Abstract
Hoarding frequently occurs in obsessive-compulsive disorder (OCD), and some evidence suggests that it constitutes a distinct OCD subtype, with genetic contributions. This study investigated differences between OCD patients with and without hoarding symptoms. Of the 473 OCD patients studied, 24% were classified as hoarders according to combined interviewer and self –ratings, which were validated with the Savings Inventory-Revised in a subsample. Hoarders suffered from significantly more severe OCD symptoms, [especially compulsions] and had greater impairment and dysphoria. Hoarders also had more comorbid psychiatric disorders. Further study revealed that many of these differences were attributable to the female subjects: compared to female non-hoarders, female hoarders were more likely to suffer from bipolar I, substance abuse, panic disorder, binge-eating disorder, and had greater OCD severity. Male hoarders had an increased prevalence of social phobia compared to non-hoarding males. These results suggest that there are gender-specific differences in the hoarding sub-phenotype of OCD.
Hoarding, defined as the acquisition and retention of apparently useless possessions (Frost & Gross, 1993), is increasingly recognized as a substantial public health burden and a serious form of psychopathology that warrants further investigation. Extensive clutter, which often accompanies severe saving behaviors, is associated with marked disability in daily functioning and can lead to unsanitary conditions or fire hazards (Frost, Steketee, Williams, & Warren, 2000). Hoarding may thus result in significant costs not only to the individual, but also to the community (Frost, Steketee, & Williams, 2000). Although these extreme saving behaviors are sometimes seen in other disorders, including depression (Shafran & Tallis, 1996), anorexia (Frankenburg, 1984), schizophrenia (Luchins, Goldman, Lieb, & Hanrahan, 1992), and dementia (Hwang, Tsai, Yang, Liu, & Lirng, 1998), hoarding is most often associated with obsessive-compulsive disorder (OCD).
OCD, which is characterized by recurrent intrusive thoughts and ritualized actions, affects between 1% and 3% of the general population (Karno, Golding, Sorenson, & Burnam, 1988; Weismann et al., 1994, Kessler et al., 2005). Recent research has highlighted the heterogeneous nature of this disorder, and investigations are beginning to explore the range of symptoms that fall under the broader categories of obsessions and compulsions (Mataix-Cols, Rosario-Campos, & Leckman, 2005). Hoarding behaviors can be thought of as one type of OCD symptom, and there is evidence that suggests individuals who hoard make up a distinct subtype within the larger construct of OCD. Converging evidence for the distinctiveness of hoarding compared to other OCD symptoms has been garnered from neuroimaging (Saxena et al., 2004; Mataix-Cols et al., 2004), genetic (Zhang et al., 2002; Samuels et al., in press), and treatment studies (Saxena et al., 2002; Winsberg, Cassic, & Koran, 1999). Hoarding can also occur outside of OCD, with some individuals apparently having hoarding problems only, or having hoarding as a symptom of other medical or psychological disorders (Maier, 2004).
A growing number of clinical investigations has attempted to accurately characterize hoarding features in OCD, so as to evaluate further validation for this potential OCD subtype. Results across studies have revealed clinically significant differences between OCD patients with and without hoarding symptoms. Samuels et al. (2002) found an earlier age of OCD onset among hoarders, as well as increased prevalence rates of social phobia, personality disorders and pathological grooming behaviors. In a more recent study with a larger sample, Samuels and colleagues (2006) did not find an association between hoarding and earlier OCD onset, but did find that OCD hoarders had less insight and suffered from more severe OCD symptoms. That investigation revealed that hoarders had a greater prevalence of social phobia, generalized anxiety disorder and obsessive-compulsive and dependent personality disorders. Fontenelle, Mendlowicz, Soares and Versiani (2004) also reported that hoarding patients had an earlier age of onset. They furthermore found that hoarders had higher education, and more symmetry obsessions and ordering, repeating and counting compulsions. Lochner et al. (2005) reported significantly greater functional impairment and OCD symptom severity among OCD-hoarders as well increased rates of major depressive disorder, dysthymia, specific phobia and generalized anxiety disorder. Finally, Lasalle-Ricci et al. (2006) reported a positive correlation between hoarding scores and bipolar I, posttraumatic stress disorder (PTSD), and body dysmorphic disorder comorbidities. This investigation also used the NEO Personality inventory (Costa & McCrae, 1992) and found that hoarding was associated with higher scores on the Neuroticism personality factor and was negatively correlated with Conscientiousness.
Despite these advances in characterizing the hoarding factor within OCD, research on this phenomenon is still in its nascent stages and many unresolved questions remain. For example, no consensus exists for the prevalence of hoarding behaviors in OCD, with rates ranging from 18% to 42% (Hanna, 1995; Rasmussen & Eisen, 1992; Samuels et al., 2002). The large discrepancy between these prevalence rates may result from the lack of consensus regarding the best method for assessing hoarding behaviors. The most widely used scale to assess OCD symptoms is the Yale-Brown Obsessive Compulsive Scale – Symptom Checklist (Y-BOCS-SC), which contains 71 questions pertaining to a wide range of obsession and compulsions. While the Y-BOCS-SC is often viewed as the “golden standard” for assessing OCD symptoms in general, it contains only two questions that tap hoarding thoughts and behaviors (Goodman et al., 1989). The majority of the phenotypic investigations of OCD-hoarding has used these two questions to determine hoarding group-status (e.g., Frost, Steketee, Williams, & Warren 2000; Fontenelle, Mendlowicz, Soares, & Versiani, 2004; Lochner et al., 2005). Other investigations have relied on clinician ratings to determine the extent of hoarding (Samuels et al., 2002; Grisham et al., 2005). Despite the reliance on a reliable measure and qualified raters, both of these assessment approaches may not accurately capture hoarding status. The reliability of self-report measures may be compromised by the diminished insight hoarders often demonstrate with regard to their saving behaviors (Samuels et al., 2006). Similarly, interview data may be unreliable given that individuals may underreport their hoarding symptoms due to embarrassment. Thus, neither assessment approach, in and of itself, may accurately capture hoarding status.
