Abstract
Purpose
To examine attitudes toward exercise among a vulnerable aged population characterized by low socioeconomic status, poor functional status and lack, of available therapeutic exercise resources.
Method
This cross-sectional survey among public low-income housing residents (n = 94), aged > 70 years utilizes these assessments: Physician-based Assessment & Counseling for Exercise (PACE) scale, exercise self-efficacy score, Short Physical Performance Battery (SPPB), Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL.) scales.
Results
Readiness to exercise differed significantly (p < 0.001) across physical performance levels and ADL and IADL groups. Exercise self-efficacy also differed significantly (p < 0.001) across performance levels. The highest performance level (score 7–12) had a significantly (p < 0.05) higher Self-efficacy score (x̄ = 7.0 ± 2.8) than the medium performance level (score 4–6) (x̄ = 5.3±2.8) and the lowest performance level (0–3) (x̄= 4.3 ±: 2.5) groups. Exercise self-efficacy also differed significantly (p < 0.001) across ADL and IADL groups, However, interest in home-based or class-based exercise participation was high among all groups. More than 70% of subjects reported interest with no significant difference noted among groups.
Conclusion
Attitudes toward exercise are significantly associated with observed physical function and self-reported disability among vulnerable older adults living in public low-income housing.
Keywords: Aging, activities of daily living, disability, exercise, attitudes, mobility, self-efficacy, health promotion
Introduction
Due to increasing life expectancy, the population of older adults in the USA is rising rapidly. Consequently, considerable public health interest has focused on preserving health interest has focused on preserving health and independent function in older age groups. The general benefits of regular physical activity and exercise are well documented [1–4]. Analyses from the Established Populations for Epidemiologic Studies of the Elderly (EPESE) revealed nearly a two-fold increased likelihood of living a long life without disability among the most physically active persons aged 65 or older compared to those who were sedentary [5. In part, it is this recognition of the relationship between physical activity and disability that has led to the interest in exercise as therapy for older adults at risk for disability.
A challenge in creating and targeting therapeutic exercise interventions is linking these to clinical tools that appropriately screen patients at the greatest risk for functional decline and disability. Clinical questionnaires addressing activities of daily living have been commonly used but do not address individuals who are at risk but have yet to develop overt disability [6]. Recent reports and editorials have identified mobility performance measures as important screening tools for those at risk for developing disability. This is largely based upon work by Guralnik and colleagues that demonstrated that the Short Physical Performance Battery (SPPB) is predictive of adverse outcomes including morbidity, mortality and disability among healthy and disabled populations [7–9]. In reviewing these studies and the work of others, Morley advocated using mobility performance testing in clinical settings to screen individuals who may benefit most from therapeutic exercise and rehabilitation [10].
Being a voluntary behaviour, exercise is influenced by a variety of attitudes that modulate its potential effect on disability [11–12]. Exercise is defined as bodily exertion for the sake of restoring organs and functions to a healthy state [13]. For the purpose of this manuscript exercise designated to enhance physical function or activities of daily living will be defined as therapeutic exercise or just exercise. Patient’s willingness to participate in therapeutic exercise programmes may be limited by their attitudes and beliefs. Previous studies have found that attitudes toward exercise play an important role in determining exercise participation [14–17]. Confidence in one’s own ability to exercise, or exercise self-efficacy, is strongly associated with adoption of and adherence to exercise [18–19]. As described in Social Learning and Social Cognitive Theories, proposed by Bandura, self-efficacy is fundamental to the processes of behavior change [20,21]. Research has shown that low self-efficacy is a risk factor for further functional decline in older persons who already have experienced reduced physical performance [22]. Jette and colleagues found higher adherence rates to home-based exercise programmes in older adults with positive attitudes toward exercise [23]. A number of other studies have evaluated attitudes that influence older adults’ participation in exercise. The Hebrew Home Study of Impairment and Exercise demonstrated a significant association between attitudes toward exercise and physical performance level in community-dwelling older adults [24]. However, the results were limited in that they involved subjects of relatively high socioeconomic status and excluded participants with the lowest performance scores. Other investigations have attempted to specifically focus upon low-income, multi-ethnic and rural residing participants [25,26]. These populations are particularly important to focus on because of their higher prevalence of inactivity and various barriers to physical activity compared to other segments of the general population [27–29]. To our knowledge, no investigation has sought to evaluate how attitudes toward therapeutic exercise are linked to physical performance among a multi-ethnic population of elders with low socioeconomic status at very high risk for disability. We hypothesize that associations will exist between attitudes toward exercise and both observed and self-reported physical function. In an attempt to understand how best to design future intervention studies and ultimately to create clinical programmes targeting therapeutic exercise for these underserved populations of older adults, we conducted the following cross-sectional study of residents of subsidized senior housing within the city of Boston.
