Abstract
Objectives
To evaluate the effectiveness of an integrated approach to the teaching of evidence-based complementary and alternative medicine (CAM) in a pharmacy curriculum.
Design
Evidence-based CAM education was integrated throughout the third, fourth, and fifth years of the pharmacy curriculum. Specifically, an introductory module focusing on CAM familiarization was added in the third year and integrated, evidence-based teaching related to CAM was incorporated into clinical topics through lectures and clinical case studies in the fourth and fifth years.
Assessment
Students' self-assessed and actual CAM knowledge increased, as did their use of evidence-based CAM resources. However, only 30% of the fourth-year students felt they had learned enough about CAM. Students preferred having CAM teaching integrated into the curriculum beginning in the first year rather than waiting until later in their education.
Conclusion
CAM education integrated over several years of study increases students' knowledge and application.
Keywords: complementary and alternative medicines, curriculum, evidence-based education
INTRODUCTION
More than 50% of the world's population uses complementary and alternative medicine (CAM), mostly in combination with conventional medication. There is growing evidence outlining the benefits as well as the possible adverse and side effects of CAM.1 As primary care providers, pharmacists are both accessible to patients and one of the most trusted healthcare professionals. As such they are at the forefront, providing information and guidance to patients about safe and effective use of all medicines.
Pharmacists generally rate their knowledge relating to CAM as inadequate and are not confident in answering patient inquiries.2-5 A survey among Australian community pharmacists showed that 57% of the pharmacists stated that their training had not met their needs regarding CAM knowledge, that they relied heavily on manufacturers' information about CAM, and that their lack of suitable training was one of the perceived barriers to information provision about CAM.6
Studies surveying pharmacy schools in the US concluded that while approximately 80% of schools offer some form of CAM training in the curriculum, CAM education was primarily offered as electives and generally focused on natural products rather than the full range of CAM practices.7-9 Similar to the studies in the US, the extent to which CAM is taught and integrated varies widely among Australian and New Zealand pharmacy schools, which is partly because in Australia the integration of CAM into pharmacy and medical curricula is not mandatory and is handled quite differently at various institutions.10-12
Importantly, most surveys of medical and pharmacy students revealed that the majority of students welcomed the inclusion of CAM education in the medical13-16 and pharmacy curricula.17,18 However, most of the studies indicated that students had insufficient knowledge to be able to recommend or counsel about CAM.13,19
By interviewing practicing Australian community pharmacists, Semple et al identified the need for integrated, nonbiased, evidence-based undergraduate CAM training that is not conducted by CAM manufacturers.6 Such findings support the debate to integrate CAM training as a core component into health professional education instead of offering it as electives, as it will provide students with the expected knowledge.9 Moreover, an elective course could be seen as marginalizing CAM in the minds of students and staff members as a fringe topic only appealing to a few.20 Integrated CAM education provides students not only with CAM specific knowledge, but also encompasses much broader themes, encouraging them to think outside the box, thus promoting critical evaluation of the evidence.11,21 As such, integrated CAM education can be the “bridge between allopathic medicine and CAM,”22 thus closing the gap between the 2 streams of healthcare and allowing medical pluralism, which is demanded today by patients and students alike.21,23
The integration of CAM education into existing pharmacy curricula aims to increase the understanding and knowledge of CAM modalities by broadening students' horizons and instilling a greater acceptance and appreciation of patient choices to achieve better health outcomes.21, 24, 25
A variety of educational programs have been evaluated internationally for their effectiveness in CAM training; however, evaluating CAM curricula is difficult. For example, the National Centre for Complementary and Alternative Medicine in the United States (NCCAM) awarded funding to 15 academic programs through the R25 Education Grant program to include CAM education into existing medical, nursing, and allied health curricula using a variety of approaches.26,27 As a result, studies have been published that focus on institutional strategies and barriers to implementing CAM into existing programs.28 Other studies describe for example single educational programs (ie, a core CAM teaching session to first-year medical students),29 elective programs (ie, a 3-week elective CAM rotation),30 and short intervention educational programs (ie, 4 weeks of intensive “CAM camp”).31 However, methods to evaluate curricula changes conducted were diverse among the 15 programs, thus limiting the ability to compare programs and outcomes.32
Moreover most educators and professionals share the belief that a multi-factorial approach to teaching evidence-based CAM would be preferable33 and that CAM education should be included at all levels of medical education, from day one of the undergraduate program.20,34
Thus far, only one study that specifically evaluated a mostly integrative approach to CAM education has been published.35 However, this study evaluates CAM training that is integrated into a medical rather than a pharmacy curriculum. Also, the curriculum is not described in much detail and only interviews are used to evaluate the program.35
In this article, the design and underlying teaching concept of evidence-based CAM education integrated into a core pharmacy curriculum is described. In addition, an evaluation of how the integrated education approach affected students' motivations, concepts, and knowledge towards CAM is presented. By distinguishing between complementary medicines and complementary therapies, possible differences in students' qualifications, learning, and use of knowledge with regard to different CAM modalities were explored. Our study is the first that thoroughly describes an integrated approach to CAM teaching for a pharmacy curriculum and evaluates it among different student cohorts using a survey instrument, as well as interviews. The evaluation aims to provide beginning evidence for integrated CAM teaching and course design in core pharmacy curricula and to allow for recommendations for further research to develop multidisciplinary teaching of CAM in health professional education.
