Abstract
Pain on the ulnar side of the wrist is common among elite tennis players. Ten years of experience has allowed identification of a pathology involving the extensor carpi ulnaris (ECU) tendon. On the basis of 28 clinical cases seen over the last five years, three clinical patterns are described: (a) acute instability of the ECU; (b) tendinopathy; (c) ECU rupture. Each of these clinical entities requires a different therapeutic approach. A review of the relevant anatomy is provided.
Keywords: extensor carpi ulnaris, tennis, wrist, tendinopathy
Our interest in ulnar wrist injuries has developed over 10 years of clinical experience monitoring elite tennis players at the National Training Centre at Roland Garros and at the Bercy Tournament. Ulnar wrist pain is caused by specific technique problems: the increased use of the wrist to create topspin, the use of the double handed backhand, and the use of a higher string tension, increasing the effect when the ball hits the racquet.
The purpose of this article is to describe three pathologies specific to elite tennis players, requiring standardised therapeutic management to enable the scheduled return of the player to the tennis court. These pathologies are tendinopathy of the extensor carpi ulnaris (ECU) tendon, traumatic instability of the ECU tendon, and rupture of the ECU tendon.
Materials and methods
Our office is located at the medical centre of the French Tennis Federation National Training Centre where the top 50 French tennis players train. We also provide medical care during the Grand Slam Tournament at Roland Garros and the Super Nine ATP tournament at Paris Bercy. Since 2000, we have been studying pain on the ulnar side of the wrist and we have developed a standardised clinical examination and additional work up combining radiography, ultrasound, and magnetic resonance imaging (MRI) of the affected joint. Damage to the wrist accounts for 11.2% of reported injuries in men and 15.7% in women. Of these injuries, ECU pain accounts for 76% in men and 45% in women. ECU pathology is the most common wrist problem for which players seek medical advice. We studied 28 cases of ulnar sided wrist pain related to the ECU.
The study population consisted exclusively of elite tennis players of both sexes, with the following characteristics. Seventeen were male and 11 were female players. Their mean age was 23 years (range 13–31). Sixteen of the 28 were ranked in the top 100 of the ATP or WTA ranking, and two players had previously been ranked no 1 in the world. They played three to four hours of tennis a day.
Patients with ulnar pain of other origins were eliminated from this cohort—that is, pain related to the triangular fibrocartilage complex, the triquetrum‐lunate ligament, and pisiform‐triquetrum joint and fractures of the lunatum, triquetrum, and hook of the hamate.
Using our experience with these 28 cases, we were able to isolate three distinct clinical entities which differed in their onset, clinical presentation and imaging, and finally their outcome.
Traumatic instability of the ECU tendon. In 12 cases, pain occurred suddenly, corresponding to a traumatic instability of the ECU tendon within the osteofibrous groove at the inferior section of the ulna.
Tendinopathy of the ECU. There were 14 cases in which no initial trauma was reported. Pain occurred gradually, and the clinical picture suggested a tendinopathy of the ECU.
Rupture of the ECU tendon. There were two cases of a complete ECU tendon rupture following a classic pattern.
Anatomical review
Classically, the muscle fibres of the ECU tendon are described as ending in a tendon a little above the wrist.1 The tendon passes behind the lower end of the ulna in an osteofibrous sheath which runs through an osseous groove between the head of the ulna and its articular process. The tendon inserts on to the internal process of the 5th metacarpal.
