Abstract
Inflight medical emergencies occur at a rate of 20 to 100 per million passengers, with a death rate of 0.1 to 1 per million. Cardiac, neurologic, and respiratory complaints comprise the more serious emergencies, as defined by aircraft diversion or use of ground-based medical assistance. In this paper, we review changes seen in the resting electrocardiogram in normal individuals exposed to high altitude, alongside important implications for patients with heart diseases in high altitude exposures and the possible effects of high altitude to permanent cardiac pacemakers. Arrhythmias in pilots and public safety are revisited together with the guidelines of the Joint Aviation Requirements (JAR) in Europe. The situation of Military flights is also discussed. Physicians ought to become knowledgeable about the specific medical job standards for their patients when asked to render opinions regarding fitness to fly. A database must be established to obtain prospective data that defines the risk of accidents in patients who are or were being treated for arrhythmias. Current guidelines could then be updated and revised as appropriate.
According to data from US, about one billion people travel on domestic and international airlines each year1. Inflight medical emergencies occur at a rate of 20 to 100 per million passengers, with a death rate of 0.1 to 1 per million2. The precise incidence of inflight medical emergencies is unknown because there is no uniform or required reporting system, and flight crews do not routinely report minor inflight medical incidents that do not require ground medical support3. The most common medical complaints to airplane crews include gastrointestinal, traumatic, cardiac, neurologic and respiratory. Cardiac, neurologic, and respiratory complaints comprise the more serious emergencies, as defined by aircraft diversion or use of ground-based medical assistance2,4. Among these, cardiac emergencies are most common. A medical professional is present for 40 to 70 percent of inflight medical emergencies, and a doctor is present in 30 to 60 percent4,5. These numbers may be higher; fear of liability prevents some clinicians from intervening6.
Normal cardiovascular response to high altitude – recommendations for patients
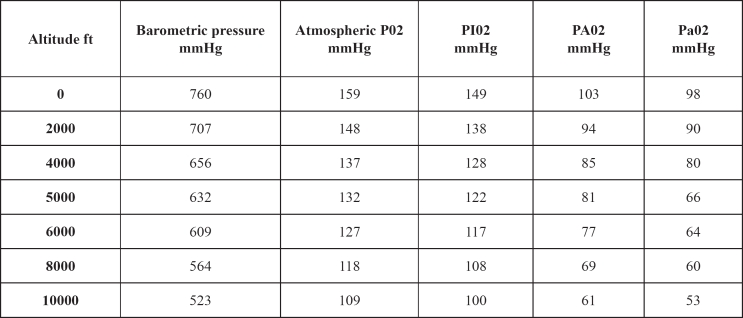
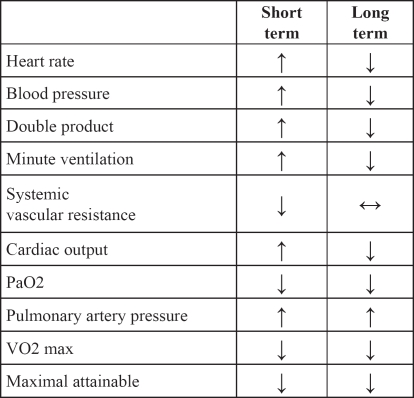
Commercial airplanes typically cruise between 22.000 and 44.000 feet (6.700-13.400 meters). Cabin pressure altitude varies from 3000 to 8.000 feet (910- 2.439 meters)7. At an altitude equivalent to 8.000 feet, the barometric pressure is decreased to 564 mmHg (compared to 760 mmHg at sea level). PiO2 is 109 mmHg, with associated partial pressures of oxygen in the alveoli and arterial blood of normal individuals of 69 mmHg and 60 mmHg respectively (Table 1)8. Cardiovascular system responds to high altitude within minutes after exposure with transient epinephrine and more sustained norepinephrine secretion mediated by stimulation of the carotid body. Immediate changes include increase in ventilation, heart rate, cardiac output and blood pressure (Table 2). The initial hyperventilation leads to hypocapnia and respiratory alkalosis, which in turn inhibits ventilation. As a result, the ability to improve oxygenation by hyperventilation becomes limited9.
