Abstract
Objective
To determine fourth-year Canadian pharmacy students' knowledge of herbal medicine and whether that knowledge is associated with mandatory instruction in herbal medicine.
Methods
Standardized multiple-choice tests assessing students' herbal knowledge were distributed to all fourth-year BSc pharmacy students at 5 pharmacy schools in Canada.
Results
The Quebec response rate was too low to include in the analysis. Herbal knowledge test scores were positively associated with having previously taken an herbal medicine class and completion of a pharmacy practicum. However, postsecondary education, age, and gender were not associated with herbal knowledge test scores. Students at the University of British Columbia had the highest score, followed by Alberta, Nova Scotia, and Ontario.
Conclusion
Pharmacy students' knowledge of herbal medicine varies depending on the school attended and higher herbal knowledge test scores appear to be most closely related to mandatory herbal instruction.
Keywords: herbal supplements, complementary and alternative medicine, assessment
INTRODUCTION
According to the Natural Health Products Directorate (NHPD), 71% of Canadians have taken a natural health product1 such as herbal remedies; traditional Chinese medicine, Ayurvedic, Native North American medicines; homeopathic medicines; and supplements such as probiotics, amino acids, essential fatty acids, vitamins and minerals.2 As the demand grows, more pharmacists have begun to stock natural health prodcuts in their pharmacies. In 1999, the growth of natural health products sales in US pharmacies was surpassed only by the growth of Internet and practitioner-direct sales. By 2003, US expenditures on natural health products were estimated at $1.4 billion.3,4 Together with the increase in sales has come an increase in the number of consumer inquiries. Consumers are looking to pharmacists for evidence-based information about natural health products.3,5-9 The purpose of this study was to assess the herbal medicine knowledge of graduating Canadian pharmacy students and to explore factors that might be associated with increased herbal medicine knowledge. Herbal medicine was chosen as the topic of focus because herbs are commonly used and frequently identified as a key area where pharmacists' knowledge is lacking.5,10-12 The popularity of herbal medicines 1,13,14 and their increasing clinical importance9,15-19 were the 2 driving factors for initiating this study.
Since most natural health products sold in Canada and the United States are purchased from pharmacies,3,20,21 the pharmacist's role with respect to natural health products is important to consider.5,14 As health care professionals, it has been argued that pharmacists should be able to provide information about all the products stocked in their pharmacies—patients expect it, and ask questions.3,6,7,9,12,20,21 Professional associations such as the Canadian Society of Hospital Pharmacists (CSHP), the American Society of Health-System Pharmacists,22 and the American College of Clinical Pharmacy (ACCP) have each stated that pharmacists' responsibility to improve medication safety by monitoring and preventing adverse interactions includes the risks posed by herb-drug interactions.9,19,23 The problem, however, is that many pharmacists appear to graduate with little knowledge of natural health products, making them ill-equipped to implement these recommendations.11,18,24 Aware of this knowledge deficit, these organizations have released position papers advocating for more complementary and alternative medicine (CAM) education for pharmacists in their undergraduate schooling, asserting that without this education pharmacists cannot completely fill their role as information providers to their patients.9,19,23
The North American Pharmacist Licensure Examination (NAPLEX) has added a competency that specifically addresses knowledge of dietary supplements (natural health products are referred to as dietary supplements in the United States).25 Also in 2005, the Accreditation Council for Pharmacy Education released a draft of revised standards and guidelines that included patient use of dietary supplements, CAM treatments, the safety and efficacy of CAM, and drug-herb interactions.26 Finally, the Pharmacy Examining Board of Canada (PEBC), which is the national certification board for pharmacists in Canada, recommends that students planning to take the Qualifying Examination or the Evaluating Examination become competent in the subject of CAM.27,28
Pharmacists themselves have identified their lack of knowledge about natural health products, especially in the areas of mechanisms of action, adverse effects, drug interactions, and dosage.3,5,10,12,18,22, 29 However, most of the studies to date have evaluated only self-reported knowledge.3 Of the 3 studies that tested knowledge, 1 had a small sample size (N =18) and only 6 test questions.10 Another study had a larger sample size (N = 537) and multiple-choice questions, but only 46 of the participants were pharmacists (the others were physicians, advanced practice nurses, and dietitians).29 The third study (N = 164) had 15 true-or-false questions, giving respondents a 50% chance of guessing correctly.5 Furthermore, all previous surveys were administered in an informal setting where it may have been possible for participants to discuss their answers with colleagues. Our study addresses these gaps by testing the herbal knowledge of Canadian pharmacy students at the end of their formal training (prior to graduation) using a standardized test format with 14 multiple-choice questions to directly assess what the participants know.
