Abstract
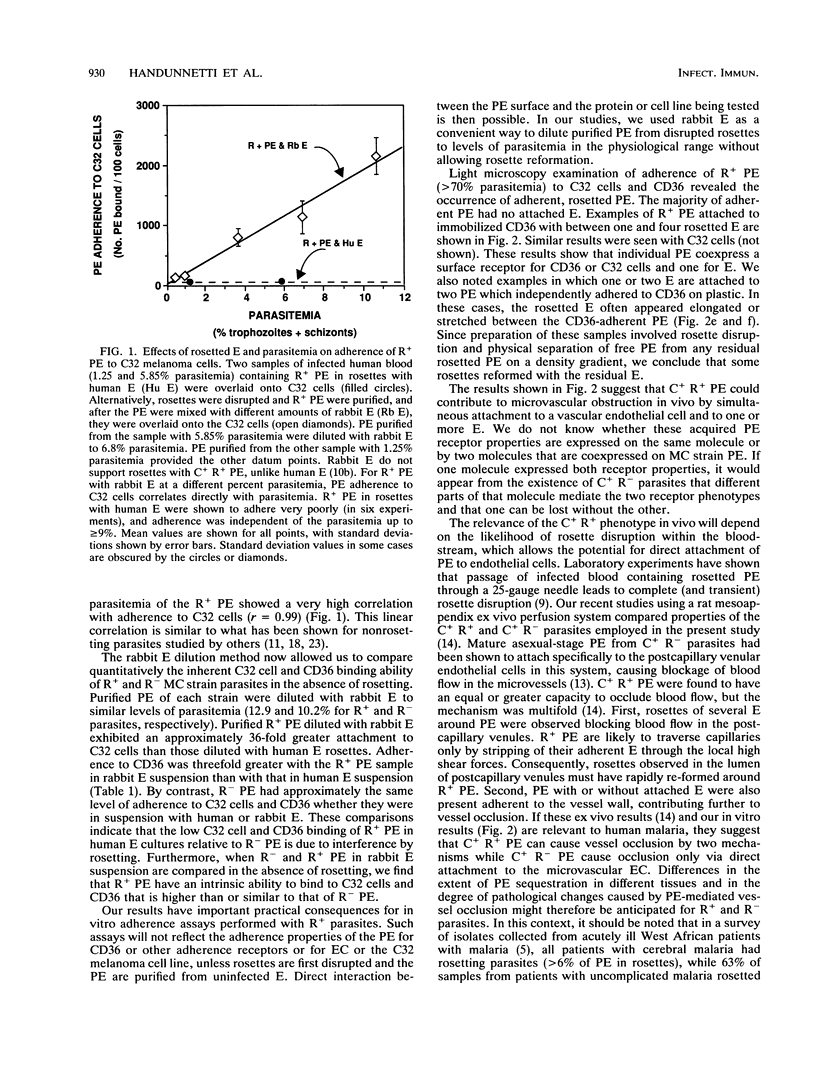
Plasmodium falciparum malaria parasites modify the human erythrocytes in which they grow so that some parasitized erythrocytes (PE) can cytoadhere (C+) to host vascular endothelial cells or adhere in rosettes (R+) to uninfected erythrocytes. These C+ and R+ adherence properties of PE appear to mediate much of the pathogenesis of severe malaria infections, in part by blocking blood flow in microvessels. From one parasite strain, PE were selected in vitro for C+ R+ or C+ R- adherence properties and examined in model adherence assays. The C+ R+ PE cytoadhered poorly to C32 melanoma cells or to immobilized CD36 in a settled-cell assay when uninfected human erythrocytes were present and formed rosettes with PE. C+ R- PE adhered well in the same assays. However, C+ R+ PE adhered very well, even better than C+ R- PE, when the rosettes were disrupted and the C+ R+ PE were purified. Adding back rabbit erythrocytes, which do not form rosettes with C+ R+ PE, had simply a dilutional effect. The ability of rosettes to interfere with the detection of adherence must be dealt with in all future assays of malarial PE adherence. Individual PE were observed attached simultaneously to C32 cells and to a few erythrocytes, suggesting that C+ and R+ adherence properties are coexpressed on the same PE. Coexpression of these adherence properties on the same PE may have pathological importance in vivo, where passage of rosettes through capillaries may shear uninfected erythrocytes from rosetted PE and allow direct PE attachment to postcapillary venule walls before rosettes reform.