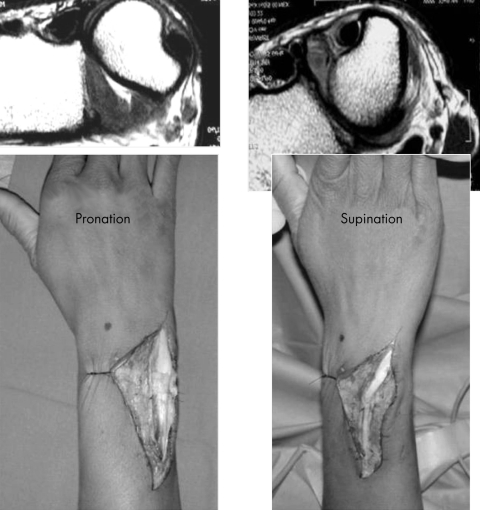
The ECU tendon is stabilised in the osseous groove. It lies in the sixth compartment formed by duplication of the deep antebrachial fascia inserted on to the osseous groove, forming a tunnel (ECU subsheath).2 The dorsal retinaculum, which runs over the five dorsal compartments, passes above it, like a bridge. The retinaculum is not attached to the inferior ulna and inserts on to the triquetrum and pisiform, allowing both pronation and supination. Finally, there is an anatomical entity composed of longitudinal fibres, the “linea jugata”, which reinforces the ulnar insertion of the ECU subsheath (figs 1 and 2).3
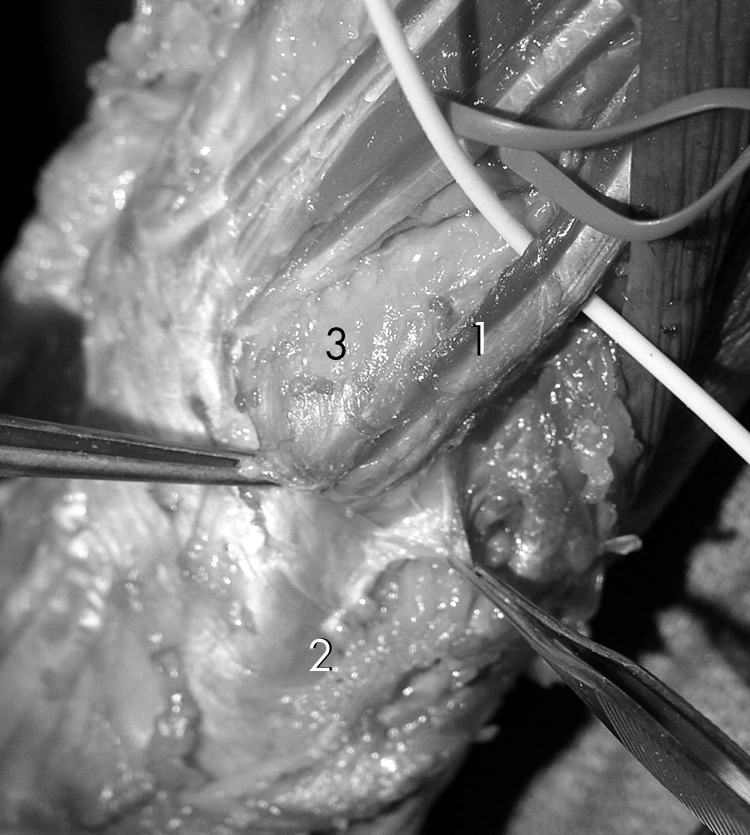
Figure 1 Anatomy of the wrist: 1, extensor carpi ulnaris (ECU) tendon; 2, ECU subsheath; 3, ulna head.

Figure 2 Extensor carpi ulnaris (ECU) subsheath is on top of the tendon, and the dorsal retinaculum, without any attachment to the ulna, is on top of the ECU subsheath.
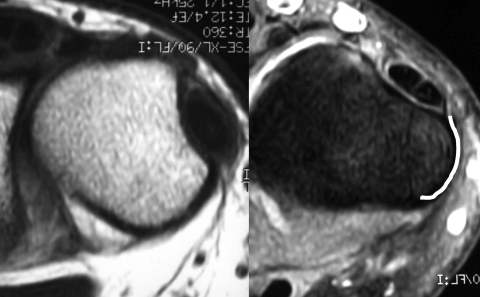
These anatomical features play an important role in maintaining ECU stability in the osteofibrous groove and ensure that the tendon is closely bound to the ulnar head. Therefore it moves less freely than the other extensor tendons. This results in stress on the ECU tendon during pronation and supination. During pronation, the ECU tendon is situated on the inner surface of the ulnar head, far from the extensor digiti minimi. A gap is therefore created between the two tendons, with the ECU tendon having a direct course. During supination, the ECU tendon moves closer to the extensor digiti minimi, obliterating the space between the two. The ECU tendon is subjected to maximal traction and has to adopt an approximately 30° angle to reach the base of the 5th metacarpal. These changes in anatomical position explain the onset of traumatic injury to the ECU retinaculum occurring during modern tennis play, whereby the angle of the wrist constantly changes (fig 3).