METHODS
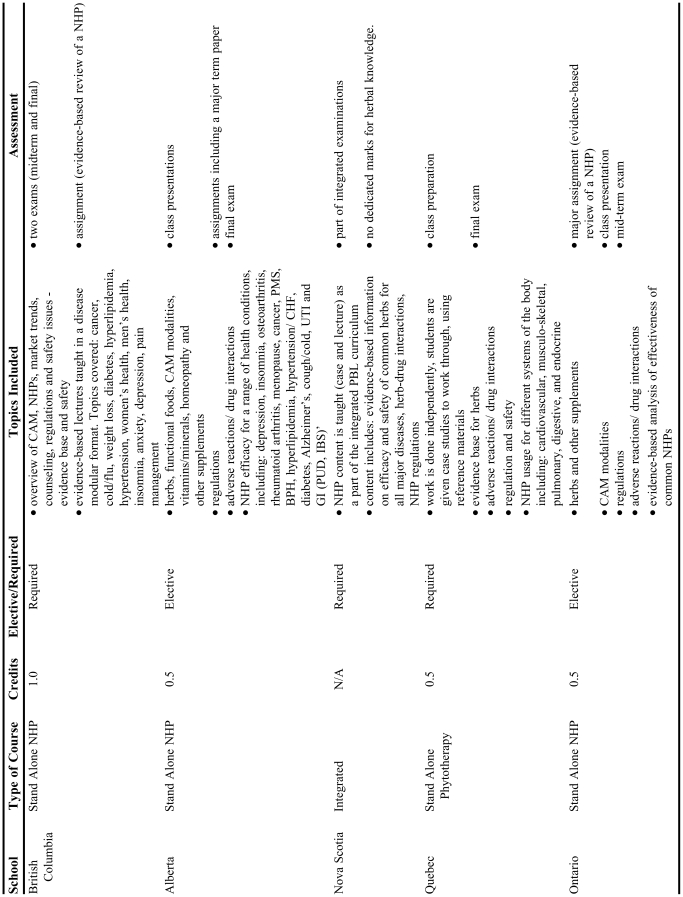
A review of herbal medicine instruction at 4 Canadian schools was undertaken to provide background for the test instrument design. A summary of these courses is presented in Table 1. The course materials cover a range of natural health products and complementary/alternative medicine therapy content, including the adverse effects and drug interactions associated with natural health products. The standalone courses assessed the students' herbal knowledge via examinations and assignments, but there is no designated assessment specific to natural health products in the one school (Nova Scotia) that is currently teaching a fully integrated curriculum.
Table 1.
Summary of Herbal Course Material at Selected Canadian Pharmacy Schools
A standardized multiple-choice test was designed to assess students' knowledge of the safety and efficacy of common herbal products (Appendix 1). To create the test, instructors of courses with herbal medicine content were identified at each participating university. Each instructor shared sample questions and topic ideas that reflected the content and style of questions they have previously used on herbal medicine examinations. Fourteen questions assessing knowledge of efficacy, safety, and regulation of herbal medicines were designed based on the availability of the evidence to support the correct answer.
The draft test was pilot tested by a group of individuals (n=23) with a broad education base. As predicted, naturopathic doctors scored highest overall (mean score = 71%), followed by recent pharmacy graduates (mean score = 50%), and people employed in nonhealth-related fields scored lowest (mean score = 37%). During this process, the test questions were also analyzed for “test-wiseness.”30 Question distracters that seemed obvious (eg, questions that participants with little or no training consistently guessed correctly) were modified to be more challenging and/or congruous with the other distracters. Feedback received from participants (eg, comments regarding clarity of wording) was also taken into account. The pilot test demonstrated that the herbal knowledge test could be completed in 10 minutes or less. The test was translated into French (and then back translated) for distribution to students in Quebec.