DESIGN
The pharmacy degree at this Australian University is a combined 4½-year degree that consists of a 3-year bachelor of pharmaceutical sciences degree followed by a 1½-year master of pharmacy degree. Both programs are integrated and, only if completed, jointly lead to registration as a pharmacist.
In this educational approach, CAM education was integrated into the third, fourth, and fifth years of the pharmacy curriculum. At the third-year level, an introductory module (6 weeks) on the quality use of CAM was incorporated into the undergraduate course, Quality Use of Medicines. Thus, it provided students with an overview of quality, safety, and efficacy issues of CAM, as well as illustrating the overall role of CAMs in the maintenance of health. The module was comprised of 17 lectures, 4 workshops, 1 industry visit, and 1 community pharmacy placement.
The CAM module was divided into various submodules. The first submodule introduced terminology, modalities, regulation, and the overall role of CAM in healthcare. During their first workshop, students learned about the variety of web sites that contain CAM-related information, such as the Australian-specific Therapeutic Goods Administration, Complementary Healthcare Council, and Australian Self-Medication Industry web sites, as well as important international web sites such as World Health Organization, NCCAM in the United States, and European Scientific Cooperative on Phytotherapy.
The second submodule focused specifically on herbal medicines and their regulation, preparation, natural product classes, quality control, and safety aspects. During this submodule, students visited an herbal medicine manufacturer and its research and development department. They had to complete a visit exercise that highlighted questions regarding the standardization, quality control, and research aspects of herbal medicines.
A third submodule focused on the efficacy of specific herbal medicines and nutritional supplements. In the respective workshop, a practicing pharmacist (with degrees in herbal medicines and clinical nutrition) compared different CAM products and outlined differences in quality, safety, and efficacy. Moreover, students were familiarized with evidence-based CAM information sources and the critical evaluation of evidence for efficacy of CAM products because education research shows that CAM education should involve methods for analyzing and critically assessing the available evidence.36,37 The newly acquired knowledge about CAM evidence evaluation was then applied by groups of students to prepare an oral presentation about the clinical use of spices/herbs included in general food recipes. This exercise was designed to highlight the relationships between health and diet and food and medicine. Students had to incorporate all previously acquired knowledge by highlighting spice/herb origin, traditional use, active constituents, pharmacological effects, evidence for clinical use if applicable, and possible safety or quality concerns. The group presentations take place in a subsequent workshop.
A fourth submodule provided basic knowledge about alternative practices such as homeopathy, traditional Chinese medicine, Ayurvedic medicine, and naturopathy, including their utilization, underlying philosophies, evidence, quality, and safety. The final submodule gave an overview about therapies such as meditation and biomagnetism. The fourth and fifth submodules utilized videos to emphasize and underline unfamiliar healing principles to the students. During a community pharmacy visit at the end of the module, students were asked to complete a practice-based exercise, observing CAM-counseling in pharmacies. A fourth workshop was used for feedback, review, and evaluation.
The CAM module taught in the third year set the scene for evidence-based CAM education integrated into 3 clinical courses, Pharmacotherapeutics 1, 2 and 3, which were taught in the fourth and fifth year of the degree. These clinical courses focused on the management of specific disease states for various body systems. In the past, educators have highlighted that information about CAM should be included in clinical courses as well being covered in courses focused on the principles of evidence-based practice.38 Therefore, evidence-based CAM information was delivered as specific lectures for various disease states (eg, “Use of CAM in Cancer” or “Use of CAM in respiratory conditions” or “Use of CAM in gastrointestinal conditions”).
As part of the clinical Pharmacotherapeutics courses 1, 2 and 3, workshops were designed during which student groups had to solve real clinical cases. These case studies were examples of peer-directed teaching/learning activities39 and were intended to provide students with procedural and conditional knowledge that would hopefully lead them to gain professional knowledge by graduation time. Such clinical cases have been reported in the literature to be one of the best ways of teaching professional skills to pharmacy students.40 Moreover, as a practical step for the inclusion of CAM education into the curriculum, Wetzel et al highlighted the incorporation of CAM into clinical cases.20 Therefore, CAM problems (eg, beneficial CAMs, possible interactions with drugs, dosing, adverse effects, safety issues) were integrated into the clinical cases throughout all 3 Pharmacotherapeutics courses. As such, the CAM training was directed toward community practice independent of manufacturers, and highlighted possible beneficial as well as harmful effects of using CAM in patient care.6
Data were collected by cross-sectional survey and qualitative interviews. Ethical clearance for the study was obtained through the HREC of the institution. A cross-sectional questionnaire was administered following lectures in week 10 of the second semester in 2006. One hundred ten pharmacy students (36 students from second year, 34 from third year, and 40 from fourth year) completed the questionnaire. The 50-item questionnaire included demographic information about students, items related to self-assessment of CAM knowledge, items related to use of CAM knowledge during placements, items related to sources of information and knowledge about CAM, and a CAM knowledge test, as well as barriers to CAM use, and items related to the general attitudes towards and perceptions of CAM.
The CAM knowledge test was part of the questionnaire; thus, the same CAM knowledge testing instrument was used for all the students surveyed. The 10 knowledge questions could be answered with 3 possible responses: true, false, and don't know. All other items were either multiple-choice answers or lists where multiple options could be marked, except for the attitude and perception items, where a 5-point Likert rating scale was used.
