Abstract
Objectives
The aim of this study was to determine the general characteristics of childhood falls, factors affecting on mortality, and to compare the Injury Severity Score (ISS) and the New Injury Severity Score (NISS) as predictors of mortality and length of hospital stay in childhood falls.
Methods
We retrospectively analysed over a period of 8 years children aged younger than14 years who had sustained falls and who were admitted to our emergency department. Data on the patients' age, sex, type of fall, height fallen, arrival type, type of injuries, scoring systems, and outcome were investigated retrospectively. The ISS and NISS were calculated for each patient. Comparisons between ISS and NISS for prediction of mortality were made by receiver operating characteristic (ROC) curve and Hosmer‐Lemeshow (HL) goodness of fit statistics.
Results
In total, there were 2061 paediatric trauma patients. Falls comprised 36 (n = 749) of these admissions. There were 479 male and 270 female patients. The mean (SD) age was 5.01 (3.48) years, and height fallen was 3.8 (3) metres. Over half (56.6%) of patients were referred by other centres. The most common type of fall was from balconies (38.5%), and head trauma was the most common injury (50%). The overall mortality rate was 3.6%. The cut off value for both the ISS and NISS in predicting mortality was 22 (sensitivity 90.5%, specificity 95.4% for ISS; sensitivity 100%, specificity 88.7% for NISS) (p>0.05). Significant factors affecting mortality in logistic regression analysis were Glasgow Coma Scale (GCS) <9, ISS >22, and NISS >22. There were no significant differences in ROC between three scoring systems. The HL statistic showed poorer calibration (p = 0.02 v p = 0.37, respectively) of the NISS compared with the ISS.
Conclusions
In our series, the head was the most frequent site of injury, and the most common type of fall was from balconies. Scores on the GCS, NISS, and ISS are significantly associated with mortality. The performance of the NISS and ISS in predicting mortality in childhood falls was similar.
Keywords: childhood falls, injury severity score, new injury severity score, mortality
Trauma is an important cause of both morbidity and mortality in children and young adults.1 According to US based data, over 1.5 million childhood traumas occur annually, resulting in approximately 500 000 hospitalisations. Furthermore, trauma is the leading cause of mortality in the paediatric population, accounting for 15 000–20 000 deaths each year.2 Falls, on the other hand, are the most common cause of admission to the emergency department (ED) during childhood, and are the fourth leading cause of trauma deaths.3,4,5,6,7
An important role of any trauma centre is to study the frequency, distribution, cause, and pattern of its trauma population and to compare these data with other trauma centres, in order to develop strategies to prevent injuries, which are applicable regionally and locally.8,9,10 Several trauma scoring systems have been developed to measure the severity of the injury, and to analyse its impact on morbidity and mortality for trauma research. The most common scoring systems used include the Glasgow Coma Scale (GCS),11 Revised Trauma Score,12 Pediatric Trauma Score (PTS),13 Injury Severity Score (ISS),14 and the Trauma and Injury Severity Score.15
The ISS has been the “gold standard” for anatomical severity scoring since it was introduced in 1974. The ISS sums the severity score for the three most severe injuries, but it only considers one injury per body region. Therefore it may lead to an underestimation of the patient's overall anatomical injury severity, because the patient's most severe injuries may not represented.16,17 To improve the accuracy, Osler et al18 introduced in 1997 a modification of the ISS and named it the New Injury Severity Score (NISS). The NISS sums the severity score for the three most severe injuries, regardless of body region. Although there have been several studies comparing ISS and NISS for adult trauma patients, only a few exist on paediatric trauma patients. In the paediatric age group, the superiority of the NISS compared with the ISS is not certain. However, Sullivan et al19 demonstrated that in cases with severe injuries, the NISS was better for mortality and locomotor functions. Studies based on specific trauma contribute to this discussion. In addition, these types of study help to answer the question of which scale should be used in measuring the success of trauma management.
Based on the above information, our study had two objectives. (a) As the characteristics of childhood falls in our country, and especially our locality, are unknown, we aimed to determine the epidemiological and clinical characteristics and factors affecting outcome of childhood falls admitted to our hospital, which has level 1 trauma centre facilities. (b) We also aimed to determine the relationship between the clinical characteristics and mortality using the GCS, PTS, ISS, and NISS, and especially to compare the ISS and NISS with regard to mortality induced by childhood fall injuries and length of hospital stay.