In the final phase of the project, the entire populations of fourth-year (final year) BSc pharmacy students at 5 schools across Canada (approximately 650 students) were asked to participate in the study. The schools were located in each of the following provinces: British Columbia, Alberta, Nova Scotia, Ontario, and Quebec. Seniors were selected because they were near the end of their formal pharmacy education and it seemed unlikely that their knowledge of herbal medicine would significantly change before they began practice. Schools of pharmacy were selected from across the country because it was predicted that there may be significant variability in knowledge between the students at different schools due to differences in herbal curricula and provincial culture.
To ensure that students did not feel coerced to participate, tests were administered by personnel who were not connected with evaluating or grading students in the pharmacy curriculum. Hard copies of tests were distributed to the entire cohort of final year students in core classes (wherever possible) between December 2006 and May 2007. Each test paper was assigned a code number to protect the identity of participating students. Participation was encouraged by entering all students into a drawing for a $100.00 cash prize. In addition, as an incentive to encourage students to do their best, the student from each school with the highest test score was awarded a $100.00 prize (except at the Nova Scotia school).
Student scores were entered into the Statistical Package for Social Sciences (SPSS), Version 14.0, for Windows. Data were then cleaned using frequency tables to check for blanks and nonsensical numbers (eg, an age of 100 years). Two-tailed t tests were used to test the association of the continuous variable “test score” with dichotomous variables (eg, gender, completion of practical experience, previously taken herbal medicine class, age group, total number of years of post-secondary education) and analysis of variance was used for assessing the association between continuous measurement and polytomous variables. Linear regression analysis was used to determine the relative impact of all the variables that were found to be significantly associated with test score in the bivariate analyses. SPSS was used to carry out all the analyses. All tests were two-sided, and p values less than 0.05 were considered statistically significant. Ethical approval was obtained from the ethics boards at each of the 5 universities that participated in the study.
RESULTS
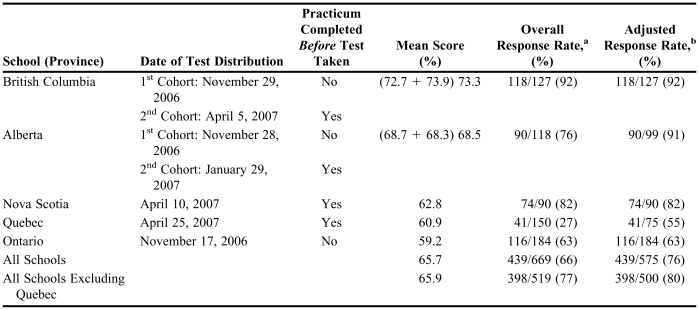
Quebec had the lowest overall response rate (27%) due to logistical challenges with distributing the questionnaire. The low response rate at the Quebec school meant that there was not sufficient power to draw conclusions about the Quebec students' knowledge and thus their data were eliminated from further analyses. All students were in the final year of their pharmacy undergraduate (BSc) degree, and the mean age of participants for all schools was 24.5 years. Overall, the response rate, excluding the Quebec sample, was good: 77% of fourth-year students at all schools participated and 80% of those who received the survey instrument responded (Table 2). British Columbia had the highest response rate with 92% of students participating. Ontario had the lowest response rate (63%) of the schools included in the analysis because many students were not present for class the day the test was distributed. Almost all Ontario students who did attended class that day volunteered to take the test. Eighty-two percent of students from Nova Scotia participated, and the overall response rate for Alberta was 76%.
Table 2.