Methods
This study was conducted at six inner-city Boston Housing Authority facilities for low-income seniors and disabled adults. Subjects were recruited via informational sessions, fliers and brochures within the housing facilities. Inclusion criteria were age 70 years or older, English speaking, and having one or more chronic conditions. A total of 94 participants took part in the survey, representing an estimated 20–40% of eligible persons in each building. The study was approved by the Institutional Review Boards at Hebrew Rehabilitation Centre for the Aged and the Harvard Medical School.
The in-home interview included questions related to 10 areas of interest: (i) sociodemographic variables, (ii) medical diagnoses and chronic conditions, (iii) health behaviours, including physical activity, (iv) functional status, (v) psychosocial status, (vi) disease self-management characteristics, (vii) impact of illness, (viii) self-efficacy and helplessness, (ix) health beliefs, (x) medical care and utilization. Trained research assistants administered the SPPB, a composite measure of usual gait speed measured in a 4-m walk, standing balance, and timed chair stands. The SPPB is a validated and reliable performance measure of mobility that is predictive of subsequent morbidity, disability and mortality among healthy and disabled older adults [7,30]. Categories of the SPPB scores were 7–12, 4–6, and 0–3, reflecting high-, middle-, and low-performance, respectively. Two validated scales assessed attitudes and beliefs about exercise. To evaluate readiness for exercise we used the Physician-based Assessment & Counseling for Exercise (PACE) scale created by the Centers of Disease Control and Prevention [31]. This scale rates individuals numerically from 1–11 based upon their readiness for exercise and level of current physical activity. Scores of 6 or higher indicate current engagement in at least moderate physical activity three or more days per week; scores of 2–5 indicate less active or sedentary but contemplating exercise; and scores of 1 indicate not contemplating exercise, or pre-contemplator. Exercise self-efficacy was determined by questions developed by Lorig and colleagues [32]. Three separate questions assessing confidence for exercise participation are each scored on separate 10-point numerical rating scales, with 1 indicating not at all confident and 10 indicating extremely confident. Scores for the three items are summed and averaged leading to a maximum score of 10 for those with the greatest self-efficacy. Self-reported disability was any difficulty in ADL, bathing, dressing, transferring, toileting, and eating [6], and IADL, light housework, heavy housework, preparing meals, and shopping [33]. There were three categories for each domain of disability, IADL and ADL disability, based on a report of no difficulty in any one activity, difficulty in only one activity, and difficulty in two or more activities in each domain.
We used descriptive statistics to show means and proportions of health and demographic characteristics among the study group participants. We performed chi-square tests to compare the distributions of categorical variables. We performed an analysis of variance to compare average self-efficacy values across SPPB, ADL and IADL groups, and, as necessary, post-hoc tests (Tukey) to determine which particular groups differed statistically, with an alpha level of 0.05. All statistical analyses were performed using SAS [34].
Results
Descriptive information about the study participants is presented in Table I. A total of 94 residents participated in the study, ranging in age from 70–96 years, with an average age of 79 years. More than two-thirds were women, and the diverse sample was 55% white, 33% African-American and 12% other. The average annual income of the group was less than $10,000 and half had not completed high school. Nearly half of the participants described their health as fair or poor, more than one-third were obese (Body Mass Index [BMI] > 30), and very few (6.4%) had severe cognitive impairment as manifested by low scores on the Mini Mental Status Exam (MMSE ≤ 17) [35]. Nearly all participants lived alone (90%).