METHODS
The study was conducted in a university hospital with an emergency medicine residency program and a volume of over 30 000 annual visits. The hospital is located in Bursa, which is the fourth largest city of Turkey, with a population of over 2 million, and is the only hospital with level I trauma centre facilities in the South Marmara region. In our country, prehospital trauma patient care is provided by 112 medical services, governed by the Ministry of Health, and the patient is then transported to hospital. However, this system is not yet mature and is still developing. A triage system appropriate to an Advanced Trauma Life Support (ATLS) programme is not fully operational due to many socioconomic problems (especially problems with finance, hospital capacity, and training). Therefore, patients fulfilling the criteria given in table 1 as being appropriate for ATLS are accepted as patients with serious trauma, and primary and secondary surveys were performed by a multidisciplinary team in our centre.
Table 1 Summary of the Uludag University Medical School Hospital Trauma Protocol Inclusion Criteria*.
| Criterion | Details |
|---|---|
| Disturbed physical parameter | RTS<11, PTS<9, GCS<13. |
| Systolic blood pressure <90 mmHg | |
| Respiratory rate<10 or >29 | |
| Penetrating injuries | All penetrating trauma to head, neck, thorax, abdomen, and extremities proximal to elbow and knee |
| Specific blunt injuries | Injuries in more than two regions |
| Two or more proximal long bone fractures | |
| Amputation proximal to wrist/ankle | |
| Unstable fracture of pelvic ring | |
| Spinal injuries | |
| Flail chest | |
| High energy trauma | Motor vehicle crash>40 km/h |
| Major motor vehicle deformity | |
| Bicycle/moped/pedestrian versus motor vehicle | |
| Fall >3 metres | |
| Death of other crash victim | |
| Ejection from vehicle |
RTS, Revised Trauma Score; GCS, Glasgow Coma Scale; PTS, Pediatric Trauma Score. *The inclusion set is designed to include all patients with reasonable chance of severe injuries likely to require the attention of the trauma team.
Children ⩽14 years of age who were admitted between 1 January 1997 and 31 December 2004 to our ED due to falls were included in our study. All patients were resuscitated according to ATLS principles, and underwent diagnostic and therapeutic procedures according to existing protocols. Data on the patients' age, sex, type of fall, height fallen, whether the patient was referred from another hospital, type of injuries, and outcome in the ED were obtained by examining the ED patient records and trauma forms.
GCS and PTS scores on admission to our ED were taken from the trauma records of the patients. The GCS is based on an estimation of the impairment of consciousness. The following parameters are assessed: eye opening (1–4 points), verbal response (1–5 points), and best motor response (1–6 points). A score of 15 points indicates normal findings, and a score of <8 points defines a comatose condition. In the PTS, respiration, alertness, systolic blood pressure, estimated body weight, and the presence and severity of soft tissue injuries and fractures are evaluated, each scoring between −1 and +2. Scores <9 points are considered to be indicative of a life threatening situation. For each patient, we computed the ISS (sum of the squares of the highest Abbreviated Injury Scale (AIS) score in each of the three most severely injured body regions) and the NISS (the sum of the squares of the three highest AIS scores regardless of the body region in which they occur). The AIS identifies the most severe individual injury. Here, scores of between 0 (no injury) and 5 (life threatening injury) points are made for six regions of the body. A score of 6 identifies an injury that is incompatible with survival.
We further divided the patients into two groups on the basis of whether the ISS and NISS were concordant (ISS = NISS) or discordant (NISS > ISS). These two groups were analysed with regard to distance fallen, site of injury, type of admission to hospital (referred or direct), mortality rate, and duration of hospitalisation. Length of hospital stay, any surgical interventions, final diagnosis, and overall mortality rate were determined by examining the records of patients who were transferred from the ED to various clinics.
Statistical analysis
Epidemiological data were analysed with SPSS software (version 11.0; SPSS Inc., Chicago, IL, USA). Data were presented as mean (SD) for continuous variables, and as frequency and percentage (n, %) for categorical variables. Categorical data were compared using χ2 and t tests. In univariant analysis, to determine the contribution of statistically relevant factors to mortality, the receiver operating characteristics (ROC) analysis was performed and cut off values determined. These parameters were divided into two groups and examined with logistic regression analysis.