Mean Scores and Response Rates for Each School
aNumber of students who took the test/all 4th year students enrolled at that school
bNumber of students who took the test/students enrolled in the class in which the test was given. Accounts for schools where test was not given in core class, and some students did not have the opportunity to take the test. Does not account for students who skipped class the day of the test
The overall mean test score for all schools was 65.9%, with students correctly answering 9.2 out of 14 knowledge questions on average (Table 2). Students from the schools with the highest attendance in a course devoted exclusively to herbal medicine (ie, British Columbia and Alberta) had the highest mean herbal knowledge test scores. Students from schools without such a course (ie, Nova Scotia), or without a high attendance at such a course (ie, Ontario), had lower mean test scores. To better understand the relevance of each school's mean score, we obtained the overall fourth-year grade averages for the British Columbia, Alberta, and Ontario schools (Nova Scotia averages were not available). Overall, students' scores on the herbal knowledge test were markedly lower than their overall yearly grade averages, except in British Columbia.
An ANOVA showed that the schools' mean test scores were significantly different (p < 0.001). Post-hoc analyses using pairwise comparison with Bonferroni correction corroborated the ANOVA, showing that the British Columbia scores were, on average, significantly highest, followed by those of Alberta, Nova Scotia, and Ontario (p < 0.05). There was no statistical difference between the Ontario and Nova Scotia scores.
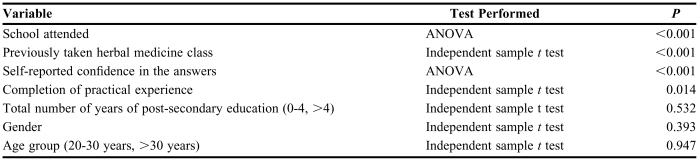
Test scores were positively and significantly associated with having previously taken an herbal medicine class (p = 0.01, R2 = 0.172), self-reported confidence in herbal knowledge (p < 0.001, R2 = 0.231), and completion of practical experience training (p < 0.05, R2 = 0.185). There was no association found between tests scores and age, gender, or total number of years of post-secondary education (Table 3).
Table 3.
Correlation of Herbal Test Score with Other Variables
A linear regression was performed to assess whether previously taken herbal class, school attended, or completion of practical experience training accounted for the majority of the differences seen in test scores. Adjusting for the effect of school (using dummy variables), on average, students who had taken an herbal class scored 6% higher than those who had not, and students who had completed their practical experience scored 2% higher than those who had not. Alberta students who said they had taken the herbal course scored the same as those who said they had not (69% vs. 68%). However, Ontario students who reported taking the elective scored higher than those who said they had not (75% vs. 58%). A second series of linear regression was run, excluding one school at a time, to asses the robustness of the relative impact of the key variables identified in the previous regression. Adjusting for the effect of school, each time, the results remained consistent, with having taken an herbal class accounting for most of the difference in scores (p < 0.05).
DISCUSSION
Overall, the test results appear to be closely related to whether students took an herbal medicine class. Results could also be influenced by 3 other factors: whether students had completed their pharmacy practical experience; anomalies in how the test was conducted at each school, and/or whether residents of different provinces have more background knowledge of herbals. Each of these points is explored in detail, along with a discussion of the applicability of the results to practice.
Whether a student had taken an herbal class was the most significant factor associated with how well they performed on the herbal medicine knowledge test. British Columbia and Alberta are the schools that had the highest enrollment in an herbal class—either because it is mandatory or a well-attended elective—and these were the schools with the highest mean herbal medicine knowledge scores. Our review of the herbal curricula of each school (Table 1) helps to explain our data, showing that the schools with the highest attendance in classes in which a large amount of material on natural health products was presented scored the highest.
A key discussion point is whether a 6% difference in scores between students with or without an herbal course translates to a significant difference in practice. Given that the test evaluated the most basic knowledge of herbs, it is not surprising that there was such a small difference between the scores of those who had taken a dedicated course on herbs and those who had not. Ultimately, this may be a positive finding from the patient perspective because it means that in many pharmacy schools, even students who do not take an herbal course still graduate with basic knowledge about common herbs. Had the test been longer, and evaluated other, more complicated safety, efficacy, and regulatory issues, the gap between students with and without additional specialized training in natural health products may have been wider. What our test shows is that graduates of some pharmacy schools have modest knowledge about common herbs and that this is an issue that needs to be addressed. Students scores on an assessment of basic knowledge herbal products are generally lower than their average academic results on other topics. Our results suggest that a mandatory course with herbal content could be the answer.
