Abstract
Human infections with Ebola virus (EBOV) result in a deadly viral disease known as Ebola hemorrhagic fever. Up to 90% of infected patients die, and there is no available treatment or vaccine. The sporadic human outbreaks are believed to result when EBOV “jumps” from an infected animal to a person and is subsequently transmitted between persons by direct contact with infected blood or body fluids. This study was undertaken to investigate the mechanism by which EBOV can persistently infect and then escape from model cell and animal reservoir systems. We report a model system in which infection of mouse and bat cell lines with EBOV leads to persistence, which can be broken with low levels of lipopolysaccharide or phorbol-12-myristate-13-acetate (PMA). This reactivation depends on the Ras/MAPK pathway through inhibition of RNA-dependent protein kinase and eukaryotic initiation factor 2α phosphorylation and occurs at the level of protein synthesis. EBOV also can be evoked from mice 7 days after infection by PMA treatment, indicating that a similar mechanism occurs in vivo. Our findings suggest that EBOV may persist in nature through subclinical infection of a reservoir species, such as bats, and that appropriate physiological stimulation may result in increased replication and transmission to new hosts. Identification of a presumptive mechanism responsible for EBOV emergence from its reservoir underscores the “hit-and-run” nature of the initiation of human and/or nonhuman primate EBOV outbreaks and may provide insight into possible countermeasures to interfere with transmission.
Ebola virus (EBOV) has caused sporadic outbreaks in isolated areas of equatorial Africa since its discovery more than 30 years ago. Because the natural host for EBOV remains unknown, implementing programs to control or eliminate viral reservoirs of transmission to human or nonhuman primate (NHP) populations has been impossible. The rapid progression of EBOV infection, which affords little opportunity to develop an effective immune response, along with the unavailability of antiviral therapy or approved vaccine (1–6), make targeting interventions at the initial spread from a reservoir to humans an important goal.
It has long been believed that, like several other classical viral zoonotic diseases, EBOV persists in some reservoir species as a chronic/persistent infection that does not (or only rarely) produce disease, with both the reservoir and the virus kept alive for a sufficient period to allow transmission to other susceptible hosts. Many different species, including bats, mice, shrews, and other small terrestrial animals, have been suspected (7), but despite an intensive search, none has been found to produce live EBOV under natural conditions. Although outbreaks often have been traced to contacts with NHPs, these species are unlikely to be reservoir sources, because they also suffer similar high lethality as humans from EBOV. Following the discovery of EBOV in 1976, and again after the 1994 case in the Côte d'Ivoire and the 1995 outbreak in the Democratic Republic of Congo, intensive efforts have been made to identify the natural reservoir; to date, however, neither potential hosts nor arthropod vectors have been identified (8–11).
The search for the natural reservoir for EBOV and Marburg virus continues. Although a report by Morvan et al. (12) indicated detection of EBOV RNA in rodents (Muridae and Soricidae) captured in the Central African Republic and suggested mice, rats, and shrews as possible reservoir species, these findings have not been confirmed by an alternative methodology (i.e., serology, antigen detection or virus isolation) or by other groups. Although this would have implications for transmission through the close approximation of infected rodent/shrew species to human populations, as has been reported for Lassa virus (13), because of the close affiliation of these rodents to human populations and the sporadic nature of human outbreaks, it is unlikely that these species are involved in the transmission of EBOV to humans. Rodent species have been used as model systems for studying filovirus pathogenesis; nonetheless, these species do not exhibit lethality after wild-type infection, but require adaptation through serial passage (14–18). Through such studies, many details of the pathogenesis have been deciphered, including the type I interferon (IFN) response, which plays a key role in the resistance of normal mice to mouse-adapted Zaire ebolavirus (MA-ZEBOV) (15, 19). What remains unclear is the mechanisms underlying the high susceptibility of some species (i.e., humans and NHPs) to wild-type virus compared with other species (i.e., mice and possibly bats). Recent work has provided support for a role of fruit bats as a reservoir species for EBOV and Marburg virus (20–22), but whether other species also are involved is not known, and the mechanism of the spillover from reservoir to humans and NHPs remains unclear.
This study was designed to investigate the nature of EBOV in a model system of a reservoir host. We used mouse and bat cell lines to model the mechanism of the establishment of a low-level persistent infection with wild-type ZEBOV, as well as of the escape of the virus from this low-level state through activation of the Ras/MAPK pathway and its suppressive effects on the IFN response. We show that a similar release from low-level infection can occur in an in vivo model of Balb/C mice infected with ZEBOV through stimulation with phorbol esters and reactivating virus 7 days after the initial infection.
Results
In an effort to find cell lines that mimic the natural reservoirs' predicted ability to survive and support persistent infection, we screened a number of cell lines. We found that the mouse lines NIH 3T3 and RAW264.7 (mouse fibroblast and macrophage line, respectively), as well as a Mexican free-tailed bat line (Tb1.Lu, a bat lung fibroblast), have this capacity. After infecting cells with a multiplicity of infection (MOI) of 0.1 of ZEBOV strain Mayinga or ZEBOV strain Mayinga expressing enhanced green fluorescence protein (GFP) from an additional transcriptional unit inserted stably into the genome between the nucleoprotein and VP35 genes (ZEBOV/GFP) (23), RAW264.7 cells showed very little cytopathic effect and could be passaged and maintained in a similar fashion as uninfected cells. For each of the experiments described herein, persistently infected cells, designated RAWZEBOVpi or RAWZEBOV/GFPpi, were used at passage numbers >7 and <22. Persistent infection was confirmed by removal of supernatants, centrifugation of cellular debris, and transference to uninfected Vero E6 cells for virus titration using either a focus-forming unit (FFU) or a TCID50 (tissue culture infectious dose leading to cytopathic effect in 50%) assay. We were able to recover viable ZEBOV and ZEBOV/GFP from both the RAWZEBOVpi and RAWZEBOV/GFPpi persistently infected cells lines for up to 10 months after the initial infection. Titers obtained from these cultures varied from 2.0 × 103 to 3.4 × 103 FFU/ml for RAWZEBOVpi and from 1.2 × 103 to 8.1 × 103 for RAWZEBOV/GFPpi over the 10-month period.