Figure 3 Views of the wrist showing that, during pronation, the extensor carpi ulnaris tendon follows a straight path, whereas during supination it is forced to adopt an approximately 30° angle. Informed consent was obtained for publication of this figure.
In view of this anatomy, it is evident that once the osteofibrous sheath has ruptured or detached from the ulna, the ECU tendon can luxate within and slide under the intact dorsal retinaculum.
Barfred et al4 described the possible duplication of the ECU at its inferior insertion. In a letter to the author, Hollister5 pointed out that anatomical variations in the ECU are not rare, and finally Nakashima6 found duplication in 82 of 240 wrists studied (34.2%).
The three clinical entities
Traumatic ECU instability (12 cases)
We saw 12 cases at the first presentation and were able to follow up eight (including diagnosis, medical treatment, and return to competition). Four players were lost to follow up.
This injury occurs suddenly and was described as being “like a bolt out of the blue”. If the player was performing a double handed backhand (10 cases), the hand closest to the racquet head was damaged. In the two cases that occurred during a forehand stroke, the dominant hand was involved. Pain at the ulnar side of the wrist was severe and the player was unable to resume play for a few minutes. Players most often describe the pain as violent but rarely reported rebound pain in the ulnar styloid (three cases). This clinical picture was slightly different in three cases in which the severe pain occurring after a particular stroke was managed by the players themselves with a tubular bandage and adaptation of their swing pattern (hitting a flatter stroke). This was followed two days later by recurrence of the pain as soon as the player tried to put topspin on the ball again.
The clinical examination conducted 1–30 days after the incident can be summarised as follows:
Intense pain on passive supination
Pain on palpation of the ECU tendon where it passes into the ulnar groove
Slight local swelling, which disappears after a few days
The remainder of the clinical examination was normal. During a clinical examination, an attempt must be made to reproduce the instability using isometric stress in both resisted supination and pronation. Sometimes a click can be produced or the sensations experienced during play are reproduced, indicating a traumatic instability.
Anatomically, two phenomena can occur: (a) the actual ECU retinaculum has completely ruptured and the tendon has left its sheath; (b) the tendon leaves the sheath during supination and recovers its position during pronation. This is full ECU luxation.7,8 Three possible kinds of damage to the actual retinaculum are described in the literature:9 ulnar rupture of the fibro‐osseous sheath, whereby the torn sheath lies superficial to the tendon (type A) (fig 4); radial disruption of the fibro‐osseous sheath, whereby the sheath lies in the ulnar groove beneath the tendon (type B); and detachment of the periosteum from the ulnar side of the ulna, whereby the fibro‐osseous sheath forms a false pouch (type C). These types will be discussed below (eight cases).
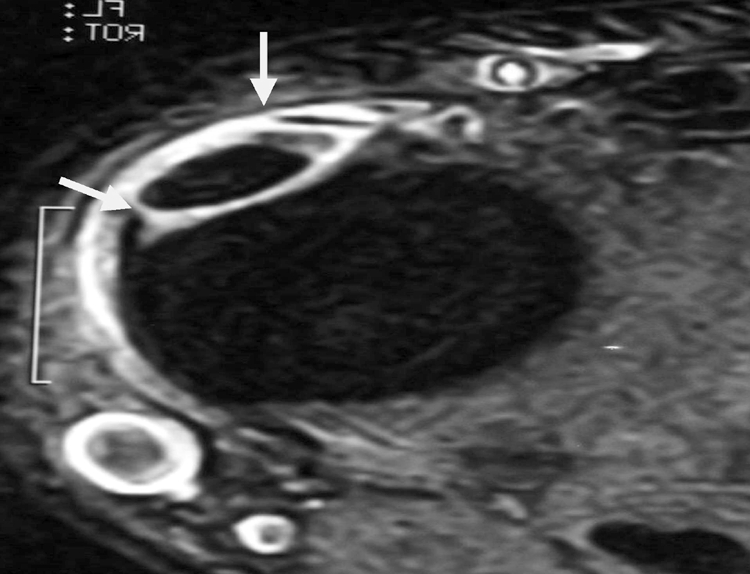
Figure 4 Magnetic resonance image showing that the extensor carpi ulnaris subsheath is completely torn.