Whether or not a student completed their pharmacy practical experience was also a significant factor associated with how well they performed on the herbal medicine knowledge test. It was postulated that completion of a pharmacy practicum could affect test scores because students might familiarize themselves with some of the more common herbs as part of the practicum experience, and our analysis supports this hypothesis.
Differences in curriculum designs among the pharmacy schools in the study allowed us to explore the impact of pharmacy practicum on herbal knowledge test scores. Table 2 shows that in both British Columbia and Alberta, mean test scores for students were essentially the same regardless of whether or not students had completed their practicum. This would suggest that, contrary to our hypothesis, completion of pharmacy practicum prior to taking the herbal knowledge test did not appear to have an effect on the test score. However, in Alberta, 1 group had the herbal course and no practicum, while the other group had the practicum but no herbal course. Since our results indicate that both may have influenced the test scores, this could explain why the 2 groups of Alberta students scored so similarly. In contrast, students in the second cohort in British Columbia had completed both an herbal course and a practicum.
At the Nova Scotia school, all students who participated had already completed their practicum, and their lower scores would also seem to contradict our hypothesis. In contrast, Ontario students were given the herbal knowledge test immediately prior to beginning their pharmacy practicum, and this lack of a practicum might account for the Ontario students' relatively low scores, but there may also be other factors that we have not yet identified.
Due to the specific directives of different ethics boards, as well as various curricular constraints at each school, the test was not distributed in a uniform manner across schools, which may have affected test scores. In fact, the school with the highest score, British Columbia, was the only school where the test administration methods were executed exactly as planned.
In Alberta, the ethics board required that the tests be given out at the end of class instead of at the beginning, to give students the opportunity to leave if they did not want to participate. This may have decreased the response rate, and increased the mean, as the students who stayed to participate may have been more interested/knowledgeable in herbal medicine.
Many students at the Nova Scotia school did not fully complete the test, leaving, in some cases, up to 13 questions blank. This pattern of not completing the test was not seen at the other schools and may have been because the performance incentive (highest scoring students entered in a draw for a $100 prize) was forbidden by the ethics board in Nova Scotia, and therefore not offered at this school. However, overall participation rates in the study were comparable to other schools.
In Quebec, the tests were given out at the end of a pharmacotherapy examination, instead of at the beginning of a core class. This was due to curricular constraints, and likely considerably decreased the response rate and mean score, as the students who stayed after the examination to participate may have been tired and less focused on completing another test, especially one that did not confer any academic benefit. Due to these adverse conditions and the very low response rate, it is not possible to draw any concrete conclusions on the herbal knowledge of the Quebec students.
In Ontario, almost all students present in the class participated in the test, but only approximately 60% of students enrolled in the class were present. There is no way of knowing whether the students who missed class had a higher or lower knowledge of herbals than those who attended.
Overall, it is likely that the inconsistencies in test distribution lowered the response rates and may have affected mean test scores, perhaps with the exception of Alberta, where the students who volunteered to complete the test at the end of class may have had more interest and knowledge about herbal medicine. A key challenge for future studies of this nature is to better standardize the administration of the tests.
The culture of a province with respect to natural health product use may also have influenced the students' scores on the test. How much a population in a certain part of Canada collectively endorses the use of natural health products may affect how much general knowledge residents have simply due to their lifetime exposure to public information about herbal products.
A 2005 national survey assessing the use of natural health products in Canada found that residents of British Columbia and Alberta were the most likely to say they used a natural health product on a daily basis.1 In contrast, Atlantic Canadians and Quebeckers were more likely to be seasonal users of natural health products. Atlantic Canadians were more likely to be unfamiliar with natural health products, whereas British Columbia, Quebec, and Ontario residents were more likely to rate themselves as very familiar with natural health products. Atlantic Canadians also reported the lowest personal use of NHPs.1 The schools that scored the highest were situated in provinces with the most frequent use of natural health products, so it would make sense for students in these provinces to have more background knowledge; however, it is not clear if that made a significant difference to students' performance on our test. In addition, based on the 2005 survey finding that Ontarians identified themselves as very familiar with natural health products and yet students in Ontario produced the lowest average test scores, it would seem that provincial culture cannot predict pharmacy students' scores as well as having completed a course with herbal content.