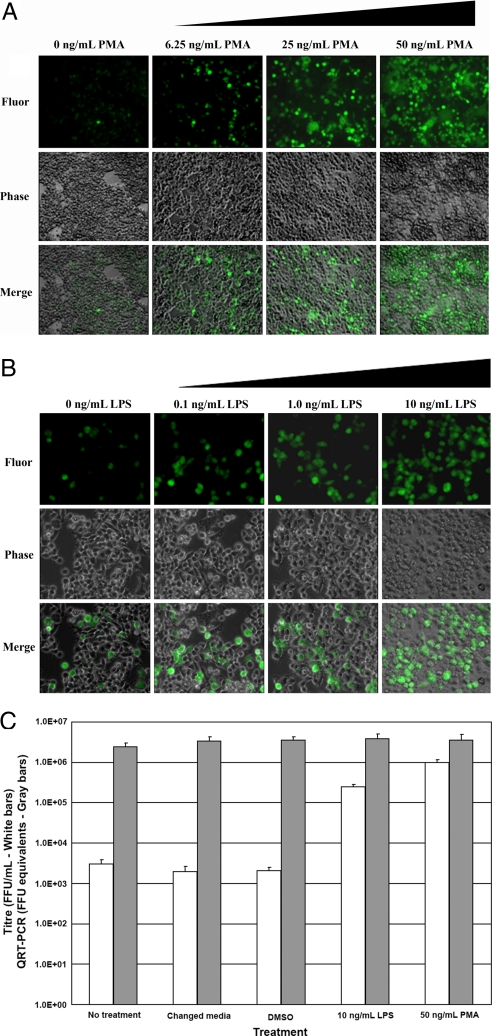
Although the mechanisms of emergence from viral latency have been studied most thoroughly in viruses with nuclear replication strategies, a few RNA viruses with cytoplasmic replication, such as paramyxoviruses, hantaviruses, arenaviruses (24–28), and possibly filovirus (29), also may have longer-term persistence using similar strategies. We next tested to see whether latent ZEBOV infection, like other latent infections, such as herpesvirus or human immunodeficiency virus (HIV) (30–32), could be induced to replicate to higher titers through physiological treatments. Typically, RAWZEBOVpi cells produced low levels of viral expression, as determined by GFP expression (Fig. 1 A and B), and resulted in virus production of ≈103 FFU/ml (Fig. 1C). But treatment of the RAWZEBOVpi with phorbol-12-myristate-13-acetate (PMA) or lipopolysaccharide (LPS) dramatically increased the amount of viral GFP expression and infectious outputs (averaging 3.0 × 103 FFU/ml in controls, 2.5 × 105 FFU/ml for LPS-treated cells, and 9.8 × 105 FFU/ml for PMA-treated cells) in a dose-responsive fashion (Fig. 1 A–C). By performing quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) on RNA isolated from these persistently infected cell lines, we determined that the increased virus output under PMA and LPS treatments occurred not at the level of viral RNA transcription/replication (Fig. 1C), but rather at the level of viral protein production (Fig. 1 A and B).
Fig. 1.
PMA and LPS cause increased viral expression in ZEBOV persistently infected RAW264.7 cells but do not significantly change viral RNA levels. Dose-dependent induction of GFP expression from RAWZEBOV/GFPpi cells by PMA (A) and LPS (B) at 24 h posttreatment. (C) Infectious titer (white bars) and viral RNA (gray bars) output from supernatants from RAWZEBOV/GFPpi following no treatment or treatment with changed media (containing 10% FBS), media containing DMSO, media containing 10 ng/ml LPS, or media containing 50 ng/ml PMA as determined by plaque titration on VeroE6 cells using an FFU assay or quantitative RT-PCR of the EBOV glycoprotein (GP) gene as the target. All cells were originally infected with MOI of 0.1 of ZEBOV/GFP and passaged for at least 7, but not more than 22, passages. Results are expressed as average and standard deviations from triplicate runs.
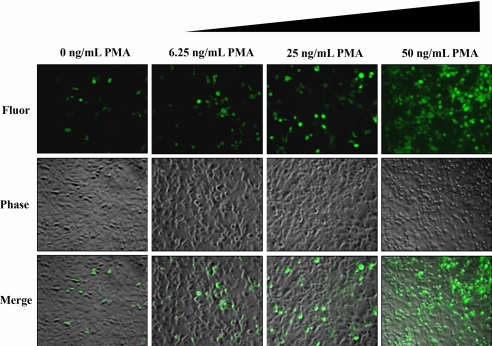
Because bat species have long been suspected reservoirs for filoviruses and have been recently shown to harbor viral RNA and/or virus-specific antibodies (20–22), we evaluated a bat cell line for this capability. Similar to RAW264.7, Tbl.Lu cells established ZEBOV persistence and showed little virus propagation, but could be induced to more productive viral infection after PMA treatment (Fig. 2).
Fig. 2.
PMA causes dose-dependent increased viral expression of ZEBOV in the persistently infected Mexican free-tailed bat cell line Tb1.Lu. Dose-dependent induction of GFP expression from Tb1.Lu ZEBOV/GFPpi cells by PMA at 24 h posttreatment.