Survey data were entered into SPSS version 14.0. Descriptive statistics such as frequencies, means, standard deviations, and ranges were used to summarize the data. For the Likert responses, all responses with any degree of agreement were grouped together as positive responses, and all responses with any degree of disagreement were grouped together as negative responses. T tests and chi-square were used to analyze differences between cohorts as appropriate. Results were considered significant when the p value was less than 0.05.
Semi-structured interviews (15-25 minutes) were conducted with 9 students (3 from each cohort) in weeks 11 and 12 of the second semester in 2006. The interviews took place in the School of Pharmacy and were audio taped. In a conversational style, specific topics such as students' motivations and purposes related to studying CAM, their expectations and satisfaction with the curriculum, and their attitude towards CAM were pursued.
The transcripts from the interviews were independently coded and analyzed by both authors, and were read and re-read while checking the tape recording for accuracy. Qualitative content analysis techniques were then employed.41 The text was coded, each sentence was read, and a label attached to the text. These codes were then grouped together into descriptive categories.41
Students were familiar with the distinction between complementary medicines and therapies as it was explained and used in lectures and workshops. Moreover, a paragraph outlining the distinction between complementary medicines and therapies was given at the start of the questionnaire and was read to the students at the start of each interview.
The second-, third-, and fourth-year cohorts were chosen, as these cohorts represented students at different stages of their CAM education. Thus, at the time of the survey the second-year students had received no CAM training apart from one CAM lecture with some information regarding the mechanism of interactions of drugs with the herbal medicine, St John's wort. At the time of the questionnaire and interview, the third-year students had attended the introductory module on the quality use of CAM in the previous semester and fourth-year students had already received integrated evidence-based CAM training in the clinical subjects throughout the previous 2 semesters.
ASSESSMENT
The response rates for the survey were 75% for first-year students, 50% (36/72) for second-year students, 77.3% (34/44) for third-year students, and 97.6% (40/41) for fourth-year students. Differences in age and gender between the 3 cohorts did not reach statistical significance. Overall, 80.9% were equal or younger than 24 years of age and 68.1% were female.
Work experience in a pharmacy differed significantly between second-, third- and fourth-year (p = 0.004). Of the second-year students, 63.9% specified working in a pharmacy outside of visit and placement hours, while 77.1% of third-year students and 94.9% of fourth-year students had done this. Overall, only 7.2% of students had qualifications in complementary medicines (chi-square = 1.2; p = 0.54); none had qualifications in complementary therapies (CTs). The number of students who indicated they had received CAM training in addition to a possible previous CAM qualification and the pharmacy degree did not differ between the groups. Overall, only one third (27.3%, chi square = 2.3; p = 0.31) of pharmacy students received CAM training through means other than formal qualifications or a pharmacy degree.
Scores in the knowledge test increased significantly from year to year (second year: mean = 3.9, SD = 1.8; third year: mean = 6.6, SD = 2.4; fourth year: mean = 7.9, SD = 1.6; p = <0.0001; one-way ANOVA).
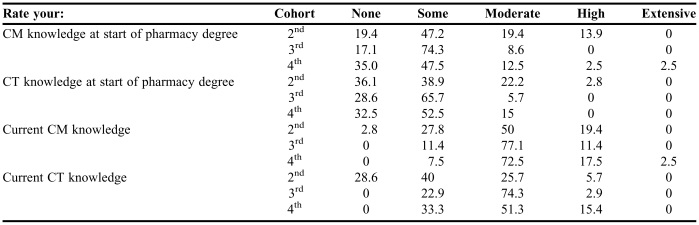
Student's self-assessed knowledge regarding complementary medicines and therapies was different in each cohort (Table 1). Within the fourth-year cohort, 15% of students identified their starting complementary medicine knowledge as “moderate” and “high,” whereas when asked about their current knowledge, 90% of the students classified it as “moderate” and “high,” indicating their perception of an increase in their knowledge about complementary medicines over the course of their program. The increase, over the course of the program, in the proportions of students reporting “moderate” and “high” levels of knowledge was more profound with regards to complementary medicines than complementary therapies. When comparing all 3 cohorts, the third-year cohort displayed the largest increase in the proportion of students who self-assessed their CAM knowledge as “moderate” and “high” from the start of their degree to currently. For example, 79.9% more students stated their current knowledge on complementary medicines as “moderate” and “high” in the third year in comparison to 75% in the fourth year and only 36% in the second year. This mimics the increase in CAM education from the first and second years (virtually none) to the third year (a 6 weeks module).
Table 1.
Self-Assessed CAM Knowledge of Students from All Cohorts, %
Abbreviations: CAM = complementary and alternative medicine; CM = complementary medicine; CT = complementary therapy
There seemed to be a disproportionate number of second-year students who assessed their starting and current CAM knowledge as high. This may be due to the fact that the second-year students had not received any formal CAM training as part of their degree at the time of the survey. Whereas third- and fourth-year students had, possibly through more training, realized the breadth of the CAM field and how much they still had to learn and were therefore more careful when evaluating their own knowledge.
