Abstract
The disparities in the burden of ill health caused by environmental risks should be an important consideration beyond their aggregate population effects. We used comparative risk assessment methods to calculate the mortality effects of unsafe water and sanitation, indoor air pollution from household solid fuel use, and ambient urban particulate matter pollution in Mexico. We also estimated the disparities in mortality caused by each risk factor, across municipios (counties) of residence and by municipio socioeconomic status (SES). Data sources for the analysis were the national census, population-representative health surveys, and air quality monitoring for risk factor exposure; systematic reviews and meta-analyses of epidemiological studies for risk factor effects; and vital statistics for disease-specific mortality. During 2001–2005, unsafe water and sanitation, household solid fuel use, and urban particulate matter pollution were responsible for 3,000, 3,600, and 7,600 annual deaths, respectively. Annual child mortality rates would decrease by 0.2, 0.1, and 0.1 per 1,000 children, and life expectancy would increase by 1.0, 1.2, and 2.4 months, respectively, in the absence of these environmental exposures. Together, these risk factors caused 10.6% of child deaths in the lowest-SES communities (0.9 deaths per 1,000 children), but only 4.0% in communities in the highest-SES ones (0.1 per 1,000). In the 50 most-affected municipios, these 3 exposures were responsible for 3.2 deaths per 1,000 children and a 10-month loss of life expectancy. The large disparities in the mortality effects of these 3 environmental risks should form the basis of interventions and environmental monitoring programs.
Keywords: environmental health, environmental justice, global health, population health, risk assessment
Unsafe water and sanitation, indoor air pollution from household solid fuel use, and ambient urban particulate matter (PM) pollution are responsible for an estimated 3.4%, 2.7%, and 0.6% of the global burden of disease, respectively, with 90%, 71%, and 7% of the disease burden from these risk factors borne by infants and young children in low- and middle-income countries (1). The burden of disease associated with environmental exposures is likely to vary across population subgroups, based on their socioeconomic status (SES), place of residence, or race and ethnicity. Past research on SES, the environment, and health has focused on disparities in exposure to environmental contaminants, with a more limited body of research investigating disparities in disease outcomes (e.g., deaths or episodes of illness) that are caused by an environmental exposure (2). However, few studies have quantified both the disparities in exposure to environmental risks and the disease burden that is actually attributable to these exposures (3, 4).
Disparities in the burden of disease caused by one or multiple environmental exposures are determined both by disparities in exposure and by differences in susceptibility (2, 5). Susceptibility, defined as greater health effects at a given exposure level, can be determined by biological factors (e.g., gene–environment interaction), differential exposure to other risks that affect the same diseases as the environmental exposures (e.g., undernutrition or tobacco smoking), or disparities in health-care access and treatment that can reduce disease severity and mortality risk.* Data on health outcomes (e.g., disease-specific deaths or incidence) and exposure, both stratified on SES, are needed to quantify disparities in disease burden attributable to environmental risks.
Mexico is an ideal country to examine the relationship among SES, the environment, and health, both because high-quality population, environmental, and mortality data are available at the municipio (county) level and because of its environmental and epidemiological characteristics. Residents of urban areas in Mexico have experienced substantial exposure to urban air pollution associated with industrial activities and transportation in recent decades. At the same time, in some poor and marginalized communities, exposure to indoor smoke from household solid fuel use and to inadequate water and sanitation infrastructure remains high. Between 1990 and 2005, the proportion of population without household sanitation decreased from 42% to 21% (6), and the proportion using solid fuels decreased from ≈20% to 15% (7, 8). Improvement in urban air quality has been less consistent: PM concentrations have improved in only a few cities since monitoring began (9). Mexico is also at an advanced stage of the epidemiological transition, with most disease burden caused by chronic diseases, yet child mortality remains moderately high in some areas, especially in the poorer Southern states (10).
