Abstract
Background
Hamstring injuries are common especially in athletes. Partial and complete tears of the proximal origin may cause pain and functional loss.
Objective
To evaluate the results of surgical treatment for partial proximal hamstring tears.
Methods
Between 1994 and 2005, 47 athletes (48 cases, 1 bilateral) with partial proximal hamstring tears were operated on. The cases were retrospectively analysed. Before surgery, 42 of the patients had undergone conservative treatment with unsatisfactory results, whereas in five patients the operation was performed within four weeks of the injury.
Results
The mean length of the follow up was 36 months (range 6–72). The result of the operation was rated excellent in 33 cases, good in nine, fair in four, and poor in two. Forty one patients were able to return to their former level of sport after an average of five months (range 1–12).
Conclusion
In most cases, excellent or good results can be expected after surgical repair of partial proximal hamstring tears even after conservative treatment has failed.
Keywords: hamstring, muscle, partial tear, surgical treatment, injury
Hamstring muscle strain is one of the most common injuries in sports that involve running and jumping with rapid acceleration and deceleration.1 These injuries have been reported in various sports, such as soccer, Australian football, track and field, and rugby.2,3,4,5,6
The hamstring muscle group consists of the biceps femoris (long and short head), the semimembranosus, and the semitendinosus muscles. They are the major flexors of the knee and also aid in hip extension. These muscles attach proximally to the ischial tuberosity, except for the short head of the biceps femoris, which originates from the linea aspera and the lateral supracondylar ridge of the femur.7 The semitendinosus and the long head of the biceps femoris have a conjoint origin from the posteromedial aspect of the ischial tuberosity.8 The semimembranosus arises from a long flat tendon at the posterolateral aspect of the ischial tuberosity, lateral to the conjoint tendon of the biceps femoris and semitendinosus.8
Most injuries associated with hamstring muscles are strains and are treated by conservative means.1,9,10 The most serious injury is a complete rupture of the hamstring muscles. Despite the severity and potentially devastating effect of this injury, the results of surgical treatment can often be good.11,12,13
In this study we present a series of 48 cases of partial proximal hamstring tear and the results of surgical treatment. To our knowledge this is the largest reported series of this particular injury.
The study protocol was approved by the local hospital ethics committee of Satakunta Central Hospital, Pori, Finland.
Materials and methods
In this study, 47 consecutive athletes (48 cases, 1 bilateral) with surgically treated partial proximal hamstring tears were retrospectively analysed. Only partial proximal hamstring tears in athletes were included. There were 13 professional athletes (international level), 15 competitive level athletes, and 19 recreational athletes (table 1). Many of the athletes were referred from other centres after failed conservative treatment.
Table 1 Sports activities of the 28 professional and competitive level athletes with a partial proximal hamstring muscle tear.
| Activity | Professional | Competitive level |
|---|---|---|
| Soccer | 7 | 5 |
| Sprinting | – | 3 |
| Basketball | 1 | 1 |
| Ice hockey | 1 | 1 |
| Aerobics | 1 | – |
| Ballet | – | 1 |
| Figure skating | – | 1 |
| Finnish baseball | – | 1 |
| Judo | 1 | – |
| Karate | 1 | – |
| Middle distance running | – | 1 |
| Pole vault | 1 | – |
| Powerlifting | – | 1 |
| Total | 13 | 15 |
There were 32 men and 15 women with an mean age of 33 years (range 16–61). The mean age of the professional and competitive level athletes was 25 years and that of the recreational athletes 45 years. The right side was affected in 31 cases and the left in 17 cases.
In all patients, the injury mechanism was similar: an acute hyperflexion of the hip with the ipsilateral knee in extension often combined with a violent eccentric hamstring muscle contraction. Direct trauma to the ischial tuberosity was not reported in any of the cases. Forty six of the injuries occurred during sporting activities. The most common sport was soccer (16 cases). The two non‐sports related cases resulted from slipping on ice.
Ten of the 28 professional and competitive level athletes were able to participate in their sport before surgery. However, despite conservative treatment and rehabilitation, their athletic performance decreased and they suffered pain and weakness during athletic activity. Their symptoms prevented the remaining 18 athletes from participating.
