Abstract
Objectives:
Few minority patients with sleep apnea have been evaluated or treated. This study ascertained adherence rate to referrals for sleep apnea evaluation by primary care physicians in a community-based sample of black patients; it also examined baseline characteristics likely to influence adherence rates.
Methods:
A retrospective chart audit was conducted at a hospital-based sleep clinic. Scrutiny was limited to male and female patients between the ages of 20 and 80 years. Data obtained for this analysis included baseline characteristics from a detailed sleep history and/or screening questionnaires and polysomnographic parameters.
Results:
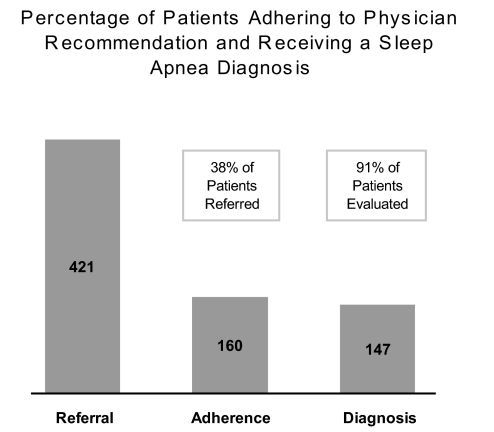
Of the 421 patients referred by their private care physicians, 38% (n = 160) adhered to the recommendation for a sleep consultation, but all who showed up for their appointment underwent polysomnographic studies. Logistic regression analyses showed that obesity and daytime sleepiness were the most important factors predicting adherence, with multivariate-adjusted odds ratios of 2.69 [95% CI: 1.54–4.71, p < 0.001] and 6.98 [95% CI: 3.86–12.64, p < 0.001], respectively. Of the patients who underwent a polysomnographic sleep evaluation, 91% received a sleep apnea diagnosis and were treated.
Conclusions:
Black patients may be underutilizing available sleep services, but direct comparisons with other ethnic groups could not be made because of insufficient archival data. While the present study does not identify specific barriers to accessing services for sleep problems, it indicates that blacks who are obese and/or are experiencing daytime sleepiness are likely to adhere to recommendations of their physician. Targeted culturally congruent educational interventions to increase awareness of sleep apnea in black communities might help to increase adherence rate.
Citation:
Jean-Louis G; von Gizycki H; Zizi F; Dharawat A; Lazar JM; Brown CD. Evaluation of sleep apnea in a sample of black patients. J Clin Sleep Med 2008;4(5):421–425.
Keywords: Sleep apnea, ethnicity, adherence, obesity, sleepiness
Converging epidemiologic and clinical data indicate that sleep apnea is an important public health concern, affecting an estimated 18 million Americans.1–3 There is some evidence suggesting that 82% of men and 93% of women with sleep apnea in the United States remain undiagnosed.1 Underdiagnosis of sleep apnea has been attributed in part to lack of training of primary care physicians.4–7 This is consistent with data showing rates of recognition and diagnosis of sleep disorders in community-based outpatient clinics and university-based clinics are low: 0.1% and 3.1%, respectively.8 Even when primary care physicians are able to recognize patients with sleep apnea symptoms, they are not likely to refer them for sleep evaluation.9
Underdiagnosis of sleep apnea among blacks is of great concern since the burden of sleep apnea is worse in that population.10 One study comparing community-dwelling older blacks and whites found that blacks experienced severe sleep apnea with a relative risk twofold that of their white counterparts.11 Results of that study are in tandem with a case-control family study sampling participants ages 2 to 86 years, which demonstrated that 31% of blacks and 10% of whites had a respiratory disturbance index (RDI) >10.10 In sum, review of the extant literature suggests that physiologic, genetic, and anatomic findings favor greater risks of sleep apnea for blacks.12–14
The aforementioned evidence indicates that the majority of suspected cases in black communities may be undiagnosed and therefore untreated. Whether underdiagnosis among blacks could be explained by lack of awareness by the public and healthcare professionals or by non-adherence to physician recommendations for sleep apnea evaluation remains unclear. It is interesting to note that even if healthcare professionals could recognize symptoms of sleep apnea, diagnostic rates might not necessarily increase, as blacks tend to underreport sleep problems.15,16 Moreover, although the frequency of snoring, the principal sleep apnea symptom, is higher among blacks, they are less likely than whites to report it.12,17 Results of a prospective study showed that 33% of blacks who were interviewed considered snoring to be normal, relative to 20% of whites.12
Delineating the factors preventing timely diagnosis of sleep apnea among blacks might require several systematic studies. These might include an assessment of knowledge, belief systems, and attitudes toward sleep apnea, physician awareness of sleep apnea, and adherence to physician recommendation for sleep assessment. The present study sought to ascertain the adherence rate to physician referrals for sleep apnea evaluation in a community-based sample of black patients. It also examined baseline characteristics likely to influence adherence rates. Finally, it assessed the rate of sleep apnea diagnosis among individuals adhering to physician recommendations.
