Abstract
Background
Patient preference may influence intervention effects, but has not been extensively studied. Randomized controlled design (N=1075) assessed outcomes when women (60 years +) were given a choice of two formats of a program to enhance heart disease management.
Methods
Randomization to "no choice" or "choice" study arms. Further randomization of "no choice” to: 1) Group intervention program format, 2) Self-Directed program format, 3) Control Group. "Choice" arm selected their preferred program format. Baseline, four, twelve, and eighteen month follow-up data collected. Two analyses: health outcomes for choice compared to being randomized; and preference effect on treatment efficacy.
Results
Women who chose a format compared to being assigned a format had better psychosocial functioning at four months (p=0.02) and tended toward better physical functioning at twelve months (p=0.07). At eighteen months women who chose versus being assigned a format had more symptoms measured as: number (p=0.004), frequency (p=0.006) and bother (p=0.004). At four months women who preferred the Group format had better psychosocial functioning when assigned the Group format than when they were assigned the Self Directed format (p=0.03). At eighteen months women preferring a Group format had more symptoms: number (p=0.001), frequency (p=0.001), bother (p=0.001) when assigned the Group format than when assigned the Self Directed format.
Conclusions
Choice and preference for the Group format each enhanced psychosocial and physical functioning up to one year. Despite the preference for Group format, over the longer term (eighteen months) cardiac symptoms were fewer when assigned the Self-Directed format.
INTRODUCTION
Patient choice or preference for a particular treatment type has been examined in a few studies of drug therapy (see, e.g. [1]; [2]) and other clinical interventions (see, e.g., [3]; [4]). How patient preference influences outcome is not precisely understood, but the idea that it does affect results has been posited. A review article [5], for example, suggests that randomized controlled clinical trials of behavioral interventions generally involve a complex set of behaviors (e.g., day to day management of a chronic disease). Behavioral interventions can make differing demands on time, level of commitment and willingness to undertake new, sometimes challenging, tasks. Choosing the intervention most amenable to an individual situation may enhance motivation and, therefore, program efficacy. Further, often such interventions address psychological factors such as confidence to change behavior or the belief that taking an action will produce the desired outcome and various learning events attempt to elicit these responses [6]. The extent to which a patient prefers the pedagogical means by which this new learning is expected to occur may influence results [7]. An underlying assumption in the literature regarding choice is that people will do better in an intervention that meets their expectations.
This randomized clinical trial examined the effect on health outcomes of choice of format of a self management program, "Women take PRIDE" (WTP), designed for older women with heart disease [8]. Two versions of the WTP intervention were developed: 1) a Group format where participants met at an appointed time to learn management strategies collectively, and 2) a Self-Directed format where participants studied strategies individually at home on their own schedules. The hypothesis was women who chose and received their preferred intervention format would realize better health outcomes than those randomly assigned to a format or to a Control Group. Specifically, older women given a choice rather than being assigned a format would exhibit improved physical and psychosocial functioning and decreased frequency and severity of symptoms. Further, it was anticipated that improvements would be greater for women who chose the Group format, as these women may reap the additional benefit of social support from group members.
METHODS
Design and Study Population
All study procedures were approved by the University of Michigan Institutional Review Board (IRB) and the IRBs of participating hospitals. Potential subjects were identified through five hospital sites in southeastern Michigan and met the following inclusion criteria: female; 60 years of age or older; diagnosed cardiac condition; treated by daily heart medication; seen by a physician within the past year; and lived within one hour of the study site. The cardiac diagnosis was defined as any condition directly involving the heart (i.e., arrhythmia, angina, myocardial infarction, congestive heart failure, or valvular disease). Subjects were excluded if hypertension was the only diagnosis because it is often asymptomatic.
A small number of participants were excluded if the physician assessed they were unable to participate fully in the program due to other medical reasons, e.g., terminal illness or memory loss.