In this study, we used data on exposure to 3 major environmental risks (unsafe water and sanitation, indoor air pollution from household solid fuel use, and ambient urban PM pollution) and on cause-specific mortality at the municipio level in Mexico to estimate the mortality effects of these 3 risks at the municipio level. We also used national censuses to assign a composite SES score to all municipios. These data allowed us to examine not only the disparities in exposure to these environmental risk factors but also the disparities in the mortality burden caused by these exposures, both by the place of residence and by community SES.
National Mortality Effects of Environmental Risks.
During 2001–2005, ambient urban PM pollution was responsible for 7,600 deaths per year, more than twice those caused by either household solid fuel use (3,600) or unsafe water and sanitation (3,000). Thirty-eight percent of deaths due to urban PM (2,900) occurred in the Mexico City metropolitan region, principally because of its large population (35% of Mexico's urban population); an additional 23% occurred in the metropolitan areas of Guadalajara, Monterrey, Puebla, and Toluca. Jointly, exposure to these 3 risk factors caused an estimated 14,000 annual deaths, representing 3.0% of total deaths in Mexico.
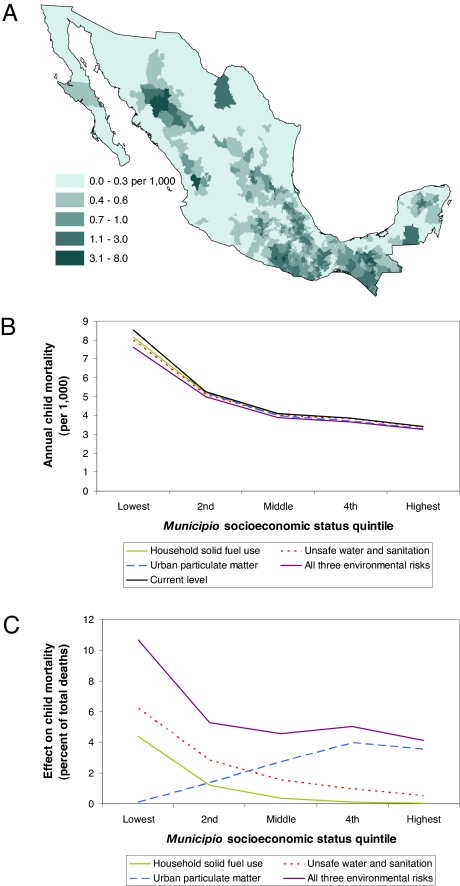
An estimated 1,900 child deaths (3.4% of total child deaths) were attributable to unsafe water and sanitation, 1,100 (1.9%) to household solid fuel use, and 1,000 (1.7%) to urban PM pollution. The annual child mortality rate in Mexico is 5.7 per 1,000, typical of upper-middle-income countries. If exposure to all 3 environmental risks were removed, child mortality would be 5.4 per 1,000 (a 6.3% decrease, equivalent to 3,900 annual child deaths).
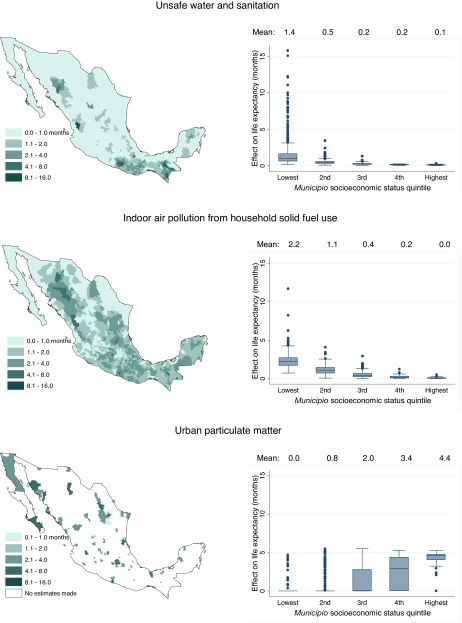
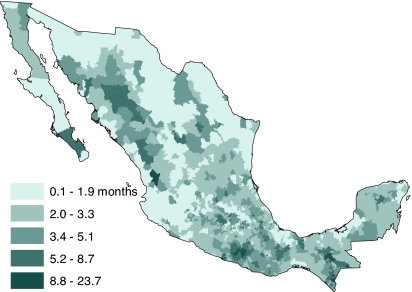
Average life expectancy in Mexico for 2000–2005 was 72.3 years for men and 77.8 for women. If exposure to unsafe water and sanitation were removed, life expectancy would be higher by 1.0 month; the corresponding gains would be 1.2 months for providing clean household fuels, 2.4 months for reducing urban PM pollution, and 4.6 months for the combined effects of all 3 risks [≈13% of the 3-year difference between Mexican and U.S. life expectancies (11)].