The relationship between the GCS, PTS, ISS, and NISS scores and the distance fallen was measured using Pearson's correlation test, with p<0.05 considered as significant. Comparisons between the ability of different measures of severity of trauma (ISS, NISS) to predict mortality were made by ROC curve and Hosmer‐Lemeshow (HL) goodness of fit statistics. MedCalc was used for ROC analysis. The ROC statistic is a general measure of the power of a test to separate two mutually exclusive subpopulations. It is defined as the area under the graph of sensitivity ×1 minus specificity. A ROC value of 1 corresponds to a test that perfectly separates two subpopulations, whereas a ROC value of 0.5 corresponds to a test that performs no better than chance. The best value for balancing the sensitivity and specificity of the variable is represented by the point on the curve closest to the upper left hand corner accepted cut off point. The HL statistic measures the callibration of a test (in this case, calibration of the ISS and the NISS); a value of p>0.05 suggests an evenly calibrated test. A more evenly calibrated test is more applicable to all ranges of injury severity.
RESULTS
Epidemiological and clinical characteristics of the patients
In total, 2061 children aged 0–14 years were admitted to the ED during the study period. Of these, 749 (36.3%) had sustained falls, and were analysed. The general characteristics of the 749 patients are shown in table 2. Of the 749 patients, 64% were male and 36% female. Mean (SD) age was 5.01 (3.48) years (range 7 days to 14 years), with 56% being ⩽5 years of age.
Table 2 Characteristics of the 749 patients.
| Characteristic | |
|---|---|
| Age (years), mean (SD) | 5.01 (3.5) |
| Age groups, n (%) | |
| 0–2 years | 199 (26.6) |
| 3–10 years | 476 (63.6) |
| 11–14 years | 73 (9.8) |
| Sex, n (%) | |
| Male | 479 (64) |
| Female | 270 (36) |
| Height of fall | 3.8 (3) |
| Arrival type, n (%) | |
| Directly admitted to our hospital | 319 (43.4) |
| Referred from other centres | 416 (56.6) |
| Trauma score, mean (SD) | |
| GCS | 13.35 (3) |
| PTS | 10.03 (2.3) |
| ISS | 8.7 (7.75) |
| NISS | 10.2 (9.8) |
| Type of fall, n (%) | |
| Balcony | 270 (38.5) |
| Stairs | 157 (22.5) |
| Wall | 56 (8) |
| Window | 51 (7.3) |
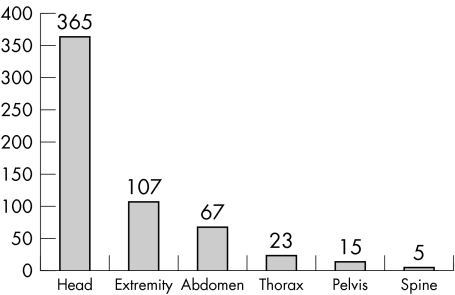
The most common types of falls were from balconies (38.5%), stairs (22.5%), and walls (8%). Mean (SD) height fallen was 3.8 (3) metres (0.3–15 m). Over half (56.6%; n = 416) of the patients were referred by other centres, whereas 43.4% (n = 319) were transported directly to the hospital. When we examined the types of injuries in the 749 patients, head injury was the most common (50%,), followed by injury to the extremities (14.5%), and abdomen (9%). Uncommon sites of injuries were the thorax (3%), pelvis (2%), and vertebrae (0.7%) (fig 1). Of the 749 cases, 24.6% (n = 181) were discharged from the ED, 40% (n = 295) were transferred to other healthcare centres, 34% (n = 248) were admitted to various clinics, and 1.6% (12) died in the ED. Data for the remaining 13 patients were missing, thus no information on their outcome could be obtained.
Figure 1 Figure 1 Distribution of the patients according to site of injury.
Of the 248 hospitalised patients, 138 (55.6%) had head injury. Surgery was performed on 36.3% (50/138) of these patients. The number of inpatients with extremity injury was 33 (20.6%), and in 50% of these (16/33), open reduction plus internal fixation were performed. The number of patients admitted due to abdominal injury was 29 (18%), with laparatomy performed in three, while the others were monitored conservatively. There were no deaths due to abdominal injury. The mean length of stay for all 248 patients was 5.6 days (range 1 to 33).