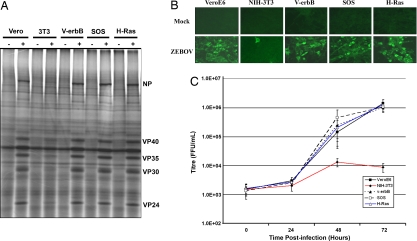
Because previous studies have shown that exogenous stimulation of cells can decrease the cells' type I IFN responses (33–36), we investigated whether similar mechanisms were at play here. Specifically, because both LPS and PMA are known to stimulate the Ras/MAPK pathways (37–40), and because activation of the Ras/MAPK pathway has been shown to antagonize the effects of type 1 IFN (33–36), we next tested whether the robustness of ZEBOV protein synthesis is affected by specifically activating the Ras/MAPK pathway. Like RAW264.7 cells, NIH 3T3 cells are poorly infectible by ZEBOV (Fig. 3 A and B). We took advantage of this feature and NIH 3T3 cells stably transformed with activated versions of the v-erbB, SOS, and H-Ras oncogenes to investigate whether the efficiency of infection of the parental NIH 3T3 line could be bolstered with these activated oncogenes. As shown in Fig. 3C, titers obtained from the parental NIH 3T3 line were substantially lower than those from Vero E6 cells, whereas titers from the v-erbB, SOS, and H-Ras cells were comparable to those from Vero E6. Similarly, the amount of viral protein produced in the v-erbB–, SOS-, and H-Ras-transformed cells was comparable to that obtained from Vero E6 and substantially higher than that from the NIH 3T3 parental line (Fig. 3 A and B). It is important to note that most laboratories use the Vero E6 cell line to propagate ZEBOV, because these cells are highly susceptible by ZEBOV and are known to not produce type I IFN (41, 42). To address the question of whether the enhanced viral productivity was due to increased production of ZEBOV proteins in infected cells or rather to an increased percentage of cells expressing viral proteins, we performed an immunofluorescent assay with a ZEBOV/VP40-specific antibody. As shown in Fig. 3B, the percentage of infected cells was <5% in the NIH 3T3 cells, compared with 60%−80% in the Vero E6 and transformed cell lines.
Fig. 3.
ZEBOV infects v-erbB–, SOS-, and H-Ras–transformed cells with higher efficiency than parental NIH 3T3 cells. (A) Various cell lines were infected with ZEBOV at MOI of 0.1 and continuously 35S-labeled from 48–72 h postinfection, showing that transformed cells produced viral proteins at levels comparable to VeroE6 cells, whereas NIH 3T3 cells produced substantially lower amounts of ZEBOV proteins. “+” refers to infected with ZEBOV, and “–” refers to mock infection. (B) Immunofluorescent assay using α-VP40 monoclonal antibody (59) (1:800 dilution in PBS), followed by goat anti-mouse FITC-conjugate (1:250 dilution in PBS with 10% goat serum) demonstrating that NIH 3T3 cells had a lower percentage of infected cells at 48 h postinfection compared with the transformed cells or VeroE6. (C) Infectious titer output from supernatants from ZEBOV-infected cell lines over 72 h as determined by plaque titration on VeroE6 cells. Results are expressed as average and standard deviations from triplicate runs.
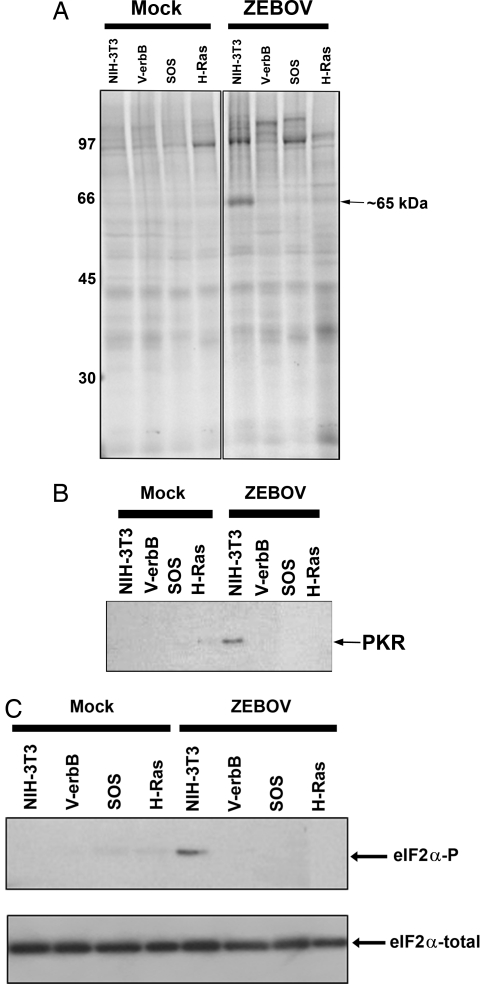
Previous studies have shown that activated Ras/MAPK transformation affects IFN response through the interference of double-stranded RNA-dependent protein kinase (PKR) and eukaryotic initiation factor 2α (eIF2α) activities (33, 34, 43). This property, along with the observation that ZEBOV transcripts are produced in the poorly infectible cells but not translated lead us to speculate that double-stranded PKR and eIF2α may be conveying translational suppression in the untransformed cells. To test whether the enhanced infectibility conferred by the activated oncogenes resulted from the suppression of PKR and eIF2α activity, we performed in vitro kinase reactions using γ [33P]-ATP. As shown in Fig. 4A, a ≈65-kDa phosphoprotein was produced in the NIH 3T3 cells only after exposure to ZEBOV. No such ≈65-kDa phosphoprotein was produced in the cells with the activated oncogenes or any mock-infected cell line. This ≈65-kDa phosphoprotein was precipitable with a PKR-specific antibody (Fig. 4B). Moreover, Western blot analysis using an antibody specific for the phosphorylated form of eIF2α showed that only ZEBOV-exposed NIH 3T3 cells produced phosphorylated eIF2α (Fig. 4C). Therefore, in untransformed cells, viral RNA stimulates a cellular defense mechanism through the activation of PKR. Activated PKR prevents the translation of transcripts by inactivation of eIF2α through phosphorylation (44). The oncogene signaling interferes with this defense mechanism by inhibiting virus-induced PKR activation, thereby allowing the synthesis of ZEBOV proteins.
Fig. 4.
PKR and eIF2α are phosphorylated in less infectible cells. (A) In vitro kinase assays from cell lysates of the various cell lines at 48 h post-ZEBOV infection (MOI = 0.6) versus mock infection, demonstrating the production of a ≈65-kDa phosphoprotein only from the NIH 3T3 cells and only postexposure to ZEBOV. (B) Immunoprecipitation of the in vitro kinase lysates from (A) with 5 μg of PKR antibody demonstrating that the ≈65-kDa phosphoprotein is PKR. (C) eIF2α was phosphorylated in NIH 3T3 cells only post-ZEBOV infection, as demonstrated by Western blot using anti-phosphospecific eIF2α (10 μg/ml diluted in Tris-buffered saline diluted in 5% milk) (Upper). Total eIF2α is shown as a loading control (Lower)].