All patients complained of pain and discomfort of the posterior thigh as well as weakness of the affected lower extremity. Other commonly reported symptoms were poor leg control and instability of the knee joint while walking. On clinical examination, tenderness to palpation was reported slightly below or at the ischial tuberosity. A haematoma was found in the posterior thigh in the patients that were seen early. In most chronic injuries, atrophy of the hamstring muscles was a common finding.
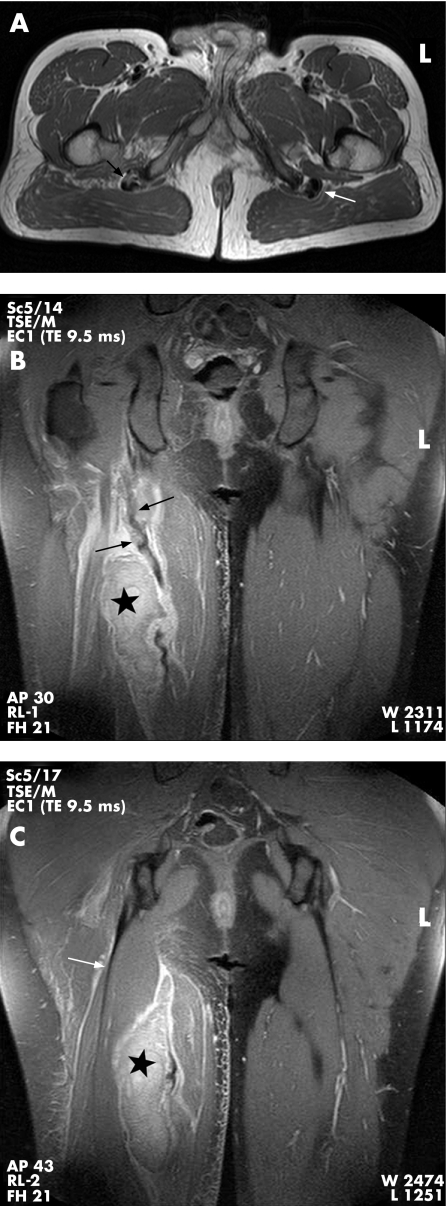
A diagnosis of partial tear of the proximal hamstring muscle was suspected on the basis of history, clinical examination, and radiological findings. Magnetic resonance imaging was performed to confirm the diagnosis and evaluate more precisely the extent of the injury (fig 1).
Figure 1 Magnetic resonance images of a patient with a partial proximal hamstring tear. (A) Axial image (proton density (PD) TR/TE 3217/15 milliseconds) with an intact left hamstring muscle origin (white arrow). A partially torn right anterior tendon with some intact fibres (black arrow head) can be seen at the level of the ischial tuberosity. (B,C) Coronal images (PD with fat suppression TR/TE 3200/9.5 milliseconds) showing torn tendon, indicated with black arrows, and a haematoma between the muscle bellies, indicated with a black star. The biceps femoris part of the conjoint tendon has remained intact (white arrow).
All of the patients were treated surgically between 1994 and 2005. Two patients were operated on twice. The delay from the injury to the operation varied from two weeks to nine years (mean 13 months; median six months). Five of the operations were performed within four weeks of the injury. The remaining patients had at first undergone conservative treatment with unsatisfactory results. At the time of the surgical treatment, none of the patients were satisfied with their athletic performance because of the symptoms of the proximal hamstring tear.
Spinal anaesthesia was used in all cases. The patient was placed in a prone position, the affected leg was draped to allow free movement, and the knee was kept in 30° of flexion. A vertical skin incision was made over the posterior thigh starting from the ischial tuberosity extending 10–15 cm distally. In two operations, a transverse gluteal crease incision was used. The lower edge of the gluteus maximus muscle was freed, and haemostasis was performed. The posterior cutaneous femoral nerve was identified and spared. Fasciotomy was continued distally approximately 15 cm from the origin of the hamstring muscles. The ischial tuberosity was exposed by retracting superiorly the inferior border of the gluteus maximus muscle. In acute injuries, the sciatic nerve was easily exposed lateral to the ischial tuberosity. In chronic cases, careful neurolysis was performed if the sciatic nerve was surrounded by adhesions and scar.