Municipio-Level Mortality Effects of Environmental Risks.
A small number of communities were disproportionately affected by the risks associated with unsafe water and sanitation and household solid fuel use [Fig. 1 and supporting information (SI) Fig. S1]. The effects of unsafe water and sanitation and solid fuel use were largest in some municipios in Chiapas, Oaxaca, and Guerrero, in northern and eastern Puebla, and in the mountainous regions of Chihuahua, Durango, and Nayarit, where exposure to these risks and child mortality were both high. For example, unsafe water and sanitation was responsible for 0.17 deaths per 1,000 children nationally vs. ≥2 deaths per 1,000 in 17 municipio units with the largest effects (Fig. S1). Geographical patterns of, and disparities in, life expectancy loss attributable to these 2 risks were similar to those of their effects on child mortality, with the life-expectancy loss attributable to poor water and sanitation >1 year in several municipios in Chiapas and Guerrero (Fig. 1).
Fig. 1.
Life expectancy reduction as a result of 3 environmental risk factors, by municipio of residence and by municipio SES quintile.
The effects of urban PM pollution on child mortality were largest in Toluca and Puebla (0.53 and 0.43 per 1,000 children, respectively, vs. 0.18 for all urban areas) because of high PM concentration in Toluca and high child mortality in Puebla. The effects of this risk factor on life expectancy showed less geographical variation than the 2 household exposures, ranging between 3 and 5.5 months in urban municipios. This was because both ambient PM pollution and mortality rates of adults, the primary age group affected by ambient air pollution, were relatively similar across urban areas.
When all 3 risk factors were considered together, disparities in mortality effects were even more striking (Figs. 2 and 3). In the 50 most-affected municipio units, these exposures led to 3.2 deaths per 1,000 children and a life expectancy loss of 10 months, compared with national averages of 0.3 per 1,000 and 4.6 months. These municipios contain 1.5% of Mexico's population yet experience 5.8% of all deaths and 16.2% of child deaths caused by these 3 environmental risk factors; unsafe water and sanitation had the largest mortality effects of the 3 risks in these communities. These municipios are located primarily in Chiapas, Guerrero, Oaxaca, and Puebla and are predominantly indigenous (64% of the population speaks an indigenous language vs. 7.2% nationally).
Fig. 2.
Effects of 3 environmental risk factors on child mortality, by municipio of residence and by municipio SES quintile. (A) Child mortality rate attributable to all 3 risks by municipio of residence. (B) Current and expected child mortality rate if individual or multiple risk factors were removed. (C) Proportion of child deaths attributable to the 3 risk factors.
Fig. 3.
Loss of life expectancy caused by all 3 environmental risks by municipio of residence.
The correlation between the loss of life expectancy caused by unsafe water and sanitation and its risk-weighted exposure was 0.42. This moderate correlation indicates that other factors, such as access to treatment (including oral rehydration therapy, ORT), which is an important determinant of child survival from diarrheal diseases, affect which communities suffer the highest absolute mortality burden caused by inadequate water and sanitation (12). Correlations were higher for solid fuel use (0.83) and ambient urban PM (0.92), indicating that communities with highest exposure were the same as those with the largest associated mortality burden.
Municipio SES and Mortality Effects of Environmental Risks.