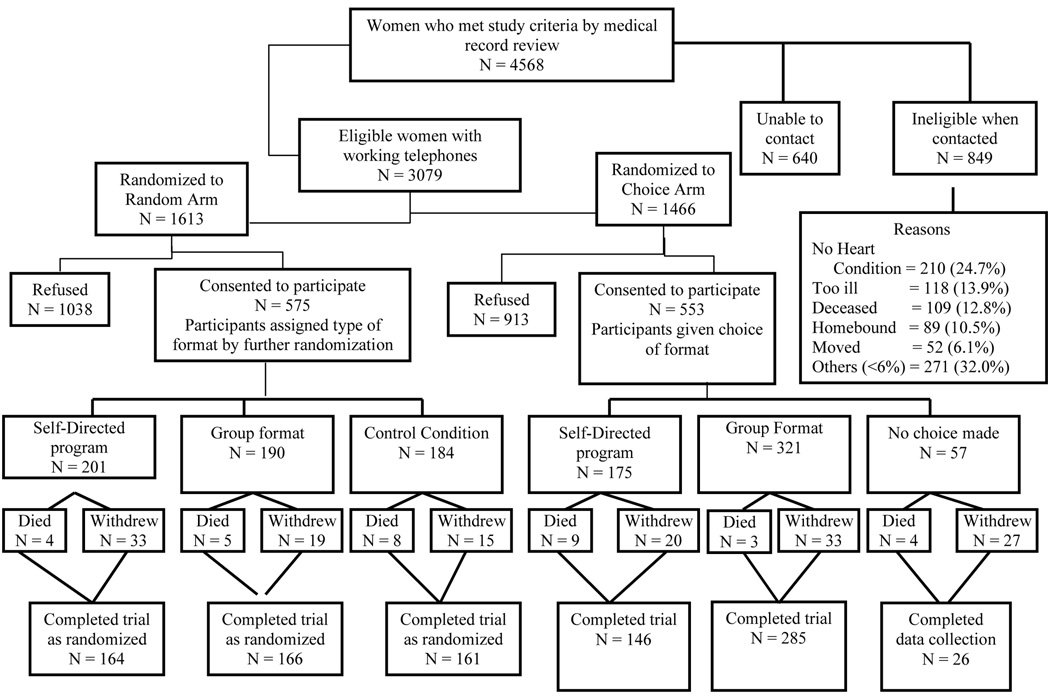
Figure 1 depicts the research design and describes subject participation. A two-step randomization scheme was employed [9]. Before initial contact, women meeting the eligibility criteria were randomly assigned to receive a recruitment script for either the No Choice or the Choice arms of the study. Using an allocation concealment protocol [10] and a random-numbers table to prepare sequentially numbered and sealed envelopes, the study coordinator randomized women meeting the study criteria to either the No Choice or Choice Arm. Potential subjects were randomized in a 55/45 No Choice arm versus Choice arm [11] ratio to account for potentially greater participation from women given a choice.
Figure 1.
Design of “Women Take PRIDE“ Study
In the second step, all potential subjects then received an introductory letter explaining the research and their physician’s participation, followed by a telephone contact scripted to their study arm. Complete study details were provided at this time.
Women agreeing to participate in the No Choice Arm were further randomized using the procedure described above and in equal numbers to one of three groups; the Group format WTP intervention, the Self-Directed format, or the "usual care" Control Group. Control women saw their physicians on their usual schedules and received any information provided as part of regular care. Women agreeing to participate in the Choice Arm were offered a choice of either the Group or Self-Directed formats of the program. Baseline data were collected before intervention assignment and choice. Study personnel, except the coordinator, were masked to program assignment. Unless a study participant happened to mention the study during the course of a routine visit, clinicians had no knowledge of which patients had agreed to participate in the research (Table 1).
Table 1.
Baseline Demographics and Health Characteristics
| Total Sample (n=1071) | Control (n=184) | Randomized to Intervention (n=391) | Randomized to Choice of Intervention (n=496) | p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age: mean (range) | 72.46(60,90) | 72.50(60,90) | 72.89(61,88) | 72.11(60,87) | 0.19 |
| Race (% white) | 83.82% | 82.97% | 82.78% | 84.96% | 0.64 |
| Education | |||||
| <HS % | 16.62% | 16.85% | 18.93% | 14.72% | |
| =HS % | 40.15% | 41.30% | 35.29% | 43.55% | 0.13 |
| >HS % | 43.23% | 41.85% | 45.78% | 41.73% | |
| Employed % | 11.67% | 12.50% | 10.23% | 12.50% | 0.54 |
| Income (%>20k) | 61.49% | 59.65% | 62.81% | 61.14% | 0.76 |
| Married % | 52.39% | 54.40% | 52.43% | 51.62% | 0.81 |
| Living Alone % | 35.16% | 34.81% | 33.59% | 36.51% | 0.66 |
| Heart Diagnoses | |||||
| Arrhythmia | 55.18% | 58.70% | 52.17% | 56.25% | 0.28 |
| Heart Attack | 40.60% | 45.65% | 39.85% | 39.31% | 0.30 |
| Angina | 36.67% | 39.67% | 36.57% | 35.63% | 0.62 |
| Valve problem | 27.01% | 25.00% | 26.09% | 28.48% | 0.58 |
| Congestive Heart Failure | 23.57% | 27.17% | 21.23% | 24.09% | 0.27 |
| Hypertension | 72.15% | 73.37% | 72.89% | 71.11% | 0.78 |
| Health Outcomes | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Functional Status | |||||
| SIP physical dimension score (0–100) | 9.31(10.13) | 10.71(11.12) | 8.82(9.84) | 9.18(9.95) | 0.10 |
| SIP psychosocial dimension score (0–100) | 7.43(10.32) | 7.92(10.36) | 7.20(9.78) | 7.44(10.72) | 0.74 |
| 6-minute walk (ft walked) | 749.60(460.20) | 735.64(450.55) | 766.61(469.80) | 741.77(457.03) | 0.72 |
| Cardiac Symptom Experience | |||||
| Cardiac symptom number (0–5) | 1.08(1.14) | 1.08(1.10) | 1.08(1.14) | 1.08(1.16) | 1.00 |
| Cardiac symptom frequency (0–25) | 3.15(3.74) | 3.15(3.58) | 3.10(3.50) | 3.19(3.97) | 0.94 |
| Cardiac symptom bother (0–25) | 3.44(4.28) | 3.51(4.21) | 3.41(4.32) | 3.44(4.28) | 0.96 |
Recruitment began in February 1998 and ended in February 2001. Of 3079 potential participants, 1613 were randomized to the No Choice arm of the study and of these 575 (35.6%) agreed to participate in the research. Of the 1466 potential subjects randomized to the Choice arm, 553 (37.7%) agreed to participate. The primary reasons for declining participation included format of the study (e.g. time commitment (34%), “not interested” (30 %), and health issues (16%)) with no significant differences between study arms. The overall participation rate of 36.6% is comparable with similar research involving older adults (See for example, [12]; [13]).