The overall mortality rate was 3.6% (27/749); 24 of these patients (89%) were referred by other centres. The cause of death of these patients was investigated by checking the postmortem examination and/or burial records, and was found to be head injury in all cases.
Trauma scores and analysis of the clinical characteristics
The mean (SD) GCS, PTS, ISS, and NISS scores of the 749 patients were 13.4 (2.7), 10 (2.2), 8.7 (7.75), and 10.2 (9.8), respectively, and median scores were 15, 10, 9, and 9, respectively.
The relationship between patient age, sex, height of the fall, GCS, PTS, ISS, NISS, and mortality rate was analysed. In the young age group (<3 years of age), the mortality rate significantly increased (p<0.05). There was no significant relationship between sex and mortality rate (p>0.05). With increasing height of the fall, especially for falls from 2 metres and higher, the mortality rate also increased significantly (p<0.05). In logistic regression analysis, GKS <9 (odds ratio (OR) = 7735, p<0.0001), ISS >22 (OR = 7291, p<0.0001) and NISS >22 (OR = 1985, p = 0.042) were found to be independent prognostic factors (table 3). As falling from a balcony was the most frequent type of fall (38.5%, n = 270), comparison of this patient group with other types of falls was performed (table 4).
Table 3 Factors affecting on mortality in logistic regression analysis.
| Variable | Coefficient (β) | SE | Wald χ2 | P | ||||
|---|---|---|---|---|---|---|---|---|
| Constant | −0.0105 | 0.026 | – | – | ||||
| GCS <9 | 0.201 | 0.026 | 7.73 | <0.0001 | ||||
| ISS >22 | 0.231 | 0.031 | 7.29 | <0.0001 | ||||
| NISS >22 | 0.0424 | 0.022 | 1.98 | 0.042 |
Table 4 Comparison between falls from a balcony and other types of fall.
| Characteristic | Falls from balcony | Other types of fall | p | |||
|---|---|---|---|---|---|---|
| Age (years) | 4.34 (2.9)* | 5.35 (3.7) | 0.001 | |||
| Height of fall (m) | 5.5 (3) | 2.5 (2) | 0.000 | |||
| GCS | 12.7 (3.4) | 13.8 (2.2) | 0.001 | |||
| PTS | 9.7 (2.7) | 10.2 (2) | 0.001 | |||
| ISS | 10 (8.4) | 8 (7) | 0.001 | |||
| NISS | 11.7 (10.7) | 9.4 (9) | 0.001 |
*Data are mean (SD).
The mean (SD) GCS, PTS, ISS, and NISS scores of the patients referred by other centres were 13 (3), 9.6 (2.5), 9.8 (8.1), and 11.8 (10.4), respectively, which were significantly different from patients who were transported directly to our hospital (14 (2), 10.5 (2), 7 (6.5), 8 (7.1)) (p = 0.001). The mortality rate was also significantly higher (p = 0.001). Clinical outcome of 12 patients who died in the ED and 248 patients hospitalised in various clinics (in total 260 patients) was analysed. Comparison of survivor and non‐survivor patients is given in table 5. Final outcome of two of the 260 patients could not be obtained, so the results for 258 patients are included in the table. We found a significant difference for all of the parameters (mean age, height of fall, GCS, PTS, ISS, and NISS) between the two groups.
Table 5 Comparison of the demographic characteristics and trauma scores between survivors and non‐survivors.
| Characteristic | Survivors (n = 231) | Non‐survivors (n = 27) | p | |||
|---|---|---|---|---|---|---|
| Age (years) | 5.5 (3.7) (4) | 2.97 (2.2) (2.5) | 0.001 | |||
| Height of fall (m) | 4.95 (3.6) (4) | 6.74 (3.6) (6) | 0.016 | |||
| GCS | 12.3 (2.8) (14) | 4.67 (2.4) (3) | <0.001 | |||
| PTS | 9.9 (2) (10) | 3.2 (3.5) (2) | <0.001 | |||
| ISS | 13.4 (7.7) (13) | 25 (6) (25) | <0.001 | |||
| NISS | 15.6 (9.6 )(16) | 30.2 (8.2) (29.5) | <0.001 |
*Data are mean (SD) (median).