METHODS
Participants
Data were obtained from a chart audit survey conducted at the Kingsbrook Sleep Center, located in East Flatbush, Brooklyn. Scrutiny was limited to a total of 421 black patients (age range: 20–80 years) who were referred to the clinic by their primary care physicians because of an indication of sleep related breathing difficulties and who filled out a brief sleep apnea screening questionnaire. Their average age was 51 ± 14 years; 57% were female and 43% were male. Of note, the number of white and Hispanic patients was too small for valid comparison; thus, they were not included in the present analyses.
Procedures
Upon receipt of the referrals, patients were contacted to schedule a visit to the clinic for a detailed sleep history by a sleep clinician. Referred patients were first contacted during the day, and those who did not respond were called during evening hours; messages were left when no one answered phone calls. All patients were reminded of their appointments the day before the scheduled visit, and those who did not show up for their first appointment were rescheduled. Referring physicians were informed of patients who either declined the invitation for a clinic appointment or who did not show up for their appointments. Details regarding how many appointments were necessary for each scheduled visit were not available.
Patients meeting clinical criteria were scheduled to spend a night at the clinic for an overnight diagnostic polysomnographic (PSG) recording using Bio-logic digital polysomnograph (Bio-logic Systems Corp. Mundelein, Illinois). According to practice parameters established by the American Academy of Sleep Medicine, polysomnography, the gold standard in sleep recording, is indicated for the diagnosis of sleep apnea.18 All patients had health insurance and consented to undergo sleep evaluation.
Full polysomnographic recordings were performed for all patients in the study. These included electroencephalogram (C3/A2, C4/A1, O1/A2, O2/A1), bilateral electrooculogram, electromyogram (using submental and anterior tibialis muscles), nasal airflow (pressure transducer), oxygen saturation (pulse oximetry), electrocardiogram, respiratory efforts (using thoraco-abdominal straps), and body position. Patients were encouraged to stay in bed for a minimum recording period of 6 hours.
All recordings were manually scored by a trained technician using standard criteria.19 Standard physiological parameters were derived including, sleep structure, SpO2, heart rate, respiratory effort, airflow, EEG- and snoring-related arousals, and total sleep time. Individuals received a confirmed diagnosis of sleep apnea, if they met the revised nosologic criterion (i.e., apnea-hypopnea index [AHI] ≥5). AHI refers to the total number of apneas (complete cessation of breathing ≥10 s) and hypopneas (50% reduction in airflow ≥10 s, followed by SpO2 desaturations [4%] or EEG arousals) divided by the patient's total sleep time. Patients who received a sleep apnea diagnosis were treated using continuous positive airway pressure.20 All patients scheduled for diagnostic or treatment studies received phone reminders the day before scheduled studies.