Intervention
The WTP intervention is based on social cognitive theory, particularly the principle of self-regulation [14]; [15]. The program introduces participants to a process for identifying and resolving problems encountered in following the heart regimen recommended by their health care provider. PRIDE is an acronym for the steps in this self-regulatory process and includes: problem selecting; researching one's daily routine; identifying a behavioral goal; developing a plan to reach one's goal, and evaluating one's progress. All participants learn the PRIDE steps and then apply them to the specific problem area they have identified. The theoretical underpinnings of the program are described elsewhere [16].
The materials and content of both formats of the program tested in this study were the same, with physical activity used as the model behavior through which women learned the PRIDE problem-solving process. The pedagogical approach was highly similar in both although the group format drew more on the concepts of dialogue and peer support, while the self-directed format relied more on self-study [17]; [18].
The Group format program included six to eight older women per program session who met for two hours per week at a hospital site and were facilitated by a health educator and a peer leader. Participants in the Self-directed format program attended an initial one-hour orientation at the hospital site, and thereafter worked on an individual basis at home over six weeks to complete the six program "units". Self-directed participants received encouragement and support as they completed the program through weekly telephone calls from the health educator or peer leader.
Data Collection and Measures
Data were collected at baseline four, twelve, and eighteen months followed-up by telephone interviews (averaging 57 minutes in length) and clinical assessments. Interviewers completed training to assure that standardized interviewing techniques and procedures were employed. Ongoing supervision and supplement training were provided. Research nurses followed a detailed written protocol to conduct the clinical measurements (Six-Minute Walk test) at participating hospitals.
Functional Health Status
(Primary outcome): The measures of functional health status were the Sickness Impact Profile (SIP) physical dimension score and SIP psychosocial dimension score.
The SIP is a comprehensive generic instrument that assesses functional health status. Its psychometric properties have been examined extensively [19]; [20]. The SIP contains 136 items and provides a total score and two dimension scores. The SIP physical dimension comprises the categories of ambulation, mobility, and body care and movement. The SIP psychosocial dimension includes the categories of social interaction, communication, emotional behavior, and alertness. Scores are derived by adding the values for the items with predetermined weights for each item within that category and dividing the sum by the maximum possible dysfunction score for that dimension. The scores range from 0–100, with higher scores representing greater dysfunction.
Cardiac Symptom Experience (Secondary Outcome)
Participants were asked about the presence, frequency, and bothersomeness of five cardiac symptoms routinely assessed by clinicians in history taking. The cardiac symptoms are a subset of the Symptom and Health Problem Profile used by the investigators in previous work, yielding a mean test-retest reliability score of 0.79 [21]. The five cardiac symptoms were: chest pain, shortness of breath, rapid or irregular heart beat, waking with chest pain, and waking with shortness of breath. Assessment was the presence of each symptom in the seven previous days. Frequency and bothersomeness were measured on a five-point Likert Scale. Totals were calculated by summing the responses for each of the five symptoms. Symptom frequency and bothersomeness scores ranged from 0–25, with higher scores indicating worse cardiac symptoms.
Ambulation (Tertiary Outcome)
Six-minute walk test: The six-minute walk test (Guyatt et al.1985) is an objective measure of functional status. Participants were asked to walk a premeasured course as far as they could, at their own pace, for a maximum of six minutes, and the distance in feet was recorded. Cahalin et al [22] found a significant correlation between the six-minute walk, peak V02 (r=0.64, p<0.001), and predicting short-term event-free survival in heart failure patients (p=0.04). In a Phase II/III cardiac rehabilitation population similar to that in the current study, Hamilton and Haennel [23] documented the validity and reliability of the six-minute test and found a moderate correlation with scores from the Duke Activity Status Index (r=0.502, p<0.001) and the Physical Function subscale of the SF-36 (r=0.624, p<0.001).