In 43 cases, the torn tendon(s) was reattached using suture anchors (Mitek, Norwood, Massachusetts, USA). The bony surface of the ischial tuberosity was debrided, and one or two anchors were used to reattach the tendon(s) usually slightly distal and medial to the original site of the ischial tuberosity to avoid tension. However, in operations performed early, the re‐fixation could be carried out in the anatomical location. In cases in which the torn tendon(s) was distally retracted, the muscles were first mobilised to achieve tension‐free contact with the ischial tuberosity. In five cases, the fixation was performed by suturing the torn tendon(s) to the periosteal bone and to the proximal tendon stump.
An elastic bandage was used for one to two weeks after the operation. No immobilisation, casts, or orthoses were used. The patients were allowed to begin partial weight‐bearing within two weeks of the operation, and full weight bearing was allowed two to four weeks after surgery. Sitting was avoided for the first two weeks. Swimming and water training was allowed two to three weeks after surgery. Isometric muscle exercises and cycling, with gradually increasing time and intensity, were begun after four to six weeks. Heavier weight training was started two months and running two to four months after the operation.
The patients were followed at our outpatient clinic. During the first four to five months, there were monthly routine visits, and after that if necessary. Additional long term follow ups were scheduled for study purposes. At the most recent follow up, the patients were asked about possible symptoms (pain, weakness, stiffness), overall satisfaction, and their return to pre‐injury level of sport.
The result was graded as excellent if the patient was asymptomatic and able to return to the pre‐injury level of sporting activity. If there were minor symptoms in the affected leg during sport but the patient was able to return to the pre‐injury level of sport, the result was classified as good. A classification of fair was assigned to the result when moderate training was possible but the patient was unable to carry out strenuous exertion. Finally, the result was classified as poor when the patient had disturbing symptoms even in activities of daily living.
Results
In all 48 cases, a partial proximal hamstring tear was found during surgery. The conjoint tendon of the biceps femoris and the semitendinosus was involved in all cases. In 17 cases, the conjoint tendon alone was torn and the semimembranosus tendon was intact, whereas in 31 cases the semimembranosus tendon and the conjoint tendon were both torn. However, in all 31 cases either the medial or the lateral part of the conjoint tendon remained attached to the ischial tuberosity. In other words, no complete ruptures of the hamstring muscle group were included in the study. Two examples of the surgical findings are presented as schematic drawings (figs 2 and 3).
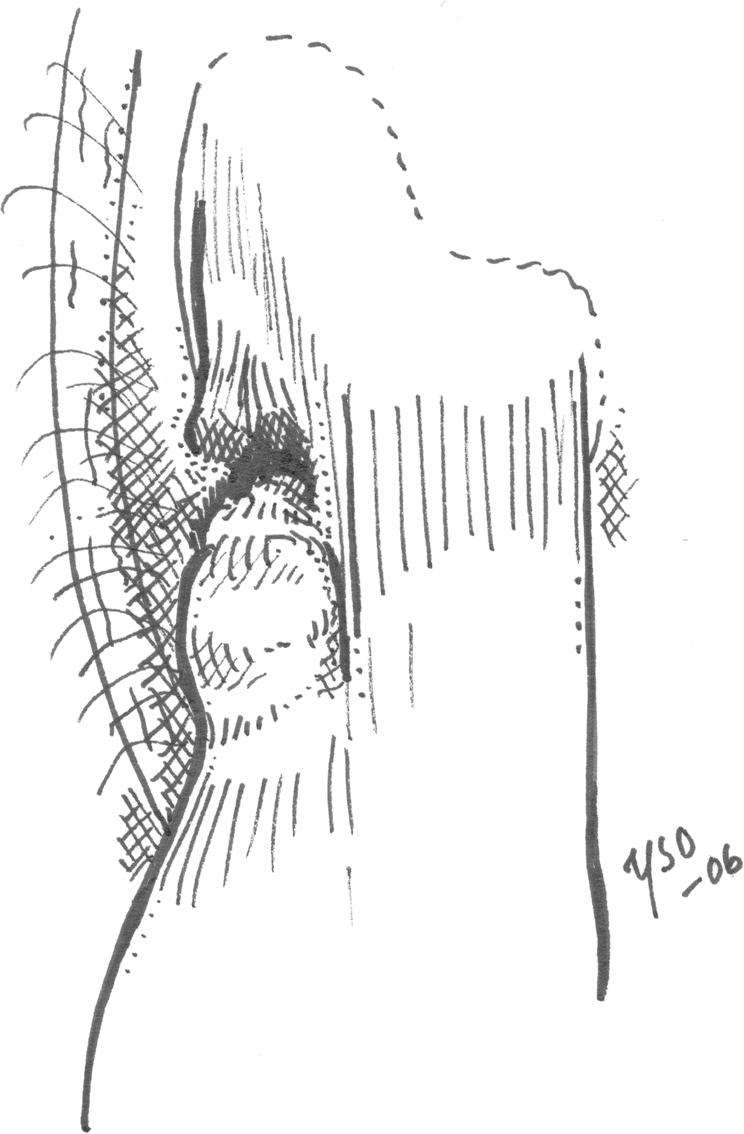
Figure 2 A schematic drawing of partial rupture of left hamstring muscle origin. The semimembranosus tendon and the lateral part of the conjoint tendon of biceps femoris and semitendinosus have torn away from the ischial tuberosity. The medial part of the conjoint tendon has remained intact. The sciatic nerve curves obliquely beneath the hamstring muscles from the lateral side of the ischial tuberosity.