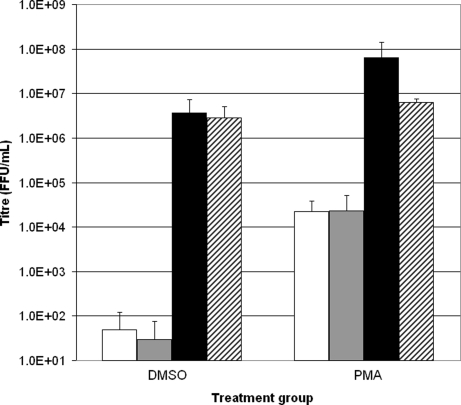
Finally, to test whether this effect of establishing persistence and reactivation of ZEBOV can occur in vivo, we infected female BALB/c mice with either ZEBOV/GFP or MA-ZEBOV (1000 FFU/ml) through intraperitoneal (i.p.) injection, recorded daily weights, and scored for symptoms. Then, 6 days later, we stimulated the mice for 24 h with an i.p. injection of PMA or dimethyl sulfoxide (DMSO) (the diluent control), then euthanized them on day 7. Viral output was analyzed through plaque titration. The results, shown in Fig. 5, demonstrate that viral titers from the livers and spleens of ZEBOV/GFP–infected mice after i.p. injection of PMA were almost three logs higher than those after i.p. injection of DMSO.
Fig. 5.
PMA induces higher production of infectious ZEBOV/GFP in livers and spleens of BALB/c mice. Female BALB/c mice were infected with either ZEBOV/GFP (1000 FFU in 200 μl of DMEM) or MA-ZEBOV (1000 FFU in 200 μl of DMEM) and allowed to incubate for 6 days. Then 200 μl of DMEM containing 100 ng/ml of PMA or an equivalent amount of DMSO (diluent for PMA) was injected i.p. After 24 h, the mice were euthanized, organs were harvested, and focus-forming assays were performed on the serially diluted homogenates. Results are shown from livers of ZEBOV/GFP–infected mice (white bars), spleens of ZEBOV/GFP–infected mice (gray bars), livers of MA-ZEBOV–infected mice (black bars), and spleens of MA-ZEBOV–infected mice (cross-hatched bars). Mock-infected mice were treated similarly and served as negative controls (data not shown). Five mice were used for each group. Results are expressed as average plus standard deviation.
Discussion
Although it was originally thought that resistance of normal adult mice to filovirus infection resulted from an inability of these viruses to infect murine cells, mice deprived of their type 1 IFN response proved to be susceptible to lethal infection by a number of filoviruses (15). Therefore, mouse cells seem to be resistant to EBOV infection through the establishment of a persistent low-level infection, due to the induction of the IFN antiviral response by EBOV. Suppressing this antiviral response by stimulating the Ras/MAPK pathway causes a switch from a low-level infection to a more productive infection. EBOV's persistence in a form that continually produces RNA but suppresses the translation of that RNA until the Ras/MAPK pathway is activated is a novel mechanism of viral reactivation from persistence. This mechanism relies on the IFN response through PKR and eIF2α signaling and is supported by previous studies showing suppression of IFN signaling by oncogenic transformation (33–36), as well as by exogenous stimulation of these pathways (45).
This is not the first evidence indicating that EBOV is capable of causing prolonged infection in cells, animal models, or even human patients. Calain et al. (46) were able to passage undiluted ZEBOV to eventually arrive at a virus stock containing defective interfering particles, allowing for the establishment of persistently infected cell lines. Gupta et al. (47) were able to establish persistent infection with MA-ZEBOV in immunodeficient mice. The fact that during naturally acquired human infections filoviruses have been isolated from seminal fluid months after disease onset and recovery, also suggests that more prolonged filoviral infections or delay in virus clearance from privileged sites can occur (29, 48–51).
Although the present study does not identify the reservoir host, it does provide a mechanism for the establishment of viral persistence, as well as a potential mechanism of spillover. These data also support earlier findings demonstrating the replication and circulation of ZEBOV in experimentally infected fruit and insectivorous bats in the absence of illness (7). Nonetheless, the higher titers shown in the experimental bat model raise questions as to why virus isolation has not been achieved from any of the naturally infected bat species (20–22). One suggestion is that virus titers may be very low in these naturally infected animals; consistent with the need for nested RT-PCR to detect ZEBOV-specific nucleic acid, and that specific physiologic or environmental stimuli are needed to stimulate virus production (20). The finding that ZEBOV may require activation of the Ras/MAPK pathway for productive infection may be the first clue as to the nature of the physiologic or environmental stimuli needed to activate virus expression in nature. Although definitive proof of this mechanism requires the establishment of persistent EBOV infection in a reservoir species, followed by provocation by the methods described in this report, this will have to await future studies, including definitive identification of the reservoir species.
If we assume (as now seems likely) that bats play a role as a reservoir species for filoviruses, then examining the roles of seasonal, environmental, and temporal physiological factors (e.g., pregnancy, other stresses) in facilitating virus replication and subsequent transmission to other susceptible hosts will be important. The activation of EBOV through stimulation of the Ras/MAPK pathway may explain the cryptic nature of its emergence; due to the fact that production of EBOV from these species would be transient and that contact with the stimulated organism to NHP or humans would be infrequent. This also could explain the periodicity of some filovirus outbreaks occurring during the late rainy season or early dry season (52), possible periods of stress or switching of food types, which may correlate with enhanced Ras/MAPK signaling in the reservoir. Alternatively, phorbol esters or other naturally occurring homologues produced during restricted ecologic/climactic periods may account for this infrequency. The fact that LPS also was capable of enhancing EBOV productivity from mouse macrophages also belies the possibility of synergy between virus and bacteria as occurs for HIV and syphilis, influenza and Streptcoccus pneumoniae, and herpes and periodontal bacteria (53–55). Other factors also may contribute, including pregnancy, which has been suggested to play a role in the transmission of Hendra virus from bats to horses (56, 57). Because the pregnancy state is one of enhanced MAPK signaling (58), this role certainly could be explained by this mechanism.