Statistical Analysis
Analyses were based on intention-to-treat and used SAS software, version 8.2 (SAS Institute, Inc.). The projected sample size of 1075 women (actual = 1128) enrolled in the study was based upon a statistical power of 80% (two sided alpha values of 0.05) to detect a three unit reduction in the SIP psychosocial dimensions mean score, allowing a 15% dropout rate for each condition. The findings reported here are based on a final sample (at 18 months follow up) of 330 intervention and 161 control participants in the No Choice arm and (310 vs. 431) intervention participants in the Choice arm.
Differences in rates of death or withdrawal from the study were not statistically significant between the two arms. Fifty-seven women did not make a choice when offered the opportunity. This subgroup when compared to women who made a choice were less likely to be married (p=0.04) or to have incomes greater than $20,000 per year (p=0.006) and to have more than a high school education (p=0.004). Data from these 57 women are not included in the outcomes analyses. No baseline differences were observed on demographics, diagnostic categories or functional status between the two study arms.
We report here results from three analyses: (A) comparisons of the outcomes at three time points, four, twelve and eighteen months post baseline, between those randomized to the choice group and those randomized to the Control Group (Table 2); (B) comparisons of the outcomes at the three time points of those randomized to the choice group and those randomized without choice to one of the intervention formats (Table 3); and (C) comparisons of the treatment effect (Group vs. Self-Directed) at four and eighteen months in the subpopulations of individuals preferring Group and preferring Self-Directed (Table 5). Analyses (A) and (B) concern the comparisons of three treatment schemes: 1) women choose their treatments (choice scheme); 2) women are randomized to either Group or Self-Directed program (randomization scheme); 3) women are randomized to usual care (control). In terms of improving health outcomes measures of interest, analysis (A) answers the question whether choice scheme is better than control, and analysis (B) answers the question whether the choice scheme is better than the randomization scheme. Analysis (C) concerns the effect of treatment preference, defined as the difference in treatment effects (Group vs. Self-Directed) in the subpopulation that prefers Group and the subpopulation that prefers Self-Directed. In other words, analysis (C) answers the question whether the format preference is an effect modifier in the comparison of treatment formats.
Table 2.
Comparison of Program Participants Given a Choice of Intervention Format and the Control Group (Total number of obs=2040).
| Data Collection Timepoints | |||
|---|---|---|---|
| Health Outcomes | 4-Months Treatment Effectsa (p-value) | 12-Months Treatment Effectsa (p-value) | 18-Months Treatment Effectsa (p-value) |
| Functional Status Scores | |||
| SIP physical dimension | −0.092 | −0.319 | −0.250 |
| (0.568) | (0.051)* | (0.124) | |
| N***=1705 | |||
| SIP psychosocial dimension | −0.346 | −0.124 | −0.208 |
| (0.066)** | (0.513) | (0.273) | |
| N=1705 | |||
| 6-minute walk | 7.87 | 25.55 | 8.29 |
| (0.809) | (0.433) | (0.802) | |
| N=1110 | |||
| Cardiac Symptoms | |||
| Cardiac symptom number | −0.138 | 0.078 | 0.034 |
| (0.342) | (0.594) | (0.817) | |
| N=1715 | |||
| Cardiac symptom frequency | −0.146 | 0.047 | 0.085 |
| (0.431) | (0.801) | (0.648) | |
| N=1703 | |||
| Cardiac symptom bother | −0.225 | 0.105 | 0.024 |
| (0.236) | (0.584) | (0.900) | |
| N=1710 | |||
Controlling for baseline value, age, race, education and employment; outcome on the log-transformed scale except for 6-min walk.
p≤0.05
p≤0.10
N: the number of subjects used in each analysis.
Table 3.
Comparison of Program Participants Given a Choice of Intervention Format and Participants Randomized to an Intervention Format (No Choice) (Total number of observations = 2661)
| Data Collection Timepoints | |||
|---|---|---|---|
| Health Outcomes | 4-Months Treatment Effect a (p-value) | 12-Months Treatment Effect a (p-value) | 18-Months Treatment Effect a (p-value) |
| Functional Status Scores | |||
| SIP physical dimension | 0.080 | −0.239 | −0.121 |
| (0.569) | (0.072) | (0.361) | |
| N***=2143 | |||
| SIP psychosocial dimension | −0.381 | −0.182 | 0.079 |
| (0.016)** | (0.230) | (0.600) | |
| N=2143 | |||
| 6-minute walk | −29.53 | −33.80 | −9.91 |
| (0.253) | (0.182) | (0.700) | |
| N=1403 | |||
| Cardiac Symptoms | |||
| Cardiac symptom number | 0.067 | 0.079 | 0.338 |
| (0.589) | (0.504) | (0.004)* | |
| N=2160 | |||
| Cardiac symptom frequency | 0.046 | 0.137 | 0.414 |
| (0.771) | (0.366) | (0.006)* | |
| N=2145 | |||
| Cardiac symptom bother | 0.015 | 0.075 | 0.434 |
| (0.925) | (0.626) | (0.004) * | |
| N=2154 | |||
Controlling for baseline value, age, employment, education and race; outcome on the log-transformed scale except for 6-min walk.
p≤0.01
p≤0.05
N: the number of subjects used in each analysis.
