Abstract
A modified version of the Revised Memory and Behavior Problems Checklist (RMBPC; L. Teri et al., 1992) was administered across 6 different sites to 1,229 family caregivers of community-dwelling adults with dementia. The total sample was divided randomly into 2 subsamples. Principal components analyses on occurrence responses and reaction ratings from the first subsample resulted in a 3-factor solution that closely resembled the originally proposed dimensions (memory-related problems, disruptive behaviors, and depression). Confirmatory factor analyses on data from the second subsample indicated adequate fit for the 3-factor model. Correlations with other caregiver and care-recipient measures supported the convergent and discriminant validity of the RMBPC measures. In addition, female caregivers and White caregivers reported more problems, on average, than male caregivers and African American caregivers, respectively.
It has been estimated that 80% of individuals with Alzheimer’s disease or a similar dementia are cared for at home by family members (Haley & Bailey, 1999). Although dementia is, by definition, characterized by a decline in cognitive functions, other behavioral complications such as emotional disturbances and disruptive behaviors are also common. Standardized instruments that assess the occurrence and severity of cognitive, emotional, and behavioral problems exhibited by persons with dementia are helpful not only for assessing behavior disturbance in Alzheimer’s disease but also for identifying the specific challenges that confront family caregivers.
The Revised Memory and Behavior Problems Checklist (RMBPC; Teri et al., 1992) is one such instrument that provides assessments of the frequency of problems and the impact that these problems have on the caregiver. Exploratory factor analyses of the RMBPC and similar measures of memory and behavior problems have indicated that multiple dimensions underlie these measures (Dura, Bornstein, & Kiecolt-Glaser, 1990; Fuh, Liu, Wang, Wang, & Liu, 1999; McCarty et al., 2000; Teri et al., 1992). In general, memory-related problems have been found to cluster on distinct factors that are largely independent from emotional difficulties and other behavior problems. However, significant inconsistencies across previous studies are evident, both in terms of item content and resulting factor structures. Factor structures with as few as three (Fuh et al., 1999; Teri et al., 1992) and as many as eight (Dura et al., 1990) different factors have been reported.
In constructing the RMBPC, Teri and colleagues (1992) expanded from a list of items previously used by Zarit and Zarit (1983) and assembled a set of 64 items. These items were then administered to 169 caregivers of patients diagnosed with dementia and 32 caregivers of geriatric patients without a diagnosis of dementia. For each item, caregivers rated the frequency of the problem on a 0 (never) to 4 (daily or more often) scale, and for any problems that occurred at least once per week, caregivers also rated how much this problem “bothered or upset” the caregiver on a 0 (not at all) to 4 (extremely) scale. After the data were collected, the item pool was reduced by (a) eliminating 17 items that were not reliably classified by licensed psychologists as being in one of three hypothesized content areas: memory-related problems, depression, or disruptive behaviors; (b) eliminating 19 items that did not load significantly on one of the first six rotated factors from an initial principal components analysis on the frequency ratings; and (c) eliminating 4 items that did not load significantly on one of the first three rotated factors from a second principal components analysis on the same data. This left 24 items that provided assessments of the three content domains that were targeted.
Although one subsequent study found a similar three-factor model following principal components analysis (Fuh et al., 1999), additional work is needed to evaluate the factor structure underlying this instrument. Some studies have proceeded to examine subscales for both frequency and reaction data (e.g., Weiner et al., 2000), even though all previous factor analytic studies of the RMBPC and related instruments have been restricted to analyses of frequency ratings only. At present, the factor structure and psychometric properties of the reaction ratings are unknown. Furthermore, some investigators have used modifications of the RMBPC that have replaced frequency ratings with simple occurrence responses in which caregivers are asked only whether a particular problem occurred in the past week (Gitlin et al., 2003; Wagner, Teri, & Orr-Rainey, 1995). It is not known whether these occurrence responses will show similar psychometric properties to those displayed by the frequency ratings. Finally, all previous factor analyses of the RMBPC and related instruments have implemented exploratory factor analysis methods. Through confirmatory factor analysis methods, it should be possible to evaluate the fit of the three-factor model and to compare it to competing models.
The purpose of the present study was to obtain an independent evaluation of the factor structure underlying the 24-item RMBPC and to extend this psychometric work to simple occurrence responses and caregiver ratings of perceived burden. A modified version of the RMBPC was administered to 1,229 family caregivers as part of the National Institutes of Health multisite initiative, Resources for Enhancing Alzheimer’s Caregiver Health (REACH; Coon, Schulz, & Ory, 1999; Gitlin et al., 2003; Wisniewski et al., 2003). Because of the large size of the overall REACH sample, we randomly divided the data into exploratory and confirmatory sub-samples for factor analytic purposes. After the optimal factor structure was identified, subscales were created and the convergent and discriminant validity of the subscales were examined. RMBPC measures were not expected to vary significantly as a function of care-recipient age. Measures of caregiver depression and the amount of time spent providing care were expected to correlate positively with RMBPC measures, especially those involving reaction ratings. Conversely, small negative correlations were expected between RMBPC measures and indices of leisure time satisfaction and positive aspects of caregiving. An objective measure of care-recipient cognitive status was obtained, and this measure was expected to show an inverted, ∪-shaped, curvilinear relationship with RMBPC memory-related measures. Curvilinear associations between the frequency of memory problems and objective cognitive status have been found previously (McCarty et al., 2000), although significant negative linear correlations have also been reported (Dura et al., 1990; Teri et al., 1992). Finally, we sought to identify any gender or racial differences on the RMBPC measures in this large multisite sample.
Method
Participants
The participants in this study consisted of 1,229 family caregivers of individuals with dementia. These caregivers provided baseline data as part of the REACH initiative. REACH is a multisite program sponsored by the National Institute on Aging and the National Institute for Nursing Research that funded six intervention sites and a coordinating center to develop interventions for family caregivers of individuals with a moderate level of cognitive impairment. Participants from all six intervention sites provided data for the analyses reported in this article (Birmingham, AL: N = 140; Boston: N = 100; Memphis, TN: N = 245; Miami, FL: N = 225; Palo Alto, CA: N = 264; Philadelphia: N = 255). All data were sent to a coordinating center at the University of Pittsburgh where they were verified for accuracy and organized into suitable files for analysis. The coordinating center also conducted site visits to ensure adherence to study protocols and to confirm the exclusive use of trained and certified research interviewers.
Caregiver/care-recipient dyads were recruited from multiple community sites and social service agencies. More detailed information about the recruitment procedures and the interventions tested at each site are reported elsewhere (Coon et al., 1999; Gitlin et al., 2003; Wisniewski et al., 2003). In this article, the results of psychometric analyses are reported for the RMBPC data that were obtained at the baseline evaluation before any interventions were administered.
