Abstract
Objective
To determine whether being admitted with major trauma to an emergency department outside rather than within working hours results in an adverse outcome.
Methods
The data were collected from hospitals in England and Wales participating in the Trauma Audit and Research Network (TARN). Data from the TARN database were used. Admission time and discharge status were cross matched, and this was repeated while controlling for Injury Severity Score (ISS) values. Logistic regression was carried out, calculating the effects of Revised Trauma Score (RTS), ISS, age, and time of admission on outcome from major trauma. This allowed observed versus expected mortality rates (Ws) scores to be compared within and outside working hours. As much of the RTS data were missing, this was repeated using the Glasgow Coma Score instead of RTS.
Results
In total, 5.2% of people admitted "out of hours" died, compared with 5.3% of people within working hours, and 12.2% of people admitted outside working hours had an ISS score greater than 15, compared with 10.1% admitted within working hours. Outcome in cases with comparable ISS values were very similar (31.1% of cases with ISS >15 died out of hours, compared with 33.5% inside working hours.) The subgroup of data with missing RTS values had a significantly increased risk of death. Therefore, GCS was used to calculate severity adjusted odds of death instead of RTS. However, with either model, Ws scores were identical (both 0%) within and outside working hours.
Conclusions
Out of hours admission does not in itself have an adverse effect on outcome from major trauma.
Keywords: TRISS, out of hours, trauma audit
Trauma remains the third most common cause of death worldwide and the leading mode of death in the first four decades of life. In major trauma in the UK, the majority of patients sustain blunt injuries, with road traffic accidents being the most common cause of injury (36.3% of blunt injuries). Small falls (<2 m) account for 33.1% of blunt trauma, the second most common cause of injury.1
The Royal College of Surgeons believed that improvements to trauma management would significantly reduce mortality and in 1988 suggested a number of changes to both pre‐hospital and hospital care,2 indicating that implemented changes needed to be assessed to measure their effectiveness.
One way to assess trauma care is to compare the actual outcome of trauma against the predicted outcome. The outcome from major trauma (death or survival) can be predicted using the Trauma and Injury Severity Score (TRISS) method. This uses a measure of the anatomical severity of injury (the Injury Severity score; ISS) with a measure of the physiological disturbance which results from the injury (the Revised Trauma Score; RTS). These can be combined with information on the patient's age and the type of injury (penetrating or blunt) to determine the probability of survival. This has been described elsewhere.3 Although it has been criticised, TRISS remains a standard method for the prediction of survival from major trauma, and has been used for this purpose since 1988 in the Trauma Audit and Research Network (TARN) in the UK and in the Major Trauma Outcome Study in the USA.
It has been recorded that mortality from major trauma is worse during the night and at weekends compared with working hours. We conducted a literature review on the relationship between time of admission and outcome from major trauma, which revealed that this topic had not been researched extensively, nor had large databases been examined. One article found that the relationship could be due to higher ISS and increased frequency of penetrating trauma suffered outside working hours, as well as the increased volume of major trauma recorded at night and the weekend.4
The increased amount of major trauma recorded outside working hours may put increased pressure on the reduced resources of the night and weekend shifts, which could then lead to a knock on effect on outcome from major trauma. It is necessary to have access to rapid imaging and an appropriate surgical team for patients with severe haemorrhage, while the provision of critical care and imaging is necessary to manage any sequelae of major trauma. The, at best, delayed availability of surgeons, imaging, and inter‐ward transfer could, potentially, hamper treatment outside working hours. Some research has been carried out into the effect of night shifts on the performance of doctors in the emergency department, finding that physicians working consecutive night shifts have a much greater decline in cognitive function than those working day shifts.5 Doctor errors could therefore be more likely "out of hours". Acute admissions at weekends have been shown to suffer increased mortality rates compared with those admitted during weekdays. This correlates with a decreased level of staffing at weekends. It is suggested that the increased workload and the unpopularity of working weekends could affect the standard of care during this period.6 In a different field of medicine, it has been reported that perinatal mortality is higher in babies born at night.7 The seniority of the doctor attending the patient may affect the immediate treatment of patients in accident and emergency, and a lack of senior staff present in the department out of hours could adversely affect outcome from major trauma. Although one study has reported that the mortality of injured patients is lower if treated by a more senior doctor,8 the seniority of doctor has not been found to correlate significantly with any improvement in the observed versus expected number of survivors per 100 cases (Ws statistic).9
The relationship between time of admission and factors such as ISS, RTS, and age was tested to see if admission out of hours has an independent effect on mortality after major trauma. Our null hypothesis was that there is no statistically significant difference in case fatality out of hours compared with within working hours.