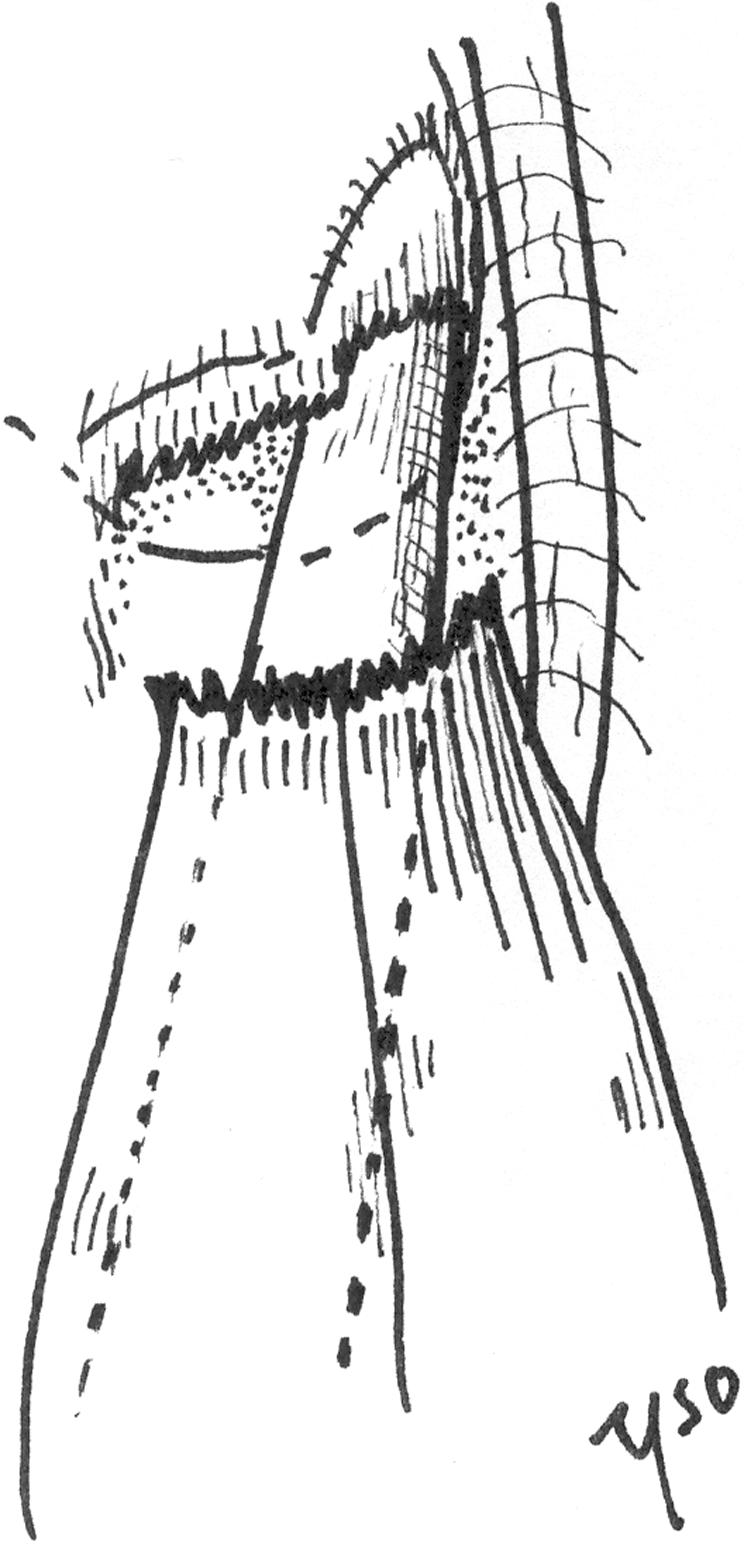
Figure 3 A schematic drawing of partial rupture of the right hamstring muscle origin. The conjoint tendon of biceps femoris and semitendinosus has completely torn away from the ischial tuberosity. The semimembranosus tendon has remained intact.