All caregivers were 21 years of age or older and identified themselves as the primary caregiver for a family member with Alzheimer’s disease or a related dementia (ADRD). The mean age of the caregivers was 62.19 years (SD = 13.64). The sample consisted of 1,001 (81.4%) female caregivers and 228 (18.6%) male caregivers. Both sexes were recruited at all sites except Palo Alto, where only female caregivers were enrolled. Caregiver relationship to the care recipient was varied, with 590 spouses (48%), 544 children (44%), and 95 other relatives (8%) serving as caregivers.
Care recipients were required to be community-dwelling older adults with a medical diagnosis of probable ADRD or a score of 23 or less on the Mini-Mental State Exam (MMSE; Folstein, Folstein, & McHugh, 1975). The mean age of the care recipients was 79.15 years (SD = 8.23), and 681 (55.4%) of the care recipients were women.
Large samples of racial and ethnic minorities were obtained in the REACH project. The sample included 679 (55.2%) caregiver/care-recipient dyads in which both partners were White, 293 (23.8%) dyads where both partners were African American, and 218 (17.7%) dyads where both partners were Hispanic. The remaining 39 (3.2%) dyads were of other racial/ethnic classifications or interracial relationships.
We randomly divided the total sample of 1,229 caregiver/care-recipient dyads into two independent subsamples prior to factor analysis using the random sampling procedures of SPSS. Table 1 contains descriptive data for both subsamples. The two subsamples did not differ significantly on any demographic variables or RMBPC measures.
Table 1.
Demographic Comparisons of Random Subsamples
| Subsample 1 (N = 615)
|
Subsample 2 (N = 614)
|
||||
|---|---|---|---|---|---|
| Variable | M | SD | M | SD | pa |
| CR age | 78.62 | 8.13 | 78.67 | 8.33 | .93 |
| CR MMSE | 12.69 | 7.70 | 12.52 | 7.59 | .71 |
| RMBPC (# of problems) | 10.13 | 4.14 | 10.29 | 4.18 | .49 |
| RMBPC (mean reaction per problem) | 1.50 | 0.91 | 1.47 | 0.91 | .56 |
| RMBPC (total reaction) | 16.49 | 13.68 | 16.97 | 13.61 | .54 |
|
| |||||
| N | % | N | % | pb | |
|
|
|||||
| Race | .97 | ||||
| White | 338 | 55 | 341 | 56 | |
| African American | 147 | 24 | 146 | 24 | |
| Hispanic | 109 | 18 | 109 | 18 | |
| Other | 21 | 3 | 18 | 3 | |
| CG gender | .19 | ||||
| Male | 123 | 20 | 105 | 17 | |
| Female | 492 | 80 | 509 | 83 | |
| CR gender | .51 | ||||
| Male | 268 | 44 | 280 | 46 | |
| Female | 347 | 56 | 334 | 54 | |
Note. CR = care recipient; MMSE = Mini-Mental State Exam; RMBPC = Revised Memory and Behavior Problems Checklist; CG = caregiver.
Independent sample t test.
Pearson chi-square test.
Procedure
Potential participants were initially interviewed at each site via telephone with a common set of screening questions. After obtaining informed consent from those who were eligible, caregivers were administered a core battery of questionnaires during a subsequent visit, usually in the caregiver’s home. Each data collection site obtained local Institutional Review Board (IRB) approval for all procedures used and for the specific interventions that were later tested at that site.
Measures
All measures used in REACH were selected with the goal of using psychometrically sound instruments that were appropriate for ethnically diverse samples (Switzer, Wisniewski, Belle, Dew, & Schulz, 1999). Preference was given to established measures, although modifications to existing instruments were sometimes made, and new instruments for specific purposes were also developed. All instruments were also made available in Spanish so that the measures could be administered to Spanish-speaking caregivers.
RMBPC
The RMBPC items that were used in REACH consisted of the same 24 items retained by Teri et al. (1992). These items inquire about problem behaviors displayed by care recipients in three content areas: memory-related problems, depression, and disruptive behaviors. A modification was made to the response format used in REACH such that instead of asking respondents to rate the frequency of each problem on a 0 (never) to 4 (daily or more often) 5-point scale, caregivers in the REACH project were simply asked to indicate whether the problem had occurred during the past week (i.e., “yes” or “no”). If the caregiver indicated that a particular problem had occurred during the past week, he or she was then asked to rate how much the problem “bothered or upset” the caregiver on the same 0 (not at all) to 4 (extremely) 5-point rating scale used by Teri et al. Three scores were calculated from these data: (a) the number of problems that occurred during the past week, (b) the average reaction rating per reported problem, and (c) the total amount of reaction reported. If no problems were reported over the past week within a certain content area, the average reaction score was coded as missing, whereas the total reaction was coded as zero. It was decided to compare these two methods of summarizing the reaction ratings because the two procedures potentially assess different constructs. The average reaction rating represents a stress appraisal process that indicates how reactive the caregiver is, on average, to any behavior problem (Haley et al., 1996). With this metric, it is possible for caregivers to have high average reaction ratings even though the number of reported problems may be relatively small. The total reaction score, on the other hand, measures the total burden or stress experienced by the caregiver. This score can be elevated through either high reaction ratings or through many problems being endorsed as occurring.
MMSE
The MMSE (Folstein et al., 1975) was administered to the care recipients by trained interviewers in order to obtain a brief assessment of general cognitive impairment. Items assess basic orientation, language, and reasoning abilities. Scores range from 0 to 30, with lower scores indicating greater cognitive decline. In the present sample, scores ranged from 0 to 29 (M = 12.61, SD = 7.64), indicating that the care recipients represented a wide range of dementia severity.
Center for Epidemiological Studies-Depression Scale (CES-D)
The CES-D (Radloff & Teri, 1986) was used as a measure of depressive symptoms of the caregivers. This instrument has been widely used in previous studies of family caregivers (e.g., Haley et al., 1996; Roth, Haley, Owen, Clay, & Goode, 2001; Schulz & Williamson, 1991). For each of the scale’s 20 items, caregivers rated the frequency of this symptom on a 0 (rarely) to 3 (most of the time) 4-point scale. Higher scores are indicative of greater depression, with a score of 16 or more considered to be clinically significant.
Leisure Time Satisfaction (LTS)
Satisfaction with time spent in leisure activities was measured with a new instrument developed by the REACH investigators. Participants were asked about six activities that are commonly listed on existing leisure measures and believed to be relevant to the dementia caregiving experience (hobbies, quiet time by yourself, church attendance, dining out or other social activities, doing fun things with others, and visiting family and friends). The caregivers were asked, “Over the past month, how satisfied are you with the amount of time you have been able to spend?” in each activity. Each item was rated on a 3-point scale (0 = not at all, 1 = a little, 2 = a lot). Ratings were summed to yield total scores that ranged from 0 to 12. Cronbach’s alpha measure of internal consistency was found to be .80 for this instrument, suggesting a high degree of reliability for the summary score.