Table I.
Characteristics of older adults living in public housing (n = 94).
| Characteristic | n | Percent |
|---|---|---|
| Age: | ||
| 70–79 | 50 | 58.1 |
| 80–89 | 27 | 31.4 |
| >89 | 9 | 10.5 |
| Missing | 8 | 8.5 |
| Female | 66 | 70.2 |
| Male | 28 | 29.8 |
| High school education or greater | 51 | 54.8 |
| Lives alone | 85 | 90.4 |
| African-American | 31 | 33.0 |
| White | 52 | 55.3 |
| Other | 11 | 11.7 |
| Fair or poor health | 44 | 46.8 |
| Obese (BMI > 30) | 34 | 36.2 |
| MMSE < 24 | 44 | 46.8 |
| Mobility Limitations (SPPB < 7) | 57 | 60.6 |
| ADL disability | 49 | 52.1 |
BMI, Body Mass Index; MMSE, Mini Mental Status Exam; SPPB, Short Physical Performance Battery; ADL, Activities of Daily Living.
Readiness to exercise, as measured by the PACE questionnaire, differed significantly (p < 0.001) across performance levels. As shown in Table II, among those at the lowest performance levels (SPPB 0–3), 44,8% were pre-contemplators, or not ready to exercise (NREx), 41.4% were contemplators, inactive but ready for exercise (REx) and 13.8% were currently physically active. Among those with moderate to severe mobility limitations (SPPB 4–6), 22.2% were NREx, 44.4% were REx and 33.3% were physically active. In contrast, of those at the highest performance levels (SPPB 7–12), only 16.2% were NREx, 18.9% were REx and 64.9% were physically active.
Table II.
Physician-based Assessment & counseling for Exercise (PACE) across varying levels of physical performance and self-reported disability among older adults living in public housing (n= 94).
| PACE score (%)
| ||||
|---|---|---|---|---|
| 1 inactive, not ready(n= 25) | 2–5 inactive, ready (n= 31) | 6 + active(n= 37) | n | |
| SPPB | ||||
| 0–3 | 44.8 | 41.4 | 13.8 | 29 |
| 4–6 | 22.2 | 44.4 | 33.3 | 27 |
| 7–12 | 16.2 | 18.9 | 64.9 | 37 |
| ADL | ||||
| 0 | 11.1 | 22,2 | 66.7 | 45 |
| 1 | 43.5 | 39.1 | 17.4 | 23 |
| 2 | 40 | 48 | 12 | 25 |
| IADL | ||||
| 0 | 10.3 | 17.2 | 72.4 | 29 |
| 1 | 21.2 | 39.4 | 39.4 | 33 |
| 2 | 48.4 | 41.9 | 9.7 | 31 |
SPPB, Short Physical Performance Battery; ADL, Activities of Daily Living; IADL, Instrumental Activities of Daily Living.
Readiness to exercise differed significantly (p < 0.001) across ADL and IADL disability groups, as well. In the group without any ADL difficulties, only 11.1% were NREx, 22.2% were REx and 66.7% were physically active. However, among those with one ADL difficulty, 43.5% were NREx, 39.1% were REx and 17.4% were physically active. In the group with two or more ADL difficulties, 40% were NREx, 48% were REx and 12% were physically active.
Similarly, the presence of IADL difficulties was associated with less exercise readiness and less physical activity. Among those without IADL problems, 10.3% were pre-contemplators, 17.2% were contemplators and 72.4% were physically active. In the group with one IADL difficulty, 21.2% were pre-contemplators, 39.4% were contemplators and 39.4% were active. However, among those with 2 or more IADL problems, 48.4% were pre-contemplators, 41.9% were contemplators and only 9.7% were physically active.
