Abstract
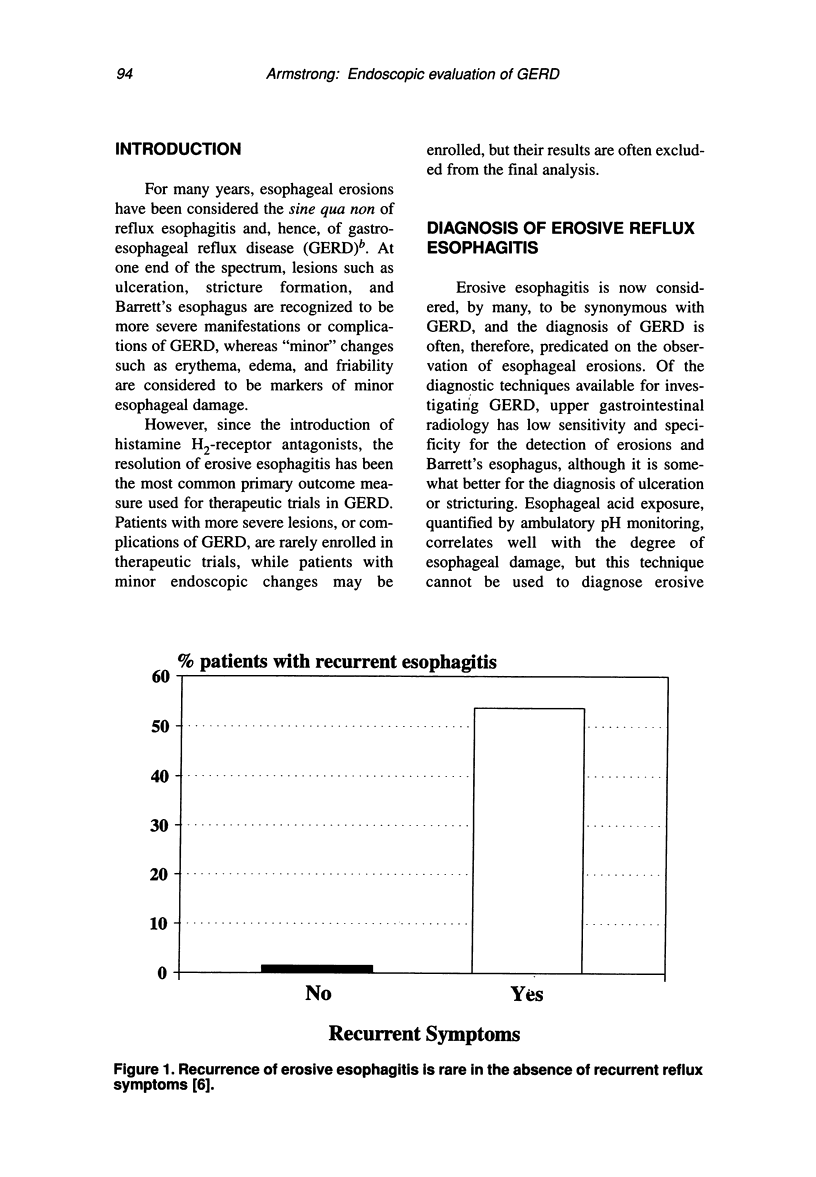
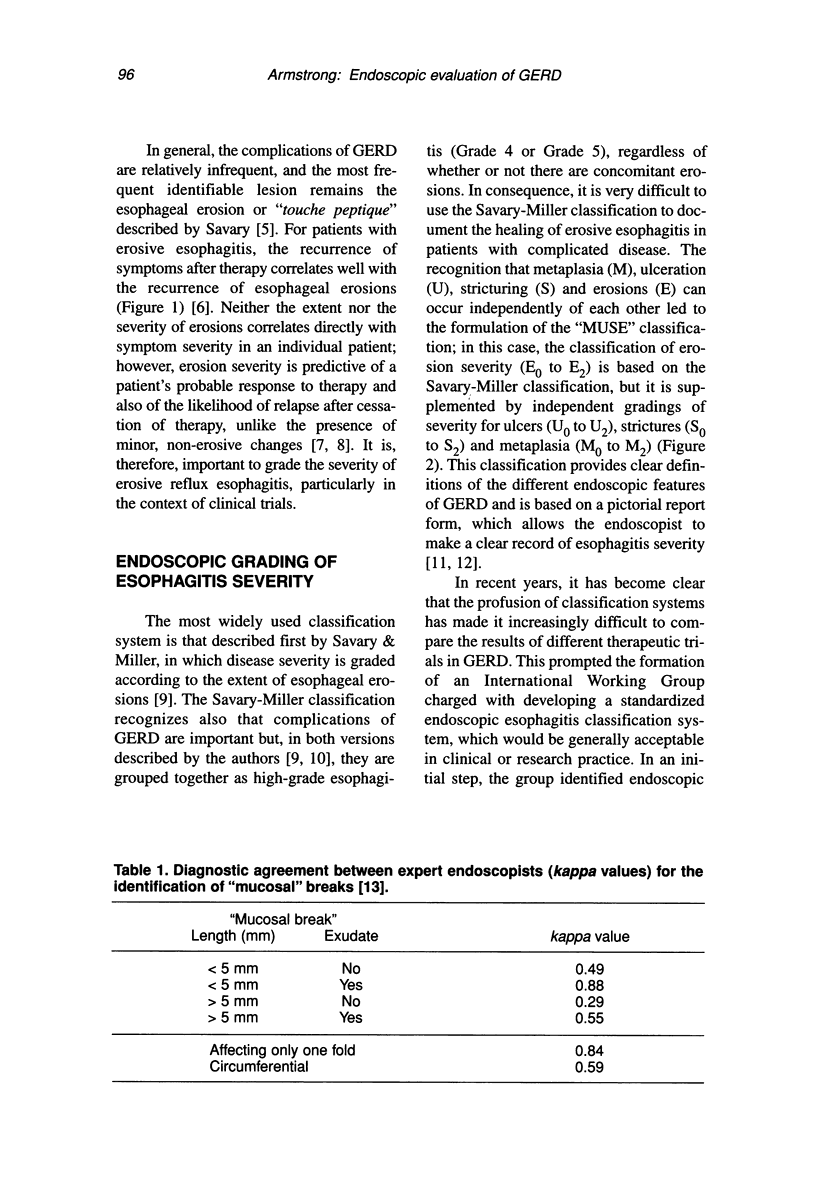
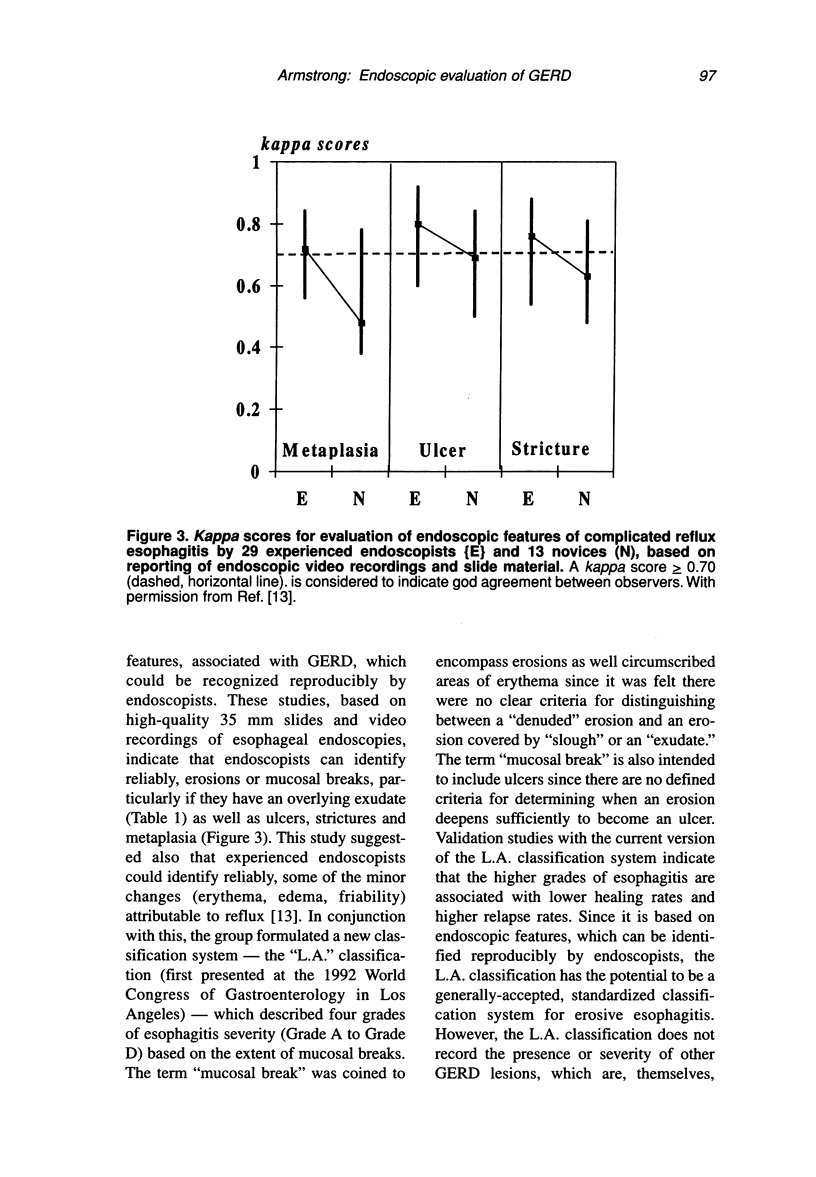
Endoscopy is, currently, the initial investigation of choice for the investigation of gastroesophageal reflux disease (GERD) in clinical practice and clinical research. Erosion severity is predictive of a patient's response to therapy and of the likelihood of relapse after therapy. It is, therefore, important to grade the severity of erosive reflux esophagitis, particularly in the context of clinical trials. The Savary-Miller endoscopic classification system is used widely but usage and interpretation are very variable. The "MUSE" (metaplasia [M], ulceration [U], stricturing [S] and erosions [E]) classification provides clear definitions of the relevant endoscopic features, and it is based on a standardized report form, which allows the endoscopist to make a clear record of esophagitis severity. Recent studies confirm that endoscopists can identify erosions or mucosal breaks, ulcers, strictures, and metaplasia reproducibly. The "L.A." (Los Angeles) classification describes four grades of esophagitis severity (A to D), based on the extent of esophageal lesions known as "mucosal breaks," but it does not record the presence or severity of other GERD lesions. Thus, for patients with "complicated" reflux