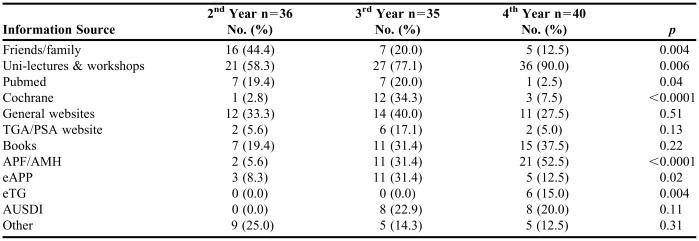
In our study, differences between cohorts were recorded for the usage of information sources (Table 2). In general the use of professional literature such as the Australian Pharmaceutical Formulary and handbook (APF)/Australians Medicines Handbook (AMH) was significantly higher in the fourth year (<0.0001). In contrast, use of friends and family as information providers was significantly lower among the fourth-year cohort compared to the other 2 groups (p = 0.004). Qualitative data indicated that this was possibly due to development of increased student competence and confidence in applying the principles of critical appraisal of research evidence.
Table 2.
Students Across Each Cohort Who Accessed Information Related to CAM
Abbreviations: TGA = Therapeutic Goods Administration; PSA = Pharmaceutical Society of Australia; APF = Australian Pharmaceutical Formulary and Handbook; AMH = Australians Medicines Handbook; eAPP = Electronic Australian Prescription Products Guide; eTG = Electronic Therapeutic Guidelines; AUSDI = Australian Drug Information for the Health Care Professional
The mean number of information sources used was lower in the fourth-year cohort than in the third-year cohort, with the third-year cohort using the most information sources (3.63). The second-year cohort used 2.28 and the fourth-year cohort used 3.1 resources (p = 0.002). Also, significantly more third-year students utilized evidence-based web sites such as the Cochrane Library (34.4 3%, p < 0.0001), PubMed (20 %, p = 0.04) and electronic Australian Prescription Products Guide (eAPP) (31.4 %, p = 0.02) in comparison to the second- and fourth-year cohorts. This is probably due to the emphasis on evidence finding and evaluation in the third year, which is so far not reinforced in the fourth year.
Most students (58%-90%) used University lectures and workshops as primary CAM information sources, with numbers increasing significantly over the years of study (p = 0.006). Thus, it seems that the educational material provided to the students was perceived as useful; however, students should also be encouraged to use other resources.
Satisfaction With the Curriculum
The proportions of students who believed that they had learned enough about complementary medicines and therapies significantly increased with the years of study (complementary medicines: chi square = 11.36, p = 0.003; and complementary therapies: 11.33, p = 0.003). However, overall only 32.5% of fourth-year students believed that they had acquired enough knowledge about complementary medicines and therapies.
Nevertheless, qualitative data showed that overall the students were satisfied with the CAM education throughout the third and fourth year. Students commented positively about the third-year module and highlighted the module's relevance as a foundation for the fourth- and fifth-year subjects.
In the qualitative interviews, students expressed a variety of opinions about the structure and length of the third-year module. Some students thought that the CAM content in the third-year module was sufficient, whereas other students commented that CAM in the third year would be better taught as a separate course and one student did not believe sufficient time was allocated to CAM in the third year.
In the interviews, most students indicated that the CAM content in the clinical subjects in the fourth year was sufficient; however, a few students requested more time be allocated to CAM education to train students in the practical application of CAM knowledge.
Some students wanted CAM to be introduced earlier in the curriculum. Reasons for this were: high amount of information to be covered, limited prior CAM knowledge, need more time to comprehend CAM knowledge, and limited pharmacy practice experience until later in the curriculum.
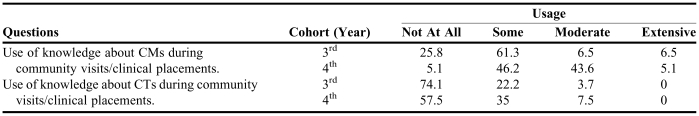
Overall, students used their knowledge of complementary medicines to a larger extent than their knowledge of complementary therapies during the community visits/placements (Table 3). However, less than 50% of the fourth-year students used their knowledge of complementary medicines to “some” and to a “moderate” degree. Over 50% of third- and fourth-year students did not use their knowledge of complementary therapies “at all.” Just 5% of students in each cohort reported extensive use of complementary medicine knowledge during their visits and placements.
Table 3.
Pharmacy Students' Self-assessed Use of CAM Knowledge During Visits and Clinical Placements, %
Abbreviations: CAM = complementary and alternative medicine; CM = complementary medicine; CT = complementary therapy
Qualitative data identified some possible reasons for only half the students using and practicing their knowledge of complementary medicines and, to a lesser extent, complementary therapies. Several reasons were identified: students and preceptors were not engaged in CAM tasks during placements, limited CAM knowledge of preceptor, no CAM resources available in the pharmacy, and limited CAM content in placement exercises.