The relationship between the GCS, PTS, ISS, and NISS scores and the height of the fall was analysed using Pearson's correlation test. While a negative correlation was found between the height of the fall and GCS and PTS (r = −0.341, p< 0.001; r = −0.220, p<0.001, respectively), a positive correlation was observed between the height of the fall and ISS and NISS (r = 0.336, p< 0.001; r = 0.313, p<0.001, respectively).
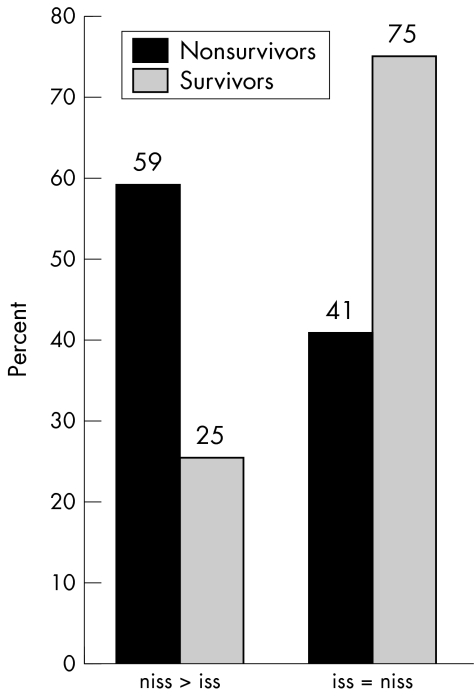
While NISS was greater than ISS in 18.5% of the patients (n = 136) (the discordant group), ISS was equal to NISS in 81.5% of the patients (n = 598) (the concordant group). In the statistical analyses, height of the fall, referral by other centres, and mortality rate were significantly higher in the discordant group (p<0.001), but although the length of hospital stay was longer, the difference was not statistically significant (p = 0.069). However, head and extremity injuries were significantly more common (p<0.001) in the discordant group. In 30.6% of the patients with head injuries, and in 30% of the patients with injuries to the extremities, NSS was higher than ISS. The mortality rates of the discordant and concordant groups are shown in fig 2.
Figure 2 Figure 2 Comparison of the concordant (NISS = ISS) and discordant (NISS > ISS) groups for survivors and non‐survivors.
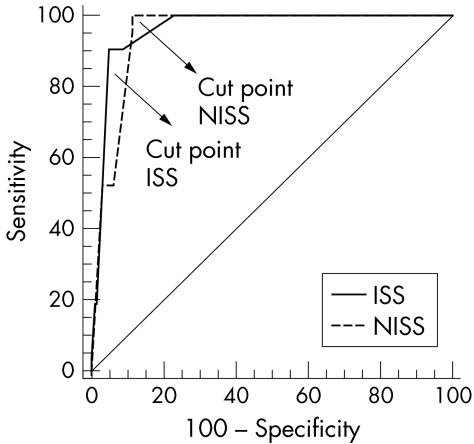
The cut off value of ISS in predicting mortality was 22, with sensitivity and specificity being 90.5% and 95.4%, respectively (area under the curve (AUC) 0.962, 95% confidence interval (CI) 0.945 to 0.974). The cut off value of NISS in predicting mortality was also 22, with sensitivity and specificity being 100% and 88.7%, respectively (AUC 0.950, 95% CI 0.931 to 0.964) (fig 3). Cut off value for GCS was 0 (sensitivity 92.3%, specificity 93.7%, AUC 0.975, 95% CI 0.961 to 0.985). There were no significant differences in ROC comparison between three scoring systems. The HL statistic showed poorer calibration of the NISS compared with the ISS (p = 0.02 v p = 0.37 respectively).
Figure 3 Figure 3 The receiver operating characteristic (ROC) Curves of ISS and NISS for predicting mortality in the whole population (749 patients). There were no significant differences between scores. Cut off points were 22 for ISS (sensitivity 90.5%, specificity 95.4%, AUC 0.962, 95% CI 0.945 to 0.974) and 22 for NISS (sensitivity 100%, specificity 88.7 %, AUC 0.950, 95% CI 0.931 to 0.964).
DISCUSSION
Falls account for up to 25–34% of all paediatric trauma admissions in major urban trauma centres.20 Musemeche et al21 found that 25% of 1463 paediatric trauma cases were a result of falls. In our study, falls made up 36.3% of paediatric trauma cases.