disease, the "MUSE" classification offers a more comprehensive description of esophagitis severity. Endoscopy is not universally applicable: 40 to 60 percent of patients with typical reflux symptoms do not have esophageal erosions and are now considered to have "endoscopy negative reflux disease" (ENRD). Thus, endoscopy is not the final arbiter as to a diagnosis of reflux disease, and it is not, therefore, a necessary prerequisite to therapy. Endoscopy is indicated at first presentation for patients with alarm symptoms referable to the upper gastrointestinal tract. It has also been proposed that all patients with chronic GERD should have a "once-in-a-lifetime" endoscopy; in the absence of Barrett's esophagus or other complications, no follow-up is required unless the patient's symptoms change significantly. A surveillance program with multiple biopsies should be instituted if there is evidence of Barrett's esophagus. Endoscopic evaluation should document the presence and extent of esophageal erosions using the L.A. or MUSE classification systems; complications should also be documented and may be recorded using the MUSE classification. Non-erosive changes such as erythema may be ignored on the basis of present evidence, and there are no clear data to support the use of endoscopic biopsies for the diagnosis of GERD.
Full text
PDF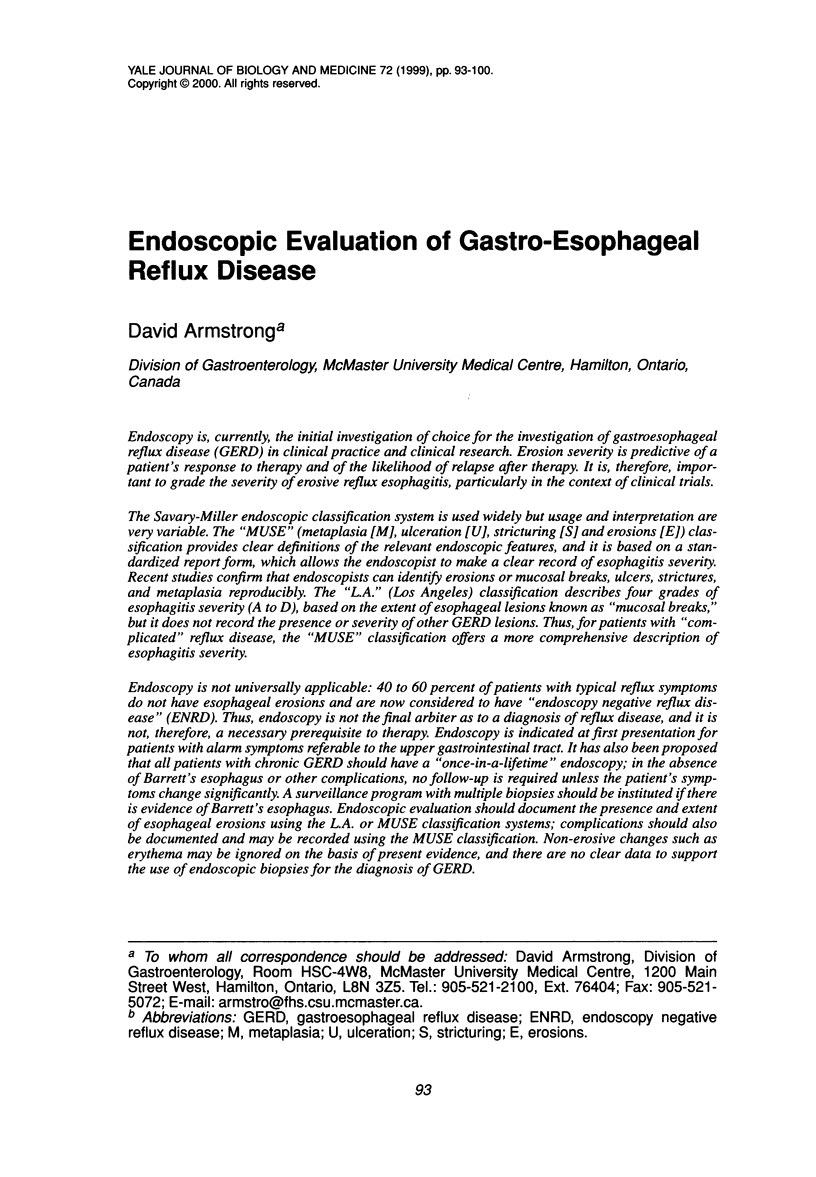
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armstrong D., Bennett J. R., Blum A. L., Dent J., De Dombal F. T., Galmiche J. P., Lundell L., Margulies M., Richter J. E., Spechler S. J. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996 Jul;111(1):85–92. doi: 10.1053/gast.1996.v111.pm8698230. [DOI] [PubMed] [Google Scholar]
- Blum A. L., Adami B., Bouzo M. H., Brandstätter G., Fumagalli I., Galmiche J. P., Hebbeln H., Hentschel E., Hüttemann W., SChütz E. Effect of cisapride on relapse of esophagitis. A multinational, placebo-controlled trial in patients healed with an antisecretory drug. The Italian Eurocis Trialists. Dig Dis Sci. 1993 Mar;38(3):551–560. doi: 10.1007/BF01316514. [DOI] [PubMed] [Google Scholar]
- Cameron A. J., Lomboy C. T. Barrett's esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992 Oct;103(4):1241–1245. doi: 10.1016/0016-5085(92)91510-b. [DOI] [PubMed] [Google Scholar]
- Ellis K. K., Oehlke M., Helfand M., Lieberman D. Management of symptoms of gastroesophageal reflux disease: does endoscopy influence medical management? Am J Gastroenterol. 1997 Sep;92(9):1472–1474. [PubMed] [Google Scholar]
- Ismail-Beigi F., Horton P. F., Pope C. E., 2nd Histological consequences of gastroesophageal reflux in man. Gastroenterology. 1970 Feb;58(2):163–174. [PubMed] [Google Scholar]
