Abstract
Introduction. Laparoscopic cholecystectomy has become the gold standard for symptomatic cholelithiasis 1. Traditionally done through four ports, three and two port surgeries have been described. We present a novel technique of single port cholecystectomy using the R-PortR (Advanced Surgical Concepts). Materials and methods. The R-PortR is a Tri-port that allows the ingress of three 5 mm instruments through a single port. Twenty patients with symptomatic cholelithiasis were subjected to single port cholecystectomy using the R-PortR through the umbilicus. Two patients also had choledocholithiasis. Modified instruments with angulated shafts were used for the surgery. A telescope with a coaxial light cable was also used. Whenever necessary, an extra needle for retraction or an additional 5 mm port was used. Results. Single port laparoscopic was accomplished in 17 of the 20 patients. In one patient an additional port was used for the cholecystectomy and in two others it was used for the common bile duct exploration but not for the dissection of Calot's triangle. Of the 17 patients, seven needed a single needle to retract the fundus of the gall bladder. Conclusions. Single port laparoscopic cholecystectomy is feasible and safe using the R-Port. The level of difficulty is higher and a needle for retraction or an additional port may be used whenever the visualization of Calot's triangle is unsatisfactory. Further studies and the development of better instrumentation are necessary before this can be recommended as a standard procedure.
Keywords: single port, laparoscopy, cholecystectomy
Introduction
Laparoscopic cholecystectomy is now accepted as the gold standard for the treatment of symptomatic cholelithiasis 1. Traditionally, laparoscopic cholecystectomy has been performed with four ports either using the American or the French technique 2,3. There has been a trend toward minimizing the number of incisions and ports required and this has led to the description of three and two port techniques of laparoscopic cholecystectomy 4,5,6. The regular laparoscopic ports work on the principle of one instrument per port and this has limited the reduction of ports in a laparoscopic cholecystectomy. The development of various ports like the Uni-X™ (Pnavel systems, NJ, USA), and the R-PortR (Advanced Surgical Concepts, Wicklow, Ireland) allows the introduction of multiple instruments through a single port inserted at the umbilicus. This has made single port laparoscopy feasible. We report the first few cases of laparoscopic cholecystectomy attempted using the R-Port single port through a single umbilical incision in a pilot series of 20 cases.
Materials and methods
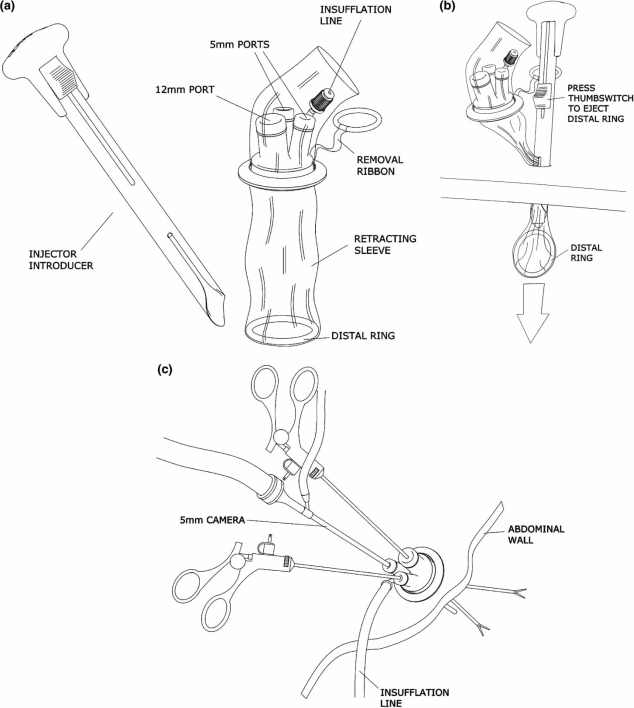
The R-port® (Advanced Surgical Concepts, Wicklow, Ireland) consists of an external disc which has three valves with a gel interface, which fits on to a double-layered plastic cylinder which serves as the common channel or a single port (Figure 1). The plastic cylinder when deployed is held in place by an inner ring very much like a miniature hand port (Figure 1). Three separate valves on the ring allow insertion of one 10 mm and one 5 mm or three 5 mm instruments at any given time. It has a separate insufflation valve. The port is introduced using an introducer through an incision in the umbilicus. The diagrammatic representation of the port and insertion are shown in Figure 7(a–c). The size of the incision can be anything from 15 to 25 mm. The plastic sleeve expands to fill the incision, held in place by the insufflating gas. The larger the incision, the more the play between the instruments. We used a 20 mm incision in our cases (Figure 4).
