Abstract
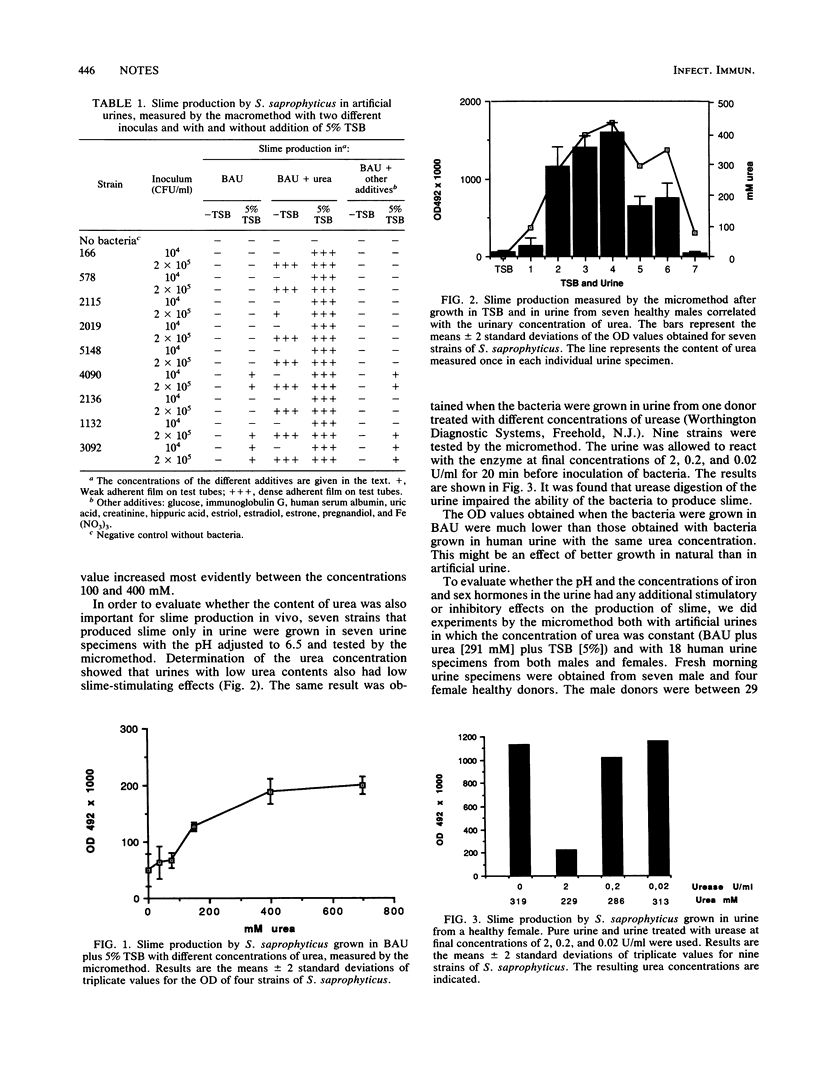
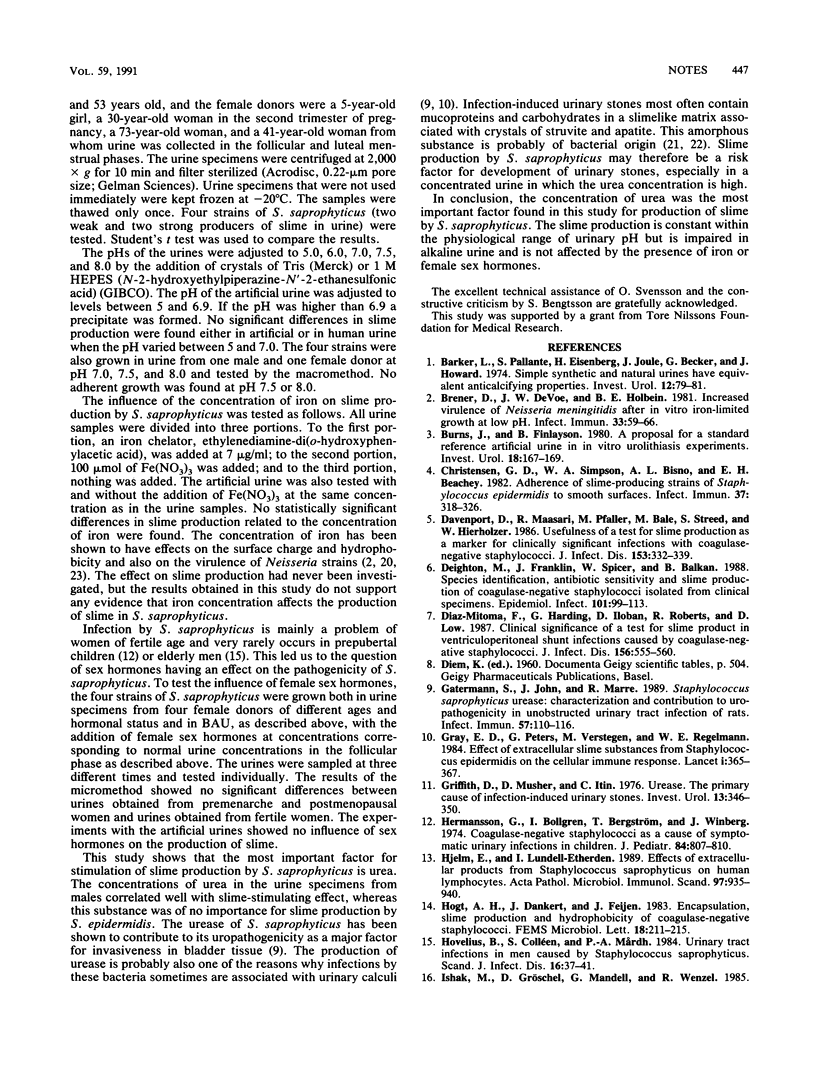
Only 9 of 30 Staphylococcus saprophyticus strains produced slime in trypticase soy broth, while all did so in urine. It was found that urea was essential for the production of slime. The pH, the iron concentration, or the presence of sex hormones did not affect slime production.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barker L. M., Pallante S. L., Eisenberg H., Joule J. A., Becker G. L., Howard J. E. Simple synthetic and natural urines have equivalent anticalcifying properties. Invest Urol. 1974 Jul;12(1):79–81. [PubMed] [Google Scholar]
- Brener D., DeVoe I. W., Holbein B. E. Increased virulence of Neisseria meningitidis after in vitro iron-limited growth at low pH. Infect Immun. 1981 Jul;33(1):59–66. doi: 10.1128/iai.33.1.59-66.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns J. R., Finlayson B. A proposal for a standard reference artificial urine in in vitro urolithiasis experiments. Invest Urol. 1980 Sep;18(2):167–169. [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport D. S., Massanari R. M., Pfaller M. A., Bale M. J., Streed S. A., Hierholzer W. J., Jr Usefulness of a test for slime production as a marker for clinically significant infections with coagulase-negative staphylococci. J Infect Dis. 1986 Feb;153(2):332–339. doi: 10.1093/infdis/153.2.332. [DOI] [PubMed] [Google Scholar]
- Deighton M. A., Franklin J. C., Spicer W. J., Balkau B. Species identification, antibiotic sensitivity and slime production of coagulase-negative staphylococci isolated from clinical specimens. Epidemiol Infect. 1988 Aug;101(1):99–113. doi: 10.1017/s0950268800029265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Mitoma F., Harding G. K., Hoban D. J., Roberts R. S., Low D. E. Clinical significance of a test for slime production in ventriculoperitoneal shunt infections caused by coagulase-negative staphylococci. J Infect Dis. 1987 Oct;156(4):555–560. doi: 10.1093/infdis/156.4.555. [DOI] [PubMed] [Google Scholar]
