Abstract
Background
Several investigators have suggested that passive tissue characteristics of the lumbar region may be altered in people with low back pain. Passive stiffness of the lumbar region has been examined during physiological movements in healthy individuals and intersegmental spine mobility and stiffness have been examined in people with and people without low back pain. However, no investigators have examined differences in passive tissue characteristics of the lumbar region during a physiological movement between people with and people without low back pain.
Methods
Subjects were moved passively through a trunk lateral bending motion on a passive movement device. Lumbar region kinematics were measured with a motion capture system and force required to move the subject was measured with a force transducer. Lumbar region extensibility was defined as the maximum excursion of the lumbar region. Passive elastic energy was defined as the area under the torque-lumbar region angle curve. Differences in lumbar region extensibility and passive elastic energy between sides were examined in people with and people without low back pain (n = 41).
Findings
People in the Rotation with Extension low back pain subgroup demonstrated greater asymmetry of passive elastic energy than people without low back pain (P = 0.04). There were no differences between groups in symmetry of lumbar region extensibility (P = 0.37).
Interpretation
Asymmetry in passive elastic energy of the lumbar region may be related to the low back pain problem in the Rotation with Extension subgroup. The asymmetry in passive elastic energy may be associated with asymmetry of loading on the spine, which has been reported to be a risk factor for low back pain. Thus, it may be important to consider the asymmetry when planning an intervention strategy for people in the Rotation with Extension subgroup.
Keywords: low back pain, passive, trunk lateral bending, stiffness
Introduction
Prior researchers have suggested that movement and alignment patterns people with low back pain (LBP) display during a clinical examination may be related to the LBP problem.(Van Dillen et al 2001; Van Dillen et al 2003a) A number of factors have been theorized to contribute to the movement and alignment patterns that people with LBP display.(Langevin & Sherman 2007; Panjabi 1992; Sahrmann 2002) The two types of factors most often noted are (1) neural control factors, and (2) biomechanical factors. Neural control factors include the timing or magnitude of trunk muscle activity either during activities that require movement of the trunk or during activities that require the trunk to remain stable.(Hodges & Richardson 1996; Hodges & Richardson 1998) Biomechanical factors may include anthropometric characteristics or passive tissue characteristics of the lumbar region. The focus of the current study is on measures of lumbar region passive tissue characteristics. Such characteristics potentially are important because they may reflect the passive resistance produced by structures of the lumbar region during a trunk movement in vivo.
Lumbar region passive tissue characteristics have been examined in vivo during a variety of trunk movements in healthy individuals.(Beach et al 2005; McGill et al 1994; Parkinson et al 2004) Investigators also have examined posterior-anterior mobility and stiffness of individual lumbar spine segments in people with and people without LBP.(Keller et al 2000; Kulig et al 2007; Lee et al 1998) To our knowledge no investigator has examined passive tissue characteristics of the lumbar region during a physiological movement in people with and people without LBP. Understanding the passive characteristics of the lumbar region in people with LBP is important because alterations in passive structures secondary to acute injury,(Zhao et al 2005) degenerative changes,(Burton et al 1996; Gay et al 2006) repeated lumbar movements,(Zhao et al 2005) or sustained lumbar positions, could result in changes in the load-bearing and stabilizing capacity of these structures.(Langevin & Sherman 2007; Panjabi 1992) Changes in the load-bearing and stabilizing capacity of passive structures may contribute to alterations in movement patterns and loading of the spine, and potentially a LBP problem. (Mueller & Maluf 2002; Sahrmann 2002)
Specifically, asymmetry of passive tissue characteristics may be especially important to examine in people with LBP. Asymmetry of passive characteristics may be either a reflection of, or a factor contributing to asymmetrical loading on the spine. The relationship between asymmetrical loading and LBP has been studied widely in occupational settings. Compared to symmetrical lifting tasks, reported increases in lateral flexion and rotation moments and decreases in muscle activity during asymmetrical tasks are proposed to result in an increase in lateral shear forces in the spine.(Granata & Marras 1995; Kingma et al 1998; Marras & Mirka 1992; Sbriccoli et al 2004; van Dieen & Kingma 1999) The increase in shear forces associated with the asymmetrical tasks could increase shear stresses,(Ueno & Liu 1987) induce changes in mechanical properties of spine tissues, and cause microdamage to the viscoelastic structures.(Mueller & Maluf 2002; Sbriccoli et al 2004) The tissue changes resulting from an increase in shear forces could provide an explanation for the reported increased risk for development of LBP with asymmetrical movements.(Marras et al 1995)
Asymmetry of passive tissue characteristics may be of particular importance for a specific subgroup of people with LBP. Previously, we reported on differences in symmetry of lumbar region movement during trunk and limb movements between two subgroups of people with LBP.(Gombatto et al 2007a; Van Dillen et al 2007) Subgroups were identified based on reports of symptom behavior and the direction of movement and alignment patterns observed during a standardized clinical examination.(Sahrmann 2002) Specifically, the subgroup of people who demonstrated a predominance of movement and alignment deviations and increased LBP symptoms with lumbar region rotation and extension movements (the Rotation with Extension subgroup) also demonstrated asymmetry of lumbar region motion during trunk lateral bending compared to the subgroup of people with deviations and increased LBP symptoms with rotation movements (the Rotation subgroup). The asymmetry of lumbar region motion was most evident early in the range of trunk lateral bending and is proposed to be related to the LBP problem for people in the Rotation with Extension subgroup. Based on the prior data, people in the Rotation with Extension subgroup may be more likely than people in other LBP subgroups to demonstrate asymmetry of passive tissue characteristics.
The purpose of the current study was to examine differences in symmetry of passive tissue characteristics of the lumbar region during passive trunk lateral bending between people with and people without LBP. Based on the prior data, we hypothesized that people in the lumbar Rotation with Extension subgroup would exhibit greater asymmetry of passive tissue characteristics across the trunk lateral bending motion (passive elastic energy) compared to people without a history of LBP. We also hypothesized there would be no differences in symmetry of end range lumbar region motion (extensibility) between groups. Examining differences in passive tissue characteristics between a subgroup of people with LBP and people without LBP is clinically important to (1) assist in understanding the relationship between lumbar region passive tissue characteristics and the LBP problem, (2) assist in selecting the most appropriate intervention, and (3) provide information to judge prognosis for success with the specific intervention.