DISCUSSION
Other studies suggest that medical students have insufficient knowledge to be able to recommend or counsel about CAM.13,19 Moreover, surveys of medical and pharmacy students indicate that the majority of students welcome the inclusion of CAM education in the medical13-16 and pharmacy curricula.17,18
Although schools offering elective CAM education report positive results, such as increased self-assessed knowledge and more positive attitudes towards CAM,30,31 such outcomes pertain only to the students who chose to take the elective. Given that higher self-awareness,24 improved core competencies for conventional health professionals, enhanced cultural competency, and patient centred care have been reported for health professionals with CAM knowledge,25 CAM curricula development should focus on integrated CAM education rather than on standalone elective courses –a notion that is supported by an increasing number of academics.20,25,33
Moreover, a clear comparison between different curricula is impossible because of the lack of an objective measure of knowledge or skills.32,42,43 That is, changes in perceived knowledge, skills, or both may not necessarily translate to actual changes in knowledge or skills.38 Furthermore, some educators reported an attitude change but no knowledge change towards CAM with increasing education.44
Our study investigated students' prior CAM knowledge, self-assessed CAM knowledge, and actual knowledge using an objective knowledge test. We found that less than 10% of pharmacy students had a qualification in complementary medicines and less than a third received some sort of CAM training external to the University, which highlights the necessity for sufficient CAM education during a professional pharmacy degree. Furthermore, our evaluation shows an increase in self-assessed knowledge in the fourth year, and a significant boost in knowledge scores in the fourth-year cohort compared to other cohorts. Increased self-assessed knowledge was also reported by students following a 3-week elective CAM rotation offered as part of their medical curriculum.30 Furthermore, a study integrating CAM training as a 4-week “CAM camp” into a nursing curriculum gave mixed (survey) and more positive results (interviews) regarding the students familiarity with CAM modalities.31 However, objective measures of knowledge gain were not utilized in both studies.
In our study the knowledge scores corresponding to more CAM education in the curriculum increased significantly; however, only a third of the fourth-year students thought they had learned enough about CAM. An additional survey with a detailed analysis regarding the adequacy of the length, coverage, and timing of specific CAM topics is anticipated to aid in a detailed understanding of students' responses to this question. However, qualitative data indicated that students seemed relatively satisfied with the amount of CAM education in our educational setting, but commented on the need for increased contact time to allow for in-depth training and application. This seems to relate to a study investigating healthcare professional's knowledge reporting on deficits, especially in knowledge relating to adverse effects, confidence in reporting side effects, routine communication with patients about CAM, and the reporting of CAM information in the medical record.45 Students suggested the integration of CAM education from the first year onwards, as has been previously recommended by other authors.20,34 Such a change would potentially increase the proportion of fourth-year students that feel they have learned enough and improve learning outcomes as more time could be spent rehearsing and applying CAM knowledge.
Strategies to include CAM education into the first and second year are being currently identified, with implementation anticipated in the near future. Moreover, the suggested extension of the third-year module from 6 weeks to a full semester would allow for more CAM familiarization before the clinical subjects and should be discussed.
Previous surveys reported different CAM information sources used by student health professionals. For example, some papers found the Internet as the main CAM information source for students,42,44,46 whereas others clearly highlighted family and friends as the primary information source.43
In our study, the distribution of students using specific evidence-based information sources shifted from third to fourth year, with a significantly higher proportion of fourth-year students using professional handbooks, whereas the use of peer-reviewed articles and reviews (eg, PubMed and Cochrane) declined significantly from third to fourth year. The higher use of PubMed and Cochrane in the third year may be due to these online resources being introduced and highly promoted as CAM resources in the third-year module. Such a “recency effect” was also reported by Lie et al who concluded that there is a need to repeat teaching of online information on CAM later in the curriculum.42 Moreover, the high usage of clinical handbooks as a CAM resource by fourth-year students was probably due to an increase in clinical teaching and awareness of professional guidelines, and highlights the importance of having up-to-date CAM content in professional pharmacy handbooks and formularies.
Our students frequently used CAM coursework material as a source of information (58%-90%), which is in contrast to other studies which reported that formal training or coursework was only used by up to 38% of pharmacy students.47
Our study also revealed that the placement experience is not sufficiently utilized for CAM training, possibly due to limited exposure of students to CAM problems and the limited CAM knowledge of some preceptors. The utilization of the placement for CAM education should be further investigated especially as a study investigating herbal medicine education highlighted the desire of students for practice-related information.48 Considering that positive clinical experiences are more likely related to how valued and supported students feel rather than the physical aspects of a placement, it is imperative that educators assess how the placements/preceptors chosen by the students offer a supportive learning environment.49
In Australia, a national strategy for pharmacy preceptor education and support has been developed for online and CD-ROM delivery.50 It contains general and specific advice including ethics, expectations, types of teaching, and learning activities, but it does not focus on specific clinical content, as this is usually covered by continuing professional education (CPE) seminars. However, CPE seminars focusing on CAM are rare. A specifically designed CAM training program for preceptors would prepare pharmacists for their role as educators, thereby improving educational outcomes for students, while also improving outcomes in pharmacy practice. For example, a study of community pharmacists, who had undergone a specific educational intervention to provide specialized asthma care demonstrated the effectiveness of an educational approach, inducing behavioral changes in pharmacy practitioners resulting in improved patient outcomes.51
Multiprofessional education for health professionals is feasible and results in positive learning outcomes such as increased interprofessional collaboration, improved communication skills, mutual respect, increased confidence levels, increased understanding of others' professional roles, and personal development.52-54 Research into interprofessional and multiprofessional education specifically focusing on CAM training is lacking, although the basis for its importance exists. For example, some community pharmacists have reported that doctor's disagree with their CAM recommendation, possibly due to insufficient information,6 leading to confusion and noncompliance by the patient. However, the content of multiprofessional training must be carefully evaluated as differences in educational preferences and needs among health professional students exist. In our study, students reported significantly more complementary medicine than complementary therapy knowledge use in their placements. This reflects the results from previous studies showing that pharmacy students prefer education in complementary medicines over complementary therapies, whereas medical and nursing students preferred education in specific complementary therapies.18,47 Nevertheless, an overlap of CAM skill and knowledge base among health care practitioners is optimal for high-quality patient care and should therefore be designed and evaluated for existing and future health professional curricula.