Exercise self-efficacy scores also differed significantly (p < 0.001) across performance, ADL and IADL groups. As shown in Figure 1, the lowest (SPPB 0–3) and intermediate (SPPB 4–6) groups had significantly lower scores in exercise self-efficacy (x̄ = 4.3 ± 2.5 and x̄ = 5.3 ± 2.8, respectively) than the highest performance (SPPB 7–12) group (x̄ = 7.0 ± 2.8). Those with one (x̄ = 4.4 ± 2.7), two or more (x̄ 4.2 ± 2.6) ADL difficulties had significantly lower self-efficacy scores than those with no ADL difficulties (x̄ = 7.2 ± 2.5). Exercise self-efficacy scores also differed significantly among those with none, one, and two or more IADL difficulties (x̄ = 7.6 ± 2.3, x̄= 6.0 ± 2.5 and x̄ = 3.7 ± 2.6, respectively).
Figure 1.
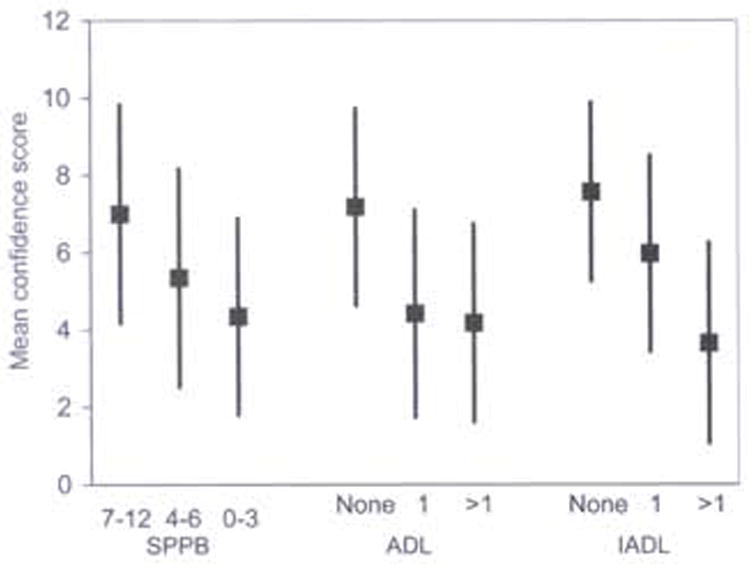
Mean self-efficacy for therapeutic exercise (and standard deviation) across levels of physical performance and self-reported disability among older adults living in public housing (n= 94).
Despite these findings, interest in participating in an exercise class or a home-based exercise programme was high among all groups (Table III). More than 70% of subjects reported such interest, with no significant differences noted across performance, ADL and IADL groups.
Table III.
Interest in home-based and class-based therapeutic exercise programs across varying levels of physical performance and self-reported disability among older adults living in public housing (n= 94).
| Interested in home-based exercise program (per cent) | Interested in class-based exercise program (per cent) | |
|---|---|---|
| SPPB | ||
| 0–3 | 80.0 | 70.0 |
| 4–6 | 96.3 | 88.9 |
| 7–12 | 89.2 | 86.5 |
| ADL | ||
| 0 | 88.9 | 86.7 |
| 1 | 91.3 | 82.6 |
| 2 | 84.6 | 73.1 |
| IADL | ||
| 0 | 96.6 | 89.7 |
| 1 | 87.9 | 87.9 |
| 2 | 81.3 | 68.8 |
SPPB, Short Physical Performance Battery; ADL, Activities of Daily living IADL, Instrumental Activities of Daily Living.