Methods
Subjects
We examined passive tissue characteristics of the lumbar region during a trunk lateral bending movement in 41 people (men=18, women=23; mean 30.8 (SD 8.9) years). Twenty-two people in the sample who reported a history of chronic or recurrent LBP for at least 6 months(Von Korff 1994) were examined and then classified in the Rotation with Extension subgroup.(Sahrmann 2002) Nineteen people in the sample reported no history of LBP. Because gender, age, and body mass index are factors that could contribute to differences in passive tissue characteristics, people with no history of LBP were tested only if the person could be matched to a participant in the LBP group based on these variables. Characteristics of subjects in both groups are summarized in Table 1. There were no statistically significant differences between groups in gender distribution, age, or body mass index. People with LBP were excluded from participating in the study if they were in an acute flare-up of the LBP problem on the day of testing,(Von Korff 1994) if they verbally reported a history of spinal fracture or surgery, or had been diagnosed by a physician with spinal deformity, a systemic inflammatory condition or another serious medical condition. They were also excluded if their LBP at the time of testing exceeded 3/10 on an 11 point verbal numeric rating scale (0–10, 10=worst possible pain),(Downie et al 1978; Jensen et al 1994) because LBP symptoms have the potential to affect the person’s ability to relax with passive movements. The testing protocol was approved by the Human Studies Committee at Washington University School of Medicine and all subjects provided informed consent.
Table 1.
Characteristics of people in the Rotation with Extension low back pain (LBP) subgroup compared to people without LBP.
| Characteristic | People in Rotation with Extension LBP subgroup |
People without LBP |
Confidence intervals of the group difference |
Statistic, degrees of freedom (df), P-value |
|---|---|---|---|---|
| (n=22) | (n=19) | |||
| Age (y), Mean (SD) | 31.23 (9.43) | 30.32 (8.45) | −6.61 – 4.78 | t = −0.32, df = 39, P = 0.75 |
| Gender (n) | Female (N=14) Male (N=8) |
Female (N=9) Male (N=10) |
not applicable |
χ2 = 1.10,df = 1, P = 0.30 |
| Mass (kg), Mean (SD) | 68.71 (11.71) | 70.21 (15.10) | −6.98 – 9.98 | t = 0.36, df = 39, P = 0.72 |
| Height (cm), Mean (SD) | 169.20 (9.10) | 169.21 (9.62) | −5.90 – 5.93 | t = 0.00, df = 39, P =1.0 |
| Body Mass Index (kg·m2), Mean (SD) | 23.97 (2.92) | 24.24 (3.02) | −1.60 – 2.15 | t = 0.30, df = 39, P = 0.77 |
| Baecke Score (3–15), Mean (SD) | 8.52 (2.48) | 8.91 (1.04) | −0.84 – 1.63 | t = 0.64, df = 39, P = 0.53 |
Subjects completed self-report measures including the following: (1) demographic and LBP-history questionnaire,(Deyo et al 1994) (2) verbal numeric rating scale of symptoms (LBP group only),(Downie et al 1978; Jensen et al 1994) (3) Modified Oswestry Disability Index,(Fritz & Irrgang 2001) and (4) Baecke Habitual Activity questionnaire.(Baecke et al 1982) The data from self-report measures for both groups are summarized in Table 1 and LBP history and symptom characteristics for people in the Rotation with Extension subgroup are summarized in Table 2 and Table 3.
Table 2.
Low back pain (LBP) history and symptom characteristics for people with LBP in the Rotation with Extension subgroup (N=22).
| Characteristic | Mean (SD) | Range |
|---|---|---|
| Symptom intensity (0–10) | ||
| Current (0–10) | 1.25 (0.91) | 0.0 – 3.5 |
| Average over past 7 days (0–10) | 2.27 (1.30) | 0.0 – 5.5 |
| Duration of LBP (y) | 6.93 (4.56) | 0.5 – 20.0 |
| Number of flare-ups of LBP in the past 12 months | 2.96 (2.27) | 0 – 10 |
| Modified Oswestry Disability Index Score (0–100%) | 13.64 (8.36) | 2.0 – 40.0 |
Table 3.
Number of people (n) in the Rotation with Extension low back pain subgroup with increased LBP during passive trials by side to which passive elastic energy is greater (N=22)*
| Direction of increased LBP | Side to which passive elastic energy is greater |
||
|---|---|---|---|
| Left | Right | ||
| left trunk lateral bending | 2 | 3 | χ2 = 3.5, 3 df, P=0.33 |
| right trunk lateral bending | 1 | 1 | |
| both right and left | 4 | 3 | |
| neither | 1 | 7 | |
Based on at least one of the three trunk lateral bending trials.
Examination and Classification
Each subject was examined by a physical therapist using a standardized clinical examination and people with LBP were classified into subgroups based on the examination.(Sahrmann 2002) The previously described standardized examination involves a series of clinical tests during which the examiner observes postures and movements in various positions and monitors LBP symptoms. At the conclusion of the examination, a person’s LBP problem is classified into one of 5 diagnostic subgroups based on the direction of lumbar region movement or alignment deviations that are consistently observed and associated with an increase in LBP symptoms across the examination.(Norton et al 2004; Sahrmann, 2002; Van Dillen et al 2003b) Low back pain subgroups include the following: (1) Extension, (2) Flexion, (3) Rotation, (4) Rotation with Extension, or (5) Rotation with Flexion.(Sahrmann 2002) Validity and reliability of the examination and classification system have been studied and found to be acceptable.(Norton et al 2004; Turner et al 2005; Van Dillen et al 1998; Van Dillen et al 2003b) In the samples of people from prior studies, and in the current study, the lumbar Rotation with Extension (RotExt) LBP subgroup was the most prevalent subgroup of people with LBP.(Gombatto et al 2007a; Turner et al 2005; Van Dillen et al 2003b) Also, data from prior studies suggest that people in the RotExt subgroup display asymmetry of movement during clinical tests.(Gombatto et al 2007a; Van Dillen et al 2007) Because the focus of the current study is on examining asymmetry of lumbar region passive tissue characteristics, analyses were conducted only on people in the RotExt subgroup compared to people without LBP.