Indoor air pollution from solid fuels and unsafe water and sanitation had a disproportionate effect on child mortality in low-SES communities. For example, providing clean fuels and clean water and sanitation to all households would reduce child mortality by 4.4% (from 8.5 to 8.1 per 1,000) and by 6.2% (by 0.5 per 1,000) in the lowest-SES communities, respectively, but have almost no effects in the highest-SES municipios, which have already attained clean household environments. In contrast, the child mortality effects of urban PM had a positive association with community SES, because urban municipios have higher average community SES (Fig. 2). This pattern would remain even if child deaths caused by ambient PM pollution were also calculated in rural municipios, with a concentration of 10 μg/m3 PM2.5, as observed in rural U.S. areas (13).
The disparity-reducing effects of providing clean water, sanitation, and fuels outweighed the disparity-increasing effect of reducing urban PM, which had a much smaller effect on child mortality. As a result, the removal of all 3 risks would lead to a 10.6% (0.9 per 1,000) reduction in child mortality in the lowest-SES quintile, compared with 4.0% (from 3.5 to 3.3 per 1,000) in the best-off communities. However, because urban PM pollution has relatively large effects on adult mortality, and because its effects were highest in the better-off communities, the combined effects of the 3 exposures on life expectancy loss were U-shaped, with a mean effect of 4.4 months in the highest-SES quintile, 2.7 months in the middle quintile, and 3.7 months in the lowest-SES quintile.
Discussion
To our knowledge, a combined national and community-level analysis of the exposure to, and mortality burden associated with, environmental risks has not previously been presented. Despite several sources of uncertainty that affected our results (SI Text), this analysis showed that, nationally, urban PM pollution is responsible for more deaths than either indoor air pollution from household solid fuel use or unsafe water and sanitation individually. In contrast, the latter 2 risk factors, both with known interventions, caused more child deaths nationwide and had disproportionately larger mortality effects in a number of rural and predominantly indigenous communities.
There was a strong correlation between exposure to urban PM pollution and its mortality effects across municipios but a much weaker relationship for unsafe water and sanitation. This occurs because diarrhea deaths may be prevented with better water and sanitation or with better child nutrition and health care, making disparities in both factors significant determinants of disparities in absolute risk. In other words, the disparities in the mortality burden of water and sanitation were due to exposure disparities as well as to differentials in background mortality risk, which may, in turn, be affected by factors such as access to treatment or inadequate child nutrition.
Such a decoupling of exposure to environmental risks and their absolute mortality effects highlights the multiple opportunities, including both health and environmental interventions (e.g., better water and sanitation, child nutrition, and treatment access), for improving both aggregate health and reducing health disparities (12). For example, the recent declines in child diarrhea mortality in Mexico have been linked to the expansion of ORT and to accelerated provision of clean water (14). The community level assessment of exposure and absolute risk is especially relevant because environmental policy and management as well as health-care programs often involve infrastructure such as better sanitation or a health center, which are implemented at the community level.
At the same time, our finding of particularly large absolute effects in low-SES indigenous communities raises the question of why neither effective environmental nor effective health-care interventions have reached these marginalized communities. The potential for, and the shortage of, multiple interventions should provide a motivation for policy and program innovations in Mexico such as the Oportunidades program (which is meant to index the beneficiary communities and households based on their SES) to add environmental interventions to their efforts (15).
Despite the value of community-level analysis for program design, implementation, and evaluation, exposures to environmental risks and their mortality effects further vary across households and individuals within each community. If individual-level effects have the same SES association as observed at the community level, the total disparities in mortality effects may be even larger than those found in this analysis. Conversely, the relationship between SES and mortality effects of risk factor exposure within communities may be opposite the relationship between SES and mortality effects among communities. For example, low-SES individuals in urban communities may be exposed to higher concentrations of air pollutants [e.g., because of longer commute or homes and workplaces located in more polluted neighborhoods (16)] and/or experience larger absolute effects for each unit of exposure. In Mexico City, there is a slight negative correlation (−0.28) between annual mean concentration of fine PM and municipio SES (17).
