Abstract
Epilepsy and obstructive sleep apnea (OSA) are two relatively common disorders known to coexist and potentially exacerbate each other.1 Vagus nerve stimulation (VNS) is a currently used, adjunctive treatment for partial epilepsy and is generally well tolerated with few associated side effects. Some of the more common side effects include hoarseness of voice, laryngeal irritation and cough, especially after VNS current increases and the first few weeks of treatment. VNS therapy also affects respiration during sleep and has been shown to worsen preexisting obstructive sleep apnea/hypopnea syndrome (OSAHS) by increasing the number of apneas and hypopneas.2 Consistent sleep related decreases in airflow and effort coinciding with VNS activation have been documented, with apneas and hypopneas found to be more frequent during VNS activation than during nonactivation.2 VNS may also interfere with effective CPAP titration.
The purpose of this case study was to examine the effects of VNS cycling on CPAP titration for OSA in a patient with medically intractable epilepsy. We found that adequate CPAP titration could not be achieved in the presence of the patient's standard VNS on/off cycling mode. However, when the patient was restudied with his VNS device turned off, a nasal CPAP pressure of 13 cm H2O resulted in effective treatment of his severe OSAHS. We suggest that polysomnography before VNS implantation should be considered in order to identify patients with OSA.
Citation:
Ebben MR; Sethi NK; Conte M; Pollak CP; Labar D. Vagus nerve stimulation, sleep apnea, and CPAP titration. J Clin Sleep Med 2008;4(5):471–473.
Keywords: Apnea, epilepsy, CPAP, VNS
Vagus nerve stimulation (VNS) is an effective nonpharmacological treatment for patients with medically refractory partial onset seizure disorder. More than 50% reduction in seizure frequency rate is achieved in most patients.3 The effects of VNS on sleep were noted when patients with implanted VNS devices and obstructive sleep apnea/hypopnea syndrome (OSAHS) underwent polysomnographic studies. Malow and colleagues were among the first to highlight the frequent coexistence of sleep disordered breathing in patients treated with VNS for epilepsy. In their initial study, they found that patients with VNS had lower airflow and breathing effort after VNS devices were implanted. This was seen during almost every “on” cycle of the devices. Most of the breathing events, were not long lasting or severe enough to be classified as apneas or hypopneas. In follow-up of 2 patients, they found a decrease in apneas and hypopneas when the stimulus frequency was decreased, but not when the intensity, pulse width, or on-time was decreased. They commented that decreasing the stimulus frequency or lengthening the time between stimulations (off period) may reduce the number of these breathing events.4 Papacostas et al.5 recently presented evidence of VNS induction of central-type sleep apneas. They reported the case of a female patient with medically intractable epilepsy and an implanted VNS device who developed central-type apneas. Changing the VNS parameters resulted in resolution of these central breathing events and return of the sleep study back to normal.5
We describe a patient who presented with sleep disordered breathing, but whose highly medication-resistant epilepsy had improved so dramatically on VNS that we were reluctant to change the chronic stimulation settings. Instead, we modified our CPAP titration for this case, and report the results of that approach.
CASE REPORT
A 54-year-old male, BMI = 39 kg/m,2 was referred by his epileptologist for a neurological sleep consultation. The patient had a history of medically refractory partial epilepsy for which he had a VNS device implanted in 1998. The device (Cyberonics, Inc. Model # 102) was set to a rapid-cycling mode (current: 1.75 mA, frequency: 30 Hz, pulse width: 500 μs, cycle: 7 sec on/12 sec off). Compared to pre-implantation seizure frequency (approximately 4 complex partial seizures/month, often with serious injuries), the patient was seizure-free at 6 months with the addition of VNS. Although we are aware that changing VNS parameters may improve sleep disordered breathing,4 we were reluctant to change the VNS because of the dramatic improvement of the patient's epilepsy. For patient safety reasons, instead we elected to evaluate and treat for sleep apnea. Sleep history was significant for loud snoring; he denied waking up with a choking or gasping sensation. His wife had never noticed him stop breathing during sleep. The patient typically woke up 1–2 times per night but had no difficulty going back to sleep. Upon awakening in the morning, he reported feeling alert; however, during the day he felt sleepy and usually took a nap lasting 2 h between 10:00 and 15:00. There was no history of anxiety or depression. The patient denied smoking and alcohol consumption, although he did consume 4–7 cups of caffeinated tea per day. His medications included phenytoin (400 mg/day) and Lotrel (amlodipine besylate and benazepril hydrochloride).
Baseline Polysomnogram with VNS On
A polysomnogram was scheduled to evaluate the possibility of sleep disordered breathing. The total study time was 8.3 h with a total sleep time of 4 h. Sleep efficiency was 54.4%. A total of 325 respiratory events occurred, with an apnea-hypopnea index (AHI) of 82.3/h. The lowest SpO2 recorded was 67%, and continuous loud snoring was noted. Total amount of REM sleep was 13.5 min. Nasal CPAP was recommended for treatment of the severe OSAHS.