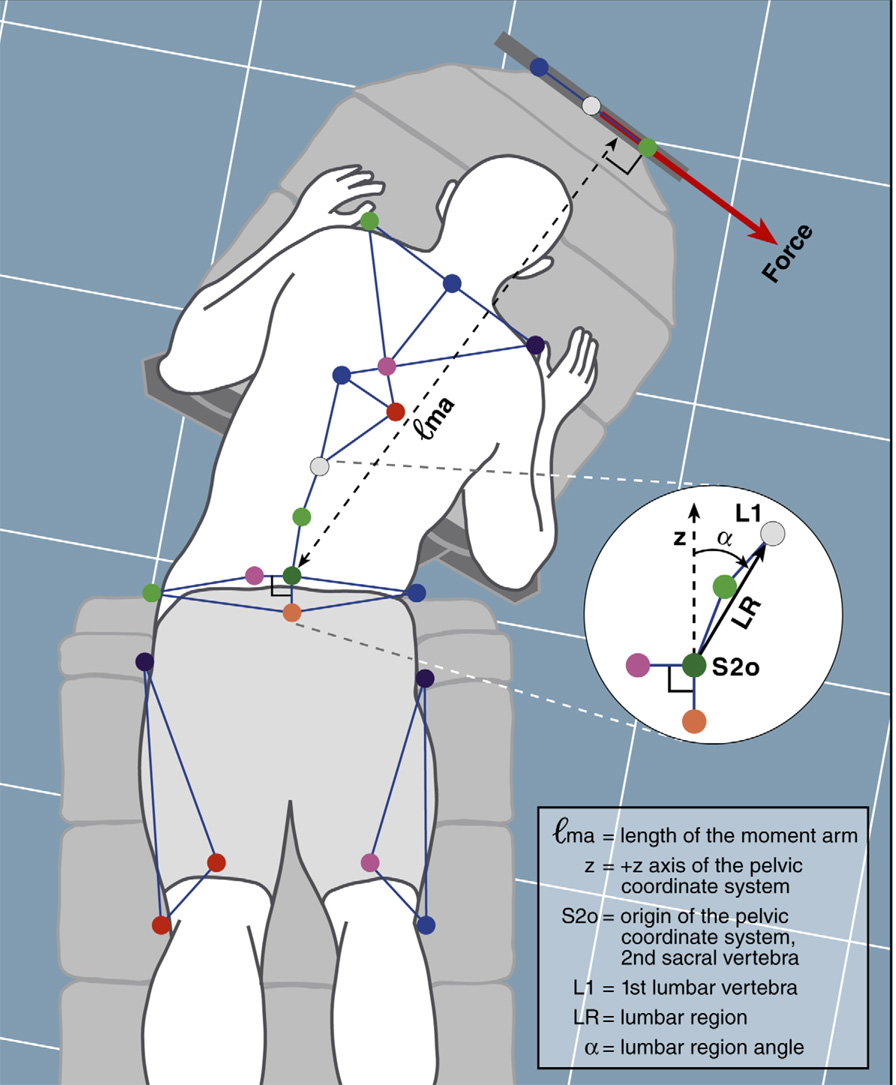
Instrumentation
The system that was used to measure passive tissue characteristics of the lumbar region consists of a passive movement device, a 6 camera, 3-dimensional, motion capture system (Motion Analysis Corporation, Santa Rosa, CA, USA), and a Myosystem 1400A surface electromyography system (Noraxon, Inc., Scottsdale, AZ, USA). The passive movement device is a modification of a device described by McGill and colleagues.(McGill et al 1994) The device consists of a table, platform, moveable cradle with air bearings, two force transducers, and a guide (Figure 1). The table is used to stabilize the pelvis and lower extremities and the cradle is used to move the subject’s trunk during passive movements. The three porous air bearings (NewWay®, Inc., Aston, PA, USA) located on the underside of the cradle are continuously supplied with compressed air, so the cradle allows virtually frictionless movement of the trunk in a single plane. Two force transducers with a 222.4 Newtons (50 pounds) capacity (Omegadyne®, Inc., Sunbury, OH, USA) and a metal guide are attached to the distal end of the moveable cradle. The guide forms a normal tangent with the distal end of the cradle. A cable is attached to each transducer to apply force to the cradle in line with the metal guide and move the cradle and subject through a trunk lateral bending motion. The signal from the force transducer is amplified and then sampled at 1200 Hz. The transducer signal is converted through a 12 bit analog to digital board (resolution of 0.13 Newtons) and synchronized in time with kinematic data using the motion capture software. Each transducer was tested and demonstrated linearity of ≥ 0.99 and maximal hysteresis of 0.89 Newtons. Before each testing session, the transducers were calibrated so that changes in transducer signal across time during the trunk lateral bending movement could be interpreted as changes in force. Force data were filtered with a 45 Hz, 4th order, dual low-pass, Butterworth filter.
Figure 1.
Passive movement device.
Kinematic data was collected during the trunk lateral bending motion with the motion capture system. The sampling rate of each camera was 60 Hz, and the resolution of the system was 1 millimeter for a volume of 1 cubic meter. Kinematic measurements during trunk lateral bending were calculated based on data from reflective markers. Locations of the reflective markers are illustrated in Figure 2. Kinematic data were filtered using a 4th order, dual low-pass Butterworth filter with a cutoff frequency of 1 Hz. The filter frequency cutoff was chosen based on the average speed of passive movements for people with and people without LBP (mean 1.9 (SD 0.4) degrees/second).(Winter 2005)
Figure 2.
Marker locations, kinematic and force measures with the passive movement device.