Given the consumer-driven development towards holistic and integrative healthcare,23 clinical knowledge including beneficial effects of CAM, as well as compounding training using ingredients regarded as complementary medicine, are a high pharmaceutical education priority55 that might be essential for future registration as a pharmacist. Thus, firm recommendations and required competencies from professional and educational bodies to assist CAM curriculum development are urgently needed.6,8,48
Further development of the CAM curriculum in our School of Pharmacy will focus on integrating CAM education into the pharmacy curriculum from the first year of study, expanding CAM familiarization at the third-year level, enhancing the integration of CAM into clinical cases, designing placement exercises, and developing preceptor CAM training, as well as conducting research into multidisciplinary teaching of CAM in undergraduate curricula for health professionals. Nevertheless, the CAM education described here could be adapted by other pharmacy schools. At a minimum it should provide the impetus for an open debate regarding what level of CAM education is sufficient in pharmacy curricula.
CONCLUSION
An integrated CAM teaching approach was effective in generating knowledge of general CAM philosophies and specific CAM modalities. It influenced CAM knowledge use during placements and students' use of evidence-based CAM resources. Students would prefer integrated evidence-based CAM education throughout their program of study. Further research into the content and focus of CAM education is necessary to meet the educational needs of our future pharmacists.
ACKNOWLEDGEMENTS
The authors thank Ms. M. Lupton (Griffith Institute of Higher Education), Dr. R. Rose'meyer (School of Medical Sciences), and Dr. P. Johnson and Prof. Nerida Smith (School of Pharmacy) for fruitful discussions about and revision of the manuscript.
REFERENCES
- 1.Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs: a systematic review. Drugs. 2001;61:2163–75. doi: 10.2165/00003495-200161150-00002. [DOI] [PubMed] [Google Scholar]
- 2.Naidu S, Wilkinson JM, Simpson MD. Attitudes of Australian pharmacists toward complementary and alternative medicines. Ann Pharmacother. 2005;39:1456–61. doi: 10.1345/aph.1G089. [DOI] [PubMed] [Google Scholar]
- 3.Dolder C, Lacro J, Dolder N, Gregory P. Pharmacists' use of and attitudes and beliefs about alternative medications. Am J Health-Syst Pharm. 2003;60:1352–7. doi: 10.1093/ajhp/60.13.1352. [DOI] [PubMed] [Google Scholar]
- 4.Koh HL, Teo HH, Ng HL. Pharmacists' patterns of use, knowledge, and attitudes toward complementary and alternative medicine. J Alternative Complementary Med. 2003;9:51–63. doi: 10.1089/107555303321222946. [DOI] [PubMed] [Google Scholar]
- 5.Brown CM, Barner JC, Shah S. Community pharmacists' actions when patients use complementary and alternative therapies with medications. J Am Pharm Assoc (Wash DC). 2005;45:41–7. doi: 10.1331/1544345052843011. [DOI] [PubMed] [Google Scholar]
- 6.Semple SJ, Hotham E, Rao D, Martin K, Smith CA, Bloustien GF. Community pharmacists in Australia: barriers to information provision on complementary and alternative medicines. Pharm World Sci. 2006;28:366–73. doi: 10.1007/s11096-006-9058-y. [DOI] [PubMed] [Google Scholar]
- 7.Dutta AP, Daftary MN, Egba PA, Kang H. State of CAM education in U.S. schools of pharmacy: results of a national survey. J Am Pharm Assoc. 2003;43:81–3. [PubMed] [Google Scholar]
- 8.Shields KM. Natural Product Education in Schools of Pharmacy in the United States. Am J Pharm Educ. 2003;67:43–8. [Google Scholar]
- 9.Mackowiak ED, Parikh A, Freely J. Herbal Product Education in United States Pharmacy Schools: Core or Elective Program? Am J Pharm Educ. 2001;65:1–6. [Google Scholar]
- 10.Brooks PM. It's time to plan our future health system. Med J Aust. 2005;183:545. doi: 10.5694/j.1326-5377.2005.tb07165.x. [DOI] [PubMed] [Google Scholar]
- 11.Owen D, Lewith GT. Teaching integrated care: CAM familiarisation courses. Med J Aust. 2004;181:276–8. doi: 10.5694/j.1326-5377.2004.tb06271.x. [DOI] [PubMed] [Google Scholar]
- 12.Brooks PM. Undergraduate teaching of complementary medicine. Med J Aust. 2004;181:275. doi: 10.5694/j.1326-5377.2004.tb06270.x. [DOI] [PubMed] [Google Scholar]
- 13.Yeo AS, Yeo JC, Yeo C, Lee CH, Lim LF, Lee TL. Perceptions of complementary and alternative medicine amongst medical students in Singapore–a survey. Acupunct Med. 2005;23:19–26. doi: 10.1136/aim.23.1.19. [DOI] [PubMed] [Google Scholar]