Imaging
It is difficult to diagnose ECU instability, because it requires two particular imaging techniques, which require special expertise to detect a lesion of the ECU tendon. We use an original combination of two imaging techniques to reveal the instability of the ECU tendon outside its sheath.
An ultrasound scan at rest and during supination, using the method developed by JLB. From a technical point of view, preferably two operators should be present during the ultrasound examination in order to reproduce the tendon instability. One operator should attempt to reproduce the ECU instability using forced supination while the other person performs the ultrasound. True instability in which the tendon leaves and re‐enters its sheath is clearly visualised on dynamic ultrasound.
An MRI with millimetre thick slices of the ulnar sheath in T1, T1 STIR, T2, T2 and FATSAT GADO modes and comparative films obtained during pronation and supination by the method developed by JLD. Forced supination images show tendon subluxation, clear disorganisation of the retinaculum, and finally major detachment of the ECU retinaculum from the medial surface of the ulna.
Full ECU luxation (fig 5)
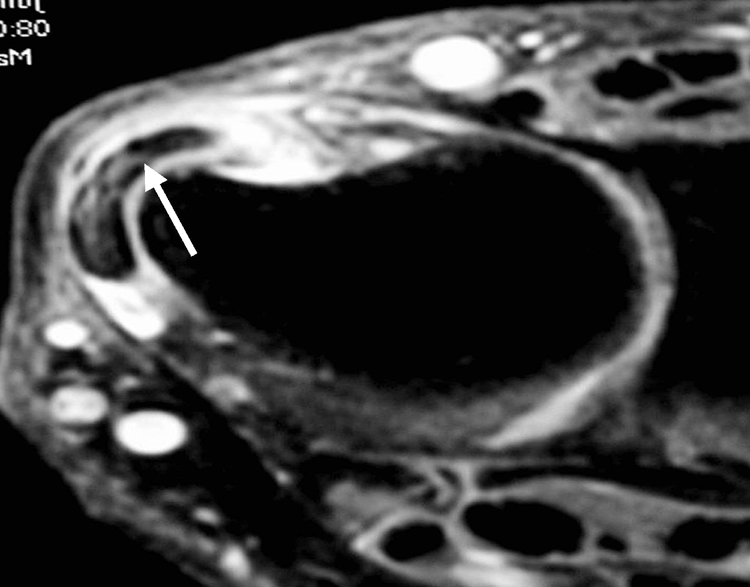
Figure 5 Magnetic resonance image showing instability of the extensor carpi ulnaris tendon.
The ECU tendon is diagnosed as unstable when MRI and ultrasound images concur. The following management strategy is then proposed (five cases): immobilisation of the wrist in a plaster cast for two to three months, with the wrist extended at 15°. The elbow is left free. The patient is asked to avoid any use of force with the elbow. Monthly combined MRI and ultrasound imaging studies should be performed to ensure that the ECU subsheath is healing and re‐inserting on to the head of the ulna.
Two months after the initial diagnosis, a stress test should be performed to check the stability of the tendon. If the tendon is stable, the player can return to the play after one month. If the actual tendon sheath has not healed around the tendon and along the head of the ulna, the wrist must be immobilised for another month, with the player wearing a support splint and avoiding all stressful supination movements.
Our experience has shown that this lengthy period of immobilisation (three or four months) results in complete and stable reconstruction of the 6th compartment, even in stressful positions. This is in contrast with the literature, which recommends surgical stabilisation for ECU luxation.8,10,11,12 It is interesting to note that the tendon often has an abnormal surgical appearance with longitudinal intratendinous fissures, but these do not hinder players once they have returned to tennis. We did not opt for surgery for these five players, because they returned to competition five to six months after the initial injury without any symptoms.
Surgery can also be envisaged as first line treatment. This consists of anatomical repair of the 6th compartment sheath using a fragment of the carpal dorsal retinaculum,8,9,11,13,14,15,16 followed by three to five weeks of immobilisation.
