Abstract
It is known that insects can cause various clinical effects such as myocardial ischaemia and hypotension from vasospasm and the myocardial toxic effects of the venom and anaphylaxis. Although myocardial ischaemia resulting from centipede sting has been reported once before, myocardial injury has not. In this report, the authors present the case of a 20 year old male patient bitten by a centipede and admitted to the emergency room with chest pain, abnormal electrocardiographic findings, and increased cardiac enzymes (cardiac troponin T) suggesting acute myocardial infarction.
Keywords: centipede sting, acute myocardial infarction, coronary vasospasm, troponin T
Various clinical situations such as anaphylaxis, skin disorders, ECG changes, cardiac specific enzyme elevation, and myocardial necrosis have been reported as the result of snake, scorpion, or bee bites.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 There has only been one case report of acute myocardial ischaemia following centipede envenomation to date.2 In this report, we present a case of acute myocardial infarction associated with a centipede bite.
Case report
A 20 year old man was bitten on his right leg by a centipede while he was sitting in his garden. Severe local pain and swelling started immediately and he applied cold pressure. Local pain and swelling declined but the patient began to experience severe left arm pain, cold sweating, nausea, and vomiting. About 24 hours after he was bitten he was brought to our hospital's emergency department. He had severe chest pain and his consciousness was normal. Blood pressure was 120/80 mmHg and heart rate was 82 bpm.
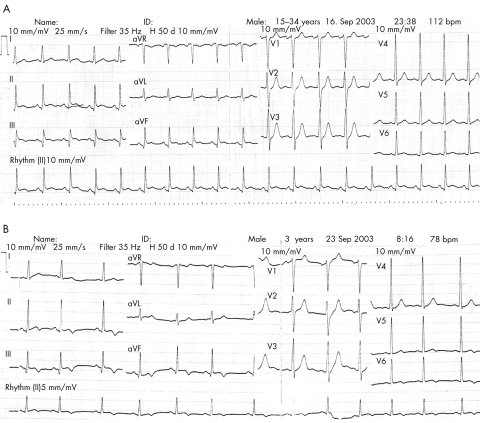
There was no abnormal finding in his cardiac, neurological, and respiratory system evaluation except oedema and there was a reddish colour around his right toe. He had no risk factors for coronary artery disease and there was no history of drug allergy or abuse. He was in sinus rhythm with sequential ST segment elevation in leads DII‐DIII‐aVF‐V6 more than 1.5 mm, suggesting acute inferolateral myocardial infarction on electrocardiography (fig 1A). The patient was admitted to the coronary care unit and nasal oxygen therapy was started at 2–4 l/minute. His treatment was planned as following: aspirin 300 mg orally, 1000 unit/hour heparin infusion after intravenous 5.000 unit bolus, and 30 μg perlinganit after 100 μg intravenous bolus infusion. Thirty minutes later, his chest pain disappeared and ECG segment elevations regressed to the iso‐electric line (fig 1B).
Figure 1 (A and B) ECG shows ST segment elevation in DII, DIII, aVF, and V6.
Twenty four hours later, ECG changes completely disappeared. All the blood tests were within normal limits but CK‐MB and CK were elevated more than three times above the normal limits and Troponin‐T was positive (>1 ng/ml); other blood tests were within normal limits. Transthoracic echocardiography was normal. Coronary angiography was performed on the fifth day and there was no atherosclerotic lesion in the coronary arteries (fig 2). Seventeen months later, the patient was completely symptom free.
Figure 2 Coronary angiography shows normal coronary arteries.