A previous investigation by this group assessed the association between hoarding behavior and a number of clinical features in a sample of individuals with OCD (Lasalle-Ricci et al., 2006). The current report seeks to extend that phenotypic examination of the hoarding factor, and furthermore hopes to address a number of methodological limitations of past investigations. For this purpose, we utilized a multi-method approach to ascertain hoarding status. By combining self-report and interview based-methods, we aimed to more accurately divide our sample of individuals with OCD into those with serious hoarding problems and those who do not endorse major hoarding problems. Second, our sample is larger than that of many other studies used to assess phenotypic differences between hoarding and non-hoarding OCD patients. Specifically, we have more than doubled the original sample reported by Lasalle-Ricci and colleagues (2006), which provides a more adequate basis to assess a number of the mixed findings reviewed above.
We first compared hoarding and non-hoarding OCD patients on a number of features, including OCD age of onset, OCD symptom severity, depressive symptomatology, and global impairment of functioning. Second, we assessed differences between hoarding and non-hoarding individuals in psychiatric comorbidity. For these analyses we set a relatively conservative significance level of p<.01 to adjust for multiple testing. Finally, we investigated the relationship between hoarding and gender. Gender differences have only rarely been investigated in OCD hoarding samples, and preliminary findings have been inconclusive (Samuels et al., 2002; Fontenelle et al., 2004). To the best of our knowledge, no previous study has sought to explicitly evaluate gender-specific differences in the hoarding phenotype. We thus compared males and females on the phenotypic and comorbidity factors outlined above. Because of the exploratory nature of these analyses we set a less conservative value of p<.05.
Method
Participants
This study included 473 OCD patients from the Adult OCD Clinic at the National Institute of Mental Health who were participating in a separate genetic investigation. Participants were recruited though referrals, newspaper advertisements, information booths at OCD and other conferences, and the NIMH website, which specifically mentioned interest in hoarding behaviors in the general context of an OCD study. Inclusion criteria consisted of having a lifetime diagnosis of OCD and being at least 18 years of age. Exclusion criteria included active psychosis, severe mental retardation and OCD symptoms that occurred solely in the context of depression.
The sample consisted of 184 (38.9%) men and 289 (61.1%) women. Participants were quite well educated, with 64.0% reporting a college degree and 20.7% achieving a graduate degree. The sample was primarily Caucasian (88.4%), but included small groups of Hispanic (2.4%), Asian (2.2%), African American (2.4%), and other (4.6%) participants. This sample was more than double the size of our initial study of OCD hoarders (LaSalle-Ricci et al., 2006), and as that study used a different ascertainment strategy that cohort was included in the present study; in addition, partial data from 20 of the 473 individuals in the present study was included in another collaborative report recently published, which also used different assessments of hoarding (Samuels et al., 2006).
Measures
Structured Clinical Interview for DSM-IV-TR Axis I Disorders Patient Edition (SCID-P)
The SCID-P (First et al., 2001) was used to diagnose major DSM-IV Axis I disorders, including OCD. Interviews were conducted by clinically trained interviewers either on site or over the telephone. To ensure reliability, a blind diagnostic procedure was used in which two independent reviewers evaluated each diagnosis. The SCID-P has been found to be a highly reliable measure for most Axis I (Segal, Hersen, & Van Hasselt, 1994).
Yale-Brown Obsessive Compulsive Scale (Y-BOCS)
The Y-BOCS (Goodman et al., 1989b) is a 10-item assessment of obsessive-compulsive symptom severity. The Y-BOCS has been found to have high inter-rater reliability, internal consistency, and excellent concurrent validity with another measure of OCD severity (Goodman et al., 1989). The Y-BOCS also includes a symptom checklist (Y-BOCS-SC), which consists of 71 items assessing present and lifetime obsessions and compulsions. The Y-BOCS-SC is divided into 15 clinically determined categories of OCD symptoms, including hoarding obsessions and compulsions (Goodman et al., 1989a). The Y-BOCS-SC exists in both clinical interview and self report forms, which have been found to yield highly correlated results (Steketee, Frost, & Bogart, 1996). Only the self report form was used in this study.
Global Assessment of Function (GAF)
The GAF is one of the axes of the DSM-IV(American Psychiatric Association, 1994). It assesses general psychological, occupational, and social functioning on a 100 point scale and has been shown to be a valid and reliable measure of psychiatric health and disturbance (Jones, Thornicroft, Coffey, & Dunn, 1995; Piersma & Boes, 1997; Sohlberg 1989).
Beck Depression Inventory (BDI)
Dysphoria was assessed with the BDI (Beck et al., 1979), a 21-question measure of current mood on a 4 point scale. The BDI has been shown to have high concurrent validity and strong convergent validity (Beck, Steer, & Garbin, 1988).
Saving Inventory-Revised (SI-R)
The SI-R is a 23-item questionnaire designed to measure hoarding-related behaviors, including difficulty discarding, acquisition, and clutter (Frost, Steketee, & Greene, 2003). It has been found to be a valid measure of hoarding behaviors in both clinical and non-clinical populations (Coles, Frost, Heimberg, & Steketee, 2003; Frost, Steketee, & Grisham, 2004). The SI-R has been found to have good test-retest reliability and strong internal consistency (Frost, Steketee, & Grisham, 2004).