Damage to the retinaculum (fig 6)
Figure 6 The extensor carpi ulnaris (ECU) sheath is disorganised along the medial face of the ulnar head and the ECU is unstable.
When the ECU subsheath has detached from the medial face of the ulnar head and no longer ensures stability of the ECU in its sheath under stress, this is not true ECU luxation. The subsheath has not ruptured and the tendon is not luxated. It is potentially unstable (three cases).
In this case, clinical examination does not induce instability, and MRI must be used to look for signs of ECU sheath detachment along the medial edge of the ulnar head. Once detected, detachment should be monitored using ultrasound (fig 6). As long as an area of detachment exists, ECU instability is possible, and this can cause repeated tenosynovitis. We believe that it is important to take retinaculum detachment into account when scheduling the possible return of the player to the tennis court. This anatomical point is important because the clinical tests are falsely reassuring. The wrist should be immobilised in a plaster cast for at least six to eight weeks, in the same position as for a complete luxation.
During this immobilisation, the patient is monitored every four weeks using combined MRI and ultrasound (with stress test). If re‐insertion is not complete, immobilisation must be continued for up to 12 weeks in total. Our experience has shown that subsheath detachment is an important factor in ECU stability. The ECU tendon remains unstable for as long as the subsheath has not completely healed, and this instability is the source of recurring tenosynovitis. Return to play too early and the use of the double handed backhand will generate recurring pain. Our three players returned to competition about four months after the initial injury.
ECU tendinopathy (14 cases)
ECU tendinopathy develops gradually. The medical history is negative for an initial violent trauma or fall. This was also the case in the series of tendinopathies reported by Nachinolcar and Khanolkar,17 Solomon,18 and Futami and Moritoshi.20 Futami and Moritoshi reported that, out of 43 subjects, 40 recovered in one to nine months using a combination of rest, wrist support, and local corticosteroid injections.
In our series we assume that repeated microtraumas caused the pain. In general, it was possible to continue to play tennis despite the pain because, although the first strokes were painful, the pain improved after warm up.
Clinical examination shows ulnar sided wrist pain. Futami and Moritoshi20 described signs of pain during flexion and pronation, but we did not find this in our patients. However, pain with forced isometric supination was found in all of our cases. Slight swelling of the ulnar sheath associated with pain on palpation was sometimes observed.
Ultrasound examination showed normal stability of the ECU tendon without ulnar sided retinacular detachment. Fluid around the tendon, sometimes associated with tendon thickening or even intratendon fissures, was occasionally found. The longitudinal fissures of the ECU tendon appeared rounded in pronation and smoothed out in supination, particularly during subluxation when the tendon stretches across the inner face of the osseous groove. MRI, which was not performed in all cases, confirmed the absence of retinaculum detachment and the presence of frequent longitudinal fissures as seen on the ultrasound images.
In most cases, the pain resolved within two to 24 weeks. It should be noted that our series was made up of professional players who often continue to play tennis while managing their own pain. Four of fourteen cases were lost to follow up.
Rupture of the ECU (two cases)
Over the last 10 years we have observed two ECU ruptures presenting as ulnar pain recurring over a period of more than six months. An initial accident was usually noted followed by recurrent pain and alternating periods of enforced rest and play. Both patients had received injections (one three times and the other twice) before the rupture occurred.
The players reported that the impact on daily life was minimal, but they were unable to use a double handed backhand because of a lack of power in the wrist. Clinical examination showed a lack of ECU strength with isometric contraction: 15° ulnar inclination with wrist in extension. Passive supination was painless. The tendon could not be palpated in its sheath. Ultrasound confirmed that the ECU tendon sheath was empty.
Surgery is necessary if the player wants to return to his or her former level of play. The ECU tendon is reconstructed using the palmaris longus tendon,16 in combination with the reconstruction of the 6th compartment.10,12 Both these players were able to return to high level tennis six months after their operation.16
In the literature13,16,21,22,23 the following typical pattern is described: an elite athlete,16,23 an initial violent trauma, several episodes of ulnar sided wrist pain, several local corticosteroid injections, eventually ending in tendon rupture. These cases are similar to ours, and our hypothesis is that the following cascade of events leads to this injury: at the outset, the tendon is unstable in its incompletely healed sheath, local corticosteroids temporarily cure the inflammation, and the tendon then ruptures because of repeated sport induced microtraumas.