The epidemiological and clinical characteristics of our study population are comparable with those in the literature. Childhood falls are most frequently experienced by preschool boys. The demographic data of our patient population showed that 64% were males, and 56% were children <5 years of age. Similar prevalence rates have been reported in various studies.3,21,22 Mosenthal et al22 reported a prevalence of 36% in the paediatric group for falls from windows, which was the most common type of fall. Similarly, falls from windows are the most common type of fall in other studies reported in the literature.5,23,24,25 In our study, the most common type were falls from balconies (38.5%). The widespread use of multistorey buildings in our country and region makes balconies the main situation for child falls. Laws governing construction of balconies in buildings (the barrier height should be at least 900 mm) are insufficient and controls are inadequate, so falls from balconies are still a threat to child safety in Turkey, especially in the younger age group (<5 years of age).
More than half (56.6%) of our patients were referred by other centres, and the GCS, PTS, ISS, and NISS scores of these patients were significantly different from patients transported directly to our hospital. The mortality rate was again significantly higher in this group. Moini et al26 reported that 57% of the patients in their study were referred by other centres, but failed to show a difference with regard to severity of trauma and mortality rate. They stated, however, that direct transportation improves the outcome of trauma patients. Pillai et al24 reported this rate as 45%. A problem with the trauma system in our region is that a high proportion of patients was referred from other centres, and this high rate of transportation shows that the triage system works inadequately.
Head injury was detected in 50% of our patients. Several studies have reported the head region as the most commonly affected body system.9,10,11,12,13 The reason for the high frequency of head injury following falls in children can be explained by their higher head/body ratio compared with adults, which makes landing on their heads more likely.7,12 Fractures of the extremities in our study had a frequency of 14.5%, which put the second place for frequency. Pelvic and vertebral trauma were rather rare (2% and 0.7%, respectively). Several studies have reported injuries to the extremities as the second most common injury, and pelvic and vertebral injuries seen less frequently.3,10,12 In our study, abdominal injuries were the third common type of injury, comprising 9% of injuries. Roshkow et al25 reported only one case of intra‐abdominal organ injury among the 45 children included in their study. This rate was reported as 2% in the study conducted by Mucemeche et al.21
The overall mortality rate in our study was 3.6%, similar to that reported as 4% by Murray et al (4%),20 and Meller et al (2%).27 Head injuries are reported to be the most common cause of death in childhood falls.2,3,7,10 Head injury was the only cause of death in all of our patients. Hall et al3 reported head trauma as the most common reason for death in child falls (70.5%) in their necropsy study; 89% of children were <5 years old and 64% were <2 years. The high mortality rate from head injuries is consistent with the anatomical fact that younger children have softer cranial bones and thus less cerebral protection.3
We determined age and height of the fall as major factors affecting mortality rate in univariete analysis. We also found that the mortality rate increases significantly with increasing height, especially in falls from >2 metres. In addition, the GCS and PTS scores increase and the ISS and NISS scores decrease, proportionally. Goodacre et al28 reported a direct relationship between height of fall and the mortality rate, but stated that height is a poor indicator of the severity of the resulting trauma. Isbister and Roberts29 and Mathis et al30 found similar results. Agalar et al31 found a significant relationship with mortality rate for ISS, age, and height. Our study shows that although factors such as age and height fallen were important factors in mortality, the main factor was the anatomical and physiological severity of the injury.
The NISS has several clinical and practical advantages over the ISS. From a clinical point of view, it is more logical than the ISS because it gives equal priority to all injuries, even if they occur in the same body region. As an example, a patient with two head injuries, each with an AIS severity score of 5, will be assigned a NISS of 50, whereas under the ISS system, he would be assigned 25, the same severity score as a patient with a single head injury. Using the NISS over the ISS does imply an important increase in severity values. The NISS was higher than the ISS for 18.5% of our patients and this figure rose to over 30% in head injured patients. From a practical point of view, it is easier to calculate than the ISS, as it requires no division of AIS codes into body regions, which can be especially complex for spinal cord and external injuries.
There are a few studies in the literature comparing these two scores in paediatric trauma patients. Grisoni et al32 analysed predictive values of the ISS and the NISS for mortality, and found similar results for both. Sullivan et al19 found scores on the ISS and the NISS of 8.1 and 10.8, respectively, but failed to detect a significant difference with regard to their predictive values for mortality. They reported, however, that the NISS is superior in patients with severe injuries (ISS >24). In our study, the mean ISS and NISS scores were 8.7 (7.75) and 10.2 (9.8), respectively. No difference could be found with regard to their predictive values for mortality between the two scores.