We believe that reducing disparities in the disease burden attributable to multiple environmental factors, based on SES or other individual and community characteristics, should be an explicit policy objective in addition to reducing the total health effects of such exposures. For example, in Mexico, urban PM pollution was responsible for more deaths than solid fuel use and poor water and sanitation, but the latter two exposures disproportionately affected the poorest and most marginalized communities. Although a global, national (or even state-level) analysis would correctly identify the larger effect of urban PM on population health, it conceals the highly unequal distribution of the mortality burden caused by the household risk factors. This is likely to be the case for other risks or diseases where local ecology (e.g., malaria) or socioeconomic factors (e.g., solid fuel use associated with indigenous status) result in a large burden in population subgroups. Such findings demonstrate the importance of community-level monitoring and reporting. However, Mexico is exceptional in terms of availability of high-quality community-level data on health and exposure to risk factors among developing and even developed countries. Even in Mexico, data on exposure to many other risk factors is available only at the state or national level. Because of the cost of regular data collection at the community level, there is also a need for relatively low-cost methods that combine innovative data collection and models that predict risk factor exposure or disease outcomes at the community level (18–22).
Materials and Methods
We used the comparative risk assessment (CRA) framework to estimate the mortality effects of unsafe water and sanitation, indoor air pollution from solid fuel use, and ambient urban PM pollution during the period 2001–2005 (1). We provide a summary of methods in this section, with additional details provided in SI Text.
We assigned a composite SES score to each of the 2,454 municipios in Mexico based on average asset ownership and housing quality (indicators of wealth) and educational attainment in the municipio using data from the 2000 and 2005 censuses (see SI Text and Table S1). Some municipios have small populations, leading to unstable estimates of mortality rates. To decrease stochastic variability in mortality estimates for small municipios, we iteratively combined each municipio with population <10,000 with its neighboring municipio in the same state with the most similar SES until each merged municipio had a population of at least 10,000, resulting in 1,458 individual or combined “municipio units.” Units were classified into 5 SES quintiles of equal population (Fig. S2 and Table S2). All subsequent analyses were performed and results presented by municipio unit or by SES quintile.
CRA analysis estimates the reduction in mortality that would be expected if population exposure to a risk factor were at an alternative level. The alternative exposure was chosen as one that minimizes risks to health, which also allows for comparability across risks (Table 2). In addition, the following data are used for the CRA analysis: (i) current population distribution of exposure for each risk factor by municipio, (ii) relative risks for each disease causally associated with risk factor exposure, and (iii) total number of deaths from each disease affected by the risk factors by municipio. We calculated water and sanitation status and household solid fuel use by municipio using the 2000 and 2005 censuses, supplemented with a population health survey that provides state-specific data (Table 2 and Fig. S3). For ambient urban PM, we used data from air quality monitoring and an energy and economic model for the same time period. We used relative risks from the systematic reviews and meta-analyses conducted in the CRA project (Table S5), using the same proportional effects for all municipios. We obtained data on causes of death for the years 2001–2005 from the vital registration system, as recorded by the Ministry of Health (Secretaría de Salud). We first adjusted the cause-of-death distribution for incomplete cause-of-death information on the death certificate and for incomparability of cause-of-death assignment. We then spatially smoothed disease-specific child deaths using a Poisson general additive model (GAM) to adjust for stochastic variability. Finally, we adjusted total deaths by age for age misreporting and death underreporting in the vital registration using standard demographic techniques, as described elsewhere (10). Adult deaths were adjusted by state, and child deaths were adjusted by municipio. All adjustments to mortality data are described in detail in SI Text, total and cause-specific deaths are listed in Table S3, and child mortality rates are shown in Fig. S4.
Table 2.