- 14.Hopper I, Cohen M. Complementary therapies and the medical profession: a study of medical students' attitudes. Altern Ther Health Med. 1998;4:68–73. [PubMed] [Google Scholar]
- 15.Greiner KA, Murray JL, Kallail KJ. Medical student interest in alternative medicine. J Altern Complement Med. 2000;6:231–4. doi: 10.1089/acm.2000.6.231. [DOI] [PubMed] [Google Scholar]
- 16.Sahar T, Sallon S. Attitudes and exposure of Israeli medical students to complementary medicine–a survey. Harefuah. 2001;140:907–10. 91. [PubMed] [Google Scholar]
- 17.Freymann H, Rennie T, Bates I, Nebel S, Heinrich M. Knowledge and Use of Complementary and Alternative Medicine among British Undergraduate Pharmacy Students. Pharm World Sci. 2006;28:13–8. doi: 10.1007/s11096-005-2221-z. [DOI] [PubMed] [Google Scholar]
- 18.Kreitzer MJ, Mitten D, Harris I, Shandeling J. Attitudes toward CAM among medical, nursing, and pharmacy faculty students: a comparative analysis. Altern Ther Health Med. 2002;8:44–47. 50-3. [PubMed] [Google Scholar]
- 19.Chez RA, Jonas WB, Crawford C. A survey of medical students' opinions about complementary and alternative medicine. Am J Obstet Gynecol. 2001;185:754–7. doi: 10.1067/mob.2001.117484. [DOI] [PubMed] [Google Scholar]
- 20.Wetzel MS, Kaptchuk TJ, Haramati A, Eisenberg DM. Complementary and alternative medical therapies: implications for medical education. Ann Intern Med. 2003;138:191–6. doi: 10.7326/0003-4819-138-3-200302040-00011. [DOI] [PubMed] [Google Scholar]
- 21.Witt CM, Brinkhaus B, Willich SN. Teaching complementary and alternative medicine in a reform curriculum. Forsch Komplementarmed. 2006;13:342–8. doi: 10.1159/000097437. [DOI] [PubMed] [Google Scholar]
- 22.Hewson MG, Copeland HL, Mascha E, Arrigain S, Topol E, Fox JE. Integrative medicine: implementation and evaluation of a professional development program using experiential learning and conceptual change teaching approaches. Patient Educ Counselling. 2006;62:5–12. doi: 10.1016/j.pec.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Hirschkorn KA. Exclusive versus everyday forms of professional knowledge: legitimacy claims in conventional and alternative medicine. Sociol Health Illness. 2006;28:533–57. doi: 10.1111/j.1467-9566.2006.00506.x. [DOI] [PubMed] [Google Scholar]
- 24.Elder W, Rakel D, Heitkemper M, et al. Using Complementary and Alternative Medicine curricular Elements to foster Medical student Self-Awareness. Acad Med. 2007;82:951–5. doi: 10.1097/ACM.0b013e318149e411. [DOI] [PubMed] [Google Scholar]
- 25.Gaylord SA, Mann JD. Rationales for CAM education in Health Professions Training Programs. Acad Med. 2007;82:927–33. doi: 10.1097/ACM.0b013e31814a5b43. [DOI] [PubMed] [Google Scholar]
- 26.Pearson NJ, Chesney MA. The CAM education Program of the National Center for Complementary and Alternative Medicine: An Overview. Acad Med. 2007;82:921–6. doi: 10.1097/ACM.0b013e31814a5014. [DOI] [PubMed] [Google Scholar]
- 27.Lee MA, Benn R, Wimsatt L, et al. Integrating Complementary and Alternative medicine Instruction into Health Professions Education: Organizational and Instructional Strategies. Acad Med. 2007;82:939–45. doi: 10.1097/ACM.0b013e318149ebf8. [DOI] [PubMed] [Google Scholar]
- 28.Sierpina VS, Schneeweiss R, Frenkel MA, Bulik R, Maypole Barriers J. Strategies, and lessons learned from Complementary and Alternative Medicine Curricular Initiatives. Acad Med. 2007;82:946–50. doi: 10.1097/ACM.0b013e31814a5092. [DOI] [PubMed] [Google Scholar]
- 29.Greenfield SM, Innes MA, Allan TF, Wearn AM. First year medical students' perceptions and use of complementary and alternative medicine. Complementary Ther Med. 2002;10:27–32. doi: 10.1054/ctim.2002.0501. [DOI] [PubMed] [Google Scholar]
- 30.Torkelson C, Harris I, Kreitzer MJ. Evaluation of a complementary and alternative medicine rotation in medical school. Alternative Ther Health Med. 2006;12:30–4. [PubMed] [Google Scholar]
- 31.Cornman BJ, Carr CA, Heitkemper MM. Integrating CAM into nursing curricula: CAM camp as an educational intervention. Explore. 2006;2:226–31. doi: 10.1016/j.explore.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 32.Stratton TD, Benn RK, Lie DA, Zeller JM, Nedrow AR. Evaluating CAM Education in Health Professional Programs. Acad Med. 2007;82:956–61. doi: 10.1097/ACM.0b013e31814a5152. [DOI] [PubMed] [Google Scholar]