METHODS
Data and inclusion criteria
Cases were included in the study, which comprised patients presenting between 1999 and 2001, inclusive and submitted by participating hospitals to TARN (which includes 50% of trauma receiving hospitals in England and Wales). Eligible patients were those of any age who sustained injury resulting in immediate admission to hospital for 3 days or longer, admission to an intensive care or a high dependency unit, or death within 93 days. Excluded cases were patients over 65 years of age with isolated fracture of the femoral neck or pubic ramus, and those with single uncomplicated limb injuries. Any patients transferred between hospitals were also excluded from the study. Details of TARN have been described elsewhere,9 Working hours were defined as Monday–Friday 0900–1700. All other times were defined as out of hours.
Initial comparisons
Initial analysis of outcome of trauma inside and outside working hours was carried out using a 2×2 contingency table to show crude mortality within and outside working hours using χ2 testing to show statistical significance. Further analysis was performed by cross tabulation between ISS converted into a categorical variable with three bands (1–8, 9–15, and >15), and time of admission.
Multivariate analysis
The data were entered into a logistic regression model to look at the outcome against the categorical variables of age and admission time and the continuous variables of revised trauma score and injury severity score. Area under the receiver operator curve (AROC) was used to demonstrate model performance.
As the full RTS was not always available, owing to respiratory rates frequently not being recorded, an analysis of missing data was carried out to see if they varied significantly from the data used in the analysis (that is, complete data). If any difference was shown, then it was planned a priori to use GCS instead of RTS to increase the number of cases in the model. The performance of the England and Wales trauma system within and out of hours was then compared using a further standardisation for case mix, which TARN routinely uses to benchmark trauma system performance – the “Ws” score, or observed versus expected mortality rate. As part of a sensitivity analysis that the effect of out of hours may be most prominent at the weekend this last Ws scoring was repeated by reclassifying the data, with 0900 Monday to 0900 Saturday being defined as working hours
RESULTS
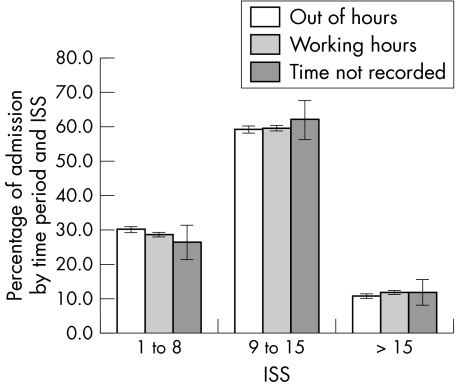
A total of 13 804 patients were admitted within working hours, compared with 27 062 patients admitted outside working hours (see table 1) Of patients admitted on weekdays, 5.3% (734 of 13 804) died, compared with 5.2% (1412 of 27 062) deaths outside working hours (χ2 = 0.17, p = 0.69). There was no recorded time of arrival for 668(1.6% of the dataset). Of the patients seen outside working hours, 12.2% had an ISS >15 compared with 10.1% of the patients who arrived within working hours (χ2 = 38.4, p<0.001, 1 degree of freedom). The proportions of different ISS ranges presenting within and outside working hours are shown (fig 1). There was no statistically significant difference in the breakdown of ISS scores <15 between the two time periods.