Statistical Analysis
Demographic and clinical data were initially retrieved from patient charts and entered in Excel spreadsheets, which were later converted in SPSS 15.0 for final analysis. Mean and frequency analyses were used to describe the sample. Fisher exact test was used to compare categorical data, and ANOVA was used for continuous data. Relationships between baseline predictors of adherence to physician referrals were examined using binary multivariate logistic regression analysis. The dependent measure was a binary variable, grouping patients into 2 categories: those who adhered to recommendations to see a sleep clinician versus those who did not. Seven factors were considered as candidate predictors including age, sex, obesity, history of hypertension, snoring, daytime sleepiness, and sleep difficulty.
RESULTS
Of the 421 patients referred to the sleep clinic by their primary care physicians, 38% (n = 160) adhered to recommendations for a sleep consultation (see Figure 1). All who complied initially underwent a nocturnal diagnostic polysomnographic evaluation. Baseline characteristics of patients who underwent PSG recordings are presented in Table 1. Sixty-three percent of the patients attending the sleep clinic were obese.
Figure 1.
Illustration of the number of patients initially referred for a sleep evaluation by their primary-care physician, the number of patients who actually adhered to the recommendation of their physician to see a sleep clinician, and the number of patients who received a diagnosis of sleep apnea
Table 1.
Baseline Clinical Data were Obtained During the Initial Interview with a Sleep Clinician
| Baseline Health Characteristics of Patients Attending Sleep Services | |
|---|---|
| Variables | % |
| High Blood Pressure | 45 |
| Family History of High Blood Pressure | 42 |
| Heart Problem | 9 |
| Family History of Heart Problem | 20 |
| Caffeine Consumption | 21 |
| History of Smoking | 21 |
| Morning Headaches | 36 |
| Depression | 25 |
| Stress | 24 |
In Table 2, we report results of ANOVA and Fisher exact test comparing demographic and health characteristics of the overall sample. Patients who adhered to their physician recommendations were more likely to be obese and to report daytime sleepiness. Other characteristics such as age, sex, history of hypertension, snoring, or sleep difficulty did not show significant group differences. These observations were further assessed using multivariate logistic regression analysis. Regression results confirmed univariate analyses showing that obesity and daytime sleepiness were 2 independent predictors of adherence, with multivariate-adjusted odds ratios of 2.69 [95% CI: 1.54–4.71, p < 0.001] and 6.98 [95% CI: 3.86–12.64, p < 0.001], respectively.
Table 2.
Demographic and Health Characteristics were Derived from Initial Referrals for Sleep Apnea Evaluation by a Primary-Care Physician Including a Brief Sleep Apnea Questionnaire
| Demographic and Health Characteristics of Patients Referred for Sleep Apnea Evaluation | |||
|---|---|---|---|
| Variable | Adherence (38%) | Non Adherence (62%) | F/χ2 |
| Age (mean) | 51 ± 14 | 52 ± 16 | 1.01 |
| Female (%) | 57 | 62 | 1.05 |
| Obesity (%) | 63 | 40 | 20.45* |
| Hypertension (%) | 45 | 39 | 1.77 |
| Snoring (%) | 52 | 43 | 3.08 |
| Daytime Sleepiness (%) | 69 | 26 | 63.45* |
| Sleep Difficulty (%) | 49 | 46 | 0.40 |
Obesity was classified according to NIH criteria. Variables were compared using ANOVA or Fisher exact test; * p < 0.01.
Of the patients who underwent a diagnostic PSG evaluation, 91% received a confirmed diagnosis of sleep apnea using the current nosologic criterion (AHI ≥5 and reported sleep related complaints). There was no significant difference in the rate of diagnosis on the basis of patient's sex (men = 92% and women = 90%). As expected, we found significant associations of severity of sleep apnea with sleep duration (r = −0.39, p < 0.001) and BMI (r = 0.20, p < 0.05).