Although we have not used the foregoing approach to positively identify the reservoir species of EBOV, it certainly could be used as a tool for such purposes. To the best of our knowledge, this approach of pharmacologically stimulating persistently infected cells has not been applied to other persistent viral infections of animals. Most notably, it has not been tried in other high-consequence RNA viral pathogens of humans that are maintained in known reservoir species, such as wild rodents (e.g., hantaviruses, arenaviruses), nor those potentially maintained in bats (e.g., Hendra virus, Nipah virus). A similar experimental approach might be used to identify reservoir hosts and provide insights into the mechanisms of escape of other viral pathogens.
Methods
Cells and Virus.
RAW264.7 and Tb1.Lu cells were obtained from the American Type Culture Collection. Parental NIH 3T3 cell lines, along with NIH 3T3 cells transformed with a number of oncogenes, were obtained from various sources. Parental NIH 3T3 and NIH 3T3 cells transfected with H-Ras were generously provided by Dr. Douglas Faller, Boston University School of Medicine. NIH 3T3 cells along with their SOS-transformed counterparts (designated TNIH#5) were generously provided by Dr. Michael Karin, University of California San Diego. Dr. H.-J. Kung, Case Western Reserve University kindly donated the parental NIH 3T3 cells along with NIH 3T3 cells transfected with the v-erbB oncogene (designated THC-11). All cells were grown and maintained at 37 °C in complete medium containing Dulbecco's modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 2 mmol/L of l-glutamine, 100 U/ml of penicillin, and 100 μg/ml of streptomycin.
Establishment of ZEBOV and ZEBOV/GFP Persistence and Treatments.
RAW264.7 or Tb1.Lu cells were originally infected with an MOI of 0.1 of ZEBOV strain Mayinga or ZEBOV/GFP and were passaged and maintained similar to the uninfected cells. Persistent infection was confirmed by removing supernatants, centrifuging cellular debris (400 × g for 10 min), and transferring the cells to uninfected Vero E6 cells for virus titration using either a FFU or TCID50 assay.
Persistently infected cells were subjected to no treatment; changed media; PMA at concentrations of 0, 6.25, 25, or 50 ng/ml in dimethyl sulfoxide (DMSO); DMSO alone (as a diluent control), or LPS from Escherichia coli O111:B4 (Sigma-Aldrich) at concentrations of 0, 0.1, 1.0, or 10 ng/ml in complete DMEM with 10% FBS, as noted in the figures. All samples were harvested for assessment at 24 h posttreatment.
Radiolabeling of Cells and Preparation of Lysates.
Cells were labeled in methionine-free DMEM containing 10% dialyzed FBS with 0.1 mCi/ml of [35S] methionine/cysteine protein labeling mixture (Perkin Elmer). After further incubation for 24 h at 37 °C, the cells were washed in phosphate-buffered saline (PBS) and lysed in the same buffer containing 1% Triton X-100, 0.5% sodium deoxycholate, and 1 mM EDTA. The supernatants were stored at −80 °C until use. Radiolabeled lysates were analyzed by discontinuous 10% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and visualized by autoradiography with a phosphoimager.
Immunofluorescence Analysis.
NIH 3T3, TNIH#5, H-Ras, and THC-11 cells were grown on coverslips and then infected with ZEBOV strain Mayinga at a MOI of ≈0.2 or mock-infected. At 48 h postinfection, cells were fixed in 10% phosphate-buffered formalin for >24 h, followed by a change of 10% phosphate-buffered formalin, then heat-sealing in a plastic pouch and submersion in 5% MicroChem solution (MicroChem Corp.), after which the samples were removed from the BSL-4 laboratory. The plates were stored in the formalin solution for another 24 h at 4 °C, followed by four washes with PBS. The fixed cells were then solublized in 0.1% Triton X-100 for 10–15 min at room temperature, washed another three times in PBS, and then exposed to the primary antibody (mouse monoclonal anti-VP40) (59) diluted 1:800 in PBS for 2 h at room temperature. After three washes with PBS, the cells were exposed to the secondary antibody [goat anti-mouse IgG (whole molecule)-fluorescein isothiocyanate (FITC) conjugate; Sigma-Aldrich] diluted 1/250 in PBS containing 10% goat serum for 1 h at room temperature. Finally, the fixed and treated cells were washed three more times with PBS and then once with double-distilled water, dried, mounted on slides in 90% glycerol, and viewed with a Zeiss Axiophot microscope on which a Zeiss camera was mounted. The magnification for all panels was × 200.
In Vitro Kinase, Immunoprecipitation, and Western Blot Analysis.
Confluent monolayers of the various cell lines were grown on 24-well cell culture plates. At 48 h postinfection, the medium was aspirated off, and the cells were lysed with a buffer containing 20 mM Hepes (pH 7.4), 120 mM KCl, 5 mM MgCl2, 1 mM dithiothreitol, 0.5% Nonidet P-40, 2 μg/ml of leupeptin, and 50 μg/ml of aprotinin. The supernatants were stored at −80 °C until use. Each in vitro kinase reaction contained 20 μl of cell extract, 7.5 μl of reaction buffer (20 mM Hepes [pH 7.4], 120 mM KCl, 5 mM MgCl2, 1 mM dithiothreitol, and 10% glycerol), and 7.0 μl of adenosine 5′-triphosphate (ATP) mixture (1.0 μCi of [γ-33P]ATP in 7 μl of reaction buffer) and was incubated for 30 min at 37 °C. Immediately after incubation, the labeled extracts were either boiled for 10 min in Laemmli SDS sample buffer or were immunoprecipitated with an anti-PKR antibody (Santa Cruz Biotechnology). Immunoprecipitation of 33P-labeled cell lysates with 1 μg of the anti-PKR antibody per 100 μl of lysate was carried out using the Protein G Immunoprecipitation Kit (Sigma-Aldrich). All samples were analyzed by discontinuous 10% SDS–PAGE, autoradiography, and phosphoimaging.