Table 1 Table of admission time against mortality from major trauma.
| Alive | Dead | Total | ||||
|---|---|---|---|---|---|---|
| Working hours | 13 070 94.7) | 734 (5.3) | 13 804 | |||
| "Out of hours" | 25 650 (94.8) | 1412 (5.2) | 27 062 | |||
| Not recorded | 625 (93.6) | 43 (6.4) | 668 | |||
| Total | 39 345 (94.7) | 2189 (5.3) | 41 534 |
Results are given as n (%).
Figure 1 Graph of ISS against admission time.
Table 2 compares outcome from major trauma with hour of admission and ISS scores, showing that of the 1393 people admitted within working hours with an ISS >15, 467 (33.5%) people died. Of the 3291 people admitted outside working hours, 1025 died (31.1%). Therefore, despite the fact that the majority of people who died with ISS >15 did so outside working hours (68.7%), this was due to the increased number of patients with ISS >15 outside working hours. The proportion of people who survive with ISS >15 was higher outside working hours. However, this difference was not statistically significant (χ2 = 22.44, p = 0.12)
Table 2 Table of admission time against major trauma mortality with comparable ISS values.
| Deaths, n of total (%) | ||||
|---|---|---|---|---|
| 1 to 15 | Working hours | 267 of 12 411 (2.2%) | ||
| "Out of hours" | 387 of 23 771 (1.6%) | |||
| >15 | Working hours | 467 of 1393 (33.5%) | ||
| "Out of hours" | 1025 of 3291 (31.1% |
Multifactorial results
From the 41 534 cases in the study, 12 624 (31%) were missing from the multifactorial analysis using logistic regression, owing to RTS values not being available. Values for all the other variables in the logistic regression model had no missing data.
Table 3 demonstrates the odds ratio (OR) for each independent variable. This demonstrates the effect each variable has on the odds of death with its introduction into the logistic regression model. The first row of figures is empty as this is the baseline age range. All other age values are compared with this. The time of admission reflects the effect of admission outside working hours on odds of death. It is evident that there is not a large effect on the odds of death (OR = 0.99, 95% confidence interval (CI) 0.85 to 1.16, p = 0.934). Age, ISS, and RTS all had a highly statistically significant relationship with mortality from major trauma with p values <0.001. The AROC for this model was 0.94.
Table 3 Odds ratios for factors predicting death after major injury, and for predicting death after major injury, using GCS in place of RTS.
| Variable | OR | 95% CI | p | |||
|---|---|---|---|---|---|---|
| Using RTS | ||||||
| Age (0–54 years) | Baseline | |||||
| Age (55–64 years) | 2.9 | 2.13 to 3.94 | <0.001 | |||
| Age (65–74 years) | 7.2 | 5.49 to 9.41 | <0.001 | |||
| Age (75–84 years) | 19.22 | 15.18 to 24.36 | <0.001 | |||
| Age (>85 years) | 47.29 | 37.05 to 60.38 | <0.001 | |||
| ISS | 1.15 | 1.14 to 1.16 | <0.001 | |||
| RTS | 0.38 | 0.35 to 0.41 | <0.001 | |||
| Time of admission* | 0.99 | 0.85 to 1.17 | 0.924 | |||
| Using GCS | ||||||
| Age (0–54 years) | Baseline | |||||
| Age (55–64 years) | 2.79 | 2.13 to 3.66 | <0.001 | |||
| Age (65–74 years) | 6.55 | 5.13 to 8.35 | <0.001 | |||
| Age (75–84 years) | 18.12 | 14.67 to 22.39 | <0.001 | |||
| Age (>85 years) | 40.81 | 32.82 to 50.75 | <0.001 | |||
| GCS | 0.71 | 0.70to 0.73 | <0.001 | |||
| ISS | 1.14 | 1.13 to 1.14 | <0.001 | |||
| Time of admission* | 0.92 | 0.80 to 1.06 | 0.232 |
*Out of hours.
Analysis of missing data
The proportion of patients with missing RTS data presenting out of hours was 65.1%. The mean ISS and age were identical in cases with and without missing data (ISS 9 and 46 years). However, 6.8% of people with RTS data missing died, compared with 4.6% of people with complete data (χ2 = 85.4, p<0.001).