Electromyographic (EMG) activity of agonist and antagonist muscles were monitored using bipolar surface electrodes with an interelectrode separation of 2 centimeters. Electrodes were placed on the external oblique and lumbar erector spinae muscles, bilaterally. Electrodes for the external oblique muscles were placed on the lateral most portion of the muscle, inferior to the ribs, and oriented parallel to the muscle fibers. Electrodes for the lumbar erector spinae muscles were placed 3 centimeters lateral to the third lumbar spinous process (L3), and oriented parallel to the muscle fibers.(McGill 1991) Electromyographic data were sampled at a rate of 1200 Hz and bandpass filtered during data collection at 10-500 Hz. The EMG data were converted with a 12 bit analog to digital board and synchronized in time with kinematic data using the motion capture software. The EMG data were full-wave rectified, filtered with a 45 Hz, 4th order, dual low-pass, Butterworth filter using custom software.(Hodges & Richardson 1999; Winter 2005)
Passive Movement Testing Procedures
The examiner palpated anatomical landmarks and marked the locations for reflective markers (Figure 2). Electromyography electrodes then were applied and maximum voluntary isometric contraction (MVIC) testing was performed for the external oblique and lumbar erector spinae muscles in supine and prone respectively. The examiner applied the resistance. For each MVIC test, EMG activity was recorded with the motion capture system and maximum EMG activity of each muscle was identified with a custom software program. During passive movement testing, muscle activity was monitored and was expressed as a percentage of the individual’s MVIC. A movement was considered passive if the activity of muscles opposing the movement direction did not exceed 2% of the subject’s MVIC for a period of 0.3 seconds during the trial.(Scannell & McGill 2003)
Each person was placed in prone on the passive movement device in the following manner (Figure 1 and Figure 2): (1) pelvis and lower extremities on the table, (2) iliac crests in line with the end of the table, (3) pelvis aligned in neutral rotation, (4) 4th lumbar vertebra centered between the table and moveable cradle, and (5) trunk supported on the cradle to the level of the 3rd lumbar vertebra. Versa-form pillows, padded clamps, and straps were used to secure the subject to both the table and cradle, with the most inferior strap on the cradle positioned just above the first lumbar spinous process. The examiner placed the reflective markers on the subject and the device (Figure 1 and Figure 2). Then the lumbar region was placed in a neutral position, defined as the position at which L1, L4 and S2 were collinear. Accuracy of the neutral position was confirmed by collecting kinematic data with the lumbar region in the neutral position and calculating the lumbar region angle with a custom software program. If the calculated lumbar region angle was not within one degree of zero, then the neutral position was corrected. The identified neutral position was marked as the starting position of the cradle for each trial.
For each passive trunk lateral bending movement, the subject was instructed to relax completely while the examiner moved him through a maximum range of motion. Speed of movement was controlled by moving the cradle a fixed distance for each beat of a metronome (at 72 beats per minute). The trial was concluded when either the (1) subject verbally reported that he/she “was unable to be moved any further or had LBP symptoms such that he/she did not wish to continue the trial” or, (2) examiner was unable to apply additional force.(McGill et al 1994) The side (right or left) to which a person was moved first was randomized, and the tester moved the subject for at least three practice passive trials before beginning testing in a new movement direction. Practice trials were performed to account for viscoelastic creep in tissues of the lumbar region(Kurutz 2006) and to insure a stable passive measure. Three repetitions of passive trunk lateral bending then were performed to each side. Change in LBP symptoms during each trunk lateral bending movement compared to symptoms in the neutral position were reported by the subject using the verbal numeric rating scale. A subject was considered to have increased symptoms with a passive trunk lateral bending movement if LBP increased during at least one of the three passive trials in the specified direction.
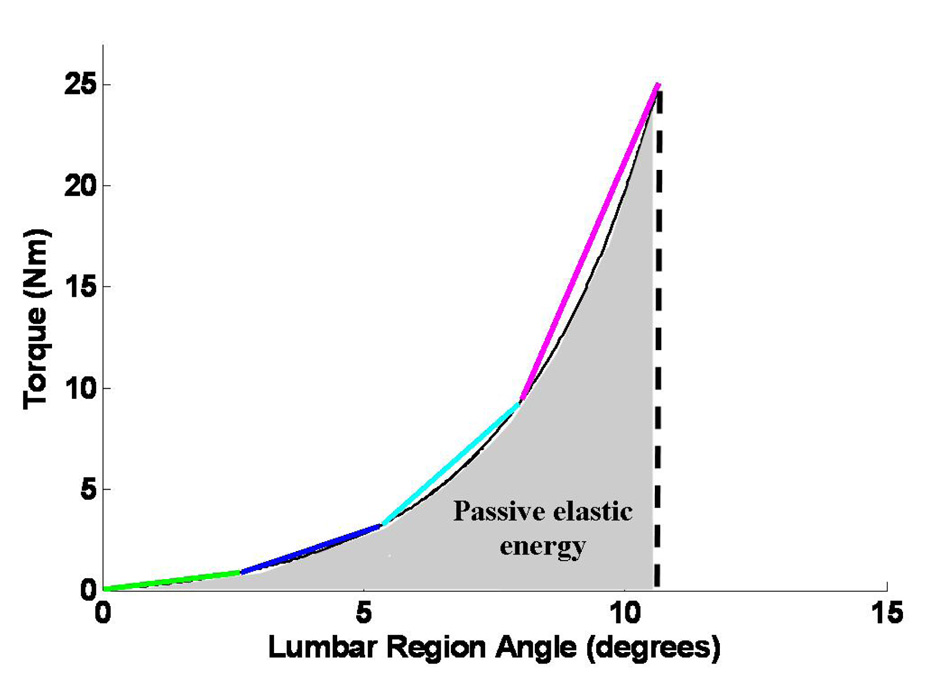
Measures of Passive Tissue Characteristics
Several terms are used across the literature to describe passive tissue characteristics, but the terms often are not clearly defined.(Gajdosik 2001) In the interest of clarity, for the current study, passive lumbar region extensibility is defined as the maximum lumbar region angle attained during a passive trunk movement. Passive elastic energy is defined as the area under the torque-lumbar region angle curve. Passive elastic energy reflects the torque required for displacement of the lumbar region across the range of movement and is a composite measure of torque at neutral and at maximum lumbar region motion, lumbar region stiffness (slope of the torque-lumbar region angle curve), and lumbar region extensibility (Figure 3).
Figure 3.
Representative torque-lumbar region angle curve for one subject.
The lumbar region segment was defined by a vector from a reflective marker on the second sacral spinous process to a marker on the first lumbar spinous process (L1)(Figure 2). The lumbar region angle (α) was defined as the relative angle between the lumbar region segment and the superior-inferior axis of a local pelvic coordinate system (Figure 2). Lumbar region extensibility was calculated as the maximum lumbar region excursion attained during the trunk lateral bending movement. Lumbar region extensibility measures used in the current study were tested for validity and reliability. Compared to a criterion standard, extensibility measures demonstrated good validity (r = 0.98) and an average error of 0.35° (SD 0.46°).(Gombatto et al 2007b) Repeated measures of lumbar region extensibility also demonstrated good reliability; intraclass correlation coefficients exceeded 0.85 both in people with and people without LBP.(Gombatto et al 2007b) The axis of rotation for the lumbar region was defined by a single marker on the second sacral spinous process. The line of action of the force was defined by two collinear markers on the guide. The length of the moment arm was defined as the linear distance between the axis of rotation and the line of action of the force (Figure 2).