Risk factors analyzed in this article, their exposure metrics, alternative exposure levels, disease outcomes, and data sources for relative risks and exposures (19, 24, 25)
| Risk factor | Exposure metric | Sources for exposure data | Alternative exposure | Disease outcomes affected | Sources for relative risks |
|---|---|---|---|---|---|
| Unsafe water and sanitation | Four categories of water and sanitation access (Table S4) | 2005 Census | Access to piped water and a flush toilet in all homes | Diarrheal disease | Systematic reviews of multicountry randomized controlled trials and observational studies (25) |
| Urban PM pollution | Average annual concentration of PM10 and PM2.5* | Municipal air quality monitoring systems, Global Model of Ambient Particulates (GMAPS)† | Annual average PM10 concentration of 15 μg/m3 and PM2.5 concentration of 7.5 μg/m3 ‡ | Acute respiratory infections in children <5 y old; lung cancer and cardiopulmonary diseases in adults ≥30 y old | Systematic review of cohort studies (19, 26) |
| Indoor air pollution from household solid fuel use | Household solid fuel use | 2000 Census, 2005 Encuesta Nacional de Salud y Nutrición | No household solid fuel use | Acute lower-respiratory infections in children <5 y old; chronic obstructive pulmonary disease in adults ≥30 y old | Systematic review and meta-analysis of cross-sectional, cohort and case-control studies (24) |
See Table S5 for relative risks.
*PM with an aerodynamic diameter of ≤10 μm and ≤2.5 μm, respectively.
†Validated annual concentration data for PM10 are available for 8 cities and for PM2.5 for only Mexico City (9). We used measured PM10 concentrations for these cities. We used PM2.5/PM10 ratios of 0.5 for cities in the central area of Mexico based on monitoring in Mexico City, 0.32 for Monterrey from early monitoring data, and 0.25 from measurements in Ciudad Juarez for the cities in the U.S. border to calculate annual average PM2.5 concentration (9, 27). For other cities with population >100,000, we used the estimated PM10 and PM2.5 concentrations from GMAPS, an energy and economic model developed at the World Bank (19). In the main analysis, we assumed that the remaining rural population was not exposed to urban PM pollution.
Table 1.
SES and health indicators for quintiles of municipios SES
| Parameter |
Municipio SES quintile |
All | ||||
|---|---|---|---|---|---|---|
| Lowest | 2nd | 3rd | 4th | Highest | ||
| No. of municipios | 1,369 | 658 | 301 | 80 | 46 | 2,454 |
| Average municipio population | 15,000 | 30,000 | 67,000 | 250,000 | 435,000 | 41,000 |
| No. of municipio units | 692 | 433 | 222 | 66 | 45 | 1,458 |
| Urban, % | 1 | 24 | 59 | 90 | 97 | 54 |
| Literate, % | 76 | 89 | 94 | 96 | 97 | 91 |
| Population >22 years of age who have completed secondary school, % | 13 | 21 | 31 | 39 | 47 | 30 |
| Population speaking an indigenous language, % | 26 | 4 | 2 | 2 | 1 | 7 |
| Child mortality rate (per 1,000 child-years) | ||||||
| All causes | 8.5 | 5.3 | 4.1 | 3.9 | 3.4 | 5.7 |
| Lower respiratory infections* | 1.0 | 0.4 | 0.3 | 0.3 | 0.2 | 0.5 |
| Diarrhea* | 0.8 | 0.3 | 0.2 | 0.1 | 0.1 | 0.3 |
| Cardiovascular disease* mortality (age-standardized, per 1,000) | 1.10 | 1.07 | 1.04 | 1.00 | 1.03 | 1.05 |
| Chronic obstructive pulmonary disease* mortality (age-standardized, per 1,000) | 0.18 | 0.16 | 0.19 | 0.19 | 0.17 | 0.18 |
| Population using solid fuels, % | 49 | 16 | 4 | 2 | 0 | 15 |
| Population exposed to each water and sanitation risk level (see Table S4 for definitions) | ||||||
| Low, % | 20 | 49 | 73 | 82 | 91 | 63 |
| Medium, % | 45 | 37 | 21 | 14 | 7 | 25 |
| High, % | 16 | 5 | 3 | 2 | 1 | 5 |
| Very high, % | 18 | 9 | 3 | 2 | 1 | 7 |
| Population living in municipios within ranges of mean annual ambient PM2.5 concentration | ||||||
| <15 μg/m3, % | 99 | 76 | 42 | 16 | 3 | 47 |
| 15–25 μg/m3, % | 0 | 5 | 30 | 25 | 13 | 15 |
| 25–39 μg/m3, % | 1 | 19 | 28 | 59 | 84 | 38 |
Quintiles were constructed based on cumulative poopulation, such that each quintile contains equal population but not an equal number of municipios.