For Western blot analysis, protein samples were subjected to 10% SDS-PAGE and transferred to poly(vinylidene difluoride) membranes (Millipore). The membrane was blocked with 5% skim milk in Tris-buffered saline (20 mM Tris and 137 mM NaCl, pH 7.3) containing 0.1% Tween 20, and then incubated with the primary antibody anti-eIF2α or anti-phospho(Ser 52)-eIF2α (both from Santa Cruz Biotechnology). After washing, the membrane was incubated with peroxidase-conjugated goat anti-mouse IgG or anti-rabbit IgG (Santa Cruz Biotechnology). Specific bands were detected by enhanced chemiluminescence (Amersham) in accordance with the manufacturer's specifications.
Polymerase Chain Reaction.
Viral RNA was isolated from RAWZEBOV/GFPpi cells after 24 h of treatment with changed complete media (DMEM containing 10% FBS, 2 mmol/L L-glutamine, 100 U/ml of penicillin, and 100 μg/ml of streptomycin), complete medium containing DMSO, complete medium containing 10 ng/ml of LPS, complete medium containing 50 ng/ml of PMA, or no treatment. RNA was isolated from these tissue culture samples by releasing cells from adherence with 0.25% Trypsin/EDTA for 10 min at 37 °C, with subsequent extraction using the QIAamp Viral RNA Mini Kit (Qiagen). ZEBOV RNA was detected using primer pairs targeting the ZEBOV GP gene as follows: Forward primer, 5′-GGCCAACGAGACGACTCAA-3′; reverse primer, 5′-AAAGGTGCGTAGCTCAGTTGTG-3′; and probe, 6FAM -CTCTTCAACTGTTCCTGAGAG - MGBNFQ using the LightCycler 480 RNA Master hydrolysis probe (Roche Diagnostics). All samples were run on the Smart Cycler (ABI Biosystems) through quantitative RT-PCR with cycling conditions as follows: reverse transcription at 63 °C for 120 seconds, activation at 95 °C for 30 seconds, 45 cycles of denaturation at 95 °C for 15 seconds, and annealing/extension at 60 °C for 30 seconds. All samples were quantified by running against known serially diluted samples extracted and run as above. The limit of sensitivity of the ZEBOV GP-specific quantitative RT-PCR is ≈0.1 FFU/ml.
Animal Experiments.
Female BALB/c mice age 5–6 weeks were obtained from a commercial supplier (Charles River Laboratories). All mice were housed in microisolator cages in BSL4 and allowed to acclimatize for at least 5 days before use in experiments. 5 female BALB/c mice were infected via i.p. injection with either ZEBOV/GFP (1000 FFU in 200 μl DMEM) or MA-ZEBOV (1000 FFU in 200 μl of DMEM), or mock infected then allowed to incubate for 6 days, followed by i.p. injection of 200 μl of DMEM containing 100 ng/ml of PMA or an equivalent amount of DMSO (diluent for PMA). Mice were euthanized 24 h later. Their organs were harvested (liver, spleen, and blood), and FFU assays were performed on the serially diluted homogenates. Mock-infected mice were treated similarly and served as negative controls.
All work with live ZEBOV was performed in the BSL-4 laboratory of the National Microbiology Laboratory, Public Health Agency of Canada. All animal experiments were performed in accordance with approved animal use documents and according to the guidelines of the Canadian Council on Animal Care.
Acknowledgments.
We thank Mike Bray and Hideki Ebihara for their helpful discussions and critical reading of the manuscript. We thank Ayato Takada for the anti-VP40 antibody, Douglas Faller for the NIH 3T3 cells and H-Ras–transformed cells, Michael Karin for the SOS-transformed cells (TNIH#5), and H.-J. Kung for the v-erbB-transformed cells (THC-11). The filovirus research done at the National Microbiology Laboratory was supported by the Public Health Agency of Canada.
Footnotes
The authors declare no conflict of interest.
References
- 1.Bausch DG, Geisbert TW. Development of vaccines for Marburg hemorrhagic fever. Expert Rev Vaccines. 2007;6:57–74. doi: 10.1586/14760584.6.1.57. [DOI] [PubMed] [Google Scholar]
- 2.Paragas J, Geisbert TW. Development of treatment strategies to combat Ebola and Marburg viruses. Expert Rev Anti Infect Ther. 2006;4:67–76. doi: 10.1586/14787210.4.1.67. [DOI] [PubMed] [Google Scholar]
- 3.Feldmann H, Jones SM, Schnittler HJ, Geisbert T. Therapy and prophylaxis of Ebola virus infections. Curr Opin Investig Drugs. 2005;6:823–830. [PubMed] [Google Scholar]
- 4.Geisbert TW, Jahrling PB. Towards a vaccine against Ebola virus. Expert Rev Vaccines. 2003;2:777–789. doi: 10.1586/14760584.2.6.777. [DOI] [PubMed] [Google Scholar]
- 5.Feldmann H, Jones S, Klenk HD, Schnittler HJ. Ebola virus: From discovery to vaccine. Nat Rev Immunol. 2003;3:677–685. doi: 10.1038/nri1154. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan N, Yang ZY, Nabel GJ. Ebola virus pathogenesis: Implications for vaccines and therapies. J Virol. 2003;77:9733–9737. doi: 10.1128/JVI.77.18.9733-9737.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swanepoel R, et al. Experimental inoculation of plants and animals with Ebola virus. Emerg Infect Dis. 1996;2:321–325. doi: 10.3201/eid0204.960407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breman JG, et al. A search for Ebola virus in animals in the Democratic Republic of the Congo and Cameroon: Ecologic, virologic, and serologic surveys, 1979–1980. Ebola Virus Study Teams. J Infect Dis. 1999;179(Suppl 1):S139–S147. doi: 10.1086/514278. [DOI] [PubMed] [Google Scholar]
- 9.Reiter P, et al. Field investigations of an outbreak of Ebola hemorrhagic fever, Kikwit, Democratic Republic of the Congo, 1995: Arthropod studies. J Infect Dis. 1999;179(Suppl 1):S148–S154. doi: 10.1086/514304. [DOI] [PubMed] [Google Scholar]
- 10.Leirs H, et al. Search for the Ebola virus reservoir in Kikwit, Democratic Republic of the Congo: Reflections on a vertebrate collection. J Infect Dis. 1999;179(Suppl 1):S155–S163. doi: 10.1086/514299. [DOI] [PubMed] [Google Scholar]
- 11.HCaPRW Group. WHO-led collaborative study in Cote D'Ivoire to identify the natural host reservoir of the Ebola virus. Press release WHO/93. 1995 http://www.who.int/archives/inf-pr-1995/pr95-93.html.