Several studies have compared the NISS to the ISS to the with respect to mortality.16,18,32,33,34,35 Some of these studies have been contradictory, but have generally found the NISS to be equivalent to the ISS in populations with low injury severity.16,19,32,35 However, the NISS appears to perform significantly better than the ISS in populations with moderate to severe injury severity, in which the discrepancy between ISS and NISS values is greater.17,18,19,33 The most important reasons for the contradictory results may be the differences in the studied populations (such as type and severity of injury and site of injury). In our study, the low number of patients is a limitation in comparing the NISS and ISS.
CONCLUSIONS
Three conclusions can be drawn from our study. (a) Falls in children occur more frequently in boys <5 years of age, and head trauma is the most common type of injury and the leading cause of death. (b) In order to prevent falls from balconies, supervision by parents should be increased, new laws regarding barriers on balconies should be enacted and application of these controlled, and campaigns including public education and media attention should be organised in our region. (c) A significant relationship was found between mortality rate and the GCS, ISS, and NISS. Our study failed to answer the question whether the ISS or the NISS is superior, but stresses the need for mortality and long term functional outcome studies in different trauma populations (such as child versus adult, and blunt versus penetrating wounds).
Abbreviations
AIS - Abbreviated Injury Scale
ATLS - Advanced Trauma Life Support
ED - emergency department
GCS - Glasgow Coma Scale
HL - Hosmer‐Lemeshow
ISS - Injury Severity Score
NISS - New Injury Severity Score
PTS - Pediatric Trauma Score
ROC - receiver operating characteristic
Footnotes
Competing interests: there are no competing interests.
References
- 1.Sawyer J R, Flynn J M, Dormans J P.et al Fracture patterns in children and young adults who fall from significant heights. J Pediatr Orthop 200020197–202. [PubMed] [Google Scholar]
- 2.Potoka D A, Schall L C, Ford H R. Improved functional outcome for severely injured children treated at pediatric trauma centers. J Trauma 200151824–834. [DOI] [PubMed] [Google Scholar]
- 3.Hall J R, Reyes H M, Horvat M.et al The mortality of childhood falls. J Trauma 1989291273–1275. [DOI] [PubMed] [Google Scholar]
- 4.Beale J P, Wyatt J P, Beard D.et al A five year study of high falls in Edinburgh. Injury Int J Care Injured 200031503–508. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics Committee on injury and poison prevention. Falls from heights: Windows, roofs, and balconies, Pediatrics 20011071188–1191. [DOI] [PubMed] [Google Scholar]
- 6.Stone K E, Lanphear B P, Pomerantz W J.et al Childhood injuries and deaths due to falls from windows. J Urban Health 20007726–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lallier M, Bouchard S, St‐Vill D.et al Falls from heights among children: A retrospective review. J Pediatrs Surg 1999341060–1063. [DOI] [PubMed] [Google Scholar]
- 8.Schall L C, Potoka D A, Ford H R. A new method for estimating probability of survival in pediatric patients using revised TRII methodology based on age‐adjusted weights. J Trauma 200252235–241. [DOI] [PubMed] [Google Scholar]
- 9.Cassidy L D, Potoka D A, Adelson P D.et al Development of a novel method to predict disability after head trauma in children. J Pediatr Surg 200338482–485. [DOI] [PubMed] [Google Scholar]
- 10.Osmond M H, Brennan‐Barnes M, Shephard A L. A 4‐year review of severe pediatric trauma in eastern Ontario: a descriptive analysis. J Trauma 2002528–12. [DOI] [PubMed] [Google Scholar]
- 11.Teasdale G, Jennet B. Assessment of coma and impaired consciousness: a practical scale. Lancet 19741381–85. [DOI] [PubMed] [Google Scholar]
- 12.Champion H R, Sacco W J, Copes WS et a l. A revision of the Trauma Score. J Trauma 198929623–629. [DOI] [PubMed] [Google Scholar]