Table 5.
Estimated Treatment Effect (Group vs. Self-Directed) by Format Preference, Adjusting for Baseline Covariates
| Data Collection Timepoints | |||||||
|---|---|---|---|---|---|---|---|
| Format | 4-Month | 18-Month | |||||
| Health Outcomes | Preference | Intervention | Effect | P-value | Intervention | Effect | P-value |
| Functional Status Scores | |||||||
| SIP physical dimension | Prefer GP | 0.031 | 0.884 | −2.104 | 0.420 | ||
| Prefer SD | −2.338 | 0.479 | 2.123 | 0.757 | |||
| Difference In Treatment effect*** | −2.369 | 0.513 | −4.227 | 0.615 | |||
| N**** | 657 | 754 | |||||
| SIP psychosocial dimension | Prefer GP | −4.848 | 0.026* | −0.347 | 0.876 | ||
| Prefer SD | 3.928 | 0.384 | 0.253 | 0.936 | |||
| Difference In Treatment effect | −8.776 | 0.116 | −0.600 | 0.900 | |||
| N | 657 | 754 | |||||
| 6-minute walk | Prefer GP | −8.665 | 0.829 | 18.844 | 0.770 | ||
| Prefer SD | 21.06 | 0.775 | −4.55 | 0.926 | |||
| Difference In Treatment effect | −29.727 | 0.791 | 23.394 | 0.955 | |||
| N | 453 | 469 | |||||
| Cardiac symptoms | |||||||
| Cardiac symptom number | Prefer GP | 0.213 | 0.332 | 0.579 | <0.001** | ||
| Prefer SD | 0.100 | 0.933 | −0.312 | 0.362 | |||
| Difference In Treatment effect | 0.113 | 0.671 | 0.891 | 0.011 | |||
| N | 661 | 760 | |||||
| Cardiac symptom frequency | Prefer GP | 0.576 | 0.391 | 1.895 | <0.001** | ||
| Prefer SD | 0.592 | 0.844 | −1.119 | 0.335 | |||
| Difference In Treatment effect | −0.016 | 0.891 | 3.014 | 0.018 | |||
| N | 657 | 755 | |||||
| Cardiac symptom bother | Prefer GP | 0.485 | 0.657 | 2.135 | <0.001** | ||
| Prefer SD | 0.702 | 0.746 | −1.112 | 0.449 | |||
| Difference In Treatment effect | −0.217 | 0.896 | 3.247 | 0.034 | |||
| N | 659 | 758 | |||||
p≤0.05
p≤0.01
The difference in treat effect between two preference groups: treatment effect in Prefer G minus treatment effect in Prefer SD.
N: the number of subjects used in each analysis.
Analyses (A) and (B) were accomplished by fitting normal linear mixed models adjusting for baseline covariates, using SAS PROC MIXED in SAS software, version 8.2 (SAS Institute, Inc.). Where necessary, a log transformation was applied to the outcomes to make the normality assumption more plausible. This approach is appropriate for repeated measures data, and makes efficient use of all the available data at each time point, under the assumption that the missing data are missing at random [24].
The key idea underlying Analysis (C) is to stratify the target population into two subpopulations based on their format preference; those who prefer group format and those who prefer the self-directed program. Treatment effects are estimated for both preference subpopulations and the preference effect is estimated as the difference between the two treatment effects. For the WTP study, the subpopulations were identified in the choice arm, that is, each format group represented the subpopulation preferring that format, whereas format preference was not observed in the randomization arm and each randomized format group was a mixture of two subpopulations. This analysis requires novel methods, since the treatment preference is not observed for women in the randomization (no choice) arm of the study. The unique hybrid design of the study allows the estimation of these effects, under the assumption that the outcome for an individual under a preferred treatment is the same whether that treatment is randomly assigned or chosen by the participant – the so-called “exclusion restriction” in the causal effects literature. The approach requires two models relating the covariates to the health outcome of interest, functional status or cardiac symptom experience, and to the format choice. An EM algorithm [25] is used to compute maximum likelihood parameter estimates, standard errors and P-values of the estimates are computed using a bootstrap method. A detailed description of this statistical methodology is published elsewhere [26].