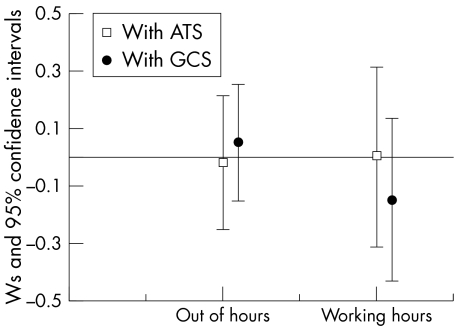
Owing to the marked increase in deaths from trauma in patients with missing data, a second multifactorial analysis was performed, using GCS instead of RTS, resulting in the number of cases not included being reduced to 4277 of 41 534 (10.3%). The OR of time of admission out of hours in the new multivariate analysis was 0.92 (95% CI 0.80 to 1.06, p = 0.232, AROC = 0.94). However, once this was further standardised for case mix the observed versus expected mortality rates were similar within and out of hours whichever model was used (fig 2). When the patients were reclassified, with 9am–9am Monday–Saturday defined as within hours, the result was identical (data not shown).
Figure 2 Standardised observed versus expected mortality rates (Ws scores) for patients presenting within and out of hours.
DISCUSSION
This analysis has shown no statistically significant relationship between time of admission and mortality from major trauma once other confounding variables (GCS, ISS, and age) were accounted for via multiple linear logistic regression. The null hypothesis, as described in the introduction, stated that there is no relationship between time of admission and case fatality from major trauma, and is supported.
The other variables (age, ISS, and GCS) have a statistically significant effect on outcome from major trauma (p<0.001). This was to be expected as these variables form the basis for the TRISS method of predicting the outcome from major trauma. Greater age had an increasing effect on odds of death from major trauma, as can be seen from the OR values, which escalate with increasing age. ISS had an OR of 1.1 and GCS had an OR of 0.71, illustrating the inverse relationship between GCS and outcome from major trauma.
The greater number of deaths seen out of hours (1412 versus 734) is due to the much larger number of patients admitted outside our definition of working hours. This increase in admissions could be explained by the fact that there are 128 hours per week out of hours compared with only 40 within hours. Any other reasons for the increased number of cases cannot be proven with this analysis.
Analysis of ISS against time of admission found that a greater percentage of patients admitted within out of hours have ISS scores >15 (12.2% v 10.1%). This is statistically significant. Once ISS values had been compared with hour of admission and outcome from major trauma, the percentage of people dying outside working hours with ISS >15 was found to be less than the percentage of people dying within working hours (31.1% v 33.5%). This analysis is a better indicator of the differences between the two admission periods, and shows that there may be little difference in terms of standard of care, as people with similar injury severity scores are faring equally well within and outside working hours, in agreement with the original null hypothesis. Although the outcome from major trauma seemed better outside working hours in this analysis, going against the original hypothesis that patients' outcome from major trauma will be worse outside working hours, there was no significant difference between the two time periods.
It is not apparent why the differences previously noted between care out of hours and within normal working hours should have no effect on case fatality from major trauma in our multivariate analysis. However, various articles have alluded to an equality of care out of hours. It has already been mentioned that the observed versus expected number of survivors per 100 cases (Ws statistic) is not significantly different in patients being seen first by consultants.9 Therefore, their decreased availability out of hours may not have a great impact on outcome from major trauma. One study found that there was no difference in mortality between patients treated by in house and on call surgeons, provided that the surgeon arrived within 15 minutes. Certain subsets of patient, however, may benefit from the presence of in house surgeons.10
There are some potential problems with the analysis. The sample was large, although the large amount of missing RTS data means that GCS was used in its place for the final analysis. The accuracy of GCS in predicting outcome from trauma was good (p<0.001). Therefore, its use, by increasing the number of cases in the model, seems justified. The data were only analysed in terms of outcome from major trauma within and outside working hours. It is possible that there might be a difference between weekdays and weekends as out of hours at a weekend covers all 24 hours of the day whereas on a weekday, out of hours covers just 16 hours. However, the sensitivity analysis (data not shown), redefining working hours as 0900 Monday to 0900 Saturday, gave results identical to those presented in this paper. As mentioned earlier, there is a longer time period within our definition of out of hours, creating a larger pool of data. However, this should not have affected the proportional analyses used in this report.