Table 1: Physical effects of change in altitude.
PI02: partial pressure of inspired oxygen; PA02: partial pressure of alveolar oxygen; Pa02: partial pressure of oxygen in arterial blood 8000 feet represents the maximum allowable altitude in commercial aircraft.
Adapted from Gong H. Exposure to moderate altitude and cardiorespiratory diseases. Cardiologica 1995;40:477
Table 2: Cardiovascular changes after short term and long term altitude exposure.
Several changes were seen in the resting electrocardiogram (ECG) in normal individuals exposed to high altitude (17.500, 20.500 and 26.200 feet) which included: increase in resting HR, prolongation of the QT interval, ST-T wave flattening, rightward shift in the frontal QRS axis, increase in P-wave amplitude in lead II10. The last two changes are thought to reflect evidence of right ventricular and right atrial "strain" arising from hypoxiainduced pulmonary hypertention. At the most extreme altitude, 3 of 12 patients developed a new RBBB and 3 others showed changes consistent with right ventricular hypertrophy. All ECG abnormalities abate upon descent to sea level and so they are not thought to be clinically important.
High altitude exposure may have important implications for patients with heart diseases. The incidence of arrhythmias induced by altitude exposure varies according to the patient group under study. Young individuals (aged 21-31 years),were observed during exercise at stimulated altitudes equivalent to the summit of Mount Everest, and no arrhythmias, conduction defects, nor ST or T wave changes to suggest ischemia were seen11. Middle aged men however doubled the incidence of both supraventricular and ventricular premature beats at an altitude of 1350 meters (4428 feet) as compared with 200 meters (656 feet)12. At even higher altitude (2632 meters – 8633 feet), the frequency of ectopy was increased six to seven fold13. In summary, it appears that altitude can aggravate arrhythmias, particularly during acute exposure and with exercise, in patients with the proper substrate. Air travel alone is probably of low risk, except in those with baseline ventricular and supraventricular arrhythmias in whom added stress of mild hypoxemia might lead to decompensation. Such patients should be cautioned about air travel or be considered for supplemental oxygen.
Another issue concerning air travel safety is the possible effect of high altitude to permanent cardiac pacemakers. There is evidence that pacemaker function is altered at high altitude. Hypoxia has proven to cause a significant increase in stimulation thresholds, while hypocapnia was associated with a reduction in pacing stimulation thresholds. Nevertheless in a more contemporary report, simulated hypobaric chamber ascent from 450 meters to 4000 meters (1476 to 13.120 feet) produced no change in stimulation threshold in spite of a significant fall in PaO2. It seems likely that the competing effects of hypoxia and hypocapnia, each pushing the pacing threshold in a different direction, may balance each other and prevent any net change during the physiologic stress of true altitude exposure14. Based on the limited data, it appears that pacing thresholds can be expected to remain unchanged at the moderate altitudes of air travel.