- Gatermann S., John J., Marre R. Staphylococcus saprophyticus urease: characterization and contribution to uropathogenicity in unobstructed urinary tract infection of rats. Infect Immun. 1989 Jan;57(1):110–116. doi: 10.1128/iai.57.1.110-116.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray E. D., Peters G., Verstegen M., Regelmann W. E. Effect of extracellular slime substance from Staphylococcus epidermidis on the human cellular immune response. Lancet. 1984 Feb 18;1(8373):365–367. doi: 10.1016/s0140-6736(84)90413-6. [DOI] [PubMed] [Google Scholar]
- Griffith D. P., Musher D. M., Itin C. Urease. The primary cause of infection-induced urinary stones. Invest Urol. 1976 Mar;13(5):346–350. [PubMed] [Google Scholar]
- Hermansson G., Bollgren I., Bergström T., Winberg J. Coagulase negative staphylococci as a cause of symptomatic urinary infections in children. J Pediatr. 1974 Jun;84(6):807–810. doi: 10.1016/s0022-3476(74)80752-3. [DOI] [PubMed] [Google Scholar]
- Hjelm E., Lundell-Etherden I. Effects of extracellular products from Staphylococcus saprophyticus on human lymphocytes. APMIS. 1989 Oct;97(10):935–940. doi: 10.1111/j.1699-0463.1989.tb00501.x. [DOI] [PubMed] [Google Scholar]
- Hovelius B., Colleen S., Mårdh P. A. Urinary tract infections in men caused by Staphylococcus saprophyticus. Scand J Infect Dis. 1984;16(1):37–41. doi: 10.3109/00365548409068407. [DOI] [PubMed] [Google Scholar]
- Jordan P. A., Iravani A., Richard G. A., Baer H. Urinary tract infection caused by Staphylococcus saprophyticus. J Infect Dis. 1980 Oct;142(4):510–515. doi: 10.1093/infdis/142.4.510. [DOI] [PubMed] [Google Scholar]