DISCUSSION
The main finding of the study is that 38% of black patients referred for a sleep evaluation by their primary care physician actually adhered to the recommendation to see a sleep clinician (see Figure 1). Unfortunately, we could not contrast the number of non-adhering blacks to non-adhering patients belonging to other ethnic groups, as representative data were not available. We are not aware of specific data permitting a direct comparison of the adherence rate of black and white individuals referred for a sleep consultation, as was examined in our study. Such comparisons are important insofar as they inform tailored educational intervention programs. Notwithstanding this limitation, our study provides preliminary adherence data that can be compared with data from blacks in geographic areas similar to Brooklyn, NY. Furthermore, they support the need for educational programs geared toward enhancing awareness of sleep apnea in black communities.
Explanation of the observation that so few blacks consulted a sleep clinician for sleep related breathing complaints is inconclusive. Unfortunately, patient charts did not contain any data suggesting possible barriers to accessing sleep services, even when such services are available in the patient's own community. What seems clear from our analysis is that patients who are obese and/or are experiencing daytime sleepiness were more likely to seek help than those who were not. It may be that patients with those characteristics had comorbid conditions, which might have predisposed them to seek sleep consultation. A previous study suggested that patients experiencing insomnia with comorbid conditions were twice as likely to seek help for insomnia.21 Interestingly, snoring, the primary complaint indicative of sleep apnea, was not a significant determinant of the likelihood to adhere to physician recommendations to see a sleep clinician. This observation seems consistent with previous reports that blacks are more inclined to consider snoring to be normal and are therefore less likely to report it, compared with whites.12,17
The finding that blacks underutilize sleep services is certainly important, but was not totally surprising. Screening rates for other medical conditions are also low among blacks.22,23 For instance, a study assessing screening rates for diabetic retinopathy showed that only 27% of blacks adhered to the recommendation for an ophthalmic exam.24 In 2 other studies conducted in similar communities in Brooklyn, NY, we consistently found that blacks reported fewer sleep problems than their white counterparts.15,16 These findings are important, given that primary care physicians are not likely to probe for sleep problems during regular clinic visits, particularly when patients do not complain of sleep related difficulties.
It appears much less convincing that underdiagnosis of sleep apnea among blacks would be explainable solely on the basis of limited access to health care because of economic barriers.25,26 We could not assess differences in socioeconomic status between adhering and non-adhering patients, but all of the patients referred to the sleep clinic had health insurance. Our results are consistent with a comparative study, showing that black beneficiaries of health insurance—whether by Medicare or private insurers—and having access to healthcare were less likely to seek treatment for sleep apnea than white beneficiaries.27
Non-adherence in our study seems to be a concern primarily at the level of the initial consultation for sleep problems. All patients scheduled for PSG kept their appointments, which may be explained by the practice implemented at the clinic consisting of an initial consultation to assess sleep problems and the use of phone reminders. Therefore, more focused research into the factors responsible for non-adherence to recommendations to see a sleep specialist is necessary. Such factors might include the appropriateness of the referrals, possible scheduling conflicts, cultural barriers, and lack of sleep apnea awareness. It is also of interest to assess how many non-adherent blacks might have initiated self-help treatments, as is often observed among patients with sleep problems.28
The other important observation in our study is that 91% of the patients that adhered to the recommendation to undergo a sleep evaluation received a diagnosis of sleep apnea and were treated. Unfortunately, we could not contrast this finding to the rate of blacks with sleep apnea in the general population because of lack of representative data. That the majority of patients received a diagnosis is consistent with the finding that patients who underwent PSG recordings were more likely to be obese and experienced daytime sleepiness. Obesity and daytime sleepiness are 2 of the most important predictors of sleep apnea.29–31 It is estimated that 60% to 90% of patients with sleep apnea are obese, and that a BMI of 28 kg/m2 has a sensitivity of 93% and a specificity of 74% for sleep apnea.30
CONCLUSIONS
Generalizability of the present findings is limited in some respects. Our results are based on a retrospective chart review, with a sampling frame restricted only to patients who were referred by a primary care physician for a sleep evaluation. Although we cannot generalize our findings to blacks in all U.S. communities, they constitute preliminary data that might form the basis for systematic inquiries into the factors affecting adherence rates among patients in similar communities. Moreover, since the number of white patients seen at the clinic was statistically underpowered, we could not contrast adherence rates of black and white patients regarding initial referrals for sleep evaluations.