This study was based on the assumption that pharmacy students who performed poorly on our standardized test of herbal knowledge would be unable to identify and prevent drug-related problems associated with herbal medicines. It is possible that this may be a false assumption, given the ease with which health product information on a variety of topics can be obtained from textbooks or evidence-based online databases. However, it could be argued that pharmacists still require fundamental knowledge in order to know how to evaluate the safety and effectiveness of an herbal product in a timely manner. Given the busy work settings of most pharmacists, it may not be possible to take the time to search for information to answer every patient question about herbal medicine. Thus, basic knowledge of the efficacy of common herbs and key safety issues (ie, herbs with “red flags” or specific known drug interactions) appears to be necessary in order for pharmacists to adequately counsel patients in an efficient manner. For example, St. John's wort is known to have a clinically significant interaction with warfarin and thus patients should routinely be counseled to avoid this combination.31-33
Based on our data, it is not possible to say with confidence which style of herbal instruction is the best. However, it appears that ensuring specific teaching about herbs needs to occur in a manner such that all students are exposed to the topic. Further research needs to explore the impact of different educational strategies for teaching this topic.
As alluded to above, this study suffered from several methodological limitations such as distributing the test at different times of the year for each school, the variety of venues in which the tests were distributed, and the incentives offered. Additional limitations may include a self-selection bias. Students who voluntarily completed the test may not be representative of other fourth-year students in that they may have had a greater interest in and thereby greater knowledge of herbal medicine. Furthermore, because this test did not count towards academic standing, students may not have given their best effort, potentially resulting in an inaccurate assessment of their knowledge. The performance incentive was provided to minimize this effect. Another topic for discussion is whether this test is a valid test of herbal knowledge. The results of our pilot test support the test's face validity. Moreover, the questions that were used on the test are similar to those that have already been used on examinations at 4 different Canadian universities. All of these points support the validity of the test to adequately assess pharmacy students' knowledge; however, a longer test would have been able to assess a wider range of herbal knowledge.
One additional limitation of the test was that it was comprised of only 14 questions, thus restricting our ability to test knowledge of a wide variety of products. We believe that the test is still instructive because the questions were primarily related to efficacy and safety, which are the 2 primary domains of a pharmacists' scope of practice. Thus, while the test was not long, it assessed the basic knowledge that it was designed to test. The results may not indicate that students with higher scores have sufficient knowledge, but they do signify that there probably is a gap in the herbal curricula of the schools that did not perform as well.
CONCLUSIONS
A test of fourth-year BSc pharmacy students at Canadian pharmacy schools found that students who had taken an herbal course scored higher on average than those who had not. Thus, taking a course devoted to natural health products appears to be associated with a higher knowledge of selected herbal medicines. Based on this finding, we recommend required herbal content for all pharmacy undergraduates to better equip them in this area when they enter the workplace. Knowledge of herbal medicine is necessary so that pharmacists can help patients make more informed decisions about herbal therapy options.
ACKNOWLEDGEMENTS
Thanks to Jean-Louis Brazier for his assistance with data collection. Thanks also to Julie DeCourval, Karine April Toupin, and Aude Motulsky for their invaluable translation services.
This study was partially funded by a Canadian Institutes for Health Research Partnerships for Health System Improvement grant and by the Advanced Foods and Materials Network National Centre of Excellence.
Appendix 1. Example Test Questions
5. Which of the following herbs are most likely to affect the blood's ability to clot if taken together with an anti-coagulant medication?
a. Garlic, ginkgo, chamomile
b. Garlic, ginkgo, St. John's wort
c. Garlic, saw palmetto, St. John's wort
d. Garlic, ginkgo, Echinacea
Correct Answer: B
6. Your best friend takes Echinacea regularly to prevent colds and flus. Your advice to her should be:
a. Stop taking Echinacea because several studies have shown that Echinacea does not seem to prevent colds and flus.
b. Stop taking Echinacea because it is expensive and it seems to only stop you from getting colds; you can still get the flu
c. Keep taking Echinacea, but make sure you buy a standardized extract
d. Keep taking Echinacea because several studies have shown that Echinacea is able to prevent both colds and flus.