Full text
PDF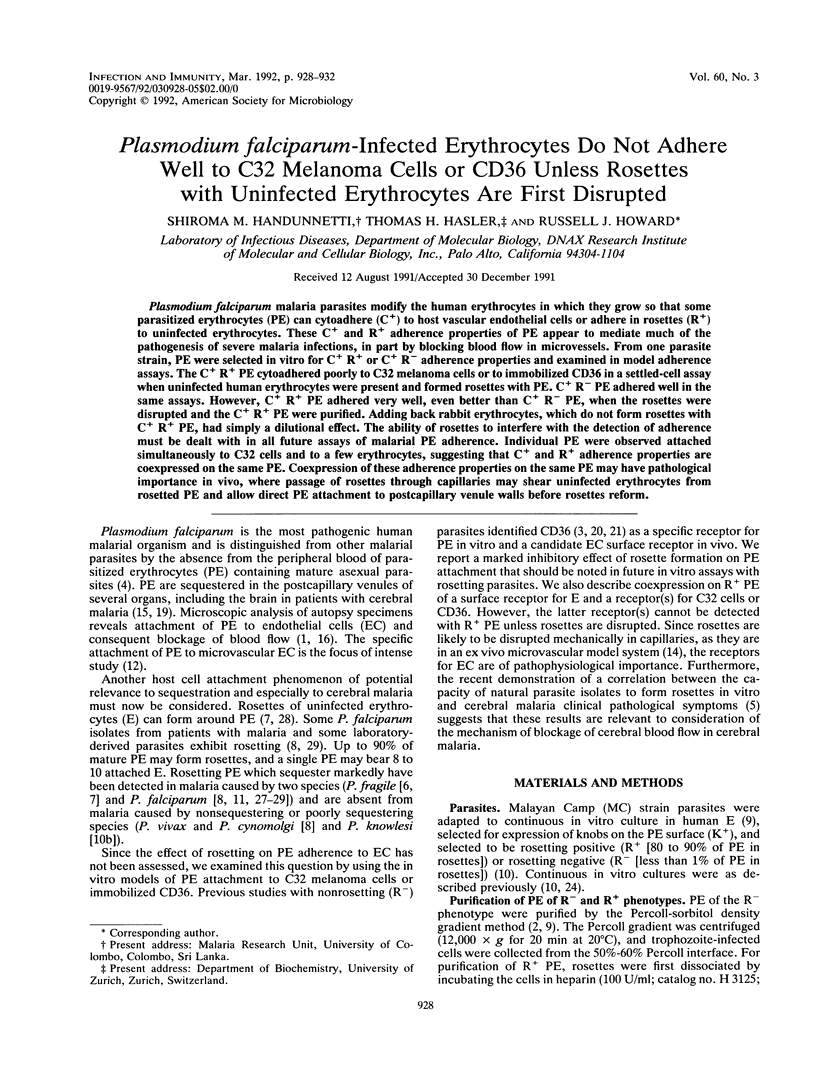

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aikawa M. Human cerebral malaria. Am J Trop Med Hyg. 1988 Jul;39(1):3–10. doi: 10.4269/ajtmh.1988.39.3. [DOI] [PubMed] [Google Scholar]
- Aley S. B., Barnwell J. W., Daniel W., Howard R. J. Identification of parasite proteins in a membrane preparation enriched for the surface membrane of erythrocytes infected with Plasmodium knowlesi. Mol Biochem Parasitol. 1984 May;12(1):69–84. doi: 10.1016/0166-6851(84)90045-8. [DOI] [PubMed] [Google Scholar]
- Barnwell J. W., Asch A. S., Nachman R. L., Yamaya M., Aikawa M., Ingravallo P. A human 88-kD membrane glycoprotein (CD36) functions in vitro as a receptor for a cytoadherence ligand on Plasmodium falciparum-infected erythrocytes. J Clin Invest. 1989 Sep;84(3):765–772. doi: 10.1172/JCI114234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson J., Helmby H., Hill A. V., Brewster D., Greenwood B. M., Wahlgren M. Human cerebral malaria: association with erythrocyte rosetting and lack of anti-rosetting antibodies. Lancet. 1990 Dec 15;336(8729):1457–1460. doi: 10.1016/0140-6736(90)93174-n. [DOI] [PubMed] [Google Scholar]
- David P. H., Handunnetti S. M., Leech J. H., Gamage P., Mendis K. N. Rosetting: a new cytoadherence property of malaria-infected erythrocytes. Am J Trop Med Hyg. 1988 Mar;38(2):289–297. doi: 10.4269/ajtmh.1988.38.289. [DOI] [PubMed] [Google Scholar]
- Handunnetti S. M., David P. H., Perera K. L., Mendis K. N. Uninfected erythrocytes form "rosettes" around Plasmodium falciparum infected erythrocytes. Am J Trop Med Hyg. 1989 Feb;40(2):115–118. doi: 10.4269/ajtmh.1989.40.115. [DOI] [PubMed] [Google Scholar]
- Hasler T., Handunnetti S. M., Aguiar J. C., van Schravendijk M. R., Greenwood B. M., Lallinger G., Cegielski P., Howard R. J. In vitro rosetting, cytoadherence, and microagglutination properties of Plasmodium falciparum-infected erythrocytes from Gambian and Tanzanian patients. Blood. 1990 Nov 1;76(9):1845–1852. [PubMed] [Google Scholar]
- Howard R. J., Gilladoga A. D. Molecular studies related to the pathogenesis of cerebral malaria. Blood. 1989 Dec;74(8):2603–2618. [PubMed] [Google Scholar]
- Kaul D. K., Raventos-Suarez C., Olson J. A., Nagel R. L. The role of membrane knobs in microvascular obstruction induced by Plasmodium falciparum-infected erythrocytes. Trans Assoc Am Physicians. 1985;98:204–214. [PubMed] [Google Scholar]
- Kaul D. K., Roth E. F., Jr, Nagel R. L., Howard R. J., Handunnetti S. M. Rosetting of Plasmodium falciparum-infected red blood cells with uninfected red blood cells enhances microvascular obstruction under flow conditions. Blood. 1991 Aug 1;78(3):812–819. [PubMed] [Google Scholar]
- Luse S. A., Miller L. H. Plasmodium falciparum malaria. Ultrastructure of parasitized erythrocytes in cardiac vessels. Am J Trop Med Hyg. 1971 Sep;20(5):655–660. [PubMed] [Google Scholar]
- MacPherson G. G., Warrell M. J., White N. J., Looareesuwan S., Warrell D. A. Human cerebral malaria. A quantitative ultrastructural analysis of parasitized erythrocyte sequestration. Am J Pathol. 1985 Jun;119(3):385–401. [PMC free article] [PubMed] [Google Scholar]