Figure 1. .
Insertion of the R-Port through the umbilicus.
Figure 7. .
(a) Graphic representation of the R-Port components; (b) graphic representation of the R-Port deployment; and (c) graphic representation of the R-Port in situ.
Figure 4. .
Scar at the end of the surgery.
Twenty patients presenting at a single private practice with symptomatic cholelithiasis and consenting to undergo single port surgery between May 2007 and December 2007 were studied. Patients presenting with severe acute attacks of cholecystitis or with prior or history of pancreatitis were excluded from the study. Two of these patients also had choledocholithiasis. Appropriate consents were taken from the patients and the hospital ethics committee.
The R-port R was inserted at the umbilicus through a 20 mm incision going through the umbilicus for added cosmesis. A 5 mm telescope with a coaxial light cable, the Endo EyeR (Olympus, Japan) was used with a standard laparoscopic set. The standard 5 mm clip applier was used in case of all cystic arteries and whenever possible for narrow ducts. A modified clip applier with a 10 mm jaws and a 5 mm shaft was used for larger ducts. Modified curved graspers and dissectors were used to give the feeling of triangulation during dissection (Figure 2). Dissection was carried out using the Ultracision® or/and the monopolar hook and whenever required, the bipolar forceps was used for hemostasis.
Figure 2. .
Grasper with an angulated shaft.
In the two patients with choledocholithiasis, a second R-port® was used to insert the choledochoscope to remove the common bile duct (CBD) stone, but the major dissection of the Calot's triangle for the cholecystectomy was achieved through the single umbilical port. The second port in these two cases was inserted in line with the CBD in the epigastrium.
Standard steps followed in all cases included retraction of the gall bladder at either the fundus or Hartmann's pouch or in between (a single 5 mm grasper used for both); exposure of Calot's triangle with separate clipping and division of cystic artery and cystic duct; separation of gall bladder from liver; removal of specimen and port together by simply pulling on the removal ribbon attached to the inner ring. If the exposure at Calot's triangle was found to be inadequate, and safety of the dissection in doubt, a port closure needle or an additional port was used to retract the fundus.
Results
There were 16 female and four male patients. Age ranged from 23 to 67 years.
All the surgeries were uneventful. One port umbilicus surgery (OPUS), in this case laparoscopic cholecystectomy, was successfully performed in 17 of the 20 patients. In 10 cases no additional ports or instrumentation was needed to finish the cholecystectomy. In seven other cases, a port closure needle was used to retract the fundus. Ironically, it was the so-called “simpler” gall bladders that required two-point traction, as they were very long and “floppy” in nature. In such gall bladders, retraction of the fundus may not make perceptible change in the position of the Hartmann's pouch. The chronic contracted or the short gall bladders with thick walls could be better retracted by a single point of mid gall bladder traction. In one of our earlier cases, an extra 5 mm port was placed at the epigastrium. The port closure needle was used when the visualization of the Calot's triangle was difficult, in our later cases, obviating the need for an extra port. The additional needle or a stitch to hold up organs is frequently used in natural orifice transluminal endoscopic surgery (NOTES) and was not considered an additional port 9.
The operating times ranged from 19 to 100 min for the cholecystectomies with an average of 40 min. The CBD explorations took 90 and 240 min, respectively. The latter being due to an impacted calculus, which ultimately had to be pulverized using the Holmium LASER, after prolonged instrumentation. No drains were inserted except for the CBD explorations. Blood loss was minimal and ranged from 50 to 100 cm3. All patients of cholecystectomy were discharged on the next day. The bile duct explorations stayed for 72 hours in keeping with our policy of discharging after drain removal.
There were no conversions to three or four port or open surgery. There was no wound infection. There was no mortality. In two patients additional ports were inserted for the choledochoscope and we had the benefit of this additional port for gall bladder removal from the fossa. Only in one patient early in our series, was it necessary to put an additional 5 mm port and the surgery was converted to a two-port cholecystectomy.
The analgesic requirements were diclofenac 50 mg three times a day for 48–72 h post procedure, which was less than that required in our experience, for our four port cholecystectomy, even though this was not a comparative study.