Patients presenting out of hours may differ greatly to those presenting inside the time period 0900–1700. One study found that over 50% of the 15–24 year age group attend out of hours. As this age group tends to stay out late at night and have alcohol related injuries such as assault or road traffic accidents, this may cause a greater degree of major trauma outside working hours.11 This finding agrees with another study, which found that young men are at a particularly higher risk of suffering road traffic accidents at night, suggesting that the roles of lifestyle, peer pressure, and inexperience may make this age group particularly at risk of serious accidents. A peak of fatal road traffic accidents was found at night.12 It is interesting in our study that the mortality of minor trauma (ISS<16) was higher during than outside working hours(2.0 v 1.5%, p<0.001). This almost certain reflects the higher mortality of older patients, who tend to present during working hours.
The influence of the time of day on outcome from major trauma has been demonstrated by one preliminary study that found that the outcome from major trauma is worse around the early morning (0500–0700), perhaps due to depleted levels of cortisol (G McMahon, personal communication). Therefore, it may have been beneficial to look at specific hours in terms of relationships with outcome from major trauma.
Several of criticisms have been levelled at TRISS methodology in terms of its accuracy in predicting outcome from major trauma, and its inability to predict resource utilisation, which would help in effective trauma centre quality improvement programmes.13 However, this report is not strictly concerned with TRISS, but rather with the ability of multiple linear logistic regression to determine whether time of admission is a significant factor in determining outcome from major trauma. The accuracy of ISS and GCS in predicting outcome from major trauma may therefore influence the accuracy of the model in calculating the effect of time of admission on outcome from major trauma. As ISS does not assess more than one severe injury from the same body part, its evaluation of trauma severity might be improved. GCS has not been used by itself in the past to predict outcome from major trauma. However, GCS and ISS both proved statistically significant in predicting outcome from major trauma. This is not surprising as the GCS, by its weighting, is the major component of the RTS.
This study did not differentiate patients with penetrating trauma from those with blunt trauma. However, owing to the small proportion of patients with penetrating trauma admitted to the database hospitals, it was not felt that this would have a statistically significant effect on the results.
CONCLUSIONS
A greater percentage of trauma patients admitted outside working hours (outside Monday–Friday 0900–1700 suffer ISS scores >15 (12.2% v 10.1%). However out of hours presentation does not increase mortality from major trauma once other confounding variables (GCS, ISS, and age) had been accounted for via multiple linear logistic regression.
Abbreviations
AROC - area under the receiver operator curve
ISS - Injury Severity Score
RTS - Revised Trauma Score
TARN - Trauma Audit and Research Network
TRISS - Trauma and Injury Severity Score
Ws - observed versus expected mortality
Appendix
PARTICIPATING HOSPITALS SINCE 1989
Addenbrooke's Hospital, Cambridge; Heatherwood & Wexham Park Hospital, Slough; Rotherham District General Hospital; The Princess Royal Hospital, Shropshire; Airedale General Hospital, Yorkshire; Hillingdon Hospital, Middlesex; Royal Albert Edward Infirmary, Wigan; Torbay Hospital, Devon; Arrowe Park Hospital, Merseyside; Hinchingbrooke Hospital, Cambridgeshire; Royal Berkshire Hospital, Reading; Trafford General Hospital, Manchester; Ashford General Hospital, London; Homerton Hospital, London; Royal Bolton Hospital, Farnworth; University Hospital, Lewisham, London.
