.37. [DOI] [PubMed] [Google Scholar]
- 6.Fox J, Guan S, Hymel AA, Navar LG. Dietary Na and ACE inhibition effects on renal tissue angiotensin I and II and ACE activity in rats. Am J Physiol. 1992;262:F902–909. doi: 10.1152/ajprenal.1992.262.5.F902. [DOI] [PubMed] [Google Scholar]
- 7.Von Thun AM, Vari RC, El-Dahr SS, Navar LG. Augmentation of intrarenal angiotensin II levels by chronic angiotensin II infusion. Am J Physiol. 1994;266:F120–F128. doi: 10.1152/ajprenal.1994.266.1.F120. [DOI] [PubMed] [Google Scholar]
- 8.Zou LX, Hymel A, Imig JD, Navar LG. Renal accumulation of circulating angiotensin II in angiotensin II-infused rats. Hypertension. 1996;27:658–662. doi: 10.1161/01.hyp.27.3.658. [DOI] [PubMed] [Google Scholar]
- 9.Nishiyama A, Seth DM, Navar LG. Renal interstitial fluid concentrations of angiotensins I and II in anesthetized rats. Hypertension. 2002;39:129–134. doi: 10.1161/hy0102.100536. [DOI] [PubMed] [Google Scholar]
- 10.Tewksbury DA, Tryon ES. Immunochemical comparison of high molecular weight angiotensinogen from amniotic fluid, plasma of men, and plasma of pregnant women. Am J Hypertens. 1989;2:411–413. doi: 10.1093/ajh/2.5.411. [DOI] [PubMed] [Google Scholar]
- 11.Schunkert H, Ingelfinger JR, Jacob H, Jackson B, Bouyounes B, Dzau VJ. Reciprocal feedback regulation of kidney angiotensinogen and renin mRNA expressions by angiotensin II. Am J Physiol. 1992;263:E863–E869. doi: 10.1152/ajpendo.1992.263.5.E863. [DOI] [PubMed] [Google Scholar]
- 12.Rohrwasser A, Morgan T, Dillon HF, Zhao L, Callaway CW, Hillas E, Zhang S, Cheng T, Inagami T, Ward K, Terreros DA, Lalouel JM. Elements of a paracrine tubular renin-angiotensin system along the entire nephron. Hypertension. 1999;34:1265–1274. doi: 10.1161/01.hyp.34.6.1265. [DOI] [PubMed] [Google Scholar]
- 13.Davisson RL, Ding Y, Stec DE, Catterall JF, Sigmund CD. Novel mechanism of hypertension revealed by cell-specific targeting of human angiotensinogen in transgenic mice. Physiol Genomics. 1999;1:3–9. doi: 10.1152/physiolgenomics.1999.1.1.3. [DOI] [PubMed] [Google Scholar]
- 14.Richoux JP, Cordonnier JL, Bouhnik J, Clauser E, Corvol P, Menard J, Grignon G. Immunocytochemical localization of angiotensinogen in rat liver and kidney. Cell Tissue Res. 1983;233:439–451. doi: 10.1007/BF00238309. [DOI] [PubMed] [Google Scholar]
- 15.Ingelfinger JR, Zuo WM, Fon EA, Ellison KE, Dzau VJ. In situ hybridization evidence for angiotensinogen messenger RNA in the rat proximal tubule. An hypothesis for the intrarenal renin angiotensin system. J Clin Invest. 1990;85:417–423. doi: 10.1172/JCI114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Terada Y, Tomita K, Nonoguchi H, Marumo F. PCR localization of angiotensin II receptor and angiotensinogen mRNAs in rat kidney. Kidney Int. 1993;43:1251–1259. doi: 10.1038/ki.1993.177. [DOI] [PubMed] [Google Scholar]
- 17.Darby IA, Congiu M, Fernley RT, Sernia C, Coghlan JP. Cellular and ultrastructural location of angiotensinogen in rat and sheep kidney. Kidney Int. 1994;46:1557–1560. doi: 10.1038/ki.1994.445. [DOI] [PubMed] [Google Scholar]