Discussion
Among older adults living in low-income, urban public housing in the city of Boston, lower values of self-efficacy and readiness for exercise were observed across decreasing levels of physical performance and self-reported disability. Fewer than one third of those in the lowest physical performance category were physically active compared to two thirds of those in the highest performance category. Nevertheless, among older persons who had substantial limitations in lower extremity mobility (SPPB <7) many were already exercising on a regular basis and at least 40% expressed readiness to begin or increase physical activity. Similarly, persons with ADL or IADL difficulty generally had less exercise self-efficacy and less readiness for exercise. In regard to IADL difficulties, activity and attitudinal differences across groups were of a similar magnitude. For example, the frequency of regular activity dropped from 72% in the non-disabled adults to 10% of those with two or more IADL difficulties; and essentially equivalent percentages (~ 42–48%) of disabled subjects expressed themselves as ‘ready’ and ‘not ready’ for exercise. Therefore, even among those in the poorest mobility performance and those with ADL or IADL difficulties, a substantial percentage (≥40%) expressed readiness for exercise. It is possible that these percentages are biased in mat disinterested ‘unready’ individuals may have chosen not to participate in our study. Nevertheless, given the very low level of physical function of these groups, these findings are encouraging, indicating that therapeutic exercise opportunities could benefit this vulnerable population.
In addition to exercise readiness, our study also examined participants’ confidence in their ability to perform certain types of exercises, such as gentle strengthening and flexibility exercises and moderate aerobic activities, without making their physical symptoms worse. We found a very strong relationship between exercise self-efficacy and measures of performance and disability. With SPPB scores <7, at the presence of at least one ADL difficulty and or at least two IADL difficulties, average self-efficacy ratings were generally 5 or lower. Others have observed a strong relationship between socio-economic status and self-efficacy, [36] but in our low-income population, we observed a broad range in our measure of self-efficacy. The important role of physical function must be considered in efforts to promote exercise in socioeconomically disadvantaged seniors.
These findings have important clinical implications. They clarify associations between physical function and attitude toward therapeutic exercise among vulnerable older adults. Previous studies aimed at elucidating factors that influence physical activity found that attitudes toward exercise play an important role [15–18], Nevertheless, the determinants of physical activity in women, the elderly, minorities and those with poor health status require further clarification and have been identified as an important area of inquiry [37]. Our study’s findings add to the existing literature regarding attitudes toward therapeutic exercise within vulnerable elders at high risk for disability. Much recent attention has been given to the importance of measuring physical functioning in the elderly within the primary care setting [10]. Because it is easily administered and can help predict adverse outcomes, use of the SPPB as a clinical “vital sign” has been advocated [9]. Our findings suggest that measuring mobility performance and self-reported disability can give clinicians information not only about physical functioning but also might reflect their patients’ readiness and self-efficacy toward exercise. By the design of our study, We are acknowledging that in the future a likely site for health promotion will be within outpatient primary care settings using these advocated screening tools (SPPB, ADL IADL). Through the examination of attitudes and within this population, relative to clinically advocated screening measures, our study offers unique insight into an at-risk population of elders. It has been emphasized that in order to prevent or ameliorate disability, exercise promotion programs must account for the vital attitudes that we investigated [11,37]. These findings, therefore, may be valuable to the future design of health promotion programmes for vulnerable groups of older adults.
This study does have several limitations. This was a cross-sectional analysis and causal relationships cannot be determined among the study’s outcomes. Additionally, our sample size was relatively small, and the recruitment response rate was estimated at 20–40% of eligible residents who participated. The individuals recruited likely represented the most motivated older adults living in this setting. However, the vulnerability of the study sample is a strength of the study, and despite its small sample size, this study begins to consider associations between attitudes toward exercise and observed physical function in older adults living in low-income housing. Future investigations should include longitudinal methods among larger samples of similar populations.
Our findings reinforce that successful therapeutic exercise programs for vulnerable older adults need to address the heterogeneity of patients’ readiness for exercise and self-confidence in ability to exercise. Interestingly, despite their generally low functional status, subjects in this study demonstrated high levels of interest in home-based and class-based therapeutic exercise programs. The study participants were seniors who were living independently in community-based housing but were clearly at risk for institutionalization. Therefore, although such patients lack confidence for exercising, our findings suggest they may have interest in supervised exercise programs if their self-confidence and other attitudes toward exercise are appropriately addressed.
Despite our study’s potential limitations, we found that among urban, multiethnic, older adults of low socioeconomic status, individuals with mobility limitations and with disability in ADL and IADL often lack self-confidence to perform exercise. Additionally, they may not be sufficiently ready to consider the incorporation of therapeutic exercise into a healthier lifestyle. Therefore, programmes aimed at improving function among at-risk elders through therapeutic exercise must include interventions to promote self-confidence and enhance readiness to exercise. Specific groups who, if offered therapeutic exercise, may require more attention toward these attitudes are those with SPPB scores less than 7 and those with ADL or IADL difficulty. Given that therapeutic exercise remains a vital means of health promotion for older adults, the importance of addressing issues that may limit exercise participation cannot be overemphasized.
Acknowledgments
This research was supported by the Harvard Older Americans Independence Center, funded by the National Institute on Aging (AG608812). The first author (JFB) was supported by a Mentored Career Development Award funded the National Institute on Aging (K23 AG019663-01) and the Dennis W. Jahnigan Career Development Scholars Award, funded by the American Geriatrics Society/Hartford Foundation.
References
- 1.Ettinger WH, Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and seniors Trial (FAST) J Am Medical Assoc. 1997;277:25–31. [PubMed] [Google Scholar]
- 2.King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. J Am Medical Assoc. 1997;277:32–37. [PubMed] [Google Scholar]
- 3.King AC, Pruitt LA, Phillips W, Oka R, Rodenburg A, Haskell WL. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health related-quality of life outcomes in older adults. J Gerontol: Medical Sci. 2000;55:M74–83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- 4.Worm CH, Vad E, Puggard L, Stovring H, Lauritsen J, Kragstrup J. Effects of a multicomponent exercise program on functional ability in community-dwelling, frail older adults. J Aging Phys Activity. 2001;9:414424. [Google Scholar]
- 5.Leveille SG, Guralnik JM, Ferrucci L, Langlois JA. Aging successfully until death in old age; opportunities for increasing active life expectancy. Am J Epidemiol. 1999;149:654–664. doi: 10.1093/oxfordjournals.aje.a009866. [DOI] [PubMed] [Google Scholar]
- 6.Katz S, Ford AB, Moskowiz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial function. J Am Medical Assoc. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 7.Guralnik JM, Ferrucci L, Pieper CF, Leveillie SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability. Consistency across studies, predictive models and value of gait speed alone compared with the short physical performance battery. J Gerontol: Medical Sci. 2000;55A:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Simonsick HM, Ferucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function; association with self-reported disability and prediction of morality and nursing home admission. J Gerontol: Medical Sci. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 9.Studenski S, Perera S, Wallace D, Chandler JM, Dunean PW, Rooney E, et al. Physical performance measures in the clinical setting. J Am Geriatrics Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 10.Morley JE. Mobility performance; A high-tech test for geriatricians. J Gerontol: Medical Sci. 2003;58:712–714. doi: 10.1093/gerona/58.8.m712. [DOI] [PubMed] [Google Scholar]
- 11.Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise. J Gerontol: Medical Sci. 2001;56:M412–423. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- 12.Phillips EM, Schneider JC, Mereer GR. Motivating elders to initiate and maintain exercise. Arch Phys Med Rehabil. 2004;85:S52–57. doi: 10.1016/j.apmr.2004.03.012. quiz S58–59. [DOI] [PubMed] [Google Scholar]
- 13.Stedman’s Medical Dictionary. 27. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 14.Ebrahim S, Rowland L. Toward a new strategy for health promotion for older women; Determinants of physical activity. Psychol Health Med. 1996;1:29–40. [Google Scholar]
- 15.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promotion. 1992;6:424–429. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- 16.McAuley E, Lox C, Duncan TE. Long-term maintenance of exercise, self-efficiency, and physiological change in older adults. J Gerontol; Medical Sci. 1993;48:P218–224. doi: 10.1093/geronj/48.4.p218. [DOI] [PubMed] [Google Scholar]
- 17.Rich SC, Rogers ME. Stage of exercise change model and attitudes towards exercise in older adults. Perceptual Motor Skills. 2001;93:141–144. doi: 10.2466/pms.2001.93.1.141. [DOI] [PubMed] [Google Scholar]
- 18.McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Preventative Med. 2003;37:110–118. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 19.Oman RF, King AC. Predicting the adoption and maintenance of exercise participation using self-efficiency and previous exercise participation rates. Am J Health Promotion. 1998;12:154–161. doi: 10.4278/0890-1171-12.3.154. [DOI] [PubMed] [Google Scholar]
- 20.Bandura A. self-efficacy; Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Social foundations of thought and action. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 22.Mendes de Leon CF, Seeman TE, Baker DI, Richardson ED, Tinetti ME. Self-efficacy, physical decline, and change in functioning in community -living elders; A prospective study. J Gerontol Soc Sci. 1996;51:S183–S190. doi: 10.1093/geronb/51b.4.s183. [DOI] [PubMed] [Google Scholar]
- 23.Jette AM, Rooks D, Lachman M, Ling TH, Levensen C, Heislein D, et al. Home-based resistance training. Predictors of participation and adherence. The Gerontologist. 1998;38:412–421. doi: 10.1093/geront/38.4.412. [DOI] [PubMed] [Google Scholar]
- 24.Chang M, Leveille SG, Cohen-Mansfield J, Guralnik JM. The association of physical performance level with attitude toward exercise in older adults. J Aging Phys Activity. 2003;11:254–264. [Google Scholar]
- 25.Collins R, Lee RE, Albright CL, King AC. Ready to be physically active. The effects of a course preparing low-income multiethnic women to be more physically active. Health Edu Behav. 2004;31:47–64. doi: 10.1177/1090198103255529. [DOI] [PubMed] [Google Scholar]
- 26.Wileox S, Bopp M, Oberrecht L, Kammermann SK, McElmurray CT. Psychosocial and perceived environmental correlates of physical activity in rural and older African-American and white women. J Gerontol; Psycholog Soc Sci. 2003;58:P329–337. doi: 10.1093/geronb/58.6.p329. [DOI] [PubMed] [Google Scholar]
- 27.Crespo CJ, Ainsworth BE, Keteyian SJ, Heath GW, Smit E. Prevalence of physical inactivity and its relation to social class in US adults; Results from the third national health and nutrition examination survey, 1988-1994. Med Sci Sports Exercise. 1999;31:1821–1827. doi: 10.1097/00005768-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Raceethnicity, social class and their relation to physical inactivity during leisure time results from the third nation health and nutrition examination survey,1998–1994. Am J Prevent Med. 2000;18:46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 29.Wilcox S, Castro C, King AC, Housemann R, Brownson RC. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the USA. J Epidermiol community Health. 2000;54:667–672. doi: 10.1136/jech.54.9.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guralnik JM, Ferucci L, Simonsick EM, Salive ME, Wallace RB. Lower extremity function over age 70 years as a predictor of subsequent disability. NEJM. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Project PACE Physician Manual. Atlanta, GA: Cardiovascular Health Branch Centers for Disease Control; 1992. [Google Scholar]
- 32.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinic Practice. 2001;4:256–262. [PubMed] [Google Scholar]
- 33.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 34.SAS, SAS/STAT. User’s Guide, Version 8 cary. NC: SAS Institute, Inc; 1999. [Google Scholar]
- 35.Folstein MF, Folstein SF, MeHugh PR. Mini-mental state”: A practice method for grading the cognitive state of patients for the clinician. Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 36.Clark DO, Patrick DL, Grembowski D, Durham ML. Socioecnomic status and exercise self-efficacy in late life. J Behav Med. 1995;18:355–376. doi: 10.1007/BF01857660. [DOI] [PubMed] [Google Scholar]
- 37.King AC. Interventions to promote physical activity by older adults. J Gerontol Med Sci. 2001;56:36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]