RESULTS
Demographics
Study women were on average 72 years of age and 84% reported their race as Caucasian. Approximately 40% reported at least a high school education, while an additional 43% reported education beyond high school. Twelve percent of the women were working at least part-time outside the home and 38% reported an annual family income of less than $20,000. Just over half were currently married and 35% lived alone. A variety of heart conditions had been diagnosed in study participants, including arrhythmia (55%), heart attack (41%), angina (37%), valve problems (27%), and congestive heart failure (24%). In addition, 72% reported hypertension.
Findings by Group Comparisons
(A) Women Given a Choice Versus Women in the Control Group
Table 2 shows differences in functioning measured by the SIP. Women randomized to the Choice Group had a marginally higher level of psychosocial functioning at four months (difference = 0.35, p=0.07) and significantly higher level of physical functioning at twelve months (difference = 0.32, p=0.05) than women randomized to the control group. Estimated differences at eighteen months favored the choice arm but were diminished and not statistically significant at the 5% level. No statistically significant differences were observed in the capacity of the women or in cardiac scores to walk distances (six minute walk) or in cardiac symptom scores.
(B) Women Given a Choice of Intervention Versus Those Assigned to a Format
Table 3 shows that at four months, women in the choice group had better psychosocial functioning (difference = 0.38, p=0.02) than those randomized to a format. No differences were observed at later time points. At twelve months women in the Choice Group exhibited a marginally higher level of SIP physical functioning (difference = 0.24, p=0.07) but this was no longer evident at eighteen months. At eighteen months women in the Choice Group had significantly worse symptom scores than women randomized to an intervention format [cardiac symptom number difference = 0.34, p=0.004, frequency difference = 0.41, p=0.006, and bother difference = 0.43, p=0.004)]. No statistically significant differences in ambulation were observed between groups.
(C) Preference Effects for Group and Self-Directed Formats
Table 4 shows the baseline differences between women preferring Group and preferring Self Directed formats. Employed women were more likely to choose the Self Directed format (p=0.043). No other comparisons were statistically significant. Those preferring the Self Directed format tended to have better symptom profiles but poorer functioning scores. Observations are consistent with previous findings [5].
Table 4.
Baseline demographics: comparison between preferring Group and preferring Self Directed format
| Variables | Preferring SD (n=175) | Preferring G (n=321) | P-Value |
|---|---|---|---|
| Age: | 72.23 | 72.04 | 0.75 |
| Race (% Caucasian) | 84.4 % | 85.3 % | 0.80 |
| Education | 0.30 | ||
| <HS % | 15.4 % | 14.3 % | |
| =HS % | 47.4 % | 41.4 % | |
| >HS % | 37.1 % | 44.2 % | |
| Employed % | 16.57 % | 10.28 % | 0.043* |
| Income (% >$20K) | 59.88 % | 61.82 % | 0.68 |
| Married % | 56.00 % | 49.22 % | 0.149 |
| Living Alone % | 33.53 % | 38.13 % | 0.311 |
| SIP physical score (0–100) | 10.02 | 8.72 | 0.64 |
| SIP psychosocial score (0–100) | 7.798 | 7.238 | 0.64 |
| 6-minute walk (ft walked) | 699.3 | 762.2 | 0.194 |
| Cardiac symptom number (0–5) | 0.965 | 1.140 | 0.097 |
| Cardiac symptom frequency (0–25) | 2.846 | 3.379 | 0.086 |
| Cardiac symptom bother (0–25) | 3.126 | 3.614 | 0.088 |
p≤0.05
Table 5 shows that at four months women who preferred the Group format (would chose the Group format if given the choice) had significantly better SIP psychosocial functioning when they received the Group format than when they were assigned to the Self-Directed format (difference = 4.85, p=0.03). There were trends in the direction of preference for other psychosocial SIP scores at different time points; however, they were not statistically significant.
Table 5 indicates that at eighteen months women who preferred the Group format had a significantly worse cardiac symptom number (difference = 0.58, p=0.001), frequency (difference = 1.90, p=0.001), and bother (difference = 2.13, p=0.001) when randomized to the Group format than when assigned to the Self-Directed format. Despite their preference for the Group format, their cardiac symptom scores were better when randomized to the Self-Directed format. This finding is somewhat counterbalanced by the fact that the death rate was higher in those who chose the Self-Directed format (9/175) than in those who chose the Group format (3/321) (See Figure 1). No between-group differences were noted for ambulation when Preference for Group and Self-Directed formats were assessed.