- Magowan C., Wollish W., Anderson L., Leech J. Cytoadherence by Plasmodium falciparum-infected erythrocytes is correlated with the expression of a family of variable proteins on infected erythrocytes. J Exp Med. 1988 Oct 1;168(4):1307–1320. doi: 10.1084/jem.168.4.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh K., Marsh V. M., Brown J., Whittle H. C., Greenwood B. M. Plasmodium falciparum: the behavior of clinical isolates in an in vitro model of infected red blood cell sequestration. Exp Parasitol. 1988 Apr;65(2):202–208. doi: 10.1016/0014-4894(88)90123-3. [DOI] [PubMed] [Google Scholar]
- Miller L. H. Distribution of mature trophozoites and schizonts of Plasmodium falciparum in the organs of Aotus trivirgatus, the night monkey. Am J Trop Med Hyg. 1969 Nov;18(6):860–865. doi: 10.4269/ajtmh.1969.18.860. [DOI] [PubMed] [Google Scholar]
- Ockenhouse C. F., Tandon N. N., Magowan C., Jamieson G. A., Chulay J. D. Identification of a platelet membrane glycoprotein as a falciparum malaria sequestration receptor. Science. 1989 Mar 17;243(4897):1469–1471. doi: 10.1126/science.2467377. [DOI] [PubMed] [Google Scholar]
- Oquendo P., Hundt E., Lawler J., Seed B. CD36 directly mediates cytoadherence of Plasmodium falciparum parasitized erythrocytes. Cell. 1989 Jul 14;58(1):95–101. doi: 10.1016/0092-8674(89)90406-6. [DOI] [PubMed] [Google Scholar]
- Schmidt J. A., Udeinya I. J., Leech J. H., Hay R. J., Aikawa M., Barnwell J., Green I., Miller L. H. Plasmodium falciparum malaria. An amelanotic melanoma cell line bears receptors for the knob ligand on infected erythrocytes. J Clin Invest. 1982 Aug;70(2):379–386. doi: 10.1172/JCI110627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood J. A., Roberts D. D., Marsh K., Harvey E. B., Spitalnik S. L., Miller L. H., Howard R. J. Thrombospondin binding by parasitized erythrocyte isolates in falciparum malaria. Am J Trop Med Hyg. 1987 Mar;36(2):228–233. doi: 10.4269/ajtmh.1987.36.228. [DOI] [PubMed] [Google Scholar]
- Trager W., Jensen J. B. Human malaria parasites in continuous culture. Science. 1976 Aug 20;193(4254):673–675. doi: 10.1126/science.781840. [DOI] [PubMed] [Google Scholar]
- Udeinya I. J., Graves P. M., Carter R., Aikawa M., Miller L. H. Plasmodium falciparum: effect of time in continuous culture on binding to human endothelial cells and amelanotic melanoma cells. Exp Parasitol. 1983 Oct;56(2):207–214. doi: 10.1016/0014-4894(83)90064-4. [DOI] [PubMed] [Google Scholar]
- Udeinya I. J., Schmidt J. A., Aikawa M., Miller L. H., Green I. Falciparum malaria-infected erythrocytes specifically bind to cultured human endothelial cells. Science. 1981 Jul 31;213(4507):555–557. doi: 10.1126/science.7017935. [DOI] [PubMed] [Google Scholar]
- Udomsangpetch R., Wåhlin B., Carlson J., Berzins K., Torii M., Aikawa M., Perlmann P., Wahlgren M. Plasmodium falciparum-infected erythrocytes form spontaneous erythrocyte rosettes. J Exp Med. 1989 May 1;169(5):1835–1840. doi: 10.1084/jem.169.5.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlgren M., Carlson J., Ruangjirachuporn W., Conway D., Helmby H., Martinez A., Patarroyo M. E., Riley E. Geographical distribution of Plasmodium falciparum erythrocyte rosetting and frequency of rosetting antibodies in human sera. Am J Trop Med Hyg. 1990 Oct;43(4):333–338. doi: 10.4269/ajtmh.1990.43.333. [DOI] [PubMed] [Google Scholar]