*International classification of disease (ICD-10) codes for selected diseases are: lower respiratory infections, J10–J18, J20–J22; diarrhea, A01, A03–A04, A06–A09; cardiovascular disease, I10–I13, I20–I25, I30–I33, I38, I40, I42, I60–I69; chronic obstructive pulmonary disease, J40–J44.
We used the estimated exposure to the 3 risk factors and disease-specific mortality by municipio with relative risks for each disease affected by the risk factors to estimate the number of deaths in each municipio unit that would have been avoided had exposure to these environmental risks been reduced to the alternate exposure level (see SI Text). We also calculated the fraction of mortality attributed to the combined effects of these risk factors, accounting for deaths that may have been caused by more than one exposure. We used the age-specific mortality effects to estimate the effect of the environmental exposures on life expectancy using standard life-table methods (23). The effects on life expectancy (i.e., loss of life years) reflect the age distribution of deaths “brought forward” in the life table population by risk factor exposure. In addition to the effects of these exposures on life expectancy, we present their effects on annual child mortality rates, calculated as the number of deaths among children <5 years of age divided by the under-5 population.
Supplementary Material
Acknowledgments.
We thank Emmanuela Gakidou, Kenneth Hill, Christopher Paciorek, Kiran Pandey, and Alan Wagstaff for valuable discussions. This work was supported by funding for analysis of risk factor and mortality data from the Secretaría de Salud (Mexico) and by the National Science Foundation for the analytical component.
Footnotes
The authors declare no conflict of interest.
*In traditional epidemiological models, either the proportional risk of a disease associated with an exposure (the relative risk) varies among population subgroups, or the background disease rate varies among the subgroups. Together, these determine the differences in absolute risk caused by the exposure (i.e., susceptibility), which is the metric of interest from a public health perspective.
This article contains supporting information online at www.pnas.org/cgi/content/full/0808927105/DCSupplemental.
References
- 1.Ezzati M, et al. Comparative quantification of mortality and burden of disease attributable to selected risk factors. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global Burden of Disease and Risk Factors. Washington, DC: The World Bank; 2006. pp. 241–396. [PubMed] [Google Scholar]
- 2.O'Neill MS, et al. Health, wealth, and air pollution: Advancing theory and methods. Environ Health Perspect. 2003;111:1861–1870. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levy JI, Greco SL, Spengler JD. The importance of population susceptibility for air pollution risk assessment: A case study of power plants near Washington, DC. Environ Health Perspect. 2002;110:1253–1260. doi: 10.1289/ehp.021101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gakidou E, et al. Improving child survival through environmental and nutritional interventions: The importance of targeting interventions towards the poor. J Am Med Assoc. 2007;298:1876–1887. doi: 10.1001/jama.298.16.1876. [DOI] [PubMed] [Google Scholar]
- 5.Sexton K, Adgate JL. Looking at environmental justice from an environmental health perspective. J Expo Anal Environ Epidemiol. 1999;9:3–8. doi: 10.1038/sj.jea.7500021. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization/United Nations Children's Fund Joint Monitoring Programme for Water Supply and Sanitation. Meeting the MDG Drinking Water and Sanitation Target: The Urban and Rural Challenge of the Decade. Geneva: WHO; 2006. [Google Scholar]
- 7.Masera OR, Díaz R, Berrueta V. From cookstoves to cooking systems: The integrated program on sustainable household energy use in Mexico. Energy Sust Dev. 2005;IX:25–36. [Google Scholar]
- 8.Olaiz Fernández G, et al. Encuesta Nacional de Salud y Nutrición. Vol. 2006. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2006. [Google Scholar]