The scars receded into the umbilicus and were hardly visible.
Discussion
Laparoscopic cholecystectomy is now accepted as the gold standard for the treatment of symptomatic cholelithiasis (1) what was anecdotal in 1985 (2) has now evolved into a well-described, easily reproducible technique. Traditionally, laparoscopic cholecystectomy has been performed with four ports either using the American or the French technique 2,3. Trend has been toward minimizing the number of incisions and ports required and this has led to the description of three and two port techniques of laparoscopic cholecystectomy 4,5,6. Minimizing scars and the quest for the “No Scar” surgery has spurred on the development of NOTES and natural orifice surgery (NOS) and billions of dollars are being poured into research in this direction. Traditionally, laparoscopic ports work on the principle of one instrument per port and this has limited the reduction in ports during a laparoscopic cholecystectomy. The development of various ports has allowed the introduction of multiple instruments through a single port inserted at the umbilicus. These are the first reported cases of cholecystectomy using a novel single port through a single incision. The initial cases presented three problems, which were surmounted by modification of instruments and using different equipments.
The instruments entering through a single port led to clashing of instruments and the so-called “chopsticks effect” (Figure 3). There was absolute loss of triangulation. This was minimized in our later cases by using modified graspers and dissectors angulated at the shaft.The instruments initially clashed with the tangential light cable on the telescope. This difficulty was overcome using the EndoEye ® which has a coaxial light cable.The third difficulty we encountered was inserting a 10 mm clip applier for larger ducts. The nature of the Tri-port allows the ingress of only three 5 mm instruments or one 5 mm and one 10 mm instrument at any given time. We used a modified clip applier having a 5 mm shaft and 10 mm jaws. This enabled us to insert the jaws of the applier with only the telescope in place and then insert the retracting grasper.
Figure 3. .
“Chopsticks effect” of instruments going in through a single port.
We report the first few cases of laparoscopic cholecystectomy done using this single port through a single umbilical incision in a pilot series of 20 cases (Figure 4). The single port procedure has been used for various urological procedures in studies 7,8. Inserting the two operating instruments and the telescope through the same port appear to negate the principles of triangulation that are embedded in our mind in laparoscopy. However, the instruments can diverge due to the flexibility of these valves externally and the low profile of the port which remains flush with the parietes on the inside and outside. This allows the insertion of instruments with angulated shafts. The angulated shafts give the effect of triangulation as the instruments diverge to zero in on the same organ. The flat profile of the port also allows free play of the instruments in spite of their proximity to each other. A gel allows ingress and egress of instruments without loss of pneumoperitoneum, during multiple entries. As the port is made of non-rigid materials it allows retrieval of specimen and serves as a plastic wound cover, giving an added advantage. Single port surgery was feasible in 17 out of 20 (85%) of the patients. In an additional two patients, the CBD exploration port was present and hence used for fossa dissection but not for the initial Calot's triangle dissection. The addition of a needle was not considered as a deviation from the single port as it required only a puncture and not an incision. This is frequently used by surgeons doing the NOTES procedures 9.
The quest for scarless surgery has driven endoscopists and surgeons alike to NOTES, but NOTES has its inherent problems. The procedure of single port cholecystectomy provides the same benefit of scarless surgery as the incision is well hidden in the umbilical cicatrix, which in itself is an embryological natural orifice making us wonder whether this should be termed as E- NOTES or E- NOS. The scars receded into the umbilicus and were invisible after six weeks making this virtually a scarless surgery (Figure 5).
Figure 5. .
Three weeks post operatively – A “No Scar” surgery.