Positive Aspects of Caregiving (PAC)
REACH investigators also developed a measure to assess positive aspects of the caregiving experience. The investigators’ goal was to assess subjectively perceived gains from the rewarding aspects of caregiving or the positive affective returns from caregiving (Lawton, Moss, Kleban, Glicksman, & Rovine, 1991). The PAC consisted of nine items, phrased as statements about the caregiver’s mental/affective state in relation to the caregiving experience. Each item began with the stem, “Providing help to the care recipient has …,” followed with specific items (e.g., “made me feel useful,” “enabled me to appreciate life more”). Each item was rated on a 5-point Likert-type scale ranging from 1 (disagree a lot) to 5 (agree a lot). Summary scores ranged from 9 to 45. Cronbach’s alpha measure of internal consistency was found to be .88 for this instrument.
Time spent caregiving
The amount of time spent in caregiving activities was obtained from the screening interview. The caregiver was asked, “On a typical day, how many hours do you spend directly caring for or supervising the care recipient?” Answers ranged from 1 to 24 hours (M = 8.01, SD = 5.19).
Statistical Analyses
We conducted exploratory factor analyses on the data from Subsample 1 (N = 615) to determine whether additional multifactor models besides the three-factor model might be suggested. Standard principal components analyses were conducted on the occurrence responses and the reaction ratings separately. These analyses were conducted with the SPSS software system. A scree test (Cattell, 1966) was used to determine the number of factors retained for interpretation, and an orthogonal varimax rotation was used (Gorsuch, 1983).
Confirmatory factor analysis methods were applied to the data from Subsample 2 (N = 614) to test the fit of the three-factor model and any additional multifactor models that were suggested from the exploratory factor analyses of Subsample 1. Confirmatory factor analysis is a form of structural equation modeling that is used to evaluate the fit of proposed measurement models (Bollen, 1989). All confirmatory factor analyses were performed with LISREL 8 (Jöreskog & Sörbom, 1996a). Separate analyses were again conducted for the occurrence and reaction data. In both analyses, weighted least squares estimation was used to model the observed polychoric correlation matrix for the 24 items. This is the recommended approach for testing measurement models for items that are measured on an ordinal scale with limited response levels (Jöreskog & Sörbom, 1996b).
The three-factor model identified by Teri et al. (1992) is summarized in the first column of Table 2. Each item was hypothesized as being an effect of only one latent variable or factor, and the strength of this effect or factor loading was estimated by means of the weighted least squares approach. The factor loadings were fixed to 0 for the two factors that were not identified for each item. Correlations between factors were free to be estimated, and a unique variance was also estimated for each item.
Table 2.
Three-Factor Model (Teri et al., 1992) and Descriptive Data for the Revised Memory and Behavior Problems Checklist Items From the Total Sample (N = 1,229)
| Mean reaction ratinga |
||||
|---|---|---|---|---|
| Item | 3-factor model | Occurrence (% yes) | Yes only | Total |
| 1. Repetitive questions | Mem | 72.15 | 1.72 | 1.24 |
| 2. Remembering recent events | Mem | 89.63 | 1.15 | 1.02 |
| 3. Remembering significant events | Mem | 74.26 | 1.16 | 0.85 |
| 4. Losing things | Mem | 65.55 | 1.73 | 1.13 |
| 5. Forgetting day | Mem | 91.65 | 0.74 | 0.67 |
| 6. Not finishing tasks | Mem | 46.43 | 1.14 | 0.52 |
| 7. Difficulty concentrating | Mem | 67.63 | 1.19 | 0.80 |
| 8. Destroying property | Dis | 10.60 | 2.05 | 0.22 |
| 9. Embarrassing activities | Dis | 30.78 | 2.21 | 0.68 |
| 10. Waking at night | Dis | 48.45 | 1.87 | 0.91 |
| 11. Talking loudly and rapidly | Dis | 28.32 | 1.64 | 0.46 |
| 12. Anxious or worried | Dep | 63.54 | 1.71 | 1.08 |
| 13. Dangerous behaviors | Dis | 18.73 | 2.75 | 0.51 |
| 14. Threatened to hurt self | Dep | 4.31 | 2.83 | 0.12 |
| 15. Threatened to hurt others | Dis | 9.94 | 2.33 | 0.23 |
| 16. Verbally aggressive | Dis | 33.12 | 2.27 | 0.75 |
| 17. Sad or depressed | Dep | 63.40 | 1.98 | 1.25 |
| 18. Hopelessness | Dep | 35.23 | 2.22 | 0.78 |
| 19. Crying or tearful | Dep | 27.18 | 2.19 | 0.59 |
| 20. Comments about death | Dep | 23.62 | 1.93 | 0.46 |
| 21. Feeling lonely | Dep | 21.99 | 1.89 | 0.42 |
| 22. Worthless or burden | Dep | 29.78 | 1.98 | 0.59 |
| 23. Feelings of failure | Dep | 12.21 | 2.16 | 0.26 |
| 24. Argumentative | Dis | 54.69 | 2.09 | 1.14 |
Note. Mem = Memory-Related Problems factor; Dis = Disruptive Behaviors factor; Dep = Depression factor.
Mean reaction ratings (a) for caregivers who responded “yes” to the occurrence question only, and (b) for the total sample of caregivers when reaction was set to 0 by default for those who responded “no” to the occurrence question.
A chi-square goodness-of-fit test was performed for each factor model. This test compares the observed polychoric correlation matrix with the matrix that can be reproduced on the basis of the model estimates. Models that completely account for the observed data are associated with nonsignificant chi-square statistics, although this is extremely rare when large samples are used because even the smallest differences between observed and model-reproduced correlations will be statistically significant. Consequently, additional procedures are usually used to evaluate model fit, especially for large samples (Bollen, 1989). In our study, the increment in fit of any multifactor model over a nested one-factor model that allowed all items to load on a single factor was determined by calculating differences in the chi-square statistics and the degrees of freedom for each model. The chi-square difference was then tested for statistical significance. In addition, standard fit indices were examined including the goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), normed fit index (NFI), root mean square residual (RMR), and the root mean square error of approximation (RMSEA). The GFI, AGFI, and NFI all range from 0 to 1, with higher values indicating better fit. For RMR and RMSEA, lower values indicate better fit, with 0 being the limit that is achieved with perfect fit.