Discussion
Centipedes live in warm, temperate, and tropic regions. They are elongated and multisegmented arthropods with a single pair of legs on each body segment. Centipedes spend most of their time underground or beneath rock piles and they usually come out at night to hunt their prey. The most dangerous species belong to the genus Scolopendra, with the largest members (Scolopendra gigantea) reaching lengths of 30 cm. Most species are smaller and relatively innocuous.2 The venom apparatus consists of modified legs on either side of the body just behind the head. A venom duct carries venom to the venom claw, which is used to envenom prey via a subterminal pore on the outer curvature of the claw.2 These arthropods are fast moving and frightening in appearance to some, and they may show aggressive behaviour. However, stings usually cause no serious morbidity or mortality.2,3,4,5
Although few studies have evaluated the effects of centipede venom, it is known that some centipede venoms are complex mixtures containing 5‐hydroxytryptamine, histamine, lipids, polysaccharides, and various enzymes (for example, proteinases, esterases). Some studies have demonstrated slowly moving lipoprotein bands, and the lipid components include phospholipids, cholesterol, free fatty acids, triglycerides, cholesterol esters, and squalene.5,6,7 A high molecular acidic and heat labile cardiotoxic protein (toxin S) 4 has been isolated from the venom of Scolopendra subspinipes. The venom of the North American giant desert centipede Scolopendra heros contains a cytolysin.1,7
There are very few studies on the physiological effects of venom in human. In cats, the toxin induces a rise in blood pressure that is not influenced by α‐adrenergic blockers. Muscarinic acetylcholine receptors participate in different physiological functions (for example, reduction of heart rate, contraction of smooth muscles). An extract from the centipede Scolopendra morsitans has been shown to arrest the heart of the toad—an effect blocked by atropine. The mechanisms for this are unknown.2,7 Centipede venom effects on the cardiovascular system have not been studied, and the mechanism of the ECG abnormalities recorded in a few cases of arthropod stings has not been elucidated. Pulmonary oedema has been observed in a few patients. Autopsy studies are very rare.8
In our case, we thought that the most probable diagnosis was myocardial infarction due to vasospasm, hypotension, increased capillary permeability, inflammatory changes, and multifactorial effects of the centipede venom. We did not give thrombolytic therapy or perform primary angioplasty because of the disappearance of chest pain and regression of the ST segment elevations.
Data concerning the morbidity and mortality possibly attributed to centipedes are scarce.16,17,18,19 Only three deaths due to centipedes have been reported worldwide. Most common symptoms following envenomation are severe pain, local tissue swelling, redness, swollen and painful lymph nodes, headache, palpitations, nausea, vomiting, and anxiety.2,3,4,5,6 The most commonly affected body parts are the hands and feet. A localised, about 10×10 cm area may be found at the sting site initially. The wounds are typically small punctures and may exhibit small haemorrhagic vesicles.3,5 Mild local bleeding is common but transient.12 The site of envenomation may become ulcerated and necrotic. Secondary infection and local necrosis can occur.2,3,4,5,6,7,8,9
The treatment of centipede stings is symptomatic and includes ice or cold compress application, simple wound care, control of pain with analgesics, and relief of pruritis with antihistamines. Tetanus prophylaxis should be provided as indicated. In rare cases of anaphylaxis or severe toxicity, more aggressive medical treatment is appropriate. Following initial care, the wound should be examined for signs of secondary infection or necrosis.2,3,4,5,6,7,8,9,10,11,12,13,14,15
Different clinical entities have been described associated with centipede sting. Eosinophilic cellulitis (Wells' syndrome) is an uncommon condition of unknown aetiology. Ilyse et al described a patient with this entity that had been triggered by a centipede sting.16 The presentation usually involves a vasculitis and tender cellulitis‐like eruption with an infiltration of eosinophils in the dermis.
The other rare clinical condition is acute coronary syndrome. Ozsarac et al reported a 50 year old patient with acute coronary syndrome after centipede envenomation.2 Our patient is the second case reported of a centipede bite associated with acute coronary syndrome. Unlike the patient in the previous case, our patient was a young male and had suffered acute myocardial infarction. The exact underlying mechanism in both cases is unknown; however, in our opinion, cardiotoxins, histamine, and serotonin‐like substances released from eosinophils may have aggravated the coronary spasm and a delayed coronary spasm may have triggered coronary thrombosis. Acute coronary syndrome may be a clinical entity associated with centipede bites such as Wells' syndrome.2,16
Cardiac evaluation in patients with centipede envenomation is an important part of the medical examination and follow up. Perlinganit, aspirin, and heparin infusion are the cornerstones of therapy if ischaemic symptoms occur.