Hoarding Classification
This study used a strict definition of hoarding that combined both the Y-BOCS-SC hoarding items and a clinician-based rating of hoarding. Patients who endorsed both of the Y-BOCS-SC hoarding questions and endorsed significant hoarding symptoms during the clinical interview were classified as hoarders. Patients who did not report hoarding on the Y-BOCS-SC or who did not mention hoarding symptoms during the clinical interview were placed in the non-hoarding group. For a minority (131 of 473) of cases the Y-BOCS-SC was unavailable, so the Thoughts and Behaviors Inventory (TBI), an updated and modified version of the Y-BOCS-SC, with high concurrent validity, was used as a substitute (Slattery et al., 2004; Hasler et al., 2005).
Results
Using our composite criteria, 115 (24.3 %) of the 473 participants with OCD in the sample were classified as hoarders. To evaluate the validity of this classification method we used an independent, well-validated, hoarding-specific rating scale to compare OCD patients with and without composite criteria-defined hoarding. Saving Inventory-Revised (SI-R) ratings were from the most-recently recruited sub-set of the larger sample (N = 322 / 473). Results confirmed that the hoarding group scored markedly higher (M = 48.4, SD = 16.8) on the SI-R than the non-hoarding group (M = 19.6, SD = 16.3; t = −13.78, p < .001). Of note, the mean SI-R score for our hoarding group was similar to that reported by Frost, Steketee and Grisham (2004) for individuals with OCD who hoard. Similarly, our non-hoarding OCD patients scored similarly to non-hoarding OCD subjects and non-hoarding non-OCD controls in that study. This confirms that our composite hoarding classification method was valid.
Analysis of demographic variables revealed that the female to male ratio was similar for both the hoarding and non-hoarding groups (64 of 289 (22.1%) females were hoarders, compared to 51 of 184 (27.7%) males). Furthermore, no significant differences were found for age, race, or education [Table 1]. When income was measured on a six category scale, in increasing increments of $15,000, the hoarding group’s average score on this socioeconomic scale was significantly lower than the non-hoarders (F = 14.18, p < .01). More detailed analysis revealed that hoarders were more likely to fall in the lowest income bracket (F = 6.64, p < .01) and were less likely to be in the highest bracket at a trend level (F = 4.59, p < .05) [Table 1]. Although the hoarding and non-hoarding groups did not differ in age, there was a trend level association in which the hoarding group was less likely to be currently married than the non-hoarding group (F = 4.44, p < .05)
Table 1.
Demographic data in OCD patients with and without hoarding.
| Variable | Hoarding
(N = 115, 24%) |
SD | Non-Hoarding
(N = 358, 76%) |
SD | Statistic |
|---|---|---|---|---|---|
| 1. Sex (% female) | 63% | 56% | χ2 = 1.90 | ||
| 2. Age | 38.62 | 13.01 | 39.23 | 13.53 | t = .42 |
| 3. College degree | 63.39% | 64.14% | χ2 = .02 | ||
| 4. Married | 32.14% | 43.39% | χ2 = 4.44 † | ||
| 5. Income bracket | % within | % within | χ2 = 14.18 * | ||
| less than $15,000 | 33.8% | 20.2% | |||
| $15,000–30,000 | 23.0% | 14.6% | |||
| $30,000–45,000 | 10.8% | 15.4% | |||
| $45,000–60,000 | 13.5% | 11.7% | |||
| $60,000–75,000 | 5.4% | 13.0% | |||
| more than $75,000 | 13.5% | 25.1% |
p < .05 (Trend)
p < 0.01
Note. 1. Sex = percentage of sample that was female; 2. Age = mean age at time of study; 3. College degree = percentage of sample that received at least a bachelor’s degree; 4. Married = percentage of sample currently married at the time of the study; 5. Income = percentage of sample with household income in each category.
SD = standard deviation where applicable; ns = nonsignificant
OCD Features, Impairment and Depressive Symptomatology
Results are summarized in Table 2. Compared to non-hoarders, the hoarding group reported greater OCD symptom severity as assessed by the Y-BOCS total score (t = −2.52, p < .01). We furthermore found that the hoarding group reported significantly greater Y-BOCS compulsion scores (t = −3.23, p < .001), but did not differ significantly from non-hoarders in terms of obsession severity. Members of the hoarding group endorsed more symptoms on the Y-BOCS-SC than non-hoarders, indicating that they experienced a greater total number of various other OCD symptoms in addition to hoarding (t = −4.7, p < .001). In terms of the different Y-BOCS-SC symptom categories, members of the hoarding group exhibited significantly more contamination, sexual, religious, symmetry, and somatic obsessions but not aggressive obsessions and more ordering compulsions. No significant difference was found between hoarders and non-hoarders with respect to OCD age of onset. The hoarding group scored significantly higher on the BDI (t = −4.41, p < .001), indicating greater levels of depressive symptoms. Finally, with regard to global impairment of functioning, hoarders had lower scores on the GAF (t = 4.39, p < .001), indicating greater levels of impairment and disability. In order to ensure that the reduced GAF scores were not a direct result of increased depressive symptoms we conducted a one-way between-groups analysis of covariance comparing hoarders and non-hoarders on their global functioning, while simultaneously taking into account depressive symptoms and gender. The independent variable was hoarding group status and the dependent variable was GAF score. Participants’ scores on the BDI were entered as covariates. After adjusting for BDI scores, we found that hoarders (adjusted mean = 62.5, standard error = 1.57) were still significantly different from non-hoarders (adjusted mean = 66.6, standard error = .85) on GAF levels F(1,284)=5.25, p=.02, eta squared=.018.
Table 2.