The results of the exploratory and confirmatory factor analyses were used to identify the meaningful dimensions or subscales that could be constructed within the RMBPC. The final stage of the analysis involved calculating subscale scores and examining the associations of these dimensions with other indicators of caregiver functioning and with demographic variables. These analyses were conducted on the entire sample of 1,229 caregiver/care-recipient dyads. Spearman rank-order correlations were calculated between RMBPC scores and other measures of caregiver and care recipient functioning in order to evaluate the convergent and discriminant validity of the RMBPC subscales. Demographic comparisons were conducted using one-way analyses of variance (ANOVAs) on the RMBPC scores to compare (a) male and female caregivers at the five sites that included both genders, (b) male and female care recipients across all six sites, (c) African American and White participants at the four sites with sizable samples of these racial–ethnic groups (Birmingham, Boston, Memphis, and Philadelphia), and (d) Hispanic and White participants at the two sites with sizable samples of these ethnic groups (Miami and Palo Alto).
Results
Table 2 contains descriptive data for the 24 items across the entire sample of 1,229 caregivers. Average reaction ratings are reported both for those who endorsed each particular problem as occurring and for the entire sample (in which reaction ratings were set to 0 for caregivers that did not report a particular problem as occurring). We find it interesting that the most common problem reported, forgetting what day it was, was also the problem that was least upsetting among those caregivers who reported the occurrence of this problem. Conversely, some of the rarest problems, such as threatening to hurt oneself and engaging in dangerous behaviors, were rated as quite upsetting when they did occur.
Principal Components Analysis
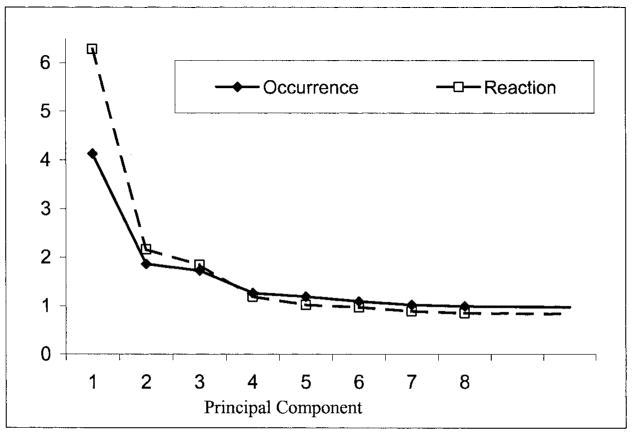
Figure 1 displays the eigenvalues from the principal components analysis for the occurrence and reaction data from Subsample 1. In the reaction analyses, ratings of 0 were assigned when no occurrence of the problem was reported. Similar results were obtained if reaction ratings were coded as missing when the problem did not occur and pairwise deletion methods were used to construct the correlation matrix. In both occurrence and reaction principal components analyses, the scree test suggested that three factors should be retained for interpretation. The varimax factor loadings that were greater than .20 for the occurrence responses and reaction ratings are displayed in Table 3. Gorsuch (1983) recommended that factor loadings as low as .30 are potentially meaningful for factor interpretation, and the lower cutoff of .20 was used here to give the reader additional information about marginal loadings and split factor loadings. Regardless of the factor loading cutoff used, both principal components analyses resulted in factor solutions that closely resembled the hypothesized three-factor model. In the occurrence analysis, every item except “repetitive questions” had its highest loading on the expected factor. Likewise, in the reaction analysis, every item except “threatened to hurt self” had its highest loading on the expected factor. Consequently, the results of the exploratory factor analysis tended to support the relevance of the hypothesized three-factor model, but they were not useful for suggesting alternative multifactor models.
Figure 1.
Scree plots of eigenvalues for occurrence and reaction principal components analyses.
Table 3.
Varimax Factor Loadings Greater Than .20 From the Principal Components Analyses for Occurrence Responses and Reaction Ratings From the Revised Memory and Behavior Problems Checklist (Subsample 1, N = 615)
| Occurrence factor loading
|
Reaction factor loading
|
|||||
|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 1 | 2 | 3 |
| 1. Repetitive questions | .24 | .33 | .44 | .39 | .21 | |
| 2. Remembering recent events | .61 | .73 | ||||
| 3. Remembering significant events | .52 | .65 | ||||
| 4. Losing things | .42 | .23 | .55 | .29 | ||
| 5. Forgetting day | .51 | .75 | ||||
| 6. Not finishing tasks | .58 | .65 | ||||
| 7. Difficulty concentrating | .59 | .73 | ||||
| 8. Destroying property | .56 | .54 | ||||
| 9. Embarrassing activities | .53 | .25 | .49 | |||
| 10. Waking at night | .29 | .32 | .34 | |||
| 11. Talking loudly and rapidly | .58 | .60 | ||||
| 12. Anxious or worried | .21 | .54 | .37 | .25 | .49 | |
| 13. Dangerous behaviors | .46 | .52 | ||||
| 14. Threatened to hurt self | .21 | .27 | .31 | .24 | ||
| 15. Threatened to hurt others | .64 | .68 | ||||
| 16. Verbally aggressive | .64 | .23 | .69 | .25 | ||
| 17. Sad or depressed | .59 | .33 | .64 | |||
| 18. Hopelessness | .73 | .20 | .76 | |||
| 19. Crying or tearful | .44 | .21 | .49 | |||
| 20. Comments about death | .23 | .46 | .57 | |||
| 21. Feeling lonely | .58 | .65 | ||||
| 22. Worthless or burden | .65 | .73 | ||||
| 23. Feelings of failure | .56 | .66 | ||||
| 24. Argumentative | .55 | .34 | .25 | .58 | .35 | |
Confirmatory Factor Analysis
The weighted least squares estimates from the LISREL confirmatory factor analyses of the occurrence and reaction data from Subsample 2 are displayed in Table 4. Correlations between factors were estimated, and these are also displayed in Table 4. The fit statistics for the one- and three-factor models are displayed in Table 5. The three-factor model was found to fit the data significantly better than the one-factor model for both the occurrence responses, χ2diff (3, N = 614) = 325.69, p < .0001, and the reaction ratings, χ2diff (3, N = 614) = 351.96, p < .0001.
Table 4.