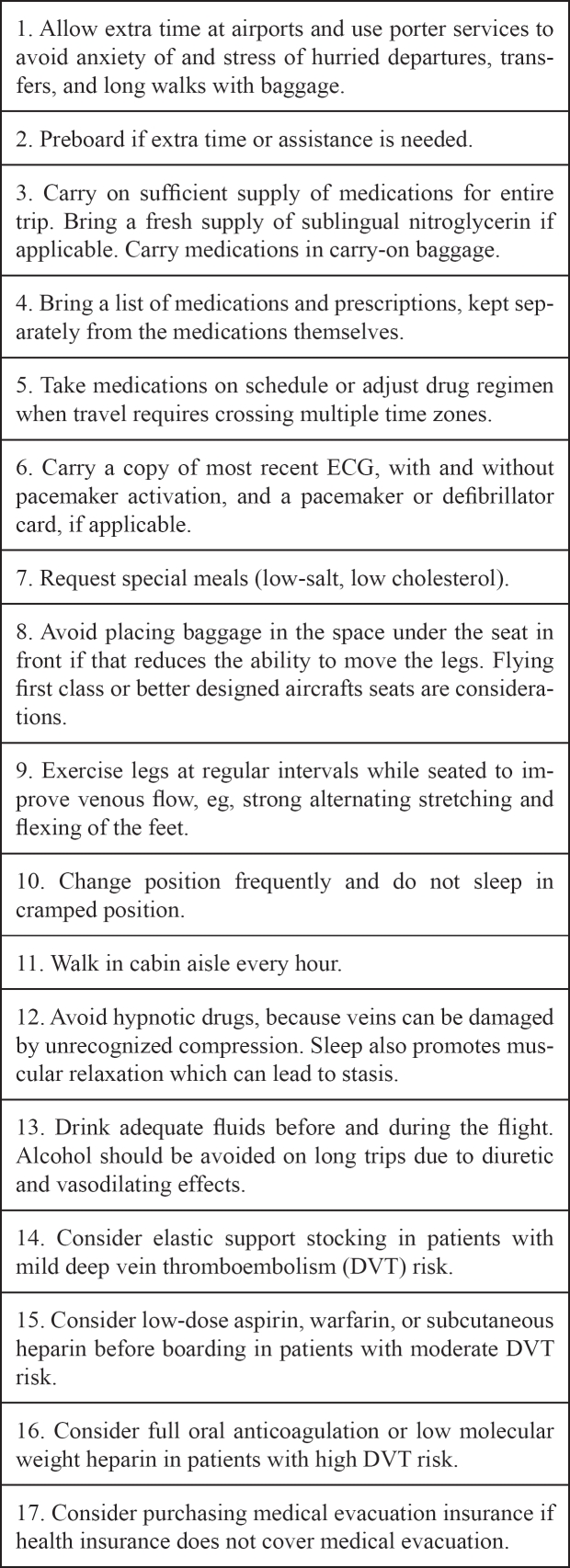
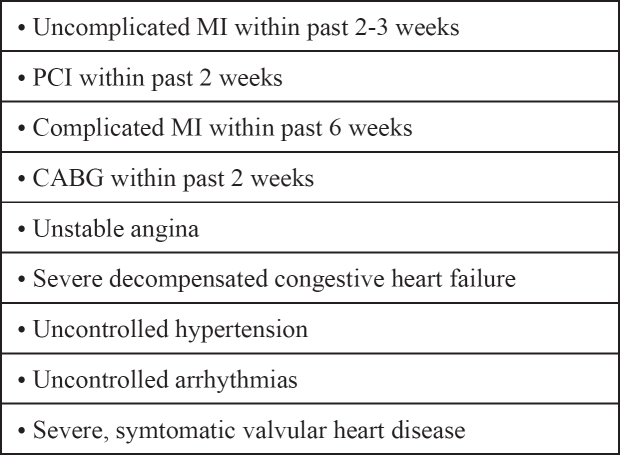
Patients with cardiovascular disease and thus with little or no cardiopulmonary reserve, probably cannot effectively compensate for the reduced arterial PaO2 during a commercial air flight and are at risk of profound arterial desaturation and cardiopulmonary decompensation. Patients who can walk 50 yards (45,7 meters) at a normal pace without becoming dyspneic or otherwise symptomatic are thought to be able to fly. Patients with PaO2 < 72 mmHg at sea level will probably need supplemental inflight oxygen15. In general most patients with well- compensated cardiac disease can travel without difficulty (Table 3). Patients with poorly controlled heart disease should be advised against air travel (Table 4).
Table 3: General recommendations to cardiopulmonary patients travelling by air.
Adapted from Gong H. Exposure to moderate altitude and cardiorespiratory diseases. Cardiologica 1995;40:477
Table 4: Cardiac contraindications to air travel.
The 2004 ACC/AHA guidelines recommend that air travel within the first two weeks after an MI (Myocardial Infarction) should be undertaken only if the patient has no angina, no dyspnea at rest and no fear of flying16,17. The patient should have a companion, carry nitroglycerine, and request airport transportation to avoid rushing. In contrast, the Aerospace Medical Association recommends that no air travel be undertaken within two to three weeks of an uncomplicated MI and within six weeks of a complicated MI18.