The force required to pull an individual passively through a trunk lateral bending movement was measured with the force transducers. Measures of force were tested and demonstrated acceptable validity when compared to a criterion standard (r ≥ 0.99) and the average error was 0.40 (SD 0.27) Newtons.(Gombatto et al 2007b) The torque applied to the lumbar region during trunk lateral bending was the force (in Newtons) multiplied by the moment arm length (in meters). Derived measures of torque demonstrated an average error of 0.72 N·m.(Gombatto et al 2007b) Torque-lumbar region angle curves were generated for each trunk lateral bending movement. Then the curves were fit with an exponential function(McGill et al 1994) and examined from the start of lumbar region movement to the point of maximum lumbar region movement (Figure 3). Passive elastic energy was defined as the area under the torque-lumbar region angle curve.(McGill et al 1994) The value for passive elastic energy was used to index passive resistance to lumbar region movement across the trunk lateral bending range of motion (Figure 3). Repeated measures of passive elastic energy were tested for reliability in people with and people without LBP. The measures demonstrated good reliability with intraclass correlation coefficients of ≥ 0.79.(Gombatto et al 2007b) An average of the measures from the three repetitions of trunk lateral bending in each direction was calculated. The average measure for lumbar region extensibility and passive elastic energy then was used for data analysis. Because asymmetry of passive characteristics could exist with values for right trunk lateral bending greater than values for left, or for left greater than right, we identified the side to which values for passive characteristics were greater (greater side) and the side to which passive characteristics values were less (lesser side).
Analyses
Independent t-tests were performed to test for differences in subject characteristics between people in the RotExt subgroup and people without LBP (Table 1). For people in the RotExt LBP subgroup, a chi-square analysis was performed to test for differences in distribution of LBP symptom behavior (increased pain during testing to the right, left, both, neither) during the passive movement between the side of greater and lesser passive elastic energy (right, left). Separate two-way, mixed model analysis of variance tests were conducted on lumbar region extensibility and passive elastic energy to test for main and interaction effects of group and side. The within-subjects factor in each analysis was side with two levels, greater and lesser. The between-subjects factor was group with two levels, RotExt LBP and no LBP. Post-hoc analyses were conducted for a significant interaction effect. All significance testing values were set at P ≤ 0.05.
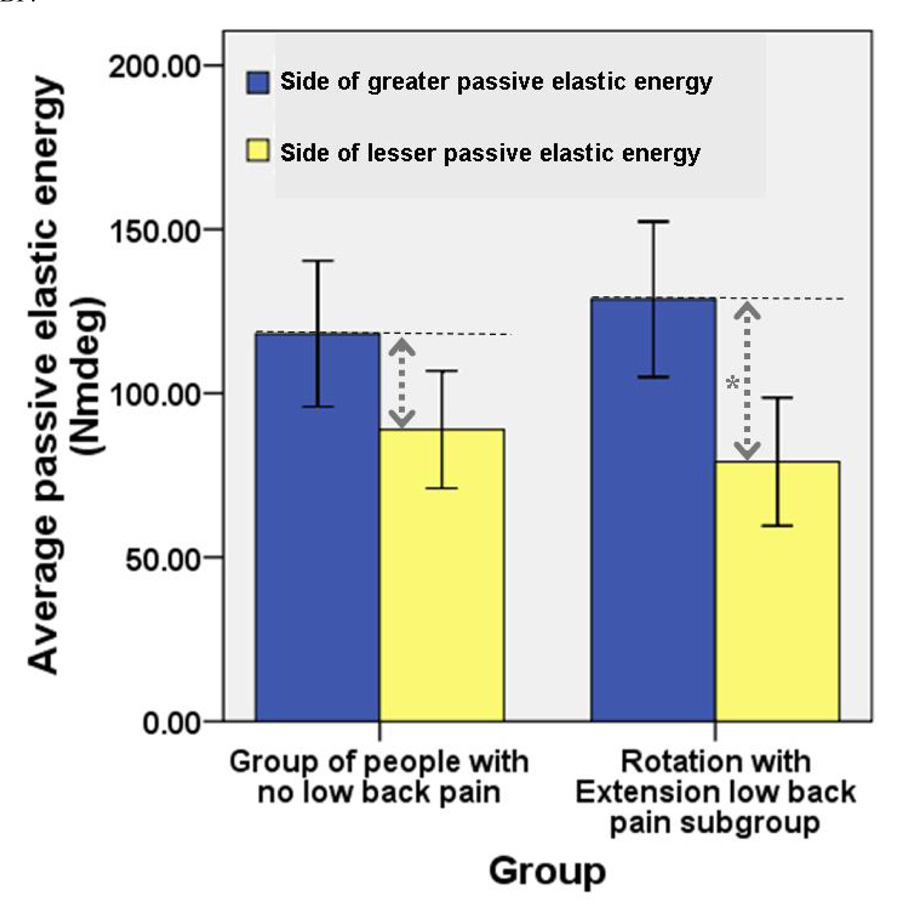
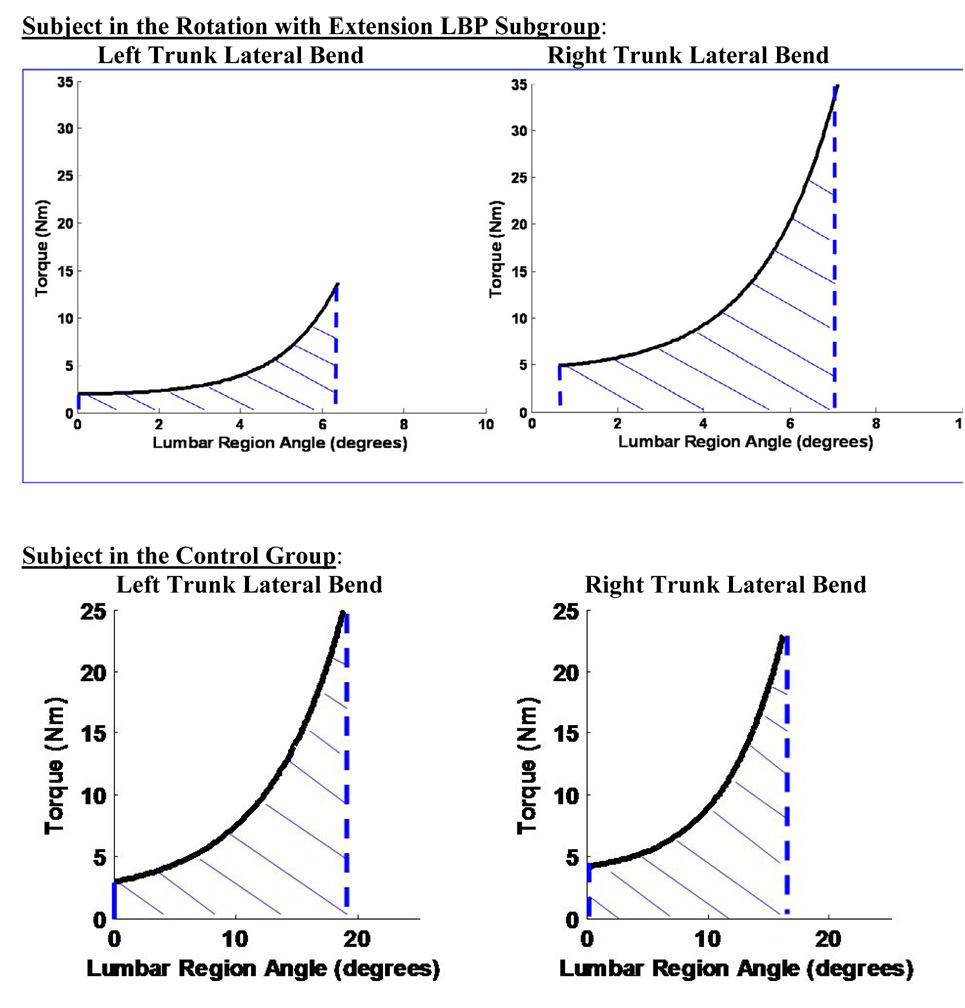
Results
There were no differences in subject characteristics between people in the RotExt subgroup and people without LBP (Table 1). There were no differences in distribution of LBP symptom behavior between the side of greater and lesser passive elastic energy (Table 3). The main effect of group was not significant for either lumbar region extensibility (P=0.58) or passive elastic energy (P=0.98) (Figure 4). The group by side interaction effect for lumbar region extensibility was not significant (P=0.37) (Figure 4). There was a significant group by side interaction effect (P=0.04), however, for lumbar region passive elastic energy (Figure 4). Post-hoc testing indicated that people in the RotExt subgroup displayed a greater difference in passive elastic energy between sides (mean 49.52 (SD 35.13) N·m·deg) than people without LBP (mean 29.23 (SD 21.36) N·m·deg)(t=−2.19, df = 39, P=0.04). Figure 5 displays the torque-lumbar region angle curves for trunk lateral bending to each side for a representative subject from each group. The figure illustrates the greater asymmetry in passive elastic energy for a person in the RotExt subgroup compared to a person without LBP.
Figure 4.
Mean (95% confidence interval) passive elastic energy with each direction of trunk lateral bending for people in the Rotation with Extension low back pain (LBP) subgroup compared to people with no LBP.
* Indicates a significant interaction of group and side (P=0.04)
Figure 5.
Torque-lumbar region angle curves for passive trunk lateral bending to the left and to the right for one representative subject in the Rotation with Extension low back pain subgroup and one representative subject in the control group.
Discussion
Summary of findings and importance