DISCUSSION
Allowing people to choose the type of health related intervention that most appeals to them is an attractive idea, and has been thought to improve adherence and outcomes [6]. Process data from the study, reported elsewhere [5], indicated that, after controlling for the effects of sociodemographic variables, participants who chose and got a group format were over four times more likely to attend at least one class and were almost twice as likely to have a higher level of attendance as the women randomized to the group format. Choice of format did not significantly affect completion of the six weekly units for the Self-Directed program participants, nor did it affect whether participants elected to withdraw from the study subsequent to baseline data collection. When the likelihood of completing key program activities (observation log and developing a plan) was examined, a trend for completion in the predicted direction was found but did not reach statistical significance. Choosing a format was associated with greater adherence to program activities compared to those randomized to a format. Regardless of the format or randomization they received, women liked the intervention. The mean score (out of a possible five) for finding the program's problem solving approach useful was 4.5 and for intending to use the approach with future problems was 4.4. When asked if they would participate again, knowing what they now know about the program, 93% said yes.
Our hypothesis was that an intervention would be more effective if women were allowed to choose and receive their preferred format for disease management education. Findings suggest that Choice produced better results related to the primary outcome, psychosocial and physical functioning. These effects were evident up to one year post baseline compared to No Choice or Control. Being given a choice, however produced worse cardiac symptom scores (secondary outcome) eighteen months post baseline.
Our hypothesis that outcomes would be better in the group format was only partially supported. Sixty-four percent of the women in this study given a choice of format preferred the Group intervention. These women also had short term functioning gains, but negative symptom outcomes by eighteen months. Being in the Group format produced results likely amenable to the influence of others including social support available from group membership. Symptom control, on the other hand, appeared to be better achieved in a self-directed format perhaps because of its individualized nature and the greater level of self-discipline required to complete it. These findings suggest that treatment effects may be more important than preference effects in particular subgroups. The reason for this observation may include intrinsic or external factors (e.g., a person's sense of control or external motivation effects). Further study of such potential explanations is warranted.
This research demonstrated that women do have a preference for the types of intervention a health care facility might offer. Choice enhanced some but not all outcomes of the intervention. Should choice be offered to patients, they may need to be counseled regarding the benefits and drawbacks of their choice in relationship to their disease management needs (e.g. symptom control versus psychosocial or physical functioning).
Choice may expand the reach of a health care facility to important patient populations. Women motivated to take part in an intervention of her choice could be encouraged, even provided with incentives, to take part in a component not chosen but shown to produce a desired result, e.g., a Self-Directed format for symptom control.
Our data also suggest that efforts to sustain initial gains over the longer term are needed. Booster instructional sessions may help to extend results over time, and/or strengthen outcomes appearing later.
Choice of intervention deserves further consideration within educational and behavioral studies [7]; [27]. Our findings support the idea that participants in a randomized clinical trial are likely to respond differently based on their preference for the intervention. A person's initial treatment preference may help to explain within or between group differences that emerge over time. Especially as the concept of treatment response variation takes hold in the medical and public health communities, the relationship of patient intervention preference to outcomes warrants closer investigation.
Study findings cannot be generalized to all older women with a heart condition as participants were not selected to be representative of any specific population. However they are likely to be similar to older female patients seeking service in like institutions.
CONCLUSION
Choice and participation in a Group format each enhanced psychosocial and physical functioning of older women with heart disease up to one year post intervention. Although women preferred a Group format, over the longer term of eighteen months, cardiac symptoms were fewer if they were assigned a Self Directed format.
Acknowledgement
This research was supported by Grant 5-R01-HL58611 from the Heart Division of the National Heart, Lung, and Blood Institute. We wish to acknowledge and thank our colleagues affiliated with the following medical centers for their assistance with this study: McLaren Regional Medical Center, Flint, Michigan; Genesys Regional Medical Center, Flint, Michigan; Henry Ford Health System, Detroit, Michigan; Providence Hospital and Medical Centers, Detroit, Michigan; and Ingham Regional Medical Center, Lansing, Michigan. [In addition we extend our thanks to Drs. Kim Eagle, Professor of Internal Medicine and Clinical Director of the University of Michigan Cardiovascular Center, and Claire Duvernoy, Assistant Professor of Internal Medicine – Cardiology University of Michigan Medical Center, for their contributions to this study.]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bakker A, Spinhoven P, van Balkom AJ, Vleugel L, van Dyck R. Cognitive therapy by allocation versus cognitive therapy by preference in the treatment of panic disorder. Psychother & Psychosom. 2000;69(5):240–243. doi: 10.1159/000012402. [DOI] [PubMed] [Google Scholar]