Arrhythmias in pilots and public safety
Patients with arrhythmias may experience chest pain, shortness of breath, palpitations, dizziness, syncope, or sudden cardiac death. Sudden Cardiac Death (SCD) is determined as the natural death due to cardiac causes, heralded by abrupt loss of consciousness within 1 hour of the onset of symptoms, in an individual who may have preexisting heart disease but in whom the time and mode of death are unexpected19.
SCD claims more lives each year than stoke, lung cancer, breast cancer and AIDS combined. The cause of SCD is in 88% arrhythmic, and only 12% is attributed to other cardiac condition20. Arrhythmias that lead to SCD is ventricular fibrillation (62%), bradycardia (17%), Torsades des Pointes (13%) and primary atrial fibrillation (8%)21. In 80% of SCD the underlying condition is coronary heart disease, while cardiomyopathies account for 15% of SCD and 5% is related to other conditions such as valvular disease, long QT syndrome, Brugada syndrome, idiopathic ventricular fibrillation and Wolf-Parkinson- White syndrome19.
The Joint Aviation Authorities in Europe (JAA) and the Federal Aviation Administration (FAA) in the United States are the responsible institutions for medical certification of pilots. Given the frequency with which medical certification is required (every six months for first class, annually for second class and third class), the FAA Aeromedical Certification Division processes 1900 new or renewal applications daily. Less than 1% is denied for failure to meet medical standards22.
According to findings from the Aeromedical Office of the Airline Pilots Association, each year approximately 42 persons with rhythm disturbances contact the office. Over one half of these persons have experienced syncopal episodes, with 5 to 10 in-cockpit syncopes per year. In a review of 102 syncopes over 5 years, less than half were attributed to ventricular arrhythmias. The majority of individuals with ventricular arrhythmias were permanently disqualified from flying, while most individuals with syncope believed to be bradyarrhythmic returned to flight after evaluation.
Cardiovascular causes are the most common cause of loss of flying licence in Western Europe, and cardiac arrhythmia is the main disqualifier in a substantial proportion of these. Frequent ventricular premature beats, nonsustained VT, and paroxysmal atrial fibrillation were the most common problem arrhythmias22.
Joint Aviation Requirements (JAR) – Europe
The Joint Aviation Authorities in Europe (JAA) has published the Joint Aviation Requirements for flight crew medical licensing23, which are summarized below.
An applicant for or holder of a Class 1 medical certificate shall not possess any abnormality of the cardiovascular system, congenital or acquired, which is likely to interfere with the safe exercise of the privileges of the applicable licence(s).
A standard 12-lead resting electrocardiogram (ECG) and report are required at the examination for first issue of a medical certificate, then every 5 years until age 30, every 2 years until age 40, annually until age 50.
Exercise electrocardiography is required only when clinically indicated.
Estimation of serum lipids, including cholesterol, is required to facilitate risk assessment at the examination for first issue of a medical certificate, and at the first examination after the 40th birthday.
Further evaluation may include:24-hour ECG recording, Electrophysiological study, Myocardial perfusion scanning, or equivalent test, Cardiac MRI or equivalent test, Coronary angiogram or equivalent test.
Any significant rhythm or conduction disturbance requires evaluation by a cardiologist acceptable to the AMS (Aeromedical Section) and appropriate follow-up in the case of a fit assessment. Such evaluation shall include:
Exercise ECG to the Bruce protocol or equivalent. The test should be to maximum effort or symptom limited. Bruce stage 4 shall be achieved and no significant abnormality of rhythm or conduction, nor evidence of myocardial ischaemia shall be demonstrated.
24-hour ambulatory ECG which shall demonstrate no significant rhythym or conduction disturbance.
2D Doppler echocardiogram which shall show no significant selective chamber enlargement, or significant structural, or functional abnormality, and a left ventricular ejection fraction of at least 50%.
Atrial arrhythmias
Applicants with significant disturbance of supraventricular rhythm, including sinoatrial dysfunction, whether intermittent or established, shall be assessed as unfit.