There were no statistically significant differences in overall lumbar region extensibility or passive elastic energy between people in the RotExt subgroup and people without LBP. There were no statistically significant differences between groups in symmetry of end-range lumbar region extensibility. People in the RotExt subgroup, however, demonstrated greater asymmetry of lumbar region passive elastic energy during trunk lateral bending compared to people without LBP. Based on these data, asymmetry of lumbar region passive characteristics across the range of the trunk lateral bending motion may be related to the LBP problem for people in the RotExt subgroup. Asymmetry of passive end-range lumbar region extensibility, however, does not appear to be related to the LBP problem in this subgroup. Asymmetry of passive characteristics across the trunk lateral bending motion either may be a factor contributing to, or reflect asymmetry of loading in the lumbar region. Asymmetry of loading has been reported as a risk factor for the development of a LBP problem.(Marras et al 1995) Asymmetry of passive characteristics during the trunk lateral bending motion in the RotExt subgroup may be an important factor to consider when deciding on an intervention for this subgroup.
In a previous study we reported that, when compared to another LBP subgroup, people in the RotExt subgroup displayed asymmetry of lumbar region movement during a clinical test of trunk lateral bending in standing.(Gombatto et al 2007a) The finding of asymmetry of movement pattern in people in the RotExt subgroup prompted us to examine the factors that may contribute to the asymmetrical movement pattern. Understanding the factors that potentially contribute to a movement pattern a person displays is important for understanding the mechanisms contributing to the LBP problem. Based on the data from the current study, asymmetry of passive elastic energy may be one factor that contributes to the asymmetry of movement pattern displayed by people in the RotExt subgroup.
To better understand the difference between groups in symmetry of passive elastic energy, we compared the “greater side” and the “lesser side” of passive elastic energy between the groups (Figure 4). On the side with greater passive elastic energy, though not statistically significant, the RotExt subgroup demonstrated more passive elastic energy than people without LBP (P=0.51, Figure 4). On the side with less passive elastic energy, though not statistically significant, the RotExt subgroup demonstrated less passive elastic energy than people without LBP (P=0.45, Figure 4). Therefore, the asymmetry of passive elastic energy in the RotExt subgroup appeared to be related to greater passive elastic energy on one side and less passive elastic energy on the other side compared to the group of people without LBP (Figure 4).
Prior studies
In previous studies, investigators have examined passive tissue characteristics of the lumbar region during physiological movements, but these studies have included only people without a history of LBP.(McGill et al 1994; Parkinson et al 2004; Scannell & McGill 2003) Investigators who have examined differences in end-range posterior-anterior lumbar intersegmental mobility have reported that people with LBP demonstrate greater mobility compared to people without LBP.(Kulig et al 2007) The current study examines group differences in lumbar region passive tissue characteristics during a physiological motion. The group differences reported in the current study were not with end-range lumbar region extensibility, but with asymmetry of passive characteristics during the trunk lateral bending motion.
People without low back pain
In our sample, the people without LBP did display a difference in passive elastic energy between sides. Our prior clinical and laboratory data suggest that people without LBP do demonstrate some degree of asymmetry in movement patterns during clinical and laboratory testing. In the current sample, however, people with LBP in the RotExt subgroup were significantly more asymmetrical with regard to passive elastic energy than people without LBP. The groups were the same with regard to all subject characteristics, the majority of individuals in both groups were right-handed, and an equal number of individuals participated in asymmetrical leisure-time sports activities. Nonetheless, people in the RotExt subgroup demonstrated significantly greater asymmetry of passive elastic energy than people without LBP. The direction of asymmetry also was such that the side of greater passive elastic energy displayed greater passive resistance and the side of less passive elastic energy displayed less passive resistance in the RotExt subgroup compared to people without LBP, suggesting an adaptation in passive tissue characteristics.