LISREL Weighted Least Squares Estimates for Occurrence Responses and Reaction Ratings for the Three-Factor Model of the Revised Memory and Behavior Problems Checklist Items (Subsample 2, N = 614)
| Occurrence
|
Reaction
|
|||||
|---|---|---|---|---|---|---|
| Item | Mem | Dis | Dep | Mem | Dis | Dep |
| Factor loadings | ||||||
| 1. Repetitive questions | .64 | 0 | 0 | .63 | 0 | 0 |
| 2. Remembering recent events | .68 | 0 | 0 | .85 | 0 | 0 |
| 3. Remembering significant events | .36 | 0 | 0 | .74 | 0 | 0 |
| 4. Losing things | .88 | 0 | 0 | .63 | 0 | 0 |
| 5. Forgetting day | .47 | 0 | 0 | .81 | 0 | 0 |
| 6. Not finishing tasks | .71 | 0 | 0 | .72 | 0 | 0 |
| 7. Difficulty concentrating | .61 | 0 | 0 | .81 | 0 | 0 |
| 8. Destroying property | 0 | .58 | 0 | 0 | .62 | 0 |
| 9. Embarrassing activities | 0 | .52 | 0 | 0 | .75 | 0 |
| 10. Waking at night | 0 | .71 | 0 | 0 | .67 | 0 |
| 11. Talking loudly and rapidly | 0 | .47 | 0 | 0 | .68 | 0 |
| 12. Anxious or worried | 0 | 0 | .81 | 0 | 0 | .73 |
| 13. Dangerous behaviors | 0 | .73 | 0 | 0 | .47 | 0 |
| 14. Threatened to hurt self | 0 | 0 | .46 | 0 | 0 | .47 |
| 15. Threatened to hurt others | 0 | .51 | 0 | 0 | .63 | 0 |
| 16. Verbally aggressive | 0 | .78 | 0 | 0 | .82 | 0 |
| 17. Sad or depressed | 0 | 0 | .74 | 0 | 0 | .72 |
| 18. Hopelessness | 0 | 0 | .90 | 0 | 0 | .86 |
| 19. Crying or tearful | 0 | 0 | .68 | 0 | 0 | .64 |
| 20. Comments about death | 0 | 0 | .81 | 0 | 0 | .86 |
| 21. Feeling lonely | 0 | 0 | .80 | 0 | 0 | .77 |
| 22. Worthless or burden | 0 | 0 | .85 | 0 | 0 | .87 |
| 23. Feelings of failure | 0 | 0 | .79 | 0 | 0 | .83 |
| 24. Argumentative | 0 | .94 | 0 | 0 | .77 | 0 |
| Factor correlations | ||||||
| Mem | — | — | ||||
| Dis | .53 | — | .79 | — | ||
| Dep | .56 | .74 | — | .70 | .74 | — |
Note. Factor loadings equal to 0 were fixed to be 0 in the three-factor model. Mem = Memory-Related Problems factor; Dis = Disruptive Behaviors Factor; Dep = Depression factor.
Table 5.
Fit Statistics for LISREL Confirmatory Factor Analysis Models (Subsample 2, N = 614)
| Model | χ2 | df | GFI | AGFI | NFI | RMR | RMSEA |
|---|---|---|---|---|---|---|---|
| Occurrence | |||||||
| 1-factor | 1,216.8 | 252 | .89 | .87 | .72 | .23 | .08 |
| 3-factor | 891.1 | 249 | .92 | .91 | .80 | .17 | .07 |
| Reaction | |||||||
| 1-factor | 1,385.6 | 252 | .90 | .88 | .77 | .22 | .09 |
| 3-factor | 1,033.7 | 249 | .92 | .91 | .83 | .16 | .07 |
Note. GFI = goodness-of-fit index; AGFI = adjusted goodness-of-fit index; NFI = normed fit index; RMR = root mean square residual; RMSEA = root mean square error of approximation.
The fit indices suggested that the simple one-factor model fit the data relatively well. However, all fit indices indicated substantial improvements in fit when correlated factors were estimated for the three-factor model. Both GFI and AGFI exceeded .90 for the three-factor model, suggesting relatively good overall fit for this model. Although the chi-square statistic, NFI, RMR, and RMSEA all indicated that the three-factor model did not provide perfect fit to the observed data, an examination of the residuals and modification indices was not helpful for suggesting simple modifications to this model that would substantially improve fit.
RMBPC Subscale Scores
Descriptive data for the number of problems, average reaction rating, and total reaction are displayed in Table 6. Cronbach’s alpha was somewhat higher for the total reaction subscales than for the number of problems subscales. Cronbach’s alpha was low for the number of memory-related problems scale, in part, due to high endorsement rates for two items (trouble remembering recent events and forgetting what day it is), which limited variability.
Table 6.
Descriptive Data for the Revised Memory and Behavior Problems Checklist Subscales
| Number of problems
|
Average reaction per problem
|
Total reaction
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | M | SD | N | Min | Max | α | M | SD | N | Min | Max | M | SD | N | Min | Max | α |
| Memory problems | 5.08 | 1.55 | 1,229 | 0 | 7 | .55 | 1.19 | 0.94 | 1,216 | 0 | 4 | 6.28 | 5.51 | 1,229 | 0 | 28 | .81 |
| Disruptive behaviors | 2.35 | 1.87 | 1,229 | 0 | 8 | .66 | 1.93 | 1.08 | 1,024 | 0 | 4 | 4.91 | 5.36 | 1,229 | 0 | 28 | .73 |
| Depression | 2.81 | 2.19 | 1,229 | 0 | 9 | .75 | 1.78 | 1.10 | 1,024 | 0 | 4 | 5.56 | 6.29 | 1,229 | 0 | 32 | .81 |
| Total score | 10.22 | 4.16 | 1,229 | 0 | 23 | .78 | 1.49 | 0.91 | 1,226 | 0 | 4 | 16.73 | 13.64 | 1,229 | 0 | 68 | .87 |
Note. Min = minimum; Max = maximum.
Convergent and Discriminant Validity
Spearman rank-order correlations between the RMBPC scores and caregiver age, care recipient age, MMSE score, time spent providing care, CES-D, LTS, and PAC across the entire sample of 1,229 caregiver/care-recipient dyads are displayed in Table 7. Overall, correlations were very similar for the average reaction and total reaction scores, and these tended to be slightly higher than the correlations with the number of problems reported. Caregiver age was slightly negatively correlated with the number of disruption and depression problems such that older caregivers reported fewer problems. However, as predicted, no significant correlations were found between RMBPC measures and care recipient age.
Table 7.
Spearman Correlation Coefficients Between the Revised Memory and Behavior Problems Checklist Scales and Other Variables (N = 1,229)
| Number of problems
|
Average reaction
|
Total reaction
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mem | Dis | Dep | Total | Mem | Dis | Dep | Total | Mem | Dis | Dep | Total |
| CG age | .01 | −.13* | −.17* | −.14* | .09* | .06 | .02 | .04 | .09* | −.08* | −.12* | −.04 |
| CR age | .04 | .00 | .04 | .04 | −.06 | −.05 | −.02 | −.05 | −.04 | −.02 | −.00 | −.02 |
| CR MMSE | .10* | −.05 | .13* | .08* | .21* | .19* | .06 | .18* | .20* | .07 | .13* | .17* |
| Time spent caregiving | .06 | .15* | .05 | .10* | −.02 | .03 | .06 | .18* | −.01 | .11* | .05 | .06 |
| CES-D | .14* | .23* | .28* | .30* | .31* | .32* | .35* | .41* | .32* | .32* | .36* | .43* |
| LTS | −.02 | −.14* | −.10* | −.12* | −.14* | −.17* | −.19* | −.22* | −.13* | −.18* | −.17* | −.21* |
| PAC | −.07 | −.10* | −.04 | −.09* | −.22* | −.29* | −.15* | −.24* | −.22* | −.22* | −.13* | −.23* |
Note. Mem = memory-related problems; Dis = disruptive behaviors; Dep = depression; CG = caregiver; CR = care recipient; MMSE = Mini-Mental State Exam; CES–D = Center for Epidemiological Studies—Depression Scale; LTS = Leisure Time Satisfaction; PAC = Positive Aspects of Caregiving.
p < .01.