- Jessurun J., Yardley J. H., Giardiello F. M., Hamilton S. R. Intracytoplasmic plasma proteins in distended esophageal squamous cells (balloon cells). Mod Pathol. 1988 May;1(3):175–181. [PubMed] [Google Scholar]
- Leu H., Schüle A., Brändli H., Pelloni S., Blum L. Glanzverlust, Farbveränderungen und erhöhte Lädierbarkeit der Speiseröhre: altersbedingte Normvarianten? Z Gastroenterol. 1978 Jul;16(7):417–421. [PubMed] [Google Scholar]
- Provenzale D., Kemp J. A., Arora S., Wong J. B. A guide for surveillance of patients with Barrett's esophagus. Am J Gastroenterol. 1994 May;89(5):670–680. [PubMed] [Google Scholar]
- Schüle A., Brändli H., Pelloni S., Koelz H. R., Pirozynski W. J., Blum A. L. Endoskopische Diagnose der Osophagitis Wo liegt die Grenze zum Normalen. Dtsch Med Wochenschr. 1977 Apr 22;102(16):606–609. doi: 10.1055/s-0028-1104940. [DOI] [PubMed] [Google Scholar]
- Seefeld U., Krejs G. J., Siebenmann R. E., Blum A. L. Esophageal histology in gastroesophageal reflux. Morphometric findings in suction biopsies. Am J Dig Dis. 1977 Nov;22(11):956–964. doi: 10.1007/BF01076193. [DOI] [PubMed] [Google Scholar]
- Weinstein W. M., Bogoch E. R., Bowes K. L. The normal human esophageal mucosa: a histological reappraisal. Gastroenterology. 1975 Jan;68(1):40–44. [PubMed] [Google Scholar]