Implications for intervention and prognosis
Asymmetry of passive characteristics during trunk lateral bending may be an important factor to consider when deciding on an intervention strategy for people in the RotExt subgroup. Other investigators have identified subgroups of people with LBP based on their response to different interventions.(Fritz et al 2005) These prior studies suggest that people with LBP who are considered hypomobile are more likely to benefit from intervention including mobilization and manipulation than people who are hypermobile.(Flynn et al 2002; Fritz et al 2004) Conversely, people with LBP who are considered hypermobile are more likely to benefit from a lumbar stabilization program than those people who are hypomobile.(Hicks et al 2005) Based on data from the current study, the difference between a subgroup of people with LBP and people without LBP was not a function of overall hypomobility or hypermobility, but asymmetry of passive characteristics. Though the differences were not statistically significant, people in the RotExt subgroup demonstrated greater lumbar region passive elastic energy to one side during trunk lateral bending than people without LBP, and less passive elastic energy to the other side. The asymmetry in passive characteristics suggests that an intervention strategy that focuses on a combination of mobilization and stabilization may be more appropriate than an approach including either general mobilization or stabilization. Encouraging mobility in the direction that is stiffer and limiting mobility in the direction that is less stiff may specifically target the passive asymmetry identified in the RotExt subgroup. The goal of intervention that targets the asymmetry would be to decrease asymmetry of loading on the spine that may be a mechanism for development or persistence of the LBP problem. Information about the passive tissue characteristics of a specific subgroup of people with LBP compared to people without LBP may provide a basis for a mechanism-based approach to intervention.
Limitations
One limitation of the current study is the position used for passive testing. Because the prone position decreases the compression load on the lumbar region, the passive measures with the current study may not be the same as the passive resistance to movement with the lumbar region in standing.(Goodwin et al 1994) However, testing passive tissue characteristics of the lumbar region in vivo in a loaded position would probably be complicated by factors such as an increase in muscle activity in the loaded position. A second limitation is that passive characteristics were examined for the lumbar region as a whole. A passive measure of the entire lumbar region does not provide information about characteristics of individual lumbar region motion segments. Measuring passive tissue characteristics of the entire lumbar region, however, potentially gives more information about the resistance provided by the lumbar region during a physiological motion. A third limitation of the current study is that there were strict inclusion criteria for people with LBP. The findings from the study, therefore, may not be generalizable either to people with conditions that were excluded, people in an acute flare-up of a LBP problem,(Von Korff 1994) or a population of people with LBP who are referred to a physical therapy clinic.
Conclusion
During a passive trunk lateral bending movement, people in the RotExt subgroup demonstrated greater asymmetry of lumbar region passive elastic energy than people without LBP, but there were no differences between groups in symmetry of end-range lumbar region extensibility. Knowing about the passive tissue characteristics of a specific subgroup of people with LBP compared to people without LBP may provide the clinician with information about one factor that may be related to the LBP problem, and that may need to be addressed in intervention for people in the RotExt subgroup.
Acknowledgements
We would like to acknowledge the assistance of John Kreitler, Supervisor of the Washington University School of Medicine Machine Shop for his assistance in the design and construction of the passive movement device described in the manuscript. We also would like to acknowledge the assistance of David Collins, PhD, Jennifer Lam, DPT, and Kara Schipper, SPT for their assistance with data processing and Jewel Binkerd, SPT and Shannon Pike, SPT for their assistance with subject recruitment.
Funding sources
Our work was partially funded by the National Institute of Child Health and Human Development, Division of the National Center for Medical Rehabilitation Research, Grant # 1 K01HD-01226-05 and Grant # 5 T32 HD07434-10 and a scholarship from the Foundation for Physical Therapy, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors acknowledge that we do not have any financial or personal relationships with other people or organizations that could inappropriately influence the work described in the current manuscript.
Reference List
- Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- Beach TA, Parkinson RJ, Stothart JP, Callaghan JP. Effects of prolonged sitting on the passive flexion stiffness of the in vivo lumbar spine. Spine J. 2005;5(2):145–154. doi: 10.1016/j.spinee.2004.07.036. [DOI] [PubMed] [Google Scholar]
- Burton AK, Battie MC, Gibbons L, Videman T, Tillotson KM. Lumbar disc degeneration and sagittal flexibility. J Spinal Disord. 1996;9(5):418–424. [PubMed] [Google Scholar]
- Deyo RA, Andersson G, Bombardier C, Cherkin DC, Keller RB, Lee CK, Liang MH, Lipscomb B, Shekelle P, Spratt KF. Outcome measures for studying patients with low back pain. Spine. 1994;19(18 Suppl):2032S–2036S. doi: 10.1097/00007632-199409151-00003. [DOI] [PubMed] [Google Scholar]
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–381. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, Butler B, Garber M, Allison S. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81(2):776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Arch Phys Med Rehabil. 2005;86(9):1745–1752. doi: 10.1016/j.apmr.2005.03.028. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Whitman JM, Flynn TW, Wainner RS, Childs JD. Factors related to the inability of individuals with low back pain to improve with a spinal manipulation. Phys Ther. 2004;84(2):173–190. [PubMed] [Google Scholar]
- Gajdosik RL. Passive extensibility of skeletal muscle: Review of the literature with clinical implications. Clin Biomech. 2001;16(2):87–101. doi: 10.1016/s0268-0033(00)00061-9. [DOI] [PubMed] [Google Scholar]
- Gay RE, Ilharreborde B, Zhao K, Zhao C, An KN. Sagittal plane motion in the human lumbar spine: comparison of the in vitro quasistatic neutral zone and dynamic motion parameters. Clin.Biomech. 2006;21(9):914–919. doi: 10.1016/j.clinbiomech.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen LR. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Phys Ther. 2007a;87(4):441–454. doi: 10.2522/ptj.20050370. [DOI] [PubMed] [Google Scholar]