- 2.Schumacher GE. Randomized 2×2 trial evaluating hormonal treatment and the duration of chemotherapy in node-positive breast cancer patients. German Breast Cancer Study Group. 1994 doi: 10.1200/JCO.1994.12.10.2086. [DOI] [PubMed] [Google Scholar]
- 3.Cooper KG, Grant AM, Garratt AM. The impact of using a partially randomized patient preference design when evaluating alternative managements for heavy menstrual bleeding. Brit J Obstet Gynaec. 1997;104(2):1367–1373. doi: 10.1111/j.1471-0528.1997.tb11005.x. [DOI] [PubMed] [Google Scholar]
- 4.Rovers MM, Straatman H, Ingels K, van der Wilt GJ, van den Broek P, Zielhuis GA. Generalizability of trial results based on randomized versus nonrandomized allocation of OME infants to ventilation tubes or watchful waiting. J Clin Epid. 2001;54(8):789–794. doi: 10.1016/s0895-4356(01)00340-7. [DOI] [PubMed] [Google Scholar]
- 5.Janevic MR, Janz NK, Dodge JA, et al. The role of choice in health education intervention trials: a review and case study. Soc Sci Med. 2003;56:1581–1594. doi: 10.1016/s0277-9536(02)00158-2. [DOI] [PubMed] [Google Scholar]
- 6.McPherson K, Britton A. Preferences and understanding their effects on health. Int J Qual Health C. 2001;10 Suppl. I:i61–i66. doi: 10.1136/qhc.0100061... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King M, Nazareth I, Lampe F, et al. Impact of participant and physician intervention preferences on randomized trials: A systematic review. JAMA. 2005;293(9):1089–1099. doi: 10.1001/jama.293.9.1089. [DOI] [PubMed] [Google Scholar]
- 8.Dodge JA, Janz NK, Clark NM. The evolution of an innovative heart disease management program for older women: Integrating quantitative and qualitative methods in practice. Health Promot Pract. 2002;3(1):30–42. [Google Scholar]
- 9.Rucker G. A two-stage trial design for testing treatment, self-selection and treatment preference effects. Stat Med. 1989;8(4):477–485. doi: 10.1002/sim.4780080411. [DOI] [PubMed] [Google Scholar]
- 10.Pildal J, Chan AW, Hrobjartsson A, et al. Comparison of descriptions of allocation concealment in trial protocols and the published reports: cohort study. BMJ. 2005;330(7499):1049. doi: 10.1136/bmj.38414.422650.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dumville JC, Hahn S, Miles JNV, Togergson DJ. The use of unequal randomization ratios in clinical trials: A review. Contemp Clin Trials. 2006;27:1–12. doi: 10.1016/j.cct.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Sears SR, Stanton AL, Kwan L, et al. Recruitment and retention challenges in breast cancer survivorship research: Results from a multisite, randomized intervention trial in women with early stage breast cancer. Cancer Epid Biomar. 2003;12:1087–1090. [PubMed] [Google Scholar]
- 13.Heid HG, Schmelzer M. Influences on women's participation in cardiac rehabilitation. Rehabil Nurs. 2004;29(4):116–121. doi: 10.1002/j.2048-7940.2004.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 14.Bandura AA. Social Foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 15.Clark NM, Zimmerman BJ. A social cognitive view of self-regulated learning about health. Health Educ Res. 1990;5(3):371–379. doi: 10.1177/1090198114547512. [DOI] [PubMed] [Google Scholar]
- 16.Clark NM, Janz NK, Dodge JA, Sharpe PA. Self-regulation of health behavior: the "take PRIDE" program. Health Educ Quart. 1992;19(3):341–354. doi: 10.1177/109019819201900306. [DOI] [PubMed] [Google Scholar]
- 17.Barlow J. Self-management approaches for people with chronic conditions: a review. Patient Educ and Coun. 2002;48:177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 18.Wilson S. Individual versus group education: is one better? Patient Educ and Coun. 1997;(32):S67–S75. doi: 10.1016/s0738-3991(97)00098-0. [DOI] [PubMed] [Google Scholar]
- 19.Bergner M. Measurement of health status. Med Care. 1985;23(5):696–704. doi: 10.1097/00005650-198505000-00028. [DOI] [PubMed] [Google Scholar]
- 20.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Clark NM, Janz NK, Dodge JA, et al. Self-management of heart disease by older adults: Assessment of an intervention based on social cognitive theory. Res Aging. 1997;19(3):362–382. [Google Scholar]
- 22.Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110(2):325–332. doi: 10.1378/chest.110.2.325. [DOI] [PubMed] [Google Scholar]
- 23.Hamilton DM, Haennel RG. Validity and reliability of the 6-minute walk test in the cardiac rehabilitation population. J Cardiopulm Rehab. 2000;20:156–164. doi: 10.1097/00008483-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Little RJ, Rubin DB. Statistical analysis with missing data. 2nd ed. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- 25.Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm (with discussion) J. Roy. Statist. Soc. B. 1977;39:1–38. [Google Scholar]
- 26.Long Q, Little RJ, Lin X. Causal inference in hybrid intervention trials involving treatment choice. J. Am. Statist. Assoc. 2007 In press. [Google Scholar]
- 27.Johnson EJ, Steffel M, Goldstein DG. Making better decisions: From measuring to constructing preferences. Health Psychol. 2005;24 Suppl. 4:S17–S22. doi: 10.1037/0278-6133.24.4.S17. [DOI] [PubMed] [Google Scholar]