Clinical data in OCD patients with and without hoarding.
| Variable | Hoarding
(N = 115) |
SD | Non-Hoarding
(N = 358) |
SD | Statistic |
|---|---|---|---|---|---|
| 1. Age-of-onset | 12.52 | 8.66 | 14.17 | 9.13 | t = 1.71 |
| 2. Y-BOCS | 23.95 | 7.27 | 21.73 | 8.39 | t = −2.52* |
| 3. Y-BOCS obsessions | 11.88 | 4.68 | 11.24 | 4.75 | t = −1.27 |
| 4. Y-BOCS compulsions | 12.06 | 3.69 | 10.49 | 4.74 | t = −3.23** |
| 5. Y-BOCS-SC total | 30.15 | 17.54 | 18.12 | 13.89 | t = −4.70** |
| 6. Obsessions | |||||
| Aggressive | 89.53% | 85.19% | χ2 = 1.02 | ||
| Contamination | 92.05% | 79.17% | χ2 = 7.44* | ||
| Sexual | 66.29% | 51.81% | χ2 = 5.57† | ||
| Religious | 76.09% | 60.16% | χ2 = 7.42* | ||
| Symmetry | 84.62% | 70.16% | χ2 = 7.24* | ||
| Somatic | 93.33% | 80.48% | χ2 = 8.09* | ||
| 7. Compulsions | |||||
| Cleaning | 78.26% | 70.31% | χ2 = 2.14 | ||
| Checking | 91.11% | 84.84% | χ2 = 2.22 | ||
| Repeating | 89.25% | 85.20% | χ2 = 0.94 | ||
| Counting | 62.77% | 55.95% | χ2 = 1.30 | ||
| Ordering | 75.53% | 57.94% | χ2 = 9.07* | ||
| 8. BDI | 21.02 | 13.19 | 14.81 | 11.34 | t = −4.41** |
| 9. GAF | 58.83 | 15.38 | 67.23 | 14.92 | t = 4.39** |
p < .05 (Trend)
p <.01
p <.001
Note. 1. Age-of-onset = mean age at onset of OCD symptoms; 2. Y-BOCS = Yale-Brown Obsessive-Compulsive Scale total score; 3. Y-BOCS obsessions = total obsession severity; 4. Y-BOCS compulsions = total compulsions severity; 5. Y-BOCS-SC total = total number of symptoms reported on the symptom checklist; 6. Obsessions = Y-BOCS-SC obsession categories; 7. Compulsions = Y-BOCS-SC compulsion categories; 8. BDI = Beck Depression Inventory; 9. GAF = Global Assessment of Function.
SD = standard deviation where applicable; ns = nonsignificant.
Comorbidity
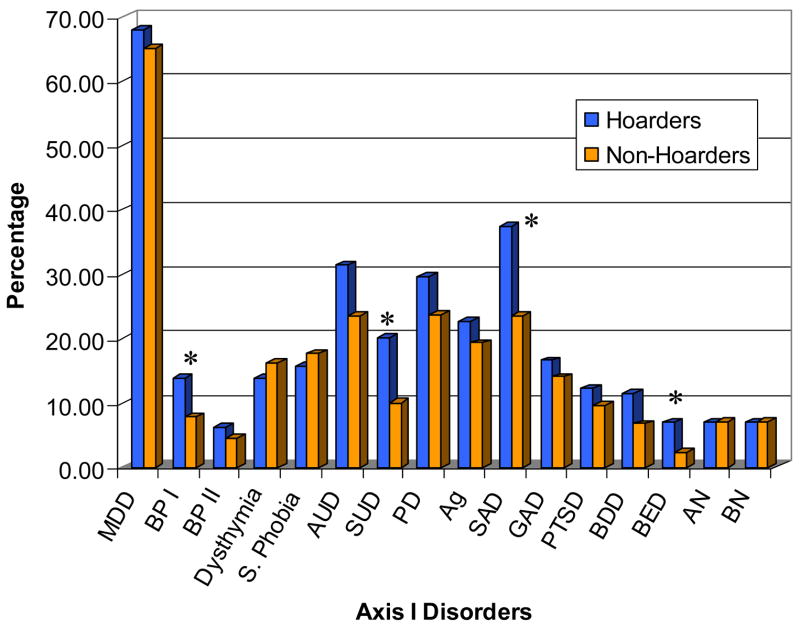
Our second aim was to compare hoarders and non-hoarders’ lifetime prevalence rates of a range of Axis I disorders that may be comorbid to the primary diagnosis of OCD. In general, comorbid psychiatric disorders were common in our sample, with 92% of participants having at least one additional diagnosis during their lifetime (M = 2.71; SD = 1.89). On average, patients in the hoarding group had significantly more additional disorders than the non-hoarding group (t = −2.8, p < .01). Results from chi-square tests comparing hoarders and non-hoarder on each specific disorder are presented in Figure 1. Compared to non-hoarders, the rates of comorbid social anxiety disorder (F = 8.6, p < .01) and substance use disorders (F = 7.89, p < .01) were significantly higher in the hoarding group. There was also a trend for hoarders to have a greater prevalence of bipolar I disorder (F = 3.83, p < .05).
Figure 1.
Lifetime comorbidity in OCD patients with and without hoarding symptoms.
Note on Figure 1. MDD = Major Depressive Disorder; BP I = Bipolar I Disorder; BP II = Bipolar II Disorder; S. Phobia = Simple Phobia; AUD = Alcohol Use Disorders; SUD = Substance Use Disorders; PD = Panic Disorder; Ag = Agoraphobia; SAD = Social Anxiety Disorder; GAD = Generalized Anxiety Disorder; PTSD = Posttraumatic Stress Disorder; BDD = Body Dysmorphic Disorder; BED = Binge Eating Disorder; AN = Anorexia Nervosa; BN = Bulimia Nervosa
*p < 0.05
An additional component of our second aim was to conduct a more comprehensive assessment of the association between hoarding and eating disorder psychopathology. A trend in the data indicated that hoarding was associated with a more than two-fold higher rate of binge-eating disorder (F = 5.94, p < .05). No association was found between hoarding and the other eating disorders, anorexia nervosa and bulimia nervosa.