As expected, RMBPC scores were found to have moderate positive correlations with the CES-D. Relatively small positive correlations were generally found between RMBPC scores and the amount of time spent in caregiving activities, but only four of these correlations were statistically significant. The RMBPC scores were also found to show small negative correlations with LTS and PAC, as predicted. These effects indicate that caregivers who reported higher levels of satisfaction with leisure activities and who reported many positive aspects of caregiving tended to report fewer problems and lower reaction ratings on the RMBPC.
The Spearman correlations indicated that the RMPBC measures tended to have small positive associations with MMSE, indicating that fewer problems were reported as MMSE scores decreased. However, regression analyses examining quadratic effects revealed significant curvilinear effects when regressing RMBPC scores on the MMSE, as predicted. Significant quadratic effects were found for all three total scores: number of problems reported (p = .001), average reaction (p = .03), and total reaction (p = .03). For the RMBPC subscales, significant quadratic effects were found for the number of depression problems reported (p = .002), total reaction to disruptive behavior problems (p = .02), and total reaction to depression problems (p = .05). Consistent with findings of McCarty et al. (2000), an inverted ∪-shaped curve was found such that the highest predicted RMBPC scores were observed for care recipients with MMSE scores toward the middle of the distribution (i.e., care recipients with moderately severe dementia). However, no such curvilinear relationships were found when regressing memory-related problems on MMSE.
Spearman correlations were also examined among the RMBPC measures themselves. The total reaction scores were highly correlated with both the number of problem scores (rs ranged from .49 to .86) and the average reaction scores (rs ranged from .74 to .94). This reflects the fact that the total reaction scores represent a combination of the number of problems endorsed and the average reaction rating per problem endorsed. The Spearman correlations between the number of problems endorsed and the average reaction scores were more modest (rs ranged from .22 to .41), suggesting that these two indices assess distinct constructs.
Effects of Gender and Race–Ethnicity on RMBPC Scales
One-way ANOVAs comparing female caregivers (N = 737) and male caregivers (N = 228) across the five sites that included both genders generally revealed higher RMBPC scores for the female caregivers. Statistically significant differences were found between female and male caregivers on all three measures from the entire instrument: total number of problems (Ms = 10.09 vs. 9.27, p= .007), average reaction rating (Ms = 1.52 vs. 1.32, p = .004), and total reaction score (Ms = 16.93 vs. 13.73, p = .002). Concerning the RMBPC subscales, female caregivers reported significantly more disruptive behavior problems than male caregivers (Ms = 2.33 vs. 1.90, p = .002), higher average reaction ratings for disruptive behavior problems (Ms = 1.90 vs. 1.55, p = .002), higher total reaction scores for disruptive behaviors (Ms = 5.04 vs. 3.42, p < .001), and higher average reaction ratings for depression problems (Ms = 1.84 vs. 1.59, p = .009).
When examining relationships between RMBPC scores and care-recipient gender, we observed a different pattern. More problems with depression were reported for female care recipients than for male care recipients (Ms = 3.01 vs. 2.56, p < .001). However, average reaction scores were higher for male care recipients than for female care recipients on all scales: total (Ms = 1.58 vs. 1.42, p = .002), memory-related problems (Ms = 1.28 vs. 1.12, p = .003), disruption (Ms = 2.07 vs. 1.82, p < .001), and depression (Ms = 1.88 vs. 1.70, p= .007). Consequently, total reaction scores were significantly higher for male care recipients than for female care recipients for memory-related problems (Ms = 6.70 vs. 5.94, p = .02) and for disruptive behaviors (Ms = 5.29 vs. 4.60, p = .02).
Comparisons between African American (N = 293) and White (N = 419) dyads across the Birmingham, Boston, Memphis, and Philadelphia sites revealed that African Americans generally had lower RMBPC scores than Whites. Statistically significant differences were observed for all three scores from the total instrument: number of problems (Ms = 9.28 in African Americans vs. 10.22 in Whites, p = .002), average reaction (Ms = 1.24 in African Americans vs. 1.56 in Whites, p < .001), and total reaction (Ms = 13.43 in African Americans vs. 17.47 in Whites, p < .001). On the RMBPC subscales, African Americans reported fewer memory problems (Ms = 4.81 vs. 5.20, p = .01) and depression problems (Ms = 2.20 vs. 2.70, p = .002) than White participants. African Americans had lower average reaction ratings than Whites on all three subscales: memory-related problems (Ms = 1.00 vs. 1.24, p < .001), disruptive behaviors (Ms = 1.69 vs. 2.03, p = .001), depression (Ms = 1.59 vs. 1.86, p = .005). In addition, the total reaction scores for African Americans were lower than those for Whites for memory-related problems (Ms = 5.05 vs. 6.79, p < .001) and depression (Ms = 4.07 vs. 5.64, p = .001).
Comparisons between Hispanic (N = 211) and White (N = 260) dyads from the Miami and Palo Alto sites revealed an interesting pattern of statistically significant differences. Hispanics reported a higher total number of problems (Ms = 11.35 in Hispanics vs. 10.30 in Whites, p = .007) but lower average reaction ratings (Ms = 1.38 in Hispanics vs. 1.74 in Whites, p < .01). On the RMBPC subscales, Hispanics reported more disruptive behavior problems (Ms = 2.68 vs. 2.18, p = .006) and more depression problems (Ms = 3.63 vs. 2.96, p < .001) than White participants. Hispanics also were found to have lower average reaction scores than Whites on all three subscales: memory-related problems (Ms = 1.02 vs. 1.43, p < .001), disruptive behaviors (Ms = 1.79 vs. 2.14, p = .001), and depression (Ms = 1.59 vs. 2.00, p < .001).