The mean length of the follow up was 36 months (range 6–72; median 36). The final outcome of the operation was evaluated to be excellent in 33 (69%) cases, good in nine (19%), fair in four (8%), and poor in two (4%) (table 2). Forty one patients (87%; 42 cases, one bilateral with both excellent results) were able to return to their pre‐injury level of sports activity after surgical treatment. This took a mean of five months (range 1–12).
Table 2 Final results of the surgical treatment in 48 cases of partial proximal hamstring tears.
| Group | Excellent | Good | Fair | Poor |
|---|---|---|---|---|
| Professional athletes | 10 | 1 | 2 | – |
| Competitive level athletes | 10 | 3 | 2 | – |
| Recreational athletes | 13 | 5 | – | 2 |
| Total | 33 | 9 | 4 | 2 |
All 47 patients felt that they had benefited from the surgery, and their athletic performance as well as the strength of the operated thigh had improved after the operation. However, the six athletes with a fair or poor result were not satisfied with their final outcome.
Two professional athletes underwent re‐operation. The first one had suffered a new hamstring injury of the operated proximal thigh. After unsuccessful conservative treatment, a second operation was performed two years after the primary operation. A new partial rupture of the proximal hamstring muscle group was surgically treated and the patient was able to return to the pre‐injury level of sport seven months after this second operation. The final outcome was evaluated to be excellent.
The other professional athlete had a second operation because of an unsatisfactory result after the first operation. He was not able to return to his pre‐injury level of sport despite the re‐operation and suffered from continuing pain and weakness of the posterior thigh in strenuous sport activities. He finished his professional career but had no symptoms in recreational sports. The final outcome was graded as fair.
After the operation, there was one superficial wound infection, which was effectively treated with antimicrobial drugs. One patient had hypertrophic scarring, and one patient suffered from hyperesthesia of the incision area probably because of a partial injury of the posterior cutaneous femoral nerve.
What is already known on this topic
Even though hamstring injuries are common and troublesome in athletes, there are no studies concerning only the surgical treatment of partial proximal hamstring muscle tears
Discussion
Hamstring strains and tears are common and can cause considerable morbidity, especially in athletes.14 Experimental and clinical studies have shown that hamstring muscle strains usually occur at the myotendinous junction.15 Most heal with time and generally approved conservative methods.10
If the tear is located at the tendinous part of the proximal hamstring muscles, it may have a tendency to remain disabling in spite of conservative treatment. This kind of partial proximal hamstring tear in top level athletes such as soccer or track and field professionals may result in decreased athletic performance and prolonged time out from sports activities because of persistent pain and weakness.
To our knowledge there are only a few previously published clinical studies in the English literature on the surgical treatment of partial proximal hamstring tears.11,16,17 In these series, most patients have had a complete rupture of the proximal hamstring muscles, and only a few cases with partial tears have been included. The present study was performed to evaluate the usefulness of surgical treatment in partial proximal hamstring tears in athletes. In our study, all patients were actively involved in sports, and many were top level athletes.
The typical hamstring injury mechanism is a rapid flexion of the hip combined with knee extension in which the muscle develops tension while lengthening.1 As noted in the present study, partial tears of the proximal hamstring muscles can occur in a variety of sports activities. However, in all injuries the mechanism was flexion of the hip with the ipsilateral knee in extension often combined with a violent eccentric hamstring muscle contraction. This kind of history should lead the doctor to suspect a proximal hamstring tear.