References
- 1.Knysak I, Martins R, Bertim C R. Epidemiological aspects of centipede bites registered in greater S. Paulo, SP, Brazil. Rev Saude Publica 199832514–518. [DOI] [PubMed] [Google Scholar]
- 2.Ozsarac M, Karcioglu O, Ayrik C.et al Acute coronary ischemia following centipede envenomation: case report and review of the literature. Wilderness Environ Med 200415109–112. [DOI] [PubMed] [Google Scholar]
- 3.Lin T J, Yang C C, Yang G Y.et al Features of centipede bites in Taiwan. Trop Geogr Med 199547300–302. [PubMed] [Google Scholar]
- 4.Menez A, Zimmerman K, Zimmerman S.et al Venom apparatus and toxicity of the centipede Ethmostigmus rubripes (Chilopoda Scolopendridae). J Morphol 1990206303–312. [DOI] [PubMed] [Google Scholar]
- 5.Bush S P, King B O, Norris R L.et al Centipede envenomation. Wilderness Environ Med 20011293–99. [DOI] [PubMed] [Google Scholar]
- 6.Barroso E, Hidaka A S, dos Santos A X.et al Centipede stings notified by the “Centro de Informacoes Toxicologicas de Belem”, over a 2‐year period. Rev Soc Bras Med Trop 200134527–530. [DOI] [PubMed] [Google Scholar]
- 7.Gomes A, Data A, Sarangi B.et al Pharmacodynamics of venom of the centipede Scolopendra subspinipes dehaani Brandt. Indian J Exp Biol 198220615–618. [PubMed] [Google Scholar]
- 8.Gueron M, Ilia R. Arthropod poisons and the cardiovascular system. Am J Emerg Med 200018708–714. [DOI] [PubMed] [Google Scholar]
- 9.Norris R L. Bite marks and the diagnosis of venomous snakebite. Wilderness Environ Med 19956159–161. [DOI] [PubMed] [Google Scholar]
- 10.Cohen E, Quistad G B. Cytotoxic effects of arthropod venoms on various cultured cells. Toxicon 199836353–358. [DOI] [PubMed] [Google Scholar]
- 11.Mohri S, Sugiyama A, Saito K.et al Centipede bites in Japan. Cutis 199147189–190. [PubMed] [Google Scholar]
- 12.Uppal S S, Agnihotri V, Ganguly S.et al Clinical aspect of bite in the Andamans. J Assoc Physicians India 199038163–164. [PubMed] [Google Scholar]
- 13.Bahloul M, Kallel H, Rekik N.et al Cardiovascular dysfunction following severe scorpion envenomation [in French]. Presse Med 200534115–120. [DOI] [PubMed] [Google Scholar]
- 14.Harada K, Asa K, Imachi T.et al Centipede inflicted postmortem injury. J Forensic Sci 199944849–850. [PubMed] [Google Scholar]
- 15.Cupo P, Hering S E. Cardiac troponin I release after severe scorpion envenoming by Tityus Serrulatus. Toxicon 200240823–830. [DOI] [PubMed] [Google Scholar]
- 16.Friedman I S, Phelps R G, Baral J.et al Wells syndrome triggered by centipede bite. Int J Dermatol 199837602–605. [DOI] [PubMed] [Google Scholar]
- 17.Logan J L, Ogden D A. Rhabdomyolysis and acute renal failure following the bite of the giant desert centipede Scolopendra heros. West J Med 1985142549–550. [PMC free article] [PubMed] [Google Scholar]
- 18.Mohamed A H, Zaid E, El‐Beihet al Effects of an extract from centipede Scolopendra morsitans on intestine, uterus and heart contractions and on blood glucose and liver and muscle glycogen levels. Toxicon 198018581–591. [DOI] [PubMed] [Google Scholar]
- 19.Magadle R, Weiner P, Waizman J.et al Acute myocardial infarction after honeybee sting. Harefuah 2000138543–545. [PubMed] [Google Scholar]