Correct Answer: A
13. If a female patient was already taking an oral contraceptive (i.e., birth control pill), what best describes the advice you would provide to her regarding St. John's wort?
a. She should take her St. John's wort one hour before or two hours after taking her oral contraceptive so they will not interact.
b. St. John's wort may increase the metabolism of her oral contraceptive so she must speak with her doctor before taking them together.
c. St. John's wort may decrease the metabolism of her oral contraceptive so she must speak with the doctor before taking them together.
d. Early evidence suggested that there may be an interaction between St. John's wort and oral contraceptives, but the most recent evidence indicates that this is no longer a concern.
Correct Answer: B
Note: Complete test is available from the corresponding author
REFERENCES
- 1.Natural Health Products Directorate. Natural Health Products Directorate; 2005. Baseline natural health products survey among consumers: final report. [Google Scholar]
- 2.Health Canada. Information: Natural Health Products Regulations, FAQ's. Health Canada. Available at: http://www.hc-sc.gc.ca/ahc-asc/media/nr-cp/2003/2003_47bk4_e.html. Accessed June 27, 2007.
- 3.Clauson KA, McQueen CE, Shields KM, Bryant PJ. Knowledge and attitudes of pharmacists in Missouri regarding natural products. Am J Pharm Educ. 2003;67(2) article 41. [Google Scholar]
- 4.Johnsen M. Despite controversy over credibility, dietary supplement sales surge - OTC/Natural Health. Drug Store News. Available at: http://findarticles.com/p/articles/mi_m3374/is_10_25/ai_108969661. Accessed June 27, 2007.
- 5.Chang ZG, Kennedy DT, Holdford DA, Small RE. Pharmacists' knowledge and attitudes toward herbal medicine. Ann Pharmacother. 2000;34:710–5. doi: 10.1345/aph.19263. [DOI] [PubMed] [Google Scholar]
- 6.Dolder C, Lacro J, Dolder N, Gregory P. Pharmacists' use of and attitudes and beliefs about alternative medicine. Am J Health-Syst Pharm. 2003;60:1352–7. doi: 10.1093/ajhp/60.13.1352. [DOI] [PubMed] [Google Scholar]
- 7.Welna EM, Hadsall RS, Schommer JC. Pharmacists' personal use, professional practice behaviours, and perceptions regarding herbal and other natural products. J Am Pharm Assoc. 2001;43:602–11. doi: 10.1331/154434503322452247. [DOI] [PubMed] [Google Scholar]
- 8.Evans E, Evans J. Changes in pharmacy students' attitudes and perceptions toward complementary and alternative medicine after completion of a required course. Am J Pharm Educ. 2006;70(5) doi: 10.5688/aj7005105. article 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller LG, Hume A, Harris IM, et al. White Paper on Herbal Products. Pharmacotherapy. 2000;20:877–91. doi: 10.1592/phco.20.9.877.35200. [DOI] [PubMed] [Google Scholar]
- 10.Rickert K, Martinez RR, Martinez TT. Pharmacist knowledge of common herbal preparations. Proc West Pharmacol Soc. 1999;42:1–2. [PubMed] [Google Scholar]
- 11.Bupendra S, Walter S, Usha M, Sonalee S. Pharmacy Student Perspectives on Classroom Education About Herbal Supplements. Am J Pharm Educ. 2005;69(5) Article 102. [Google Scholar]
- 12.Dvorkin L, Gardiner P, Whelan JS. Herbal medicine course within pharmacy curriculum. J Herb Pharmacother. 2004;4:47–58. [PubMed] [Google Scholar]
- 13.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in Alternative Medicine Use in the United States, 1990-1997: Results of a Follow-up National Survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 14.Bouldin AS, Smith MC, Garner DD, Szeinbach SL, Frate DA, Croom EM. Pharmacy and herbal medicine in the US. Soc Sci Med. 1999;49:279–89. doi: 10.1016/s0277-9536(99)00118-5. [DOI] [PubMed] [Google Scholar]