Gender Analysis
To further elucidate the relationship between hoarding and gender we conducted the above analyses for females and males separately. Compared to female non-hoarders, female hoarders had significantly greater total Y-BOCS severity scores (t = −2.87, p < .01), and higher rates of bipolar I (F = 5.28, p < .02), binge eating disorder (F = 7.93, p < .01), and substance abuse disorders (F = 12.03, p < .001). Restricting analyses to the female portion of our sample also revealed several significant results that were not observed for the sample as a whole. As shown in Table 3, female hoarders had an earlier age of OCD onset (t = 2.06, p < .04), and greater prevalence of panic disorder (F = 5.69, p < .01) and alcohol abuse disorders (F = 4.64, p < .03). Male hoarders did not differ from male non-hoarders on any of these variables, though we did find significantly greater rates of comorbid social phobia in male hoarders compared to male non-hoarders (F = 9.84, p < .01). In addition, male hoarders reported significantly more symmetry obsessions than male non-hoarders (F = 7.08, p < .01), but no differences were found for any of the other Y-BOCS SC symptom categories. Female hoarders reported greater repeating compulsions than female non-hoarders (F = 5.38, p < .01), as well as increased rates of contamination, sexual, religious, symmetry, and somatic obsessions and ordering compulsions.
Table 3.
Data from Gender- Segregated Analysis.
| Female Participants | Male Participants | |||||
|---|---|---|---|---|---|---|
| Variable | Hoarding
(N = 64) |
Non-Hoarding
(N = 225) |
Statistic | Hoarding
(N = 51) |
Non-Hoarding
(N = 133) |
Statistic |
| 1. Age-of-onset (SD) | 11.32 (7.92) | 14.07 (9.74) | t = 2.06* | 14.0 (9.37) | 14.35 (8.04) | t = 0.25 |
| 2. Y-BOCS (SD) | 24.95 (7.20) | 21.73 (8.03) | t = −2.87** | 22.68 (7.22) | 21.73 (9.0) | t = −0.67 |
| 3. Bipolar I | 17.19 % | 7.56 % | χ2 = 5.28* | 9.80 % | 8.27 % | χ2 = 0.12 |
| 4. Alcohol Abuse Disorders | 32.81 % | 25.33 % | χ2 = 4.64* | 29.41 % | 29.32 % | χ2 = 0.10 |
| 5. Substance Abuse Disorders | 26.56 % | 9.78 % | χ2 = 12.03*** | 11.76 % | 10.53 % | χ2 = 0.10 |
| 6. Panic Disorder | 40.63 % | 20.00 % | χ2 = 5.69** | 15.69 % | 21.05 % | χ2 = 0.68 |
| 7. Social Phobia | 32.81 % | 25.33 % | χ2 = 1.41 | 43.14 % | 20.30 % | χ2 = 9.84* |
| 8. Binge-Eating Disorder | 10.94 % | 2.67 % | χ2 = 7.93** | 2.00 % | 1.50 % | χ2 = 0.10 |
p < .05
p <.01
p <.001
Note. 1. Age-of-onset = mean age at onset of OCD symptoms; 2. Y-BOCS = Yale-Brown Obsessive-Compulsive Scale total score; 3. Bipolar I = percentage of subjects diagnosed with Bipolar I; 4. Alcohol Abuse = percentage of subjects diagnosed with alcohol use disorders; 5. Substance Abuse = percentage of subjects diagnosed with substance use disorders; 6. Panic Disorder = percentage of subjects diagnosed with panic disorder; 7. Social Phobia = percentage of subjects diagnosed with social phobia; 8. Binge Eating Disorder = percentage of subjects diagnosed with binge eating disorder.
SD = standard deviation where applicable; ns = nonsignificant.
Discussion
This study’s large sample size has enabled us to shed further light on conflicting findings about hoarding behaviors and also to replicate and validate some of the analyses of earlier reports. Unlike two previous investigations (Fontenelle, Mendlowicz, Soares, & Versiani, 2004; Samuels et al. 2002) we did not find an association between hoarding and an earlier age of OCD onset for our sample as a whole. That being said, female hoarders in our sample did have a younger age of onset compared to female non-hoarders, a finding of interest as individuals with an earlier age of OCD onset tend to have more severe OCD symptomatology and more familial OCD (Fontenelle, Mendlowicz, Marques, & Versiani, 2003; Chabane, et al., 2005) . We did not find that hoarders were older than non-hoarders as had been reported in some studies (Frost, Steketee, Williams & Warren, 2000; Saxena et al., 2002). Our trend-level finding that hoarders were less likely to be married at the time of the study fits in with the findings of Samuels et al. (2002). This may relate to hoarders’ increased rate of social phobia, or to their greater global impairment. Additionally, the accumulated clutter associated with hoarding itself might discourage some relationships. We found that hoarders had higher total scores on the Y-BOCS and therefore suffered from greater OCD symptom severity, in agreement with Lochner et al. (2005), though this effect was primarily driven by the females in the sample. Further analysis showed that hoarders only scored significantly higher on the compulsions portion of the scale and did not differ from non-hoarders in their obsessions severity. This is an interesting finding that may relate to the nature of hoarding symptoms. However, it could also be related to the fact that hoarders endorsed more total OCD symptoms in general. One of the shortcomings of the Y-BOCS is that it does not specifically asses the severity of each OCD symptom group. The recently developed DY-BOCS (Rosario-Campos et al., 2006) individually assesses the severity of each OCD symptom category and could help clarify this issue in future studies.
Our finding that hoarders endorsed more ordering compulsions and contamination, sexual, religious, symmetry, and somatic obsessions differs from Samuels et al.’s (2002) finding of greater symmetry obsessions and counting and ordering compulsions. These differences may in part derive from our use of the self report Y-BOCS-SC, as patients have been found to report more symptoms on the self report form than on the interview based form (Steketee, Frost & Bogart, 1996).