Discussion
Previous factor analytic studies of the RMBPC have focused exclusively on frequency ratings, and the present study expanded on this research in two important ways. First, by implementing a confirmatory factor analytic approach, we were able to examine the fit of the three-factor model more directly than has been accomplished in exploratory factor analysis studies. Second, the present results represent the first published findings concerning the factor structure of either dichotomous occurrence responses or caregiver reaction ratings. Results from both exploratory and confirmatory factor analyses supported the fit of the original three-factor model. This model includes correlated but distinct factors for memory-related problems, disruptive behavior, and depression. Although the absolute fit of this model was not perfect, no alternative models with comparable parsimony were suggested by either the exploratory analyses from Subsample 1 or by the modification indices from the confirmatory analyses on Subsample 2. For both the occurrence and reaction data, the three-factor model fit significantly better than a unidimensional model, supporting the existence of some distinctiveness for these dimensions. Acceptable indices of internal consistency were also found, particularly for the total reaction subscales. Thus, the RMPBC appears to provide an adequate screening of the occurrence of behavior problems and the subjective burden associated with these problems in three distinct domains from the family caregiver’s point of view.
The REACH sample used in this study was found to exhibit lower MMSE scores on average (M = 12.6) than the original validation sample (M = 19; Teri et al., 1992), thus extending the validation process to a more impaired population. Furthermore, Teri and colleagues performed successive reanalyses of the same data after eliminating sets of items with undesirable loading patterns, and this approach might have capitalized on chance variability in their data. The present study provides an independent replication of the three-factor model with a much larger sample. The large, multisite, multiethnic nature of the REACH sample further supports the generalizability of this factor model beyond what has previously been accomplished with single-site exploratory studies.
We found supporting evidence for the convergent and discriminant validity of the RMBPC measures. As predicted, RMBPC scores were significantly correlated with measures of caregiver depression. Smaller correlations in the expected direction were observed with measures of LTS, PAC, and time spent in caregiving activities. None of the RMBPC measures were significantly correlated with care recipient age. An inverted ∪-shaped curvilinear relationship was found between some RMBPC measures and the MMSE, consistent with findings from previous research (McCarty et al., 2000). Our findings suggest that care recipients with moderate cognitive impairment present more behavior problems to caregivers and that these problems become less frequent and less bothersome at the more advanced stages of dementia. Findings from previous research indicated moderate inverse relationships between the frequency of behavior problems and cognitive status (Dura et al., 1990; McCarty et al., 2000; Teri et al., 1992), but no such negative correlations were found between our RMBPC measures and the MMSE in the present study. It is likely that the wider range of dementia severity observed in the REACH study compared with the earlier studies allowed for these curvilinear relationships to emerge. In addition, because the REACH care recipients had higher levels of cognitive impairment, on average, than those from previous studies, the negative linear relationships found in previous studies may have been more prevalent among those with less severe cognitive impairments. This pattern of findings would be consistent with the curvilinear relationships that we found in the present investigation. Another possibility is that ratings of the frequency of behavior problems, and not just their occurrence or nonoccurrence over the preceding week, are needed to more fully understand the true association between behavior problems and objective cognitive status.
Female caregivers reported more behavior problems and higher reaction ratings than male caregivers. Previous comparisons of male and female caregivers have shown that women report not only more burden and strain due to the caregiving role but also more psychiatric symptoms than male family caregivers (Yee & Schulz, 2000). Interestingly, although more depressive behaviors were reported for female care recipients than for male care recipients, higher reaction ratings were observed for male care recipients than for female care recipients.
African American caregivers were found to report fewer memory and behavior problems than White caregivers. African Americans also consistently reported lower average reaction ratings than Whites. These racial differences are consistent with the findings of Haley et al. (1996), who found similar differences between African Americans and Whites on the stressfulness ratings of behavior problems. Furthermore, Haley and colleagues showed that these appraisal differences were partly responsible for explaining observed racial differences on measures of depression and life satisfaction. Taken together, the present findings add to a larger body of evidence that suggests African American family caregivers are less susceptible to the emotional distress associated with dementia caregiving than are White family caregivers (Connell & Gibson, 1997; Roth et al., 2001). Additional research is needed to more fully describe and explain the relative advantages that African American family caregivers consistently report in comparison with White caregivers on measures of emotional distress and caregiving burden.
Hispanic caregivers were found to report more problems than White caregivers at the Miami and Palo Alto sites, but the average reaction ratings of the Hispanic caregivers were consistently lower than their White counterparts. Older Hispanic caregivers, in particular, may not feel comfortable admitting any distress associated with family caregiving. Maldonado (1985) found that older Hispanic caregivers were less likely to attend support groups and seek information about the caregiving process than their younger, more acculturated counterparts. Moreover, many older Hispanics who were not born in the United States endorse a set of traditional cultural values that might prevent them from actively seeking the help they need in managing the caregiving role. These values include relying on family for assistance rather than seeking outside help and taking on burdensome tasks without complaint (Gallagher-Thompson et al., 2000). Recent qualitative research (Calderón & Tennstedt, 1998; John & McMillian, 1998) also suggests that while Hispanic caregivers might describe their caregiving experience in terms that are descriptive of burden (e.g., socially isolating, situationally frustrating, or fostering resentment due to lack of other family member involvement), the concept of burden itself is unpalatable to many of these individuals. Therefore, cultural values may limit the extent to which the words bother or upset as related to caregiving are reported, and caregivers who report many problems but little burden may still benefit from interventions aimed at managing these problems.
There are many limitations to this study that should be acknowledged. Combining data across six different sites led to a large sample size but also involved pooling responses across important geographic and cultural differences. The ethnic composition of our sample, for example, fluctuates from site to site, making valid ethnic comparisons that are completely independent of site differences difficult to accomplish. Also, the effects reported here due to race–ethnicity and gender were not adjusted for the effects of demographic variables such as age of the caregiver, the caregiver’s relationship to the patient, or socioeconomic status. African American family caregivers were younger on average (M = 58.2 years) than White family caregivers (M = 65.0), but the age difference between African American and White caregivers cannot account for the differences observed on the RMBPC because older caregivers, on average, reported slightly fewer problems and lower reaction ratings than younger caregivers. Nonetheless, other demographic variables and regional differences are undoubtedly involved in partially accounting for the race–ethnic differences observed here. Additional and more comprehensive analyses by the REACH investigators are addressing these ethnic differences on a range of variables, and more multisite, multivariate research is needed to better understand the effect of ethnicity on caregiver emotional adjustment.
Many family caregivers struggle to manage the chronic behavior problems that are often associated with dementia. Caregivers as a group have been found to report deteriorating physical health over time compared with noncaregivers (Roth et al., 2001), and caregivers who report being burdened by their responsibilities have been shown to have increased mortality rates (Schulz & Beach, 1999). Consequently, it is important to routinely assess the amount of ongoing memory and behavior problems that persons with dementia are displaying and the degree to which these problems are distressing to the family members who care for them. Where feasible, brief assessments such as the RMBPC can be administered in 5 to 10 min in routine, clinical practice. When this is not practical, clinicians may still find it useful to screen for the most frequent problem behaviors and for those problems that are causing the greatest distress for family caregivers. Targeted inquiries in these areas will assist clinicians in identifying families that are in need of further assessment or additional services.