No data was available permitting the assessment of knowledge and attitudes toward sleep of adherents and non-adherents to physician recommendations for a sleep evaluation. Such characteristics could be useful in the development of community-based intervention programs tailored to enhance adherence to physician recommendations. Emerging consensus suggests that healthcare practices must take into account patients' attitudes and belief systems as well as their ethnic origin and degrees of acculturation in developing intervention programs.32 Despite the lack of data that would allow the identification of specific barriers limiting access to available sleep services, our study indicates that obesity and daytime sleepiness are two important determinants of the likelihood to seek initial sleep consultations among blacks.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research was supported by funding from the NIH (1R24MD001090 and HL085042).
REFERENCES
- 1.Young T, Finn L. Epidemiological insights into the public health burden of sleep disordered breathing: sex differences in survival among sleep clinic patients. Thorax. 1998;53(Suppl 3):S16–9. doi: 10.1136/thx.53.2008.s16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phillipson EA. Sleep apnea—a major public health problem. N Engl J Med. 1993;328:1271–3. doi: 10.1056/NEJM199304293281712. [DOI] [PubMed] [Google Scholar]
- 3.Omnibus Sleep in America Poll. National Sleep Foundation. 2005:1–51. [Google Scholar]
- 4.Ball EM, Simon RD, Jr, Tall AA, et al. Diagnosis and treatment of sleep apnea within the community. The Walla Walla Project. Arch Intern Med. 1997;157:419–24. [PubMed] [Google Scholar]
- 5.Bahammam A, Kryger M. Decision making in obstructive sleep-disordered breathing: putting it all together. Otolaryngol Clin North Am. 1999;32:333–48. doi: 10.1016/s0030-6665(05)70133-x. [DOI] [PubMed] [Google Scholar]
- 6.Chung SA, Jairam S, Hussain MR, et al. Knowledge of sleep apnea in a sample grouping of primary care physicians. Sleep Breath. 2001;5:115–21. doi: 10.1007/s11325-001-0115-4. [DOI] [PubMed] [Google Scholar]
- 7.Silverberg DS, Oksenberg A, Iaina A. Sleep related breathing disorders are common contributing factors to the production of essential hypertension but are neglected, underdiagnosed, and undertreated. Am J Hypertens. 1997;10:1319–25. doi: 10.1016/s0895-7061(97)00322-1. [DOI] [PubMed] [Google Scholar]
- 8.Rosen RC, Zozula R, Jahn EG, et al. Low rates of recognition of sleep disorders in primary care: comparison of a community-based versus clinical academic setting. Sleep Med. 2001;2:47–55. doi: 10.1016/s1389-9457(00)00043-5. [DOI] [PubMed] [Google Scholar]
- 9.Kramer NR, Cook TE, Carlisle CC, et al. The role of the primary care physician in recognizing obstructive sleep apnea. Arch Intern Med. 1999;159:965–8. doi: 10.1001/archinte.159.9.965. [DOI] [PubMed] [Google Scholar]
- 10.Redline S, Tishler P, Hans M, et al. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997;155:186–92. doi: 10.1164/ajrccm.155.1.9001310. [DOI] [PubMed] [Google Scholar]
- 11.Ancoli-Israel S, Klauber MR, Stepnowsky C, et al. Sleep-disordered breathing in African-American elderly. J Gerontol. 1989;44:M18–21. doi: 10.1164/ajrccm.152.6.8520760. [DOI] [PubMed] [Google Scholar]
- 12.Friedman M, Bliznikas D, Klein M, et al. Comparison of the incidences of obstructive sleep apnea-hypopnea syndrome in African-Americans versus Caucasian-Americans. Otolaryngol Head Neck Surg. 2006;134:545–50. doi: 10.1016/j.otohns.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Lee JJ, Ramirez SG, Will MJ. Gender and racial variations in cephalometric analysis. Otolaryngol Head Neck Surg. 1997;117:326–9. doi: 10.1016/S0194-5998(97)70121-9. [DOI] [PubMed] [Google Scholar]