We also found that hoarders suffered from a greater degree of global impairment than non-hoarders. The ANCOVA analysis controlling for BDI scores revealed that this increased impairment was not solely the result of increased depressive symptoms. This finding is in line with the investigation by Lochner and colleagues (2005), as well as with a number of reports by Frost, Steketee, and colleagues (e.g., Frost, Steketee, Williams & Warren, 2000) that have found marked impairment in functioning in hoarding samples. This greater global impairment may stem from the phenotypic differences between hoarders and non-hoarders, including greater comorbidity, greater OCD symptom severity, and greater depressive symptoms. Impairment also may arise from the nature of hoarding behaviors per se. That is, the clutter associated with hoarding can be debilitating and the acquisitioning of items can consume much of an individual’s time--and sometimes even their financial resources (Frost, Steketee, & Williams, 2000). Our finding that hoarders had significantly greater scores on the BDI without having higher rates of major depressive disorder or dysthymia is intriguing and may warrant future investigation. Of note, our finding is not in agreement with other data (Wu & Watson, 2005), which reports that hoarding is less strongly related to negative affectivity than other OCD symptoms (e.g., checking). However, that study did not exclusively use an OCD sample. Rather, only 54 of the 160 psychiatric patients studied had an OCD diagnosis (Wu & Watson, 2005). Therefore it is possible that hoarding in the absence of OCD may be associated with fewer negative effects. Indeed, Grisham and colleagues found that hoarders without OCD reported less anxiety, stress and negative affectivity compared to patients with OCD and with OCD and hoarding (2005).
The results of the current study support the general finding that hoarders suffer from more comorbid psychiatric disorders. Our findings of increased prevalence rates of social phobia, substance abuse and a trend towards bipolar I among hoarders are consistent with previously reported findings (Samuels et al., 2002; LaSalle-Ricci et al., 2006). Our study sought to use a more fine-grained approach to investigate the relationship between hoarding and the individual eating disorders. Several previous studies (e.g., Samuels et al., 2002; Fontenelle et al., 2004; Lochner et al., 2005) combined a number of diverse eating disorders (e.g., anorexia nervosa and binge-eating disorder) into one general category. Our finding of a trend in which binge-eating disorder was more prevalent in hoarders is meaningful because it supports LaSalle Ricci and colleagues’ (2006) previously reported association and is in line with the findings of Fontenelle et al. (2004) of a relationship between hoarding and a combined eating disorders rating that included bulimia nervosa and binge-eating disorder. Follow-up analyses revealed that many of these comorbidity relationships were gender specific. These differences may arise from baseline differences in the disorder prevalence rates between genders. For example, panic disorder is more common in females (Pigott 2003). Social phobia, which is generally more common in women (Pigott 2003), has been found to be more common in male OCD patients than in female OCD patients (Tukel et al., 2004). That being said, prevalence rates most likely only partially account for our finding and further research is needed on gender and hoarding.
Our study included some participants whose data contributed to an earlier report by our group (LaSalle-Ricci et al., 2006). The current study has, however, more than doubled the sample size of the previous investigation, increasing it from 204 to 473. In further contrast to the study conducted by LaSalle-Ricci et al., our investigation used a newly-developed dichotomous grouping methodology to compare hoarders and non-hoarders based on a combination of interviewer assessments and self-ratings. This hoarding evaluation method was validated by comparison with an independent 23-item hoarding scale, the Saving Inventory-Revised (Frost, Steketee, & Green, 2003). Given these methodological differences, a considerable number of our findings differ from those of the previous study. For example, while LaSalle-Ricci et al. found no relationship between social phobia and hoarding, the present study found a significant increase in social phobia among hoarders. Also, whereas the previous investigation documented a relationship between hoarding and PTSD and body dysmorphic disorder, we found no significant associations between them.
One of the main findings from this study was that individuals with OCD and hoarding behaviors tended to be more impaired than their non-hoarding counterparts in terms of greater OCD symptom severity, lower global functioning ratings, and more comorbid disorders. These combined factors suggest a possible explanation for why hoarders may have poorer responses to treatments across modalities. For example, hoarders have been found to be less responsive to both cognitive behavioral (Saxena et al., 2002) and psychopharmacologic treatments (Winsberg, Cassic, & Koran, 1999), though a recent study found hoarders responded equally well to paroxetine treatment (Saxena, Brody, Maidment, & Baxter, 2006). If treatment programs are indeed less efficacious for hoarders, the increased incidence of alcohol and substance abuse in some hoarders may represent a form of self-medicating. Clinicians should assess comorbid disorders and make appropriate considerations regarding these disorders when designing treatment plans for hoarders.
Gender seems to play an important role in the phenotypic presentation of OCD patients with hoarding symptoms. The results indicate that the hoarding phenotype may differ across gender, with females hoarders experiencing more severe OCD symptoms, earlier age of OCD onset and a broader range of psychiatric comorbidity, such as bipolar I disorder, panic disorder, binge-eating disorder, alcohol abuse and substance abuse.
One of the limitations of this study was the recruitment method. Although some of our advertisements did specifically mention our interest in hoarding and collecting problems, our recruitment materials were primarily aimed at individuals who met full OCD diagnostic criteria. Individuals who had hoarding as an isolated problem are likely underrepresented in our sample. Grisham and colleagues have suggested that compulsive hoarding may be a clinically distinct syndrome in the absence of OCD (2005), something our study cannot address. All members of our OCD-hoarding group reported other OCD symptoms and on average they endorsed 30 of the 71 Y-BOCS symptoms. This was significantly greater than the number of OCD symptoms reported by the non-hoarding group, which further supports an association between hoarding and a more severe form of OCD. Further evaluation of these analyses in a non-OCD hoarding sample would be valuable to see if these results are true for hoarding in general or specific to hoarding in the context of OCD.