Acknowledgments
This research was supported by National Institute on Aging Grants U01-AG13255, U01-AG13265, U01-AG13289, U01-AG13297, AG13305, and U01-AG13313, and by National Institute of Nursing Research Grant U01-NR13269.
Contributor Information
David L. Roth, University of Alabama at Birmingham
Laura N. Gitlin, Thomas Jefferson University
David W. Coon, Institute on Aging
Alan B. Stevens, University of Alabama at Birmingham
Louis D. Burgio, University of Alabama
Dolores Gallagher-Thompson, Stanford University School of Medicine and Veterans Affairs Palo Alto Health Care System.
Steven H. Belle, University of Pittsburgh
Robert Burns, Veterans Affairs Medical Center, Memphis, Tennessee.
References
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Calderón V, Tennstedt SL. Ethnic differences in the expression of caregiver burden: Results of a qualitative study. Journal of Gerontological Social Work. 1998;30:159–178. [Google Scholar]
- Cattell RB. The scree test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Connell CM, Gibson GD. Racial, ethnic, and cultural differences in dementia caregiving: Review and analysis. The Gerontologist. 1997;37:355–364. doi: 10.1093/geront/37.3.355. [DOI] [PubMed] [Google Scholar]
- Coon DW, Schulz R, Ory MG. Innovative intervention approaches with Alzheimer’s disease caregivers. In: Biegel D, Blum A, editors. Innovations in practice and service delivery across the lifespan. New York: Oxford University Press; 1999. pp. 295–325. [Google Scholar]
- Dura JR, Bornstein RA, Kiecolt-Glaser JK. Refinements in the assessment of dementia-related behaviors: Factor structure of the memory and behavior problem checklist. Psychological Assessment. 1990;2:129–133. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fuh JL, Liu CY, Wang SJ, Wang HC, Liu HC. Revised Memory and Behavior Problems Checklist in Taiwanese patients with Alzheimer’s disease. International Psychogeriatrics. 1999;11:181–189. doi: 10.1017/s1041610299005736. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Árean P, Coon D, Menéndez A, Takagi K, Haley W, et al. Development and implementation of intervention strategies for culturally diverse caregiving populations. In: Schulz R, editor. Handbook on dementia caregiving. New York: Springer; 2000. pp. 151–185. [Google Scholar]
- Gitlin LN, Belle SH, Burgio L, Czaja SJ, Mahoney D, Gallagher-Thompson D, et al. Effect of multicomponent interventions on caregiver burden and depression: The REACH multisite initiative at 6-months follow-up. Psychology and Aging. 2003;18:361–374. doi: 10.1037/0882-7974.18.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorsuch RL. Factor analysis. 2. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- Haley WE, Bailey S. Research on family caregiving in Alzheimer’s disease: Implications for practice and policy. In: Vellas B, Fitten JL, editors. Research and practice in Alzheimer’s disease. Vol. 2. Paris: Serdi Publisher; 1999. pp. 321–332. [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CAC, Collins RP, Isobe TL. Appraisal, coping, and social support as mediators of well-being in Black and White family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology. 1996;64:121–129. doi: 10.1037//0022-006x.64.1.121. [DOI] [PubMed] [Google Scholar]
- John R, McMillian B. Exploring caregiver burden among Mexican Americans: Cultural prescriptions, family dilemmas. Journal of Aging and Ethnicity. 1998;1:93–111. [Google Scholar]
- Jöreskog KG, Sörbom DG. LISREL 8: User’s reference guide. Chicago: Scientific Software International; 1996a. [Google Scholar]
- Jöreskog KG, Sörbom DG. PRELIS 2: User’s reference guide. Chicago: Scientific Software International; 1996b. [Google Scholar]
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. Journal of Gerontology. 1991;4:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- Maldonado D. The Hispanic elderly: A socio historical framework for public policy. Journal of Applied Gerontology. 1985;4:18–27. [Google Scholar]
- McCarty HJ, Roth DL, Goode KT, Owen JE, Harrell L, Donovan K, Haley WE. Longitudinal course of behavior problems during Alzheimer’s disease: Linear and curvilinear patterns of decline. Journal of Gerontology: Medical Sciences. 2000;55A:M200–M206. doi: 10.1093/gerona/55.4.m200. [DOI] [PubMed] [Google Scholar]
- Radloff L, Teri L. Use of the Center for Epidemiological Studies-Depression Scale with older adults. Clinical Gerontologist. 1986;5:119–137. [Google Scholar]
- Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: A comparison of African American and White family caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Schulz R, Williamson GM. A 2-year longitudinal study of depression among Alzheimer’s caregivers. Psychology and Aging. 1991;6:569–578. doi: 10.1037//0882-7974.6.4.569. [DOI] [PubMed] [Google Scholar]
- Switzer GE, Wisniewski SR, Belle SH, Dew MA, Schulz R. Selecting, developing, and evaluating research instruments. Social Psychiatry and Psychiatric Epidemiology. 1999;34:399–409. doi: 10.1007/s001270050161. [DOI] [PubMed] [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: The Revised Memory and Behavior Problems Checklist. Psychology and Aging. 1992;7:622–631. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- Wagner AW, Teri L, Orr-Rainey N. Behavior problems among dementia residents in special care units: Changes over time. Journal of the American Geriatrics Society. 1995;43:784–787. doi: 10.1111/j.1532-5415.1995.tb07051.x. [DOI] [PubMed] [Google Scholar]
- Weiner MF, Tractenberg R, Teri L, Logsdon R, Thomas RG, Gamst A, Thal LJ. Quantifying behavioral disturbance in Alzheimer’s disease patients. Journal of Psychiatric Research. 2000;34:163–167. doi: 10.1016/s0022-3956(99)00042-4. [DOI] [PubMed] [Google Scholar]
- Wisniewski SR, Belle SH, Coon DW, Marcus SM, Ory MG, Burgio LD, et al. The Resources for Enhancing Alzheimer’s Caregiver Health (REACH): Project design and baseline characteristics. Psychology and Aging. 2003;18:375–384. doi: 10.1037/0882-7974.18.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yee JL, Schulz R. Gender differences in psychiatric morbidity among family caregivers: A review and analysis. The Gerontologist. 2000;40:147–164. doi: 10.1093/geront/40.2.147. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Zarit JM. Cognitive impairment. In: Lewinsohn PM, Teri L, editors. Clinical geropsychology. Elmsford, NY: Pergamon Press; 1983. pp. 38–81. [Google Scholar]