In this study, the delay from the injury to surgery was rather long in most cases with an average of 13 months (median six months). In the acute phase, underestimation of the severity of the injury was often the case, as well as poor awareness by the primary care doctors of the treatment options of partial proximal hamstring tears. Therefore the operative treatment was often delayed even when the symptoms persisted despite conservative treatment and the athletes were not able to participate in their sports activities.
In five of the six cases in which the final outcome was graded as fair or poor, the delay from the injury to surgery was 6–34 months (mean 21). In the sixth case, in which the result was evaluated to be fair, the surgical repair was performed just over a month after the injury. It seems that a long delay from injury to surgery may have an adverse effect on the result. However, there were 17 cases in which the result was excellent or good despite the delay to surgery being over six months.
According to our results, it seems that excellent or good outcomes may be expected after surgical repair in most cases of partial proximal hamstring tear. However, surgery is technically easier in the acute phase and there is often no need for neurolysis of the sciatic nerve. If conservative treatment is chosen, the possibility of surgical treatment should still be kept in mind, especially if the symptoms are prolonged. The awareness of this particular type of injury and the option of surgical repair of partial proximal hamstring tears is of great importance. An active diagnostic and treatment approach is needed as partial proximal hamstring tears may even threaten the career of an athlete. However, further studies are needed to evaluate who should be treated surgically and at which point surgery should be considered.
What this study adds
Excellent or good results can be expected after surgical repair in most cases of partial proximal hamstring tear
Acknowledgements
This study was supported financially by the Satakunta Central Hospital District.
Footnotes
Competing interests: none declared
References
- 1.Kujala U M, Orava S, Järvinen M. Hamstring injuries. Current trends in treatment and prevention. Sports Med 199723397–404. [DOI] [PubMed] [Google Scholar]
- 2.Volpi P, Melegati G, Tornese D.et al Muscle strains in soccer: a five‐year survey of an Italian major league team. Knee Surg Sports Traumatol Arthrosc 200412482–485. [DOI] [PubMed] [Google Scholar]
- 3.Woods C, Hawkins R D, Maltby S.et al The Football Association Medical Research Programme: an audit of injuries in Professional football: analysis of hamstring injuries. Br J Sports Med 20043836–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997–2000. Br J Sports Med 20023639–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennell K L, Crossley K. Musculoskeletal injuries in track and field: incidence, distribution and risk factors. Aust J Sci Med Sport 19962869–75. [PubMed] [Google Scholar]
- 6.Brooks J H M, Fuller C W, Kemp S P T.et al Epidemiology of injuries in English professional rugby union: part 2 training injuries. Br J Sports Med 200539767–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore K L.Clinically oriented anatomy. 3rd ed. Baltimore: Williams & Wilkins, 1992, 423 (chapter 5).
- 8.Bencardino J T, Mellado J M. Hamstring injuries of the hip. Magn Reson Imaging Clin N Am . 2005;13677–690. [DOI] [PubMed]
- 9.Agre J C. Hamstring injuries. Proposed aetiological factors, prevention, and treatment. Sports Med 1985221–33. [DOI] [PubMed] [Google Scholar]
- 10.Järvinen T A H, Järvinen T L N, Kääriäinen M.et al Muscle injuries: biology and treatment. Am J Sports Med 200533745–764. [DOI] [PubMed] [Google Scholar]
- 11.Brucker P U, Imhoff A B. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports TraumatolArthrosc 200513411–418. [DOI] [PubMed] [Google Scholar]
- 12.Klingele K E, Sallay P I. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med 200230742–747. [DOI] [PubMed] [Google Scholar]
- 13.Chakravarthy J, Ramisetty N, Pimpalnerkar A.et al Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med 200539569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clanton T O, Coupe K J. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg 19986237–248. [DOI] [PubMed] [Google Scholar]
- 15.Noonan T J, Garrett W E., Jr Injuries at the myotendinous junction. Clin Sports Med 199211783–806. [PubMed] [Google Scholar]
- 16.Orava S, Kujala U M. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med 199523702–705. [DOI] [PubMed] [Google Scholar]
- 17.Sallay P I, Friedman R L, Coogan P G.et al Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med 199624130–136. [DOI] [PubMed] [Google Scholar]