- 12.Morvan JM, et al. Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic. Microbes Infect. 1999;1:1193–1201. doi: 10.1016/s1286-4579(99)00242-7. [DOI] [PubMed] [Google Scholar]
- 13.Gunther S, Lenz O. Lassa virus. Crit Rev Clin Lab Sci. 2004;41:339–390. doi: 10.1080/10408360490497456. [DOI] [PubMed] [Google Scholar]
- 14.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1998;178:651–661. doi: 10.1086/515386. [DOI] [PubMed] [Google Scholar]
- 15.Bray M. The role of the type I interferon response in the resistance of mice to filovirus infection. J Gen Virol. 2001;82:1365–1373. doi: 10.1099/0022-1317-82-6-1365. [DOI] [PubMed] [Google Scholar]
- 16.Warfield KL, et al. Role of natural killer cells in innate protection against lethal Ebola virus infection. J Exp Med. 2004;200:169–179. doi: 10.1084/jem.20032141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warfield KL, et al. Development of a model for Marburg virus based on severe combined immunodeficiency mice. Virol J. 2007;4:108–121. doi: 10.1186/1743-422X-4-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Connolly BM, et al. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis. 1999;179(Suppl 1):S203–S217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- 19.Ebihara H, et al. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2006;2 doi: 10.1371/journal.ppat.0020073. 0705–0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leroy EM, et al. Fruit bats as reservoirs of Ebola virus. Nature. 2005;438:575–576. doi: 10.1038/438575a. [DOI] [PubMed] [Google Scholar]
- 21.Towner JS, et al. Marburg virus infection detected in a common African bat. PLoS ONE. 2007;2:1–5. doi: 10.1371/journal.pone.0000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swanepoel R, et al. Studies of reservoir hosts for Marburg virus. Emerg Infect Dis. 2007;13:1847–1851. doi: 10.3201/eid1312.071115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ebihara H, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis. 2007;196(Suppl 2):S313–S322. doi: 10.1086/520590. [DOI] [PubMed] [Google Scholar]
- 24.Tan CT, et al. Relapsed and late-onset Nipah encephalitis. Ann Neurol. 2002;51:703–708. doi: 10.1002/ana.10212. [DOI] [PubMed] [Google Scholar]
- 25.Ellenberg P, Linero FN, Scolaro LA. Superinfection exclusion in BHK-21 cells persistently infected with Junin virus. J Gen Virol. 2007;88:2730–2739. doi: 10.1099/vir.0.83041-0. [DOI] [PubMed] [Google Scholar]
- 26.Meyer BJ, Schmaljohn CS. Persistent hantavirus infections: characteristics and mechanisms. Trends Microbiol. 2000;8:61–67. doi: 10.1016/s0966-842x(99)01658-3. [DOI] [PubMed] [Google Scholar]
- 27.Rima BK, Duprex WP. Molecular mechanisms of measles virus persistence. Virus Res. 2005;111:132–147. doi: 10.1016/j.virusres.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 28.Martinez-Sobrido L, Zuniga EI, Rosario D, Garcia-Sastre A, de la Torre JC. Inhibition of the type I interferon response by the nucleoprotein of the prototypic arenavirus lymphocytic choriomeningitis virus. J Virol. 2006;80:9192–9199. doi: 10.1128/JVI.00555-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodriguez LL, et al. Persistence and genetic stability of Ebola virus during the outbreak in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179(Suppl 1):S170–S176. doi: 10.1086/514291. [DOI] [PubMed] [Google Scholar]
- 30.Okada Y, et al. Viral activation from latency during retrodifferentiation of U937 cells exposed to phorbol ester followed by infection with human immunodeficiency virus type 1. Immunopharmacology. 1995;30:27–39. doi: 10.1016/0162-3109(95)98646-k. [DOI] [PubMed] [Google Scholar]
- 31.Ford PW, et al. Raf/MEK/ERK signaling triggers reactivation of Kaposi's sarcoma–associated herpesvirus latency. J Gen Virol. 2006;87:1139–1144. doi: 10.1099/vir.0.81628-0. [DOI] [PubMed] [Google Scholar]
- 32.Smith RL, Pizer LI, Johnson EM, Jr, Wilcox CL. Activation of second-messenger pathways reactivates latent herpes simplex virus in neuronal cultures. Virology. 1992;188:311–318. doi: 10.1016/0042-6822(92)90760-m. [DOI] [PubMed] [Google Scholar]
- 33.Strong JE, Coffey MC, Tang D, Sabinin P, Lee PW. The molecular basis of viral oncolysis: Usurpation of the Ras signaling pathway by reovirus. EMBO J. 1998;17:3351–3362. doi: 10.1093/emboj/17.12.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mundschau LJ, Faller DV. Oncogenic ras induces an inhibitor of double-stranded RNA-dependent eukaryotic initiation factor 2 alpha-kinase activation. J Biol Chem. 1992;267:23092–23098. [PubMed] [Google Scholar]
- 35.Farassati F, Yang AD, Lee PW. Oncogenes in Ras signaling pathway dictate host cell permissiveness to herpes simplex virus 1. Nat Cell Biol. 2001;3:745–750. doi: 10.1038/35087061. [DOI] [PubMed] [Google Scholar]