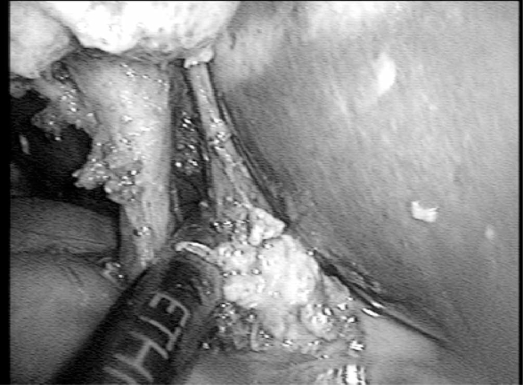
It is easier for the surgeon to adapt to, rather than NOTES, since the view and set-up through the umbilicus is the same. The instruments are simple and inexpensive modifications of existing laparoscopic instruments and there is no need for expensive delicate endoscopic instruments. Furthermore, it uses a conventional camera and there is no need for multi-channel endoscopes. There are, however, some concerns. The loss of retraction and triangulation may mean suboptimal exposure of Calot's triangle in some cases. Hence it is not recommended for “difficult” laparoscopic cholecystectomies until more experience with this procedure is gained. In our series we deliberately avoided the predictably difficult gall bladders presenting with severe acute cholecystitis and abdominal signs. Furthermore, the difficulty level is far more than a standard laparoscopic cholecystectomy, making it unsuitable presently for the beginner. The single port procedure may give less than adequate visualization of the Calots in some cases and in these it would be wise to add a needle in the right hypochondriac region for fundus or liver retraction. In most cases it is possible to get good dissection and visualization of the Calot's triangle as seen in this intraoperative picture (Figure 6). It would be possible to start of as a single port procedure and add extra needles or ports for retraction as and when required. Improved instrumentation and the use of articulating graspers and dissectors may further decrease the difficulty level. It also remains to be seen if the myriad articulations of the Robotic arms would better suit a single port procedure. Other than the obvious cosmetic advantage, studies are needed to see whether this can bring down the pain scores and the analgesic requirements in comparison to the standard four port laparoscopic cholecystectomy.
Figure 6. .
Dissection of the cystic duct triangle.
Conclusion
Single port cholecystectomy is safe using the RPort® and possible in most cases of cholelithiasis. An additional needle for retraction may and should be used whenever visualization of the Calots triangle is suboptimal. Additional ports are rarely required. It appears to be cosmetically superior to standard laparoscopic cholecystectomy. It makes no new scars, uses an existing scar (umbilicus), which is an embryological natural orifice. It uses standard laparoscopic instruments with a few simple modifications. It may offer an acceptable alternative to NOTES, as it is the more logical next step for a laparoscopic surgeon. More studies and larger series are needed to determine whether this can be recommended as a standard and reproducible procedure.
References
- 1.Begos DG, Modlin IM. LC: from gimmick to gold standard. J Clin Gast. 1994;19(4):325–30. doi: 10.1097/00004836-199412000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Cuschieri A, Dubois F, Mouiel J, Mouret P, Becker H, Buess G, et al. The European experience with laparoscopic cholecystectomy. Ann J Surg. 1991;161:385–7. doi: 10.1016/0002-9610(91)90603-b. [DOI] [PubMed] [Google Scholar]
- 3.Giacomo U, Alfonso MM, Gioacchino C, Gaspere G, David B, Arianna CS. Laparoscopic cholecystectomy: European position versus American position. Revista de Ciência de Saúde de Macau. 2002;2(1 & 2):32–4. [Google Scholar]
- 4.Kagaya T. Laparoscopic cholecystectomy via two ports, using the “Twin-Port” system. J Hepatobiliary Pancreat Surg. 2001;8(1):76–80. doi: 10.1007/s005340170053. [DOI] [PubMed] [Google Scholar]
- 5.Trichak S. 3 port v/s 4 port cholecystectomy. Surg Endosc. 2003;17(9):1434–36. doi: 10.1007/s00464-002-8713-1. [DOI] [PubMed] [Google Scholar]
- 6.Poon CM, Chan KW, Lee DW, Chan KC, Ko CW, Cheung HY.Cheung HY Surg Endosc 2003;17 (10): 1624–7. [DOI] [PubMed] [Google Scholar]
- 7.Desai MM, Rao PP, Aron M, Pascal- Haber G, Desai MR, Mishra S, et al. Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int. 2008;101(1):83–8. doi: 10.1111/j.1464-410X.2007.07359.x. [DOI] [PubMed] [Google Scholar]
- 8.Kaouk JH, Haber GP, Goel RK, Desai MM, Aron M, Rackley RR, et al. Single-port laparoscopic surgery in urology: initial experience. Urology. 2008;71(1):3–6. doi: 10.1016/j.urology.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 9.Meining A, Wilhelm D, Burian M, Dundalakis M, Schneder A, von Delius S, et al. Development, standardization, and evaluation of NOTES cholecystectomy using a transsigmoid approach in the porcine model: an acute feasibility study. Endoscopy. 2007;39(10):860–4. doi: 10.1055/s-2007-966904. [DOI] [PubMed] [Google Scholar]