- 9.Instituto Nacional de Ecología. Segundo Almanaque de Datos y Tendencias de la Calidad del Aire en Seis Ciudades Mexicanas. Mexico, D.F.: Instituto Nacional de Ecología; 2004. [Google Scholar]
- 10.Stevens G, et al. Characterizing the epidemiological transition in Mexico: National and subnational burden of diseases, injuries and risk factors. PLoS Med. 2008;5:e125. doi: 10.1371/journal.pmed.0050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. World Health Statistics 2006. Geneva: WHO; 2006. [Google Scholar]
- 12.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Environmental Protection Agency. The Particle Pollution Report: Current Understanding of Air Quality and Emissions Through 2003. Research Triangle Park, NC: U.S. EPA; 2004. [Google Scholar]
- 14.Gutierrez G, et al. Impact of oral rehydration and selected public health interventions on reduction of mortality from childhood diarrhoeal diseases in Mexico. Bull World Health Organ. 1996;74:189–197. [PMC free article] [PubMed] [Google Scholar]
- 15.Leroy JL, Vermandere H, Neufeld LM, Bertozzi SM. Improving enrollment and utilization of the Oportunidades program in Mexico could increase its effectiveness. J Nutr. 2008;138:638–641. doi: 10.1093/jn/138.3.638. [DOI] [PubMed] [Google Scholar]
- 16.Buzzelli M, Jerrett M. Racial gradients of ambient air pollution exposure in Hamilton, Canada. Environ Plan A. 2004;36:1855–1876. [Google Scholar]
- 17.Stevens G, de Foy B, West JJ, Levy J. Developing intake fraction estimates with limited data: Comparison of methods in Mexico City. Atmos Environ. 2007;41:3672–3683. [Google Scholar]
- 18.Liu Y, Franklin M, Kahn R, Koutrakis P. Using aerosol optical thickness to predict ground-level PM2.5 concentrations in the St. Louis area: A comparison between MISR and MODIS. Remote Sensing Environ. 2007;107:33–44. [Google Scholar]
- 19.Cohen AJ, et al. Urban air pollution. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative Quantification of Health Risks. Geneva: WHO; 2004. pp. 1353–1434. [Google Scholar]
- 20.Rogers DJ, Randolph SE, Snow RW, Hay SI. Satellite imagery in the study and forecast of malaria. Nature. 2002;415:710–715. doi: 10.1038/415710a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ezzati M, Utzinger J, Cairncross S, Cohen AJ, Singer BH. Environmental risks in the developing world: Exposure indicators for evaluating interventions, programmes, and policies. J Epidemiol Commun Health. 2005;59:15–22. doi: 10.1136/jech.2003.019471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raso G, et al. An integrated approach for risk profiling and spatial prediction of Schistosoma mansoni-hookworm coinfection. Proc Natl Acad Sci USA. 2006;103:6934–6939. doi: 10.1073/pnas.0601559103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preston SH, Heuveline P, Guillot M. Demography. Malden, MA: Blackwell; 2001. [Google Scholar]
- 24.Smith KR, Mehta S, Maeusezahl-Feuz M. Indoor air pollution from household use of solid fuels. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative Quantification of Health Risks. Vol 2. Geneva: WHO; 2004. pp. 1435–1493. [Google Scholar]
- 25.Prüss Üstün A, Kay D, Fewtrell L, Bartram J. Unsafe water, sanitation and hygiene. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative Quantification of Health Risks. Vol 2. Geneva: WHO; 2004. pp. 1321–1352. [Google Scholar]
- 26.Woodruff TJ, Grillo J, Schoendorf KC. The relationship between selected causes of postneonatal infant mortality and particulate air pollution in the United States. Environ Health Perspect. 1997;105:608–612. doi: 10.1289/ehp.97105608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li W-W, et al. Analysis of temporal and spatial dichotomous PM air samples in the El Paso-Cd. Juárez air quality basin. J Air Waste Manag Assoc. 2001;51:1551–1560. doi: 10.1080/10473289.2001.10464377. [DOI] [PubMed] [Google Scholar]
- 28.Pope CA, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. J Am Med Assoc. 2002;287:1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.