- Magnusson K. E., Kihlstrom E., Norqvist A., Davies J., Normark S. Effect of iron on surface charge and hydrophobicity of Neisseria gonorrhoeae. Infect Immun. 1979 Nov;26(2):402–407. doi: 10.1128/iai.26.2.402-407.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean R. J., Nickel J. C., Noakes V. C., Costerton J. W. An in vitro ultrastructural study of infectious kidney stone genesis. Infect Immun. 1985 Sep;49(3):805–811. doi: 10.1128/iai.49.3.805-811.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickel J. C., Emtage J., Costerton J. W. Ultrastructural microbial ecology of infection-induced urinary stones. J Urol. 1985 Apr;133(4):622–627. doi: 10.1016/s0022-5347(17)49116-6. [DOI] [PubMed] [Google Scholar]
- Payne S. M., Finkelstein R. A. Pathogenesis and immunology of experimental gonococcal infection: role of iron in virulence. Infect Immun. 1975 Dec;12(6):1313–1318. doi: 10.1128/iai.12.6.1313-1318.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters G., Locci R., Pulverer G. Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis. 1982 Oct;146(4):479–482. doi: 10.1093/infdis/146.4.479. [DOI] [PubMed] [Google Scholar]
- Pfaller M., Davenport D., Bale M., Barrett M., Koontz F., Massanari R. M. Development of the quantitative micro-test for slime production by coagulase-negative staphylococci. Eur J Clin Microbiol Infect Dis. 1988 Feb;7(1):30–33. doi: 10.1007/BF01962167. [DOI] [PubMed] [Google Scholar]
- Sheth N. K., Franson T. R., Sohnle P. G. Influence of bacterial adherence to intravascular catheters on in-vitro antibiotic susceptibility. Lancet. 1985 Dec 7;2(8467):1266–1268. doi: 10.1016/s0140-6736(85)91552-1. [DOI] [PubMed] [Google Scholar]
- Wallmark G., Arremark I., Telander B. Staphylococcus saprophyticus: a frequent cause of acute urinary tract infection among female outpatients. J Infect Dis. 1978 Dec;138(6):791–797. doi: 10.1093/infdis/138.6.791. [DOI] [PubMed] [Google Scholar]