- 33.Mills E, Hollyer T, Saranchuk R, Wilson K. Teaching Evidence-Based Complementary and Alternative Medicine (EBCAM); changing behaviours in the face of reticence: a cross-over trial. BMC Med Educ. 2002;2:2. doi: 10.1186/1472-6920-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frenkel M, Ben Arye E. The growing need to teach about complementary and alternative medicine: questions and challenges. Acad Med. 2001;76:251–4. doi: 10.1097/00001888-200103000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Frenkel M, Frye A, Heliker D, et al. Lessons learned from complementary and integrative medicine curriculum change in a medical school. Med Educ. 2007;41:205–13. doi: 10.1111/j.1365-2929.2006.02654.x. [DOI] [PubMed] [Google Scholar]
- 36.Grollman AP. Alternative medicine: the importance of evidence in medicine and in medical education. Is there wheat among the chaff? Acad Med. 2001;76:221–3. doi: 10.1097/00001888-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Sampson W. The need for educational reform in teaching about alternative therapies. Acad Med. 2001;76:248–50. doi: 10.1097/00001888-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Forjuoh SN, Rascoe TG, Symm B, Edwards JC. Teaching medical students complementary and alternative medicine using evidence-based principles. J Altern Complement Med. 2003;9:429–39. doi: 10.1089/107555303765551651. [DOI] [PubMed] [Google Scholar]
- 39.Biggs J. Teaching for Quality Learning at University. 2nd ed. Maidenhead, Berkshire UK: The society for research into Higher Education & Open University Press; 2003. [Google Scholar]
- 40.Wallace C, Franson K. Incorporation of Ability-Based Outcome Education into Pharmacotherapeutics Using an Expanded S.O.A.P. Format (Galley. American Journal of Pharmaceutical Education. 1996;60:87–93. [Google Scholar]
- 41.Grbich C. Qualitative Research in Health. Sydney: Allen & Unwin; 1999. [Google Scholar]
- 42.Lie D, Boker J. Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Med Educ. 2004;4:2. doi: 10.1186/1472-6920-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilkinson JM, Simpson MD. Complementary therapy use by nursing, pharmacy and biomedical science students. Nurs Health Sci. 2001;3:19–27. doi: 10.1046/j.1442-2018.2001.00067.x. [DOI] [PubMed] [Google Scholar]
- 44.Hon EK, Lee K, Tse HM, et al. A survey of attitudes to traditional Chinese medicine in Hong Kong pharmacy students. Complement Ther Med. 2004;12:51–6. doi: 10.1016/j.ctim.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Kemper KJ, Amata-Kynvi A, Dvorkin L, et al. Herbs and other dietary supplements: healthcare professionals' knowledge, attitudes, and practices. Alternative Ther Health Med. 2003;9:42–49. [PubMed] [Google Scholar]
- 46.Lie DA, Boker J. Comparative survey of Complementary and Alternative Medicine (CAM) attitudes, use, and information-seeking behaviour among medical students, residents & faculty. BMC Med Educ. 2006;6:58. doi: 10.1186/1472-6920-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harris IM, Kingston RL, Rodriguez R, Choudary V. Attitudes towards complementary and alternative medicine among pharmacy faculty and students. Am J Pharm Educ. 2006;70(6) doi: 10.5688/aj7006129. Article 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shah B, Siganga W, Mallaya U, Shah S. Pharmacy student perspectives on classroom education about herbal supplements. Am J Pharm Educ. 2005;69(5) Article 102. [Google Scholar]
- 49.Hartigan-Rogers JA, Cobbett SL, Amirault MA, Muise-Davis ME. Nursing graduates' perceptions of their undergraduate clinical placement. Int J Nurs Educ Scholarship. 2007;4 doi: 10.2202/1548-923X.1276. Article 9. [DOI] [PubMed] [Google Scholar]
- 50.Marriott J, Taylor S, Simpson M, et al. Australian national strategy for pharmacy preceptor education and support. Aust J Rural Health. 2005;13:83–90. doi: 10.1111/j.1440-1854.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 51.Saini B, Smith L, Armour C, Krass I. An educational intervention to train community pharmacists in providing specialized asthma care. Am J Pharm Educ. 2006;70(5) doi: 10.5688/aj7005118. Article 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tucker K, Wakefield A, Boggis C, Lawson M, Roberts T, Gooch J. Learning together: clinical skills teaching for medical and nursing students. Med Educ. 2003;37:630–7. doi: 10.1046/j.1365-2923.2003.01558.x. [DOI] [PubMed] [Google Scholar]
- 53.Lumague M, Morgan A, Mak D, et al. Interprofessional education: the student perspective. J Interprofessional Care. 2006;20:246–53. doi: 10.1080/13561820600717891. [DOI] [PubMed] [Google Scholar]
- 54.McNair R, Stone N, Sims J, Curtis C. Australian evidence for interprofessional education contributing to effective teamwork preparation and interest in rural practice. J Interprofessional Care. 2005;19:579–94. doi: 10.1080/13561820500412452. [DOI] [PubMed] [Google Scholar]
- 55.Breach J. How much education is enough? Aust J Pharm. 2006;87:62–3. [Google Scholar]