- 14.Buxbaum SG, Elston RC, Tishler PV, et al. Genetics of the apnea hypopnea index in Caucasians and African Americans: I. Segregation analysis. Genet Epidemiol. 2002;22:243–53. doi: 10.1002/gepi.0170. [DOI] [PubMed] [Google Scholar]
- 15.Jean-Louis G, Magai C, Cohen CI, et al. Ethnic differences in reported sleep problems in older adults. Sleep. 2001;24:926–33. doi: 10.1093/sleep/24.8.926. [DOI] [PubMed] [Google Scholar]
- 16.Jean-Louis G, Magai C, Consedine NS, et al. Insomnia symptoms and repressive coping in a sample of older Black and White women. BMC Womens Health. 2007;7:1. doi: 10.1186/1472-6874-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;26:74–9. [PubMed] [Google Scholar]
- 18.Chesson AL, Jr, Ferber RA, Fry JM, et al. The indications for polysomnography and related procedures. Sleep. 1997;20:423–87. doi: 10.1093/sleep/20.6.423. [DOI] [PubMed] [Google Scholar]
- 19.Rechtshaffen A, Kales A. Los Angeles: UCLA Brain Information Service/Brain Research Institute; 1968. A manual of standardized terminology, techniques, and scoring systems of sleep stages of human subjects; p. 10. [Google Scholar]
- 20.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 21.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18:257–61. doi: 10.3122/jabfm.18.4.257. [DOI] [PubMed] [Google Scholar]
- 22.Katz ML, James AS, Pignone MP, et al. Colorectal cancer screening among African American church members: a qualitative and quantitative study of patient-provider communication. BMC Public Health. 2004;4:62. doi: 10.1186/1471-2458-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ko CW, Kreuter W, Baldwin LM. Persistent demographic differences in colorectal cancer screening utilization despite Medicare reimbursement. BMC Gastroenterol. 2005;5:10. doi: 10.1186/1471-230X-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basch CE, Walker EA, Howard CJ, et al. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89:1878–82. doi: 10.2105/ajph.89.12.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penn NE, Kar S, Kramer J, et al. Ethnic minorities, health care systems, and behavior. Health Psychol. 1995;14:641–6. doi: 10.1037//0278-6133.14.7.641. [DOI] [PubMed] [Google Scholar]
- 26.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(Suppl 1):108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 27.McBean AM, Gornick M. Differences by race in the rates of procedures performed in hospitals for Medicare beneficiaries. Health Care Financ Rev. 1994;15:77–90. [PMC free article] [PubMed] [Google Scholar]
- 28.Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Grunstein R, Wilcox I, Yang TS, et al. Snoring and sleep apnoea in men: association with central obesity and hypertension. Int J Obes Relat Metab Disord. 1993;17:533–40. [PubMed] [Google Scholar]
- 30.Kushida CA, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med. 1997;127:581–7. doi: 10.7326/0003-4819-127-8_part_1-199710150-00001. [DOI] [PubMed] [Google Scholar]
- 31.Goncalves MA, Paiva T, Ramos E, et al. Obstructive sleep apnea syndrome, sleepiness, and quality of life. Chest. 2004;125:2091–6. doi: 10.1378/chest.125.6.2091. [DOI] [PubMed] [Google Scholar]
- 32.Sharps PW, Phillips J, Oguntimalide L, et al. Knowledge, attitudes, perceptions and practices of African-American women toward menopausal health. J Natl Black Nurses Assoc. 2003;14:9–15. [PubMed] [Google Scholar]