- 36.Battcock SM, Collier TW, Zu D, Hirasawa K. Negative regulation of the alpha interferon–induced antiviral response by the Ras/Raf/MEK pathway. J Virol. 2006;80:4422–4430. doi: 10.1128/JVI.80.9.4422-4430.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang JS, Feng WG, Li CL, Wang XY, Chang ZL. NF-kappa B regulates the LPS-induced expression of interleukin 12 p40 in murine peritoneal macrophages: Roles of PKC, PKA, ERK, p38 MAPK, and proteasome. Cell Immunol. 2000;204:38–45. doi: 10.1006/cimm.2000.1690. [DOI] [PubMed] [Google Scholar]
- 38.Lucchi NW, Moore JM. LPS induces secretion of chemokines by human syncytiotrophoblast cells in a MAPK-dependent manner. J Reprod Immunol. 2007;73:20–27. doi: 10.1016/j.jri.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 39.Marquardt B, Frith D, Stabel S. Signaling from TPA to MAP kinase requires protein kinase C, raf and MEK: Reconstitution of the signaling pathway in vitro. Oncogene. 1994;9:3213–3218. [PubMed] [Google Scholar]
- 40.Li C, et al. Both ERK and JNK pathways are required for PMA-induced MD-2 gene expression during HL-60 cell differentiation. Biol Cell. 2008;100(6):365–375. doi: 10.1042/BC20070140. [DOI] [PubMed] [Google Scholar]
- 41.Emeny JM, Morgan MJ. Regulation of the interferon system: Evidence that Vero cells have a genetic defect in interferon production. J Gen Virol. 1979;43:247–252. doi: 10.1099/0022-1317-43-1-247. [DOI] [PubMed] [Google Scholar]
- 42.Desmyter J, Melnick JL, Rawls WE. Defectiveness of interferon production and of rubella virus interference in a line of African green monkey kidney cells (Vero) J Virol. 1968;2:955–961. doi: 10.1128/jvi.2.10.955-961.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mundschau LJ, Faller DV. Endogenous inhibitors of the dsRNA-dependent eIF-2 alpha protein kinase PKR in normal and ras-transformed cells. Biochimie. 1994;76:792–800. doi: 10.1016/0300-9084(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 44.Thomis DC, Samuel CE. Mechanism of interferon action: Characterization of the intermolecular autophosphorylation of PKR, the interferon-inducible, RNA-dependent protein kinase. J Virol. 1995;69:5195–5198. doi: 10.1128/jvi.69.8.5195-5198.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou Y, Chase BI, Whitmore M, Williams BR, Zhou A. Double-stranded RNA-dependent protein kinase (PKR) is downregulated by phorbol ester. FEBS J. 2005;272:1568–1576. doi: 10.1111/j.1742-4658.2005.04572.x. [DOI] [PubMed] [Google Scholar]
- 46.Calain P, Monroe MC, Nichol ST. Ebola virus defective interfering particles and persistent infection. Virology. 1999;262:114–128. doi: 10.1006/viro.1999.9915. [DOI] [PubMed] [Google Scholar]
- 47.Gupta M, et al. Persistent infection with Ebola virus under conditions of partial immunity. J Virol. 2004;78:958–967. doi: 10.1128/JVI.78.2.958-967.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martini GA. Marburg agent disease in man. Trans R Soc Trop Med Hyg. 1969;63:295–302. doi: 10.1016/0035-9203(69)90001-7. [DOI] [PubMed] [Google Scholar]
- 49.Smith DH, et al. Marburg virus disease in Kenya. Lancet. 1982;319:816–820. doi: 10.1016/s0140-6736(82)91871-2. [DOI] [PubMed] [Google Scholar]
- 50.Emond RT, Evans B, Bowen ET, Lloyd G. A case of Ebola virus infection. BMJ. 1977;2:541–544. doi: 10.1136/bmj.2.6086.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bausch DG, et al. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis. 2007;196(Suppl 2):S142–S147. doi: 10.1086/520545. [DOI] [PubMed] [Google Scholar]
- 52.Groseth A, Feldmann H, Strong JE. The ecology of Ebola virus. Trends Microbiol. 2007;15:408–416. doi: 10.1016/j.tim.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 53.Sadiq ST, et al. The effects of early syphilis on CD4 counts and HIV-1 RNA viral loads in blood and semen. Sex Transm Infect. 2005;81:380–385. doi: 10.1136/sti.2004.012914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McCullers JA. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006;19:571–582. doi: 10.1128/CMR.00058-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slots J. Herpesviral–bacterial synergy in the pathogenesis of human periodontitis. Curr Opin Infect Dis. 2007;20:278–283. doi: 10.1097/QCO.0b013e3280964da0. [DOI] [PubMed] [Google Scholar]
- 56.Williamson MM, Hooper PT, Selleck PW, Westbury HA, Slocombe RF. Experimental Hendra virus infection in pregnant guinea pigs and fruit bats (Pteropus poliocephalus) J Comp Pathol. 2000;122:201–207. doi: 10.1053/jcpa.1999.0364. [DOI] [PubMed] [Google Scholar]
- 57.Field H, et al. The natural history of Hendra and Nipah viruses. Microbes Infect. 2001;3:307–314. doi: 10.1016/s1286-4579(01)01384-3. [DOI] [PubMed] [Google Scholar]
- 58.Yadav VK, Medhamurthy R. Dynamic changes in mitogen-activated protein kinase (MAPK) activities in the corpus luteum of the bonnet monkey (Macaca radiata) during development, induced luteolysis, and simulated early pregnancy: A role for p38 MAPK in the regulation of luteal function. Endocrinology. 2006;147:2018–2027. doi: 10.1210/en.2005-1372. [DOI] [PubMed] [Google Scholar]
- 59.Noda T, et al. Ebola virus VP40 drives the formation of virus-like filamentous particles along with GP. J Virol. 2002;76:4855–4865. doi: 10.1128/JVI.76.10.4855-4865.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]