CPAP Titration with VNS On
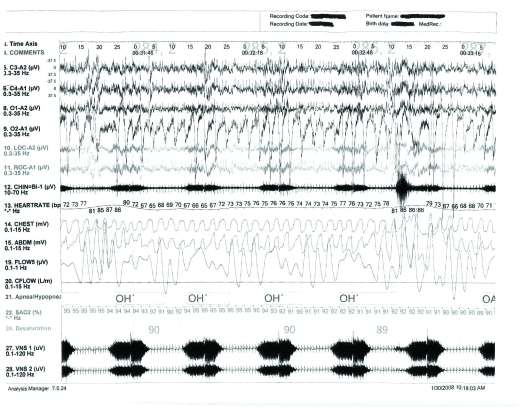
During the CPAP titration study, the total study time was 8.9 h with a total sleep time of 4.4 h. Sleep efficiency was 57.1%. At a CPAP pressure of 12 cm H2O, his AHI was reduced to 24/h, and the lowest SpO2 increased to 87%. It was difficult to titrate to pressures higher than 12 cm H2O because his sleep was so fragmented. A CPAP pressure of 13 cm H2O was attempted, but the patient was only able to sleep for 3 min at this pressure. At all CPAP pressure settings, the patient continuously had periods of reduction or cessation in the airflow signal which coincided with the on-cycling of VNS activity (see Fig. 1). For this reason, the patient was rescheduled for a split-night sleep study (half diagnostic and half treatment) with the VNS turned off.
Figure 1.
The reduction of airway flow associated with VNS stimulation (120-sec epoch). Channels 27 and 28 show the cycling of the VNS device. The events marked OH on channel 21 show obstructive hypopneas associated with VNS activation.
Figure 1 shows the reduction of airway flow associated with VNS stimulation (120-sec epoch). Channels 27 and 28 show the cycling of the VNS device. The events marked OH on channel 21 show obstructive hypopneas associated with VNS activation.
Split-Night Polysomnogram with VNS Off
The VNS was turned off 4 to 5 h before the start of the sleep study. Total amount of REM sleep was 10.5 min. On the baseline portion of this study, he had an AHI of 59/h. This AHI was significantly lower than that seen on his initial baseline study (with his VNS device cycle on), but was still severe. His lowest SpO2 was 67% (same as with VNS turned on). Sleep efficiency was 52%. On the titration portion of the study, we were able to titrate him to a pressure of 10 cm H2O. At this pressure, he slept for 139.5 min (including 14 min in REM sleep). AHI at this pressure was reduced to 0.4/h with a lowest SpO2 of 92%. His sleep efficiency, pooling all tested CPAP pressures, improved to 76%. Patient had no REM sleep on the baseline portion of the night. However, 35.5 mins of REM sleep was present during the CPAP portion of the study.
The day after this study, his VNS device was turned back on to its original values (current 1.75 mA, frequency 30 Hz, pulse width 500ms, time on 7 sec, time off 0.2 min, magnet current 1.75 mA, magnet time on 60 sec, and magnet pulse width 500ms), and he was instructed to begin using nasal CPAP at a pressure of 10 cm H2O on a nightly basis. After approximately 2 months of nightly CPAP use, he returned for a follow-up consultation. He reported feeling much more alert during the day, and he also reported losing 20 pounds. At that time he was scheduled for another CPAP titration with the VNS device on.
Retitration of CPAP with the VNS Cycle On
The results of the follow-up polysomnography with the VNS cycle on showed that at a CPAP pressure of 13 cm H2O. His AHI was reduced to 13/h, with a lowest SpaO2 of 94%. The patient was able to sleep for 91 min at this pressure including 16 min of REM sleep. His sleep efficiency, pooling all CPAP pressures tested on this study, was 80%. Total amount of REM sleep was 36 min.
DISCUSSION
Sleep apnea is a common condition, with an estimated prevalence of 4% in men and 2% in women.6 Sleep apnea and epilepsy are known to frequently coexist. VNS has been used as an adjunctive treatment in patients with epilepsy since 1997. Recently, it has also received FDA approval as treatment for medically resistant chronic depression. VNS therapy has been shown to worsen preexisting OSAHS by increasing the number of apneas and hypopneas.4,5,7–9 Apneas and hypopneas recorded during VNS activation are predominantly obstructive—effort is relatively preserved while airflow is diminished. Apneas and hypopneas occur more frequently during VNS activation than during nonactivation. Both central and peripheral mechanisms have been postulated. Stimulation of peripheral vagal afferents activates motor efferents with cell bodies in the dorsal motor nucleus of the vagus nerve and in the nucleus ambiguus. These efferents may alter neuromuscular transmission to the upper airway muscles of the pharynx and larynx producing upper airway narrowing and obstruction. VNS may also modulate central projections to the brainstem reticular formation altering the rate and depth of respiration. At relatively low current and frequency settings, VNS increases REM sleep, thereby predisposing the patient to apneas and hypopneas.7,8 However, a significant difference in REM sleep was not seen between the successful CPAP titrations with or without VNS (36 vs. 35.5 min) in our case.