- 18.Darby IA, Sernia C. In situ hybridization and immunohistochemistry of renal angiotensinogen in neonatal and adult rat kidneys. Cell Tissue Res. 1995;281:197–206. doi: 10.1007/BF00583388. [DOI] [PubMed] [Google Scholar]
- 19.Harrison-Bernard LM, Navar LG, Ho MM, Vinson GP, El-Dahr SS. Immunohistochemical localization of ANG II AT1 receptor in adult rat kidney using a monoclonal antibody. Am J Physiol. 1997;273:F170–F177. doi: 10.1152/ajprenal.1997.273.1.F170. [DOI] [PubMed] [Google Scholar]
- 20.Gavras H, Brunner HR, Laragh JH, Vaughan ED, Jr, Koss M, Cote LJ, Gavras I. Malignant hypertension resulting from deoxycorticosterone acetate and salt excess: Role of renin and sodium in vascular changes. Circ Res. 1975;36:300–309. doi: 10.1161/01.res.36.2.300. [DOI] [PubMed] [Google Scholar]
- 21.Somers MJ, Mavromatis K, Galis ZS, Harrison DG. Vascular superoxide production and vasomotor function in hypertension induced by deoxycorticosterone acetate-salt. Circulation. 2000;101:1722–1728. doi: 10.1161/01.cir.101.14.1722. [DOI] [PubMed] [Google Scholar]
- 22.Wang E, Yayama K, Takano M, Okamoto H. Sexual dimorphism of urine angiotensinogen excretion in the rat. Jpn J Pharmacol. 1994;64:243–250. doi: 10.1254/jjp.64.243. [DOI] [PubMed] [Google Scholar]
- 23.Navar LG, Harrison-Bernard LM, Nishiyama A, Kobori H. Regulation of intrarenal angiotensin II in hypertension. Hypertension. 2002;39:316–322. doi: 10.1161/hy0202.103821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lantelme P, Rohrwasser A, Gociman B, Hillas E, Cheng T, Petty G, Thomas J, Xiao S, Ishigami T, Herrmann T, Terreros DA, Ward K, Lalouel JM. Effects of dietary sodium and genetic background on angiotensinogen and renin in mouse. Hypertension. 2002;39:1007–1014. doi: 10.1161/01.hyp.0000016177.20565.a0. [DOI] [PubMed] [Google Scholar]
- 25.Tewksbury D. Angiotensinogen. In: Fray JCS, editor. The Endocrine System: Endocrine Regulation of Water and Electrolyte Balance: Handbook of Physiology. 1st ed. Oxford University Press; Oxford, UK: 2000. pp. 59–80. Section 7. [Google Scholar]
- 26.Fukamizu A, Sugimura K, Takimoto E, Sugiyama F, Seo MS, Takahashi S, Hatae T, Kajiwara N, Yagami K, Murakami K. Chimeric renin-angiotensin system demonstrates sustained increase in blood pressure of transgenic mice carrying both human renin and human angiotensinogen genes. J Biol Chem. 1993;268:11617–11621. [PubMed] [Google Scholar]
- 27.Von Thun AM, El-Dahr SS, Vari RC, Navar LG. Modulation of renin-angiotensin and kallikrein gene expression in experimental hypertension. Hypertension. 1994;23:I131–I136. doi: 10.1161/01.hyp.23.1_suppl.i131. [DOI] [PubMed] [Google Scholar]
- 28.Ingelfinger JR, Jung F, Diamant D, Haveran L, Lee E, Brem A, Tang SS. Rat proximal tubule cell line transformed with origin-defective SV40 DNA: Autocrine ANG II feedback. Am J Physiol. 1999;276:F218–F227. doi: 10.1152/ajprenal.1999.276.2.F218. [DOI] [PubMed] [Google Scholar]