- 13.Tepas J J, Mollit D L, Talbert J L.et al The pediatric trauma score as a predictor of injury severity in the injured child. J Pediatr Surg 19872214–18. [DOI] [PubMed] [Google Scholar]
- 14.Baker S P, O'Neill B, Haddon W.et al The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 197414187–196. [PubMed] [Google Scholar]
- 15.Boyd C R, Tolson M A, Copes W S. Evaluating trauma care: the TRISS method trauma score and the injury severity score. J Trauma 198727370–378. [PubMed] [Google Scholar]
- 16.Husum H, Strada G. Injury severity score versus new injury severity score for penetrating injuries. Prehosp Disast Med 20021727–32. [DOI] [PubMed] [Google Scholar]
- 17.Lavoie A, Moore L, LeSage N.et al The injury severity score or the new injury severity score for predicting intensive care unit admission and hospital length of stay. Injury Int J Care Injured 200536477–483. [DOI] [PubMed] [Google Scholar]
- 18.Osler T, Baker S P, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma 199743922–925. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan T, Haider A, DiRusso S M.et al Prediction of mortality in pediatric trauma patients: new injury severity score outperforms injury severity score in the severely injured. J Trauma 2003551083–1088. [DOI] [PubMed] [Google Scholar]
- 20.Murray J A, Chan D, Velmahos G C.et al Pediatric falls: Is height a predictor of injury and outcome? Am Surg 200066863–865. [PubMed] [Google Scholar]
- 21.Musemeche C A, Barthel M, Cosentino C.et al Pediatric falls from heights. J Trauma 1991311347–1349. [DOI] [PubMed] [Google Scholar]
- 22.Mosenthal A C, Livingston D H, Elcavage J.et al Falls: Epidemiology and strategies for prevention. J Trauma 199538753–756. [DOI] [PubMed] [Google Scholar]
- 23.Lehman D, Schonfeld N. Falls from heights: A problem not just in the Northeast. Pediatrics 199392121–124. [PubMed] [Google Scholar]
- 24.Pillai S B, Bethel C A I, Besner G E.et al Fall injuries in the pediatric population: Safer and most cost‐effective management. J Trauma 2000481048–1050. [DOI] [PubMed] [Google Scholar]
- 25.Roshkow J E, Haller J O, Hotson G C.et al Imaging evaluation of children after falls from a heights: Review of 45 cases. Radiology 1990175359–363. [DOI] [PubMed] [Google Scholar]
- 26.Moini M, Rezaishiraz H, Zafarghandi M R. Characteristics and outcome of injured patients treated in urban trauma centers in Iran. J Trauma 200048503–507. [DOI] [PubMed] [Google Scholar]
- 27.Meller J L, Shermeta D W. Falls in urban children. A problem revisited. AJDC 19871411271–1275. [DOI] [PubMed] [Google Scholar]
- 28.Goodacre S, Than M, Goyder E C.et al Can the distance fallen predict serious inury after a fall from a height? J Trauma 1999461055–1058. [DOI] [PubMed] [Google Scholar]
- 29.Isbister E S, Roberts J A. Autokabalesis: A study of intentional vertical decelartion injuries. Injury Int J Care Injured 199223119–122. [DOI] [PubMed] [Google Scholar]
- 30.Mathis R D, Levine S H, Phifer S. An analysis of accidental free falls from a height the "spring break" syndrome. J Trauma 199324123–126. [DOI] [PubMed] [Google Scholar]
- 31.Agalar F, Çakmakçi M, Sayek I. Factors effecting mortality in urban vertical free falls: Evaluation of 180 cases. Int Surg 199984271–274. [PubMed] [Google Scholar]
- 32.Grisoni E, Stallion A, Nance M L.et al The new injury severity score and the evaluation of pediatric trauma. J Trauma 2001501106–1110. [DOI] [PubMed] [Google Scholar]
- 33.Brenneman F D, Boulanger B R, McLellan B A.et al Measuring injury severity: time for a change? J Trauma 199844580–582. [DOI] [PubMed] [Google Scholar]
- 34.Frankema S P G, Steyerberg E W, Edwards J R.et al Comparison of current injury scales for survival chance estimation: an evaluation comparing the predictive performance of the ISS, NISS, and AP scores in a Dutch local trauma registration. J Trauma 200558596–604. [DOI] [PubMed] [Google Scholar]
- 35.Tay S, Sloan E P, Zun L.et al Comparison of the new injury severity score and the injury severity score. J Trauma 200456162–164. [DOI] [PubMed] [Google Scholar]