Our findings suggest that OCD patients with hoarding symptoms are clinically distinct from OCD non-hoarders. This general conclusion supports recent investigations seeking to evaluate specific genetic correlates of hoarding behaviors. Hoarding has been investigated as a specific phenotype in two genome-wide scans, one in individuals with Tourette’s syndrome (Zhang et al., 2002) and one in OCD patients (Samuels et al., in press). Both studies found evidence of suggestive linkage, with chromosomal regions on 3, 4, 5, 14 and 17 identified. The peak region in the OCD sample that was different in hoarders compared to non-hoarding OCD subjects emerged only when hoarding was considered separately, and represented a peak not identified in the initial scan based on OCD diagnosis alone (Shugart et al. 2006; Samuels et al., in press). Clarification of the definition of the hoarding phenotype in this and other studies should benefit future genotype-phenotype investigations. It is noteworthy that a large number of our findings were driven by the females in our sample. Further research into gender-related associations of hoarding will be important in both phenotypic genetic, and clinical investigations.
Acknowledgments
This research was supported by the Intramural Research Program of the NIMH, NIH. We thank T. DeGuzman, B. L. Justiment, and D. Kazuba for their contributions to this research. We would also like to thank our two anonymous reviewers for their thoughtful suggestions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael Wheaton, Laboratory of Clinical Science, National Institute of Mental Health.
Kiara R. Timpano, Florida State University
V. Holland LaSalle-Ricci, Laboratory of Clinical Science, National Institute of Mental Health.
Dennis L. Murphy, Laboratory of Clinical Science, National Institute of Mental Health
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fourth (DSM-IV) Washington, DC: APA; 1994. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Chabane N, Delorme R, Millet B, Mouren MC, Leboyer M, Pauls D. Early-onset obsessive-compulsive disorder: a subgroup with a specific clinical and familial pattern? Journal of Child Psychology and Psychiatry. 2005;46:881–887. doi: 10.1111/j.1469-7610.2004.00382.x. [DOI] [PubMed] [Google Scholar]
- Coles ME, Frost RO, Heimberg RG, Steketee G. Hoarding behaviors in a large college sample. Behaviour Research and Therapy. 2003;41:179–194. doi: 10.1016/s0005-7967(01)00136-x. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-P) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Fontenelle LF, Mendlowicz MV, Soares ID, Versiani M. Patients with obsessive-compulsive disorder and hoarding symptoms: A distinctive clinical subtype? Comprehensive Psychiatry. 2004;45:375–383. doi: 10.1016/j.comppsych.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Frankenburg FR. Hoarding in anorexia nervosa. British Journal of Medical Psychology. 1984;57:57–60. doi: 10.1111/j.2044-8341.1984.tb01581.x. [DOI] [PubMed] [Google Scholar]
- Frost RO, Gross RC. The hoarding of possessions. Behaviour Research and Therapy. 1993;31:367–381. doi: 10.1016/0005-7967(93)90094-b. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Greene KAI. Interventions for compulsive hoarding. Journal of Brief Treatment and Crisis Intervention. 2003;25:323–337. [Google Scholar]
- Frost RO, Steketee G, Grisham J. Measurement of compulsive hoarding: Saving Inventory-Revised. Behaviour Research and Therapy. 2004;42:1163–1182. doi: 10.1016/j.brat.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Williams LF. Hoarding: A community health problem. Health and Social Care in the Community. 2000;8:229–234. doi: 10.1046/j.1365-2524.2000.00245.x. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Williams LF, Warren R. Mood, personality disorder symptoms and disability in obsessive compulsive hoarders: A comparison with clinical and nonclinical controls. Behaviour Research and Therapy. 2000;38:1071–1081. doi: 10.1016/s0005-7967(99)00137-0. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Archives of General Psychiatry. 1989a;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Archives of General Psychiatry. 1989b;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Grisham JR, Brown TA, Liverant GI, Campbell-Sills L. The distinctiveness of compulsive hoarding from obsessive-compulsive disorder. Anxiety Disorders. 2005;19:767–779. doi: 10.1016/j.janxdis.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Hanna GL. Demographic and clinical features of obsessive-compulsive disorder in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:19–27. doi: 10.1097/00004583-199501000-00009. [DOI] [PubMed] [Google Scholar]
- Hasler G, Lasalle-Ricci H, Ronquillo JG, Crawley SA, Cochran LW, Kazuba D, et al. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Research. 2005;135:121–132. doi: 10.1016/j.psychres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Hwang JP, Tsai SJ, Yang CH, Liu KM, Lirng JF. Hoarding behaviors in dementia. American Journal of Geriatric Psychiatry. 1998;6:285–289. [PubMed] [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF) British Journal of Psychiatry. 1995;166:654–659. doi: 10.1192/bjp.166.5.654. [DOI] [PubMed] [Google Scholar]
- Karno M, Golding JM, Sorenson SB, Burnam MA. The epidemiology of obsessive–compulsive disorder in five US communities. Archives of General Psychiatry. 1988;45:1094–1099. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- LaSalle-Ricci VH, Arnkoff DB, Glass CR, Crawley SA, Ronquillo JG, Murphy DL. The hoarding dimension of OCD: Psychological comorbidity and the five-factor personality model. Behaviour Research and Therapy. 2006;44:1503–1512. doi: 10.1016/j.brat.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Lochner C, Kinnear CJ, Hemmings SM, Seller C, Niehaus DJ, Knowles JA, et al. Hoarding in obsessive-compulsive disorder: Clinical and genetic correlates. Journal of Clinical Psychiatry. 2005;66:1155–1160. doi: 10.4088/jcp.v66n0911. [DOI] [PubMed] [Google Scholar]