- Gombatto SP, Klaesner JW, Norton BJ, Minor SD, Van Dillen LR. Reliability and Validity of a System to Measure in Vivo Passive Stiffness and Extensibility of the Trunk in People With and Without Low Back Pain; 6th Interdisciplinary World Congress on Low Back & Pelvic Pain Diagnosis and Treatment, Conference Proceedings; 2007b. [Google Scholar]
- Goodwin RR, James KS, Daniels AU, Dunn HK. Distraction and compression loads enhance spine torsional stiffness. J Biomech. 1994;27(8):1049–1057. doi: 10.1016/0021-9290(94)90221-6. [DOI] [PubMed] [Google Scholar]
- Granata KP, Marras WS. An EMG-assisted model of trunk loading during free-dynamic lifting. J Biomech. 1995;28(11):1309–1317. doi: 10.1016/0021-9290(95)00003-z. [DOI] [PubMed] [Google Scholar]
- Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine. 1996;21(22):2640–2650. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11(1):46–56. [PubMed] [Google Scholar]
- Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80(9):1005–1012. doi: 10.1016/s0003-9993(99)90052-7. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- Keller TS, Colloca CJ, Fuhr AW. In vivo transient vibration assessment of the normal human thoracolumbar spine. J Manipulative Physiol Ther. 2000;23(8):521–530. doi: 10.1067/mmt.2000.109680. [DOI] [PubMed] [Google Scholar]
- Kingma I, van Dieen JH, de Looze M, Toussaint HM, Dolan P, Baten CT. Asymmetric low back loading in asymmetric lifting movements is not prevented by pelvic twist. J Biomech. 1998;31(6):527–534. doi: 10.1016/s0021-9290(98)00045-1. [DOI] [PubMed] [Google Scholar]
- Kulig K, Powers CM, Landel RF, Chen H, Fredericson M, Guillet M, Butts K. Segmental lumbar mobility in individuals with low back pain: in vivo assessment during manual and self-imposed motion using dynamic MRI. BMC Musculoskelet Disord. 2007;8:8–17. doi: 10.1186/1471-2474-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurutz M. In vivo age- and sex-related creep of human lumbar motion segments and discs in pure centric tension. J Biomech. 2006;39(7):1180–1190. doi: 10.1016/j.jbiomech.2005.03.021. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Sherman KJ. Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Med.Hypotheses. 2007;68(1):74–80. doi: 10.1016/j.mehy.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Lee M, Steven GP, Crosbie J, Higgs RJ. Variations in posteroanterior stiffness in the thoracolumbar spine: Preliminary observations and proposed mechanisms. Phys Ther. 1998;78(12):1277–1287. doi: 10.1093/ptj/78.12.1277. [DOI] [PubMed] [Google Scholar]
- Marras WS, Lavender SA, Leurgans SE, Fathallah FA, Ferguson SA, Allread WG, Rajulu SL. Biomechanical risk factors for occupationally related low back disorders. Ergonomics. 1995;38(2):377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- Marras WS, Mirka GA. A comprehensive evaluation of trunk response to asymmetric trunk motion. Spine. 1992;17(3):318–326. doi: 10.1097/00007632-199203000-00013. [DOI] [PubMed] [Google Scholar]
- McGill S, Seguin J, Bennett G. Passive stiffness of the lumbar torso in flexion, extension, lateral bending, and axial rotation. Effect of belt wearing and breath holding. Spine. 1994;19(6):696–704. doi: 10.1097/00007632-199403001-00009. [DOI] [PubMed] [Google Scholar]
- McGill SM. Electromyographic activity of the abdominal and low back musculature during the generation of isometric and dynamic axial trunk torque: Implications for lumbar mechanics. J Orthop Res. 1991;9(1):91–103. doi: 10.1002/jor.1100090112. [DOI] [PubMed] [Google Scholar]
- Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed "Physical Stress Theory" to guide physical therapist practice, education, and research. Phys Ther. 2002;82(4):383–403. [PubMed] [Google Scholar]
- Norton BJ, Sahrmann SA, Van Dillen LR. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthop Sports Phys Ther. 2004;34(9):524–534. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5(4):383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- Parkinson RJ, Beach TA, Callaghan JP. The time-varying response of the in vivo lumbar spine to dynamic repetitive flexion. Clin Biomech. 2004;19(4):330–336. doi: 10.1016/j.clinbiomech.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby, Inc.; 2002. [Google Scholar]
- Sbriccoli P, Yousuf K, Kupershtein I, Solomonow M, Zhou BH, Zhu MP, Lu Y. Static load repetition is a risk factor in the development of lumbar cumulative musculoskeletal disorder. Spine. 2004;29(23):2643–2653. doi: 10.1097/01.brs.0000146052.44581.5f. [DOI] [PubMed] [Google Scholar]
- Scannell JP, McGill SM. Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living. Phys Ther. 2003;83(10):907–917. [PubMed] [Google Scholar]
- Turner J, Sarvaiya-Shah S, Trudelle-Jackson E. Interrater reliability of the movement impairment classification for lumbar spine syndromes in patients with chronic low back pain. J. Orthop. Sports Phys. Ther. 2005;35(1):A67. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- Ueno K, Liu YK. A three-dimensional nonlinear finite element model of lumbar intervertebral joint in torsion. J.Biomech.Eng. 1987;109(3):200–209. doi: 10.1115/1.3138670. [DOI] [PubMed] [Google Scholar]
- van Dieen JH, Kingma I. Total trunk muscle force and spinal compression are lower in asymmetric moments as compared to pure extension moments. J Biomech. 1999;32(7):681–687. doi: 10.1016/s0021-9290(99)00044-5. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Phys Med Rehabil. 2007;88(3):351–360. doi: 10.1016/j.apmr.2006.12.021. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, Fleming D, McDonnell MK, Bloom NJ. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(8):402–413. doi: 10.2519/jospt.2001.31.8.402. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, Fleming DA, McDonnell MK, Woolsey NB. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78(9):979–988. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: A preliminary report. Arch Phys Med Rehabil. 2003a;84(3):313–322. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. Movement system impairment-based categories for low back pain: Stage 1 validation. J Orthop Sports Phys Ther. 2003b;33(3):126–142. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- Von Korff M. Studying the natural history of back pain. Spine. 1994;19(18 Suppl):2041S–2046S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- Winter DA. Biomechanics and Motor Control of Human Movement. 3rd edition. Hoboken: John Wiley & Sons, Inc.; 2005. [Google Scholar]
- Zhao F, Pollintine P, Hole BD, Dolan P, Adams MA. Discogenic origins of spinal instability. Spine. 2005;30(23):2621–2630. doi: 10.1097/01.brs.0000188203.71182.c0. [DOI] [PubMed] [Google Scholar]