Discussion
ECU instability outside its ulnar sheath was first described by Vulpius8 in 1964. His description is very accurate: an initial violent movement, associated with combined pronation towards supination of the wrist and associated with ulnar deviation with high resistance to the ECU tendon. Rebound pain in the ulnar head is also sometimes reported. In his description, he even mentioned the tennis backhand, even though the double handed backhand was not in use at that time. Several authors10,12,13,14,15,16 have reported good results after reconstruction of the 6th compartment using a fragment of the carpal dorsal retinaculum.
A series of 12 cases observed over two years was described by Inoue and Tamura,9,11 providing new surgical evidence for the source of 6th compartment rupture, which they considered to be either ulnar sided or caused by detachment of the ECU subsheath along the ulnar side of the wrist.
What can our series of 28 tennis players contribute 35 years after Vulpius' description? Before we began to study this injury in tennis players, we noticed that, in certain cases, sudden onset, ulnar sided wrist pain could cause long term residual pain, preventing a return of the player to high level tennis. We made three major observations. Firstly, the swing pattern had a major impact on the pathology—that is, in players using a double handed backhand, the hand closest to the racquet head was affected in nine out of ten cases in our series (non‐dominant hand). Secondly, clinical examination was very misleading, as two to three weeks after the initial insult, it contributes very little except for painful forced passive supination. Finally, the combined use of two imaging methods allowed us to identify more clearly the anatomical damage caused by the initial trauma and most importantly to monitor healing. The initial description of Burkhart et al14 mentions six weeks of immobilisation. We propose tailoring of treatment depending on the initial anatomical damage. We recommend using ultrasound, which allows stress testing in supination, and MRI with T2, T2 FAT, T1 STRIR images, taking millimetre thick sections of the ulnar sheath and the ECU tendon, to monitor the healing process and define an appropriate convalescent period.
What is already known on this topic
The pathology of the extensor carpi ulnaris tendon has been well described, but the clinical picture and imaging only briefly reported
Treatment is essentially surgical
What this study adds
Twenty eight cases of extensor carpi ulnaris tendon pathology in professional tennis players are reported; the non‐dominant hand of a player with a double handed backhand is affected most often
Monitoring of the healing process depends on the use of magnetic resonance imaging in conjunction with dynamic ultrasound
In the event of total luxation of the ECU tendon, time to complete recovery is three to four months. In patients with subluxation of the ECU tendon and disorganisation of the tendon subsheath along the medial side of the head of the ulna, recovery takes two to three months. If the tendon subsheath has not detached, the ECU tendon remains stable and the healing process is more rapid, taking four to six weeks. The description of the anatomy by Inoue and Tamura9 is extremely interesting. We found their detached retinaculum (type C), but to date have had difficulty in identifying types A and B using imaging methods. Finally, we are now more optimistic about the chances of successfully healing the 6th compartment, using a longer immobilisation period than those previously reported in the literature. It should be noted that our players sought medical advice shortly after the initial injury and did not continue to use the affected wrist, which may have had a positive impact on their recovery. Most other authors advocate surgery to reconstruct the ECU retinaculum and render it sufficiently stable.
Conclusions
We present a series of 28 cases of ECU pain in elite tennis players. We have identified three clinical entities: traumatic instability of the ECU tendon, ECU tendon rupture, and ECU tendinopathy. Each clinical entity requires different therapeutic management. Ultrasound with stress tests and MRI are useful as diagnostic tools and to help monitor the healing process. Anatomical identification of the actual ECU retinaculum and its lesions remain key elements in the stability of the ECU and ulnar sided wrist pain in high level tennis players.