With the increasing use of VNS as a treatment option, and the known association between VNS and sleep apnea, increased attention needs to be paid to effective ways of treating apnea in patients with comorbid epilepsy and OSAHS. Nasal CPAP remains the most effective treatment for OSAHS. It appears that for some patients at least, attempting nasal CPAP titration with the VNS turned on may prove to be a difficult task. This may be caused by a combination of sleep fragmentation from VNS stimulation and from the anxiety of using CPAP for the first time. Titration of effective CPAP level is classically performed during a full polysomnographic study with the constant attendance of a technician throughout the night. Many patients report poor sleep quality on the night of CPAP titration. Mask related issues, sleeping in unfamiliar surroundings, and frequent adjustments of CPAP pressure may all contribute. Adding to this, sleep fragmentation caused by the VNS stimulation may lead to poorer sleep quality than usual for patients. Therefore, it may be helpful to intially have the VNS device turned off to help find an effective CPAP pressure. Patients should then be restudied with the VNS device on after they have adapted to the use of CPAP. If increased apneas and hypopneas occur with the VNS turned on, the next step would be to try to abolish them by adjusting VNS stimulation parameters (decreasing the stimulus frequency or by increasing the cycling off-time [e.g., activation every 5 min rather than every 3 min]). Another possibility is to reduce current settings. Our patient was on rapid cycling mode (7 sec on/12 sec off). This frequency is similar to the timing of the apneas and cyclic alternating pattern (CAP). Therefore, it is possible that the VNS stimulation in our patient overlapped the occurrence of sleep apneas, with the rapid cycling mode synchronizing by chance with the CAP rhythm. However, this is very unlikely because the events were time locked throughout the night. If these 2 patterns coincidentally occurred, one would expect that they would desynchronize at some point, and this did not happen. In addition, the patient continued to have severe sleep disordered breathing with the VNS off.
Thus, adjustments to VNS device settings must be undertaken only when one is certain that it indeed is the cause of the sleep related apneic events; otherwise, seizure control may be jeopardized. Achieving the optimal VNS settings to control the patient's seizures and not exacerbate his preexisting OSAHS requires close coordination between the epilepsy specialist and the sleep doctor.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Hollinger P, Khatami R, Gugger M, Hess CW, Bassetti CL. Epilepsy and obstructive sleep apnea. Eur Neurol. 2006;55:74–9. doi: 10.1159/000092306. [DOI] [PubMed] [Google Scholar]
- 2.Murray BJ, Matheson JK, Scammell TE. Effects of vagus nerve stimulation on respiration during sleep. Neurology. 2001;57:1523–4. doi: 10.1212/wnl.57.8.1523. [DOI] [PubMed] [Google Scholar]
- 3.Roux FX, Turak B, Landre E. Vagus nerve stimulation for the treatment of refractory epilepsy. Neuro-Chirurgie. 2008;54:332–9. doi: 10.1016/j.neuchi.2008.02.048. [DOI] [PubMed] [Google Scholar]
- 4.Malow BA, Edwards J, Marzec M, Sagher O, Fromes G. Effects of vagus nerve stimulation on respiration during sleep: a pilot study. Neurology. 2000;55:1450–4. doi: 10.1212/wnl.55.10.1450. [DOI] [PubMed] [Google Scholar]
- 5.Papacostas SS, Myrianthopoulou P, Dietis A, Papathanasiou ES. Induction of central-type sleep apnea by vagus nerve stimulation. Electromyogr Clin Neurophysiol. 2007;47:61–3. [PubMed] [Google Scholar]
- 6.American Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic and coding manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 7.Holmes MD, Chang M, Kapur V. Sleep apnea and excessive daytime somnolence induced by vagal nerve stimulation. Neurology. 2003;61:1126–9. doi: 10.1212/01.wnl.0000086812.62554.06. [DOI] [PubMed] [Google Scholar]
- 8.Holmes MD, Miller JW, Voipio J, Kaila K, Vanhatalo S. Vagal nerve stimulation induces intermittent hypocapnia. Epilepsia. 2003;44:1588–91. doi: 10.1111/j.0013-9580.2003.19203.x. [DOI] [PubMed] [Google Scholar]
- 9.Marzec M, Edwards J, Sagher O, Fromes G, Malow BA. Effects of vagus nerve stimulation on sleep-related breathing in epilepsy patients. Epilepsia. 2003;44:930–5. doi: 10.1046/j.1528-1157.2003.56202.x. [DOI] [PubMed] [Google Scholar]