- 15.Smolinske SC. Herbal product contamination and toxicity. J Pharm Pract. 2005;18:188–208. [Google Scholar]
- 16.Lenz KL. Developing a pharmacy curriculum in complementary and alternative medicine. J Pharm Pract. 1999;12:178–86. [Google Scholar]
- 17.Stenton SB, Bungard TJ, Ackman ML. Interactions between Warfarin and herbal products, minerals, and vitamins: a pharmacists' guide. Can J Hosp Pharm. 2001;54:184–90. [Google Scholar]
- 18.Shields KM, McQueen CE, Bryant PJ. Natural product education in schools of pharmacy in the United States. Am J Pharm Educ. 2003;67(1) Article 108. [Google Scholar]
- 19.American Society of Health-System Pharmacists. American Society of Health-System Pharmacists' statement on the use of dietary supplements. Am J Health-Syst Pharm. 2004;61:1707–11. doi: 10.1093/ajhp/61.16.1707. [DOI] [PubMed] [Google Scholar]
- 20.Bokma A. What's up with herbals. Pharm Practice. 2000;16:54–61. [Google Scholar]
- 21.Levy S. ‘Healthcare 2000’ Reveals Consumer View of R.Ph.s. Drug Topics. 1999;143:64. October 4, [Google Scholar]
- 22.ASHP. American Society of Health-System Pharmacists' statement on the use of dietary supplements. Am J Health-Syst Pharm. 2004;61:1707–11. doi: 10.1093/ajhp/61.16.1707. [DOI] [PubMed] [Google Scholar]
- 23.Boon H. Information Paper: The Role of the Pharmacist With Respect to Complementary/ Alternative Medicine: Canadian Society of Hospital Pharmacists Official Publications; 2001.
- 24.Scott CJ, Riedlinger J. Promoting education about complementary or alternative medicine. Am J Health-Syst Pharm. 1998;55:2525–7. doi: 10.1093/ajhp/55.23.2525. [DOI] [PubMed] [Google Scholar]
- 25.National Association of Boards of Pharmacy. Updated NAPLEX Blueprint and New Passing Standard. Available at: http://www.nabp.net/ftpfiles/NABP01/Updatedblueprintinfo.pdf. Accessed June 27, 2007.
- 26.Accreditation Council for Pharmacy Education. Draft Revision of ACPE Standards 2000 and Proposed Guidelines. Available at: http://www.acpe-accredit.org/pdf/ACPEDraftRevisedStandardsandGuidelinesJune2005final.pdf. Accessed June 27, 2007.
- 27.The Pharmacy Examining Board of Canada. The Qualifying Examination Booklet. The Pharmacy Examining Board of Canada. Available at: http://www.pebc.ca/EnglishGraphics/QualBookletEng.pdf. Accessed July 24, 2007.
- 28.The Pharmacy Examining Board of Canada. Evaluating Examination Syllabus. The Pharmacy Examining Board of Canada. Available at: http://www.pebc.ca/EnglishGraphics/Syllabus2007.pdf. Accessed July 23, 2007.
- 29.Kemper KJ, Amata-Kynvi A, Dvorkin L, et al. Herbs and other dietary supplements: healthcare professionals' knowledge, attitudes, and practices. Altern Ther Health Med. May/June 2003;9:42–9. [PubMed] [Google Scholar]
- 30.Mahamed A, Gregory PAM, Austin Z. “Testwiseness” Among international pharmacy graduates and Canadian senior pharmacy students. Am J Pharm Educ. 2006;70(6) doi: 10.5688/aj7006131. Article 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brinker F. Herb Contraindications and Drug Interactions. 3rd ed. Eclectic Medical Publishers; 2001. [Google Scholar]
- 32.Henney JE. Risk of drug interactions with St. John's wort. JAMA. 2000;283:1679. [Google Scholar]
- 33.McIntyre M. A review of the benefits, adverse events, drug interactions, and safety of St. John's Wort. J Altern Complement Med. 2000;6:115–24. doi: 10.1089/acm.2000.6.115. [DOI] [PubMed] [Google Scholar]