Abbreviations
ECU - extensor carpi ulnaris
MRI - magnetic resonance imaging
Footnotes
Informed consent was obtained for publication of figure 3
Competing interests: none declared
References
- 1.Rouviere H.Anatomie humaine. Paris: Masson, 1970s
- 2.Spinner M, Kaplan E B. Extensor carpi ulnaris. Its relationship to the stability of the distal radio‐ulnar joint. Clin Orthop Rel Res 197068124–129. [PubMed] [Google Scholar]
- 3.Taleisinik J, Gelberman R H, Miller B W.et al The extensor retinaculum of the wrist. J Hand Surg [Am] 19849495–501. [DOI] [PubMed] [Google Scholar]
- 4.Barfred T, Adamsen A, Odense P. Duplication of the extensor carpi ulnaris tendon. J Hand Surg [Am] 199611423–425. [DOI] [PubMed] [Google Scholar]
- 5.Hollister A. Duplication of extensor carpi ulnaris tendon. J Hand Surg 1987112809–810. [DOI] [PubMed] [Google Scholar]
- 6.Nakashima T. An accessory extensor digiti minimi arising from extensor carpi ulnaris. J Anat 1993182109–112. [PMC free article] [PubMed] [Google Scholar]
- 7.Rayan G M. Recurrent dislocation of the extensor carpi ulnaris in athletes. Am J Sports Med 198311183–184. [DOI] [PubMed] [Google Scholar]
- 8.Vulpius Habitual dislocation of the extensor carpi ulnaris tendon. Acta Orthop Scand 196434105–108. [DOI] [PubMed] [Google Scholar]
- 9.Inoue G, Tamura Y. Recurrent dislocation of the extensor carpi ulnaris tendon. Br J Sports Med 199832172–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eckardt W A, Palmer A K. Recurrent dislocation of the extensor carpi ulnaris tendon. J Hand Surg [Am] 19816629–631. [DOI] [PubMed] [Google Scholar]
- 11.Inoue G, Tamura Y. Surgical treatment for recurrent dislocation of the extensor carpi ulnaris tendon.J Hand Surg 200126556–559. [DOI] [PubMed] [Google Scholar]
- 12.Loty B, Meunier B, Mazas F. Luxation traumatique isolée du tendon cubital postérieur. Rev Chir Orthop Reparatrice Appar Mot 198672219–222. [PubMed] [Google Scholar]
- 13.Allende C, Le Viet D. Extensor carpi problems at the wrist: classification, surgical treatment and results.J Hand Surg [Br] 200530265–272. [DOI] [PubMed] [Google Scholar]
- 14.Burkhart S S, Wood M B, Linscheid R L. Posttraumatic recurrent subluxation of the extensor carpi ulnaris tendon. J Hand Surg [Am] 198271–3. [DOI] [PubMed] [Google Scholar]
- 15.Palmer A K, Shaken J R, Werner F W.et al The extensor retinaculum of the wrist; an anatomical and biomechanical study. J Hand Surg [Br] 19851011–16. [DOI] [PubMed] [Google Scholar]
- 16.Xarchas K C, Le Viet D. Non rheumatoid closed rupture of extensor carpi ulnaris tendon. Report of a case in a professional athlete. Acta Orthop Belg 200268399–402. [PubMed] [Google Scholar]
- 17.Nachinolcar U G, Khanolkar K B. Stenosing tenovaginitis of extensor carpi ulnaris: brief report. J Bone J Surg [Br] 198870842. [DOI] [PubMed] [Google Scholar]
- 18.Rowlands A. Acute traumatic subluxation of the extensor carpi ulnaris tendon at the wrist. J Hand Surg [Am] 198611809–811. [DOI] [PubMed] [Google Scholar]
- 19.Solomon L. Tenovaginitis of the extensor carpi ulnaris. South Afr Med J 19643842–44. [PubMed] [Google Scholar]
- 20.Futami T, Moritoshi I. Extensor carpi ulnaris syndrome. Acta Orthop Scand 199566538–539. [DOI] [PubMed] [Google Scholar]
- 21.Angerman P. Post traumatic partial rupture of the extensor carpi ulnaris tendon. Scand J Hand Surg 199327321–322. [PubMed] [Google Scholar]
- 22.Chun S, Palmer A K. Chronic ulnar wrist pain secondary to partial rupture of the extensor carpi ulnaris tendon. J Hand Surg [Am] 1987121032–1035. [DOI] [PubMed] [Google Scholar]
- 23.Wang C, Gills T J, Zarins B.et al Extensor carpi ulnaris tendon rupture in an ice hockey player: a case report. Am J Sports Med 200331459–461. [DOI] [PubMed] [Google Scholar]