Applicants with asymptomatic sinus bradycardia or sinus tachycardia may be assessed as fit in the absence of underlying abnormality.
Applicants with asymptomatic isolated uniform supra-ventricular or ventricular ectopic complexes need not be assessed as unfit. Frequent or complex forms require full cardiological evaluation.
Bundle Branch Block
In the absence of any other abnormality, applicants with incomplete bundle branch block or stable left axis deviation may be assessed as fit.
Applicants with complete right bundle branch block (RBBB) require cardiological evaluation on first presentation and subsequently if age < 40 may be assessed as fit, otherwise if age >40 should demonstrate a period of stability of 12 months
Applicants with complete left bundle branch block (LBBB) shall be assessed as unfit. A fit assessment may be considered by the AMS:
initial class I applicants should demonstrate a 3 year period of stability.
investigation of the coronary arteries is necessary in applicants over age 40.
Atrioventricular conduction disturbances
Applicants with first degree and Mobitz type 1 AV block may be assessed as fit in the absence of underlying abnormality.
Applicants with Mobitz type 2 or complete A-V block shall be assessed as unfit. A fit assessment may be considered by the AMS after thorough evaluation.
Tachycardias / pre-excitation syndromes
Applicants with broad and/or narrow complex tachycardias shall be assessed as unfit. A fit assessment may be considered by the AMS after thorough evaluation.
Applicants with ventricular pre-excitation shall be assessed as unfit. A fit assessment may be considered by the AMS, if an electrophysiological study, including adequate drug-induced autonomic stimulation reveals no inducible re-entry tachycardia and the existence of multiple pathways is excluded.
Permanent Pacemakers
Applicants with an endocardial pacemaker shall be assessed as unfit.
Following permanent implantation of a subendocardial pacemaker a fit assessment which shall be no sooner than three months after insertion shall require: no other disqualifying condition, a bipolar lead system, that the applicant is not pacemaker dependen and regular follow-up including a pacemaker check.
Ablation
Applicants who have received ablation therapy shall be assessed as unfit. A fit assessment may be considered by the AMS in case that an electrophysiological study, undertaken at a minimum of 2 months after the ablation, demonstrates satisfactory results.
Atrial fibrillation
Recertification of applicants with Atrial fibrillation requires:
normal echocardiogram
satisfactory completion of at least three stages of a Bruce protocol graded exercise test (with no other arrhythmia or conduction disturbance),
completion of several ambulatory electrocardiographic recordings (Holter type) in which, if atrial fibrillation is present, there are no RR intervals less than 300 ms or greater than 3 seconds.
In the case of a single episode of atrial fibrillation with an apparent cause, restricted recertification is permitted with arrangements for regular medical assessment. If there are no further attacks, full certification is permitted only after 2 years. Additional attacks would result in restricted certification only if suppressed or asymptomatic.
Military flights
The US Army and Air Force have a joint policy that strives to take into account the particularly uncertain and stressful nature of operational circumstances, together with potential environmental extremes, physical stress, circadian disturbances and exposure to acceleration forces. Aim of screening for cardiovascular disease and arrhythmias in the military situation is detection before symptoms are manifested22.
Acceleration forces (G forces) act on human body during acceleration in three axes (x, y, z). Gz forces are parallel to the vertical axis (head-feet) and cause significant variation in blood pressure along the length of the subject's body. In aircraft in particular, g-forces are often towards the feet, which forces blood away from the head, with a consequent negative effect on vision and consciousness. As g-forces increase brownout/greyout can occur, where the vision loses hue. If g-force is increased further tunnel vision will appear, and then at still higher g, loss of vision, while consciousness is maintained, this is termed "blacking out". Beyond this point losing consciousness will occur, also sometimes known as g-loc (loss of consciousness).