Atkinson Morley's Hospital, London; Hope Hospital, Salford; Royal Cornwall Hospital, Truro; University Hospital of Hartlepool, Barnsley; District General Hospital, Yorkshire; Huddersfield Royal Infirmary; Royal Devon & Exeter Hospital; University Hospital of North Staffordshire; Basildon Hospital, Essex; Hull Royal Infirmary, North Humberside; Royal Gwent Hospital, Newport; University Hospital of North Tees, Cleveland; Bassetlaw Hospital, Nottinghamshire; Ipswich Hospital, Suffolk; Royal Hallamshire Hospital, Sheffield; University Hospital of Wales, Cardiff; Bedford Hospital; James Cook University Hospital, Cleveland; Royal Hampshire County Hospital, Winchester; University Hospital, Aintree, Liverpool; Birmingham Heartlands Hospital; James Paget Hospital, Norfolk; Royal Lancaster Infirmary; Walton Centre for Neurology, Liverpool; Blackburn Royal Infirmary, Lancashire; Jersey General Hospital; Royal Liverpool Childrens Hospital, (Alder Hey); Wansbeck General Hospital, Northumberland; Blackpool Victoria Hospital; John Coupland Hospital; Royal Liverpool University Hospital; Warrington Hospital, Cheshire Booth Hall Children's Hospital, Manchester; John Radcliffe Hospital, Oxfordshire; Royal London Hospital; Warwick Hospital, Warwick; Bradford Royal Infirmary, Yorkshire; Kent & Canterbury Hospital; Royal Manchester Children's Hospital, Pendlebury; Waterford Regional Hospital, Ireland; Bristol Royal Infirmary; Kent & Sussex Hospital; Royal Oldham Hospital; Watford General Hospital, Herts; Bromley Hospital, Kent Kettering General Hospital, Northamptonshire; Royal Preston Hospital; West Cumberland Hospital, Cumbria; Broomfield Hospital; Essex Kings College Hospital, London; Royal Shrewsbury Hospital, Shropshire; West Middlesex University Hospital; Burnley General Hospital; Kings Mill Hospital, Nottinghamshire; Royal Surrey County Hospital; West Wales General Hospital, Dyfed.
Calderdale Royal Hospital, Halifax; Leeds General Infirmary; Royal Sussex County Hospital, Brighton; Weston General Hospital, Avon; Cheltenham General Hospital; Leicester Royal Infirmary; Royal United Hospital, Bath; Weymouth & District Hospital, Dorset; Chesterfield & Nth Derbyshire Royal Hospital; Leigh Infirmary; Royal Victoria Hospital, Belfast, N Ireland; Whipps Cross Hospital, London Chorley District General Hospital; Leighton Hospital, Cheshire; Royal Victoria Infirmary, Newcastle Upon Tyne; Whiston Hospital, Liverpool City Hospital, Birmingham; Lincoln County Hospital; Sandwell District General Hospital, West Midlands; William Harvey Hospital, Kent Colchester General Hospital, Essex; Maidstone General Hospital, Kent; Scarborough Hospital, North Yorkshire; Withington Hospital, Manchester.
Conquest Hospital, East Sussex; Manchester Royal Infirmary; Scunthorpe General Hospital, South Humberside; Withybush General Hospital, Dyfed; Countess of Chester Hospital; Medway Hospital, Kent; Selly Oak Hospital, Birmingham; Worcester Royal Infirmary; County Hospital, Hereford; Milton Keynes Hospital; Sheffield Children's Hospital; Worthing Hospital, West Sussex; Coventry & Warwickshire Hospital; Morriston Hospital, Swansea; Skegness & District Hospital, Lincolnshire; Wrexham Maelor Hospital, Clwyd.
Craigavon Area Hospital, Co. Armagh, Northern Ireland; Nevill Hall Hospital, Wales; South Tyneside District Hospital, Tyne & Wear; High Wycombe Hospital, Bucks; Crawley Hospital, West Sussex; Newcastle General Hospital; Southampton General Hospital, Wythenshawe Hospital, Manchester; Cumberland Infirmary, Cumbria; Norfolk & Norwich General Hospital; Southend Hospital, Essex; York District Hospital; Daisy Hill Hospital, Co. Down, Northern Ireland; North Manchester General Hospital; Southmead Hospital, Bristol; Ysbyty Gwynedd District General; Darrent Valley Hospital, Kent; North Tyneside General Hospital, Tyne & Wear; Southport & Formby District General Hospital, Derbyshire Royal Infirmary; Northampton General Hospital; St Bartholomew's Hospital, London; Derriford Hospital, Plymouth; Northern General Hospital, Sheffield; St George's Hospital, London; Dewsbury District Hospital, Yorkshire; Northwick Park Hospital, Middlesex; St Helier Hospital, Surrey; Diana Princess of Wales Children's Hospital, Birmingham; Nottingham University Hospital; St James' University Hospital, Leeds; Dian; Princess of Wales Hospital, South Humberside; Ormskirk & District Hospital; St Mary's Hospital, London.