- Luchins DJ, Goldman MB, Lieb M, Hanrahan P. Repetitive behaviors in chronically institutionalized schizophrenic patients. Schizophrenia Research. 1992;8:119–123. doi: 10.1016/0920-9964(92)90027-3. [DOI] [PubMed] [Google Scholar]
- Maier T. On phenomenology and classification of hoarding: a review. Acta psychiatrica Scandinavica. 2004;110:323–337. doi: 10.1111/j.1600-0447.2004.00402.x. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:228–238. doi: 10.1176/appi.ajp.162.2.228. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Archives of General Psychiatry. 2004;61:564–576. doi: 10.1001/archpsyc.61.6.564. [DOI] [PubMed] [Google Scholar]
- Piersma HL, Boes JL. The GAF and psychiatric outcome: a descriptive report. Community Mental Health Journal. 1997;33:35–40. doi: 10.1023/a:1022413110345. [DOI] [PubMed] [Google Scholar]
- Pigott TA. Anxiety disorders in women. Psychiatric Clinics of North America. 2003;26:621–672. doi: 10.1016/s0193-953x(03)00040-6. [DOI] [PubMed] [Google Scholar]
- Rasmussen SA, Eisen JL. The epidemiology and clinical features of obsessive-compulsive disorder. Psychiatric Clinics of North America. 1992;15:743–758. [PubMed] [Google Scholar]
- Rosario-Campos MC, Miguel EC, Quatrano S, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Bienvenu OJ, 3rd, Pinto A, Fyer AJ, McCracken JT, Rauch SL, et al. Hoarding in obsessive-compulsive disorder: Results from the OCD Collaborative Genetics Study. Behaviour Research and Therapy. doi: 10.1016/j.brat.2006.05.008. In Press. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Bienvenu OJ, Riddle MA, Cullen BAM, Grados MA, Liang KY, et al. Hoarding in obsessive compulsive disorder: Results from a case-control study. Behaviour Research and Therapy. 2002;40:517–528. doi: 10.1016/s0005-7967(01)00026-2. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Shugart YY, Grados MA, Willour VL, Bienvenu OJ, et al. Signficant linkage to compulsive hoarding on chromosome 14 in families with obsessive compulsive disorder: results from the OCD collaborative, Genetics study. American Journal of Psychiatry. doi: 10.1176/ajp.2007.164.3.493. in press. [DOI] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Maidment KM, Baxter LR., Jr Paroxetine treatment of compulsive hoarding. Journal of Psychiatric Research. 2006 doi: 10.1016/j.jpsychires.2006.05.001. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Maidment KM, Smith EC, Zohrabi N, Katz E, et al. Cerebral glucose metabolism in obsessive-compulsive hoarding. American Journal of Psychiatry. 2004;161:1038–1048. doi: 10.1176/appi.ajp.161.6.1038. [DOI] [PubMed] [Google Scholar]
- Saxena S, Maidment KM, Vapnik T, Golden G, Rishwain T, Rosen RM, et al. Obsessive-compulsive hoarding: Symptom severity and response to multimodal treatment. Journal of Clinical Psychiatry. 2002;63:21–27. [PubMed] [Google Scholar]
- Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM-III-R: An evaluative review. Comprehensive Psychiatry. 1994;35:316–327. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- Shafran R, Tallis F. Obsessive-compulsive hoarding: A cognitive-behavioral approach. Behavioural and Cognitive Psychotherapy. 1996;24:209–221. [Google Scholar]
- Shugart YY, Samuels J, Willour VL, Grados MA, Greenberg BD, Knowles JA, et al. Genomewide linkage scan for obsessive-compulsive disorder: evidence for susceptibility loci on chromosomes 3q, 7p, 1q, 15q, and 6q. Molecular Psychiatry. 2006;11:763–770. doi: 10.1038/sj.mp.4001847. [DOI] [PubMed] [Google Scholar]
- Slattery MJ, Dubbert BK, Allan AJ, Leonard HL, Swedo SE, Gourley MF. Prevalence of obsessive compulsive-disorder in patients with systemic lupus erythematosis. Journal of Clinical Psychiatry. 2004;65:301–306. doi: 10.4088/jcp.v65n0303. [DOI] [PubMed] [Google Scholar]
- Sohlberg S. There’s more in a number than you think: new validity data for the Global Assessment Scale. Psychological Reports. 1989;64:455–461. doi: 10.2466/pr0.1989.64.2.455. [DOI] [PubMed] [Google Scholar]
- Steketee G, Frost R, Bogart K. The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behaviour Research and Therapy. 1996;34:675–84. doi: 10.1016/0005-7967(96)00036-8. [DOI] [PubMed] [Google Scholar]
- Tukel R, Polat A, Genc A, Bozkurt O, Atli H. Gender-related differences among Turkish patients with obsessive-compulsive disorder. Comprehensive Psychiatry. 2004;45:362–366. doi: 10.1016/j.comppsych.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Weismann MM, Bland RC, Canino GJ, Greenwald S, Hwu H, Lee CK, et al. The cross national epidemiology of obsessive compulsive disorder. Journal of Clinical Psychiatry. 1994;55:5–10. [PubMed] [Google Scholar]
- Winsberg ME, Cassic KS, Koran IM. Hoarding in obsessive-compulsive disorder: A report of 20 cases. Journal of Clinical Psychiatry. 1999;60:591–597. doi: 10.4088/jcp.v60n0905. [DOI] [PubMed] [Google Scholar]
- Wu KD, Watson D. Hoarding and its relation to obsessive-compulsive disorder. Behaviour Research and Therapy. 2005;43:897–921. doi: 10.1016/j.brat.2004.06.013. [DOI] [PubMed] [Google Scholar]
- Zhang H, Leckman JF, Pauls DL, Tsai CP, Kidd KK, Campos MR. Genomewide scan of hoarding in sib pairs in which both sibs have Gilles de la Tourette syndrome. American Journal of Human Genetics. 2002;70:896–904. doi: 10.1086/339520. [DOI] [PMC free article] [PubMed] [Google Scholar]