Various arrhythmias were observed during high Gz training. Hanada et al24 developed a criterion for suspending G-training based on observed arrhythmias. Sinus arrhythmia (48.7%), single premature atrial contraction (32.3%), and single (58.5%) or paired (9.7%) premature ventricular contraction were commonly occurring arrhythmias during high-G training and were considered as variant physiological responses to high-G training (category 1). Ventricular tachycardia (2.6%), paroxysmal supraventricular tachycardia (1.5%), and paroxysmal atrial fibrillation (0.5%) though are combined in a great proportion with cardiac anomalies. As a result, the JASDF currently categorizes these arrhythmias as indicators to suspend Gtraining and initiate cardiac workup (category 3). Other arrhythmias, such as non-sustained ventricular tachycardia (VT) or Morbitz type I atrioventricular (AV) block, were considered borderline anomalies; whether training was allowed to continue depended on the decision of the physicians monitoring the training (category 2).
Specific arrhythmias to military pilots
Bradyarrhythmias
Detection of sinus pauses is followed by Holter monitoring and exercise testing. Asymptomatic and infrequent pauses of less than 4 seconds' duration are not disqualifying
Atrial arrhythmias
Premature atrial contractions require cardiac assessment and persons with benign findings are permitted to fly.
Supraventricular tachycardias (SVT)
More than 3 consecutive SVT beats result in restriction from flying pending investigation. Hemodynamic symptoms associated with SVT, recurrent sustained SVT, or SVT with ventricular preexcitation are disqualifying
Preexcitation syndromes (e.g. WPW) who have undegone successful radiofrequency ablation may return to flying duties.
Premature ventricular contractions (PVC's)
Infrequent PVC's are not disqualifying in the absence of evident cardiac disease.
Ventricular tachycardia
VT defined as >3 consecutive ventricular complexes at a rate of 100 bpm or greater is a cause for restriction pending investigation, while recurrent VT, sustained VT, VT in the presence of cardiac disease are disqualifying.
Conduction disturbances
First degree AV block and second degree Mobitz I are not disqualifying.
Second degree Mobitz II and third degree AV block are disqualifying.
Individuals with RBBB are able to entry into flight training, and should undergo a noninvasive evaluation. In case there are no abnormal findings the situation is not disqualifying.
Individuals with LBBB should undergo both noninvasive and invasive evaluation. In case there are no abnormal finding they may return to flying duties.
Conclusions
In the context of arrhythmia management, physicians carry the responsibility of providing data and best estimates of risk for the occurrence of first or repeated medical events that may lead to impaired consciousness. Often, prospective data are not available, and clinical observation and best judgments must be used to make recommendations. State and federal regulators then have the responsibility to translate these data and recommendations into law or to propose guidelines. Physicians are obligated to become knowledgeable about the specific medical job standards for their patients when asked to render opinions regarding fitness to fly. A database must be established to obtain prospective data that defines the risk of accidents in patients who are or were being treated for arrhythmias. This will resolve the currently unavoidable problem of underreporting. A database will also permit analysis of subgroups of patients with particular arrhythmias, presentations, and therapies. Current guidelines could then be updated and revised as appropriate. In the future it may be possible to replace standards that impose absolute prohibitions on licensure with performance standards that permit individualized treatment22.
References
- 1.Medical Guidelines Task Force AMA. Medical guidelines for airline travel, 2nd edition. Aviat Space Environ Med. 2003;74:A1. [PubMed] [Google Scholar]
- 2.Lyznicki JM, Williams MA, Deitchman SD, Howe JP, 3rd Council on Scientific Affairs; American Medical Association. Inflight medical emergencies. Aviat Space Environ Med. 2000;71:832–838. [PubMed] [Google Scholar]
- 3.Sirven JI, Claypool DW, Sahs KL, et al. Is there a neurologist on this flight? Neurology. 2002;58:1739–1744. doi: 10.1212/wnl.58.12.1739. [DOI] [PubMed] [Google Scholar]
- 4.Dowdall N. "Is there a doctor on the aircraft?" Top 10 in-flight medical emergencies. BMJ. 2000;321:1336–1337. doi: 10.1136/bmj.321.7272.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeJohn C, Veronneau SJ, Wolbrink AM. The evaluation of inflight medical care aboard selected US air carriers: 1996-1997. Washington DC: Office of Aviation Medicine; Federal Aviation Administration, Technical report no. DOT/FAA/AM-0013. 2000
- 6.Rayman RB. Inflight medical kits. Aviat Space Environ Med. 1998:69–1007. [PubMed] [Google Scholar]
- 7.Cottrell JJ. Altitude exposures during aircraft flight. Flying higher. Chest. 1988;93:81–84. doi: 10.1378/chest.93.1.81. [DOI] [PubMed] [Google Scholar]
- 8.Gong H. Exposure to moderate altitude and cardiorespiratory diseases. Cardiologica. 1995;40:477–488. [PubMed] [Google Scholar]
- 9.Hultgren HN. High Altitude Medicine. Stanford: Hultgren Publications; 1997. The systemic circulation. [Google Scholar]
- 10.Karliner JS, Sarnquist FF, Graber DJ, Peters RM., Jr The electrocardiogram at extreme altitude: experience on Mt. Everest. Am Heart J. 1985;109:505–513. doi: 10.1016/0002-8703(85)90555-1. [DOI] [PubMed] [Google Scholar]
- 11.Malconian M, Rock P, Hultgren H, Donner H. The electrocardiogram at rest and exercise during a simulated ascent of Mt. Everest (Operation Everest II) Am J Cardiol. 1990;65:1475–1480. doi: 10.1016/0002-9149(90)91358-d. [DOI] [PubMed] [Google Scholar]
- 12.Kujanik S, Snincak M, Vokal' J, Podracky J. Periodicity of arrhythmias in healthy elderly men at the moderate altitude. Physiol Res. 2000;49:285–287. [PubMed] [Google Scholar]
- 13.Kujanik S, Snincak M, Galajdova K, Rackova K. Cardiovascular changes during sudden ascent in a cable cabin to the moderate altitude. Physiol Res. 2000;49:729–731. [PubMed] [Google Scholar]
- 14.Weilenmann D, Duru F, Schonbeck M, Schenk B. Influence of acute exposure to high altitude and hypoxemia on ventricular stimulation thresholds in pacemaker patients. Pacing Clin Electrophysiol. 2000;23:512–515. doi: 10.1111/j.1540-8159.2000.tb00836.x. [DOI] [PubMed] [Google Scholar]
- 15.Gong H. Advising pulmonary patients about commercial air travel. J Respir Dis. 1990;11:484–499. [Google Scholar]
- 16.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction-executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction. [DOI] [PubMed] [Google Scholar]
- 17.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/ Non–ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2007;50:e1–157. (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction) Developed in Collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. [Google Scholar]
- 18.Medical Guidelines Task Force AMA. Medical guidelines for airline travel, 2nd edition. Aviat Space Environ Med. 2003;74:A1. [PubMed] [Google Scholar]
- 19.Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. In: Zipes DP, Libby P, Bonow RO, Braunwald E, editors. Heart Disease. A Textbook of Cardiovascular Medicine. 7th edition. Philadelphia, PA: WB Saunders Company; 2005. pp. 865–908. [Google Scholar]
- 20.Albert CM, Chae CU, Grodstein F, et al. Prospective study of sudden cardiac death among women in the United States. Circulation. 2003;107:2096–2101. doi: 10.1161/01.CIR.0000065223.21530.11. [DOI] [PubMed] [Google Scholar]
- 21.BaysdeLuna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989;117:151–159. doi: 10.1016/0002-8703(89)90670-4. [DOI] [PubMed] [Google Scholar]
- 22.Epstein A, Miles W, Benditt DG, et al. Personal and Public Safety Issues Related to Arrhythmias That May Affect Consciousness: Implications for Regulation and Physician Recommendations. Circulation. 1996;94:1147–1166. doi: 10.1161/01.cir.94.5.1147. [DOI] [PubMed] [Google Scholar]
- 23.Joint Aviation Authorities. JAR-FCL 3-Flight Crew Licensing (medical) 2006 www.jaa.nl. [Google Scholar]
- 24.Hanada R, Hisada T, Tsujimoto T, Ohashi K. Arrhythmias observed during high G training: proposed training safety criterion. Aviat Space Environ Med. 2004;75:688–691. [PubMed] [Google Scholar]