Doncaster Royal Infirmary; Peterborough District Hospital; St Peter's Hospital, Surrey; Ealing Hospital; Middlesex Pilgrim Hospital, Lincs; St Thomas' Hospital, London; East Surrey Hospital, Redhill, Surrey; Pinderfields General Hospital, Wakefield; Stepping Hill Hospital, Stockport; Eastbourne District General Hospital, East Sussex; Pontefract General Infirmary; Stoke Mandeville Hospital, Buckinghamshire; Epsom Hospital, Surrey; Queen Elizabeth Hospital, Kings Lynn; Sunderland Royal Hospital, Fairfield General Hospital, Bury; Queen Elizabeth Queen Mother Hospital, Kent; Tameside General Hospital, Ashton Under Lyne; Hammersmith Hospital, London; Regional Spinal Injuries Unit, Southport, Merseyside; Taunton & Somerset Hospital; Harrogate; District Hospital, Yorkshire; Rochdale Infirmary, Lancashire; The Horton Hospital, Oxfordshire.
Footnotes
Competing interests: none declared
References
- 1.Trauma Audit and Research Network TARN database 2003. www.tarn.ac.uk
- 2.Royal College of Surgeons of England Report of the working party into the management of patients with major injuries. London: Royal College of Surgeons, 1988
- 3.Boyd C R, Tolson M A, Copes W S. Evaluating trauma care: the TRISS method. J Trauma 198727370–378. [PubMed] [Google Scholar]
- 4.Carmody I C, Romero J, Velmahos G C. Day for night: Should we staff a trauma centre like a nightclub? Am Surg 2002681048–1051. [PubMed] [Google Scholar]
- 5.Dula D J, Dula N L, Hamrick C.et al The effect of working serial night shifts on the cognitive functioning of emergency physicians. Ann Emerg Med 200239349–351. [DOI] [PubMed] [Google Scholar]
- 6.Bell C M, Redelmeier D A. Mortality among patients admtted to hospitals on weekends as compared with weekdays. N Engl J Med 2001345663–668. [DOI] [PubMed] [Google Scholar]
- 7.Luo Z C, Karlberg J. Timing of birth and death and early neonatal mortality in Sweden 1973–95: longitudinal birth register study. BMJ 20013231327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wyatt J P, Henry J, Beard D. The association between the seniority of accident and emergency doctor and outcome following trauma. Injury 199930165–168. [DOI] [PubMed] [Google Scholar]
- 9.Lecky F E, Woodford M, Bouamra O.et al Lack of change in trauma care in England and Wales since 1994. EMJ 200219520–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fulda G J, Tinkoff G H, Giberson F.et al In house trauma surgeons do not decrease mortality in a level 1 trauma centre. J Trauma 200253494–502. [DOI] [PubMed] [Google Scholar]
- 11.Downing A, Wilson R. Temporal and demographic variations in attendance at A&E departments. EMJ 200219531–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Åkerstedt T, Kecklund G. Age, gender and early morning highway accidents. J Sleep Res 200110105–110. [DOI] [PubMed] [Google Scholar]
- 13.Rutledge R, Osler T, Emery S.et al The end of the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS). ICISS, an International Classification of Diseases, ninth revision‐based prediction tool, outperforms both ISS and TRISS as predictors of trauma patient survival, hospital charges, and hospital length of stay. J Trauma 19984441–49. [